Abstract
Objective: To discuss the methods, timing and clinical outcomes of surgical treatment for open pilon fractures.
Methods: From April 2003 to July 2008, 28 patients with open pilon fractures were treated. All had type C fractures according to the Arbeitsgemeinschaft für osteosynthesefragen–Association for the Study of Internal Fixation (AO/ASIF) classification. Three operative methods were applied, the methods being determined by the types of fracture, soft tissue damage and time interval after injury. Seven cases were treated by debridement and internal fixation with plate; 19 by limited internal fixation combined with external fixation; and 2 by delayed surgery. The clinical outcomes were evaluated by the Burwell‐Charnley score.
Results: All cases were followed up for from 6 to 48 months (average 24 months). The Burwell‐Charnley score of clinical outcomes: anatomic reduction achieved in 12 cases, functional reduction in 15, and unsatisfactory reduction in 1. The healing time was from 2.5 to 11 months (average 4.7 months). Two cases had delayed union. According to the American Orthopaedic Foot and Ankle Society (AOFAS) scale for the ankle joint, there were excellent results in 8 cases, good in 14, fair in 5 and poor in 1. Complications included four cases of skin superficial sloughing, two of superficial infection, one of deep infection, two of delayed fracture union and ten of post‐traumatic arthritis.
Conclusion: It is important to perform appropriate surgeries for open pilon fracture according to fracture classification, different damage to skin and tissue and time interval after injury. Thorough debridement, proper use of anti‐infective medication, appropriate bone grafting, and postoperative ankle function exercise can reduce the occurrence of complications.
Keywords: Delayed operation, External fixators, Fractures open, Internal fixators
Introduction
Pilon fracture constitutes 1% of all lower limb fractures and about 3% to 10% of tibial fractures 1 , 2 . It is usually the result of high energy injury to the weight bearing area of the lower end of the tibia by the talus. Open fractures comprises about 10% to 30% of all pilon fractures 3 . These fractures are often associated with significant soft tissue degloving, metaphyseal bone defects and articular depression. In spite of improvements in surgical approaches and implants, treatment of tibial pilon fractures remains challenging 4 . In the present study, we discuss the methods, timing and clinical outcomes of surgical treatment for open pilon fractures.
Materials and Methods
Patient data
From April 2003 to July 2008, 28 patients with open tibial pilon fractures were treated in our hospital. There were 21 men and 7 women with an average age of 36.5 years (range, 19–61 years). Ten patients were injured on the left side, 17 on the right and 1 bilaterally (a closed fracture of the right malleolus was not counted). The interval between injury and presentation to our clinic ranged from 1 to 14 hours (average, 5.1 hours). The mechanisms of injury were high‐energy falls in 10 cases, motor vehicle accidents in 12, crushing injury in 4 cases, and sports injuries in 2. The fractures were classified according to the AO/ASIF system: 7 were classified as type C1, 17 type C2, and 4 type C3. Open soft tissue damage was graded according to the Gustilo system: 4 cases were classified as Gustilo I, 21 Gustilo II, 2 Gustilo IIIA, and 1 Gustilo IIIB. Combined injuries included fibular fractures in 25 cases, spinal fractures in 2, upper‐arm fractures in 2, rib fractures in 2, femoral fracture in 1, acetabular fracture in 1, calcaneal fracture in 1, and craniocerebral trauma in 1.
Methods
One of three different surgical protocols was performed in all patients, the choice being based on the condition of soft tissue, type of fracture and length of interval between injury and presentation for treatment.
Debridement, open reduction and internal fixation (ORIF)
This method was applied in type C1 fractures presenting with low‐grade soft tissue injury (Gustilo I, II) and interval between injury and presentation for treatment of less than 6 hours. Seven patients (four type C1 Gustilo I and three type C1 Gustilo II) were treated by this method. Surgical treatment of the pilon fractures was in four steps: (a) restoration of the correct length and stabilization of the fibula; (b) reconstruction of the articular surface of the tibia; (c) insertion of cancellous autografts; and (d) stabilization of the medial aspect of the tibia with the use of a modified cloverleaf plate. An anteromedial incision was employed to treat the tibial component and a lateral or posterolateral incision to treat the fibular fracture. The surgical incisions were planned based on the requirements of the fracture pattern, keeping in mind the soft‐tissue constraints of the individual injury. Skin closure was achieved with no tension. The tibial incisions were closed first. If necessary, the fibular incisions were left for delayed closure. One of the seven patients achieved primary closure of the medial incision, followed by delayed closure of the lateral one. A typical case is shown in Fig. 1.
Figure 1.

A 49 year‐old man with a low‐energy open pilon fracture (Gustilo I & C1) (a) Photograph showing open soft tissue injury (Gustilo I). (b) Preoperative anteroposterior and lateral radiographs showing Pilon fracture of type C1. (c) Postoperative radiographs showing the fractures have been anatomically reduced and fixed with plates. (d) Anteroposterior and lateral radiographs demonstrating fractures have healed 1 year after surgery.
Debridement, limited ORIF and external fixation
This method was applied in type C2 and type C3 fractures presenting with high‐grade soft tissue injury (Gustilo II, III) and interval between injury and presentation for treatment of less than 8 hours. Nineteen patients (16 type C2 Gustilo II, 1 type C2 Gustilo IIIA, and 2 type C3 Gustilo II) were treated by this method. The patients were managed by immediate debridement of the wound. Fibular fractures were always internally fixed, either with a 1/3 tubular plate or 3.5 mm compression plate. External fixation was applied across the ankle joint with pins in the calcaneus, metatarsal bone, and tibia, reconstruction of the ankle mortise, and stabilization with screws or Kirschner pins. Five of the 19 patients required bone grafting because of large defects of metaphyseal bone. One case underwent delayed closure of the lateral incision, and delayed split‐thickness skin grafting was applied in another case. A typical case is shown in Fig. 2.
Figure 2.
A 22 year‐old man with a high‐energy open pilon fracture (Gustilo II & C2) (a) Photograph showing open soft tissue injury (Gustilo II). (b) Preoperative radiographs showing Pilon fracture of type C2. (c) Postoperative radiographs showing the fractures have been anatomically reduced and fixed with external fixation, and the tibial fracture fixed with limited internal fixation. (d) Anteroposterior and lateral radiographs demonstrating the fractures have healed 1.5 year after surgery.
Debridement and calcaneal traction, delayed surgery
This method was applied in type C3 fractures accompanied by high‐grade soft tissue injury (Gustilo III) and interval between injury and presentation for treatment of more than 8 hours. In two patients (one type C3 Gustilo IIIA, one type C3 Gustilo IIIB), the surgeon chose a two‐stage procedure. The patients were put on calcaneal pin skeletal traction with elevation of the lower limb over a Bohler–Braun splint, and measures were taken to avoid edema. Wound drainage was removed when there was no further evidence of infection, and a second stage operation was performed when the edema had almost completely resolved. The patients were treated with limited ORIF and external fixation. The time interval between the two surgeries was 15 and 19 days, respectively. A typical case is shown in Fig. 3.
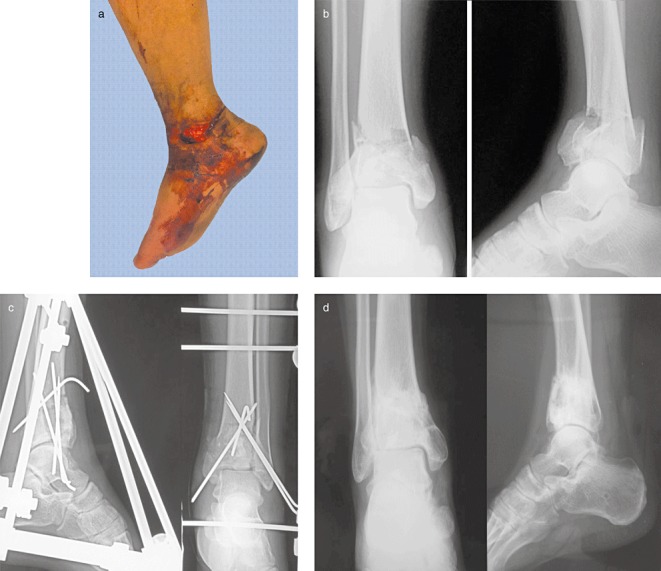
Figure 3.

A 37 year‐old man with a super high‐energy open pilon fracture (Gustilo IIIB &C3) (a) Photograph showing open soft tissue injury (Gustilo IIIB) (b) Preoperative radiographs showing Pilon fracture of type C3. (c) Postoperative radiographs showing the fractures have been anatomically reduced and fixed with external fixation, the tibial fixed with limited internal fixation, and the fibula with a plate. (d) Anteroposterior and lateral radiographs demonstrating the fractures have healed 1.5 year after surgery.
Postoperative care
Appropriate cultures were obtained during surgery, and broad‐spectrum antibiotics were administered. The choice of antibiotic was based on the extent and degree of contamination. The affected extremity was elevated continuously for the first 48 hours and then, as much as possible, for the next 7 days. Active ankle and subtalar joint range‐of‐motion exercises were begun as soon as the wound was dry, usually between 2 and 5 days after surgery. Weight‐bearing exercise was proscribed in the first 12 weeks after surgery. A supervised physical therapy program encouraging active ankle range‐of‐motion exercises was employed for the first 6 weeks. This was progressed to include passive exercises between 6 and 12 weeks. A Roll‐A‐Bout walker was used when necessary.
Results
All 28 patients were followed up from 6 to 48 months with an average of 24 months, and underwent clinical and radiological examination as outpatients. Radiographs were obtained and evaluated according to the Burwell‐Charnley system: anatomic reduction was achieved in 12 cases, functional reduction in 15 cases, and poor reduction in 1 case. The healing time of the fracture was from 2.5 to 11 months, with an average of 4.7 months.
Delayed union was found in two cases; in both it was associated with bone defects of the medial tibia. One stage wound closure was performed in 18 patients, two underwent delayed closure of their lateral incisions, and one underwent delayed split‐thickness skin grafting. There were four cases of superficial sloughing of the skin. Two patients developed surface infection with Staphylococcus epidermidis and Acinetobacter baumannii and one developed deep infection with Acinetobacter baumannii; the infection rate was 10.7% (3/28). Ten patients (35.7%) showed evidence of posttraumatic arthritis. According to the AOFAS ankle‐hind foot function evaluation, the average score was 85.2 (range, 66 to 98): excellent in 8 patients, good in 14, fair in 5, and poor in 1.
Discussion
Choice of surgical methods
In patients with type C1 fracture and Gustilo I soft tissue injury due to low‐energy forces, pilon fracture was anatomically reduced and treated with debridement and internal plate fixation following AO/ASIF principles. Open reduction and internal fixation were originally used, but it is now known that open reduction increases the risk of complications after high‐energy trauma. This is probably related to the amount of dissection and stripping of soft tissues which is needed to achieve reduction and plate fixation. Therefore, when performing ORIF procedures, the surgeons tried to limit soft tissue damage and choose suitable internal fixation. The tibia was reduced with a cloverleaf plate, dynamic compression plate or locking compression plate, depending on the level of the fracture and degree of stability required. Lin et al. reported an 83.3% good rate in 30 cases treated with ORIF followed up for 17 ∼ 39 months 5 . Kalenderer et al. also reported a similar result 6 .
External fixation and limited internal fixation were performed in all patients with type C2 and type C3 fractures presenting with high‐grade soft tissue injury (Gustilo II and III) and interval between injury and presentation at the authors' clinic of less than 8 hours. Use of external fixation during the surgical procedure enables the surgeon to assess the length and helps stabilize the limb for reconstruction of the intra‐articular component. Placement of the external fixator with a calcaneal pin and a half‐pin in the tibia allows ligamentotaxis to occur through traction on the calcaneal pin. This is helpful in reduction of the fracture and allows easier access to the ankle joint for joint reconstruction. Used as a neutralization device, there is no need for large plates with the associated increased risk of skin sloughing 7 . Minimizing internal fixation and damage to soft tissues and blood supply decreases the rate of skin sloughing and infection. We were able to correct postoperative loss of reduction by adjusting external fixation. It is also an excellent device in those severely comminuted fractures that do not allow stable fixation with the use of a plate. Several researchers have reported similar findings in regard to external fixation 8 , 9 , 10 , 11 .
Our results lead us to recommend that Type C3 tibial pilon fractures presenting with high‐grade soft tissue injury (Gustilo III) and interval between injury and presentation for treatment of more than 8 hours should be treated with a two‐stage procedure. At initial presentation, an external fixator is applied. After the soft tissues have recovered, the second stage is performed. The goal of the first stage is to re‐establish the length, alignment and rotation of the extremity and provide an environment for soft‐tissue recovery. The early application of a distraction force may help to limit any secondary injury and eliminate additional soft tissue compromise during surgical exposure 12 . Several reports have shown that the two‐stage procedure can reduce the rate of complications such as infection, skin sloughing, and post‐traumatic arthritis 13 , 14 , 15 .
Prevention of postoperative complications
It has been reported that the incidence of complications, including wound problems, skin sloughing, infection, nonunion, malalignment, joint stiffness and post‐traumatic arthritis, is high (45.1%) in patients with severe pilon fractures 16 .
Skin sloughing and infection are the most important early postoperative complications 17 . Pre‐existing severe soft tissue injury precludes open reduction in view of the potential wound problems due to ischemia or infection of the soft tissues. The precarious blood supply in this region of the tibia can contribute to the problems of both nonunion and infection 18 . In the present study, there were four cases of skin sloughing, two of superficial infections, and only one of deep bone infection. Surgical approaches are now planned based on the requirements of the fracture pattern, keeping in mind the soft‐tissue constraints of the individual injury. The incisions are kept at least 7 cm apart to prevent soft‐tissue ischemia and secondary wound breakdown. Intensive debridement, minimization of soft‐tissue stripping and proper use of antibiotics are useful for preventing infection.
Delayed union, especially in the metaphyseal portion, is also a problem with pilon fractures. We noted a 7.1% delayed union rate in this series. The severity of the injury and poor blood supply to the distal tibia may outweigh the affects of any particular approach when it comes to nonunion or delayed union, and it is also probably caused by tibial bone defect after fixation of the fibula. But there is not decided for the fibula fixation 19 , 20 . We think that fibular fracture should be fixed to restore the length of the lateral column of the tibia indirectly via ligament taxis. Megas et al. have reported that the nonunion rate in distal tibial fracture is higher than in other long bone fractures 21 . It can likely be prevented by minimizing soft‐tissue stripping and using stable internal fixation in association with suitable bone graft.
Post‐traumatic arthritis is a serious complication. Wyrsch et al. believe that arthritis is possibly caused by damage to articular cartilage and long‐term immobilization with external fixators and plaster casts 22 . We found that 9 of 10 cases of post‐traumatic arthritis developed after type C2 or type C3 fractures. Rose reported that circular frames or hybrid systems, which may be applied with a hinge axis movement at the level of the ankle joint, may become useful alternatives for improving the range of motion of the ankle 11 . Arthrodesis is indicated for the most severe arthritic changes.
However, the most important tool remains experienced operative assessment of the specific characteristics of the injury, leading to the selection of the optimal treatment plan for any given patient. It is important to make the right choice in regard to the timing of surgery and correct method of fixation according to fracture classification, extent and type of damage to skin and tissue, and interval between injury and reaching the hospital. It is the key that the correct evaluation of skin and tissue and the good protection of the blood supply to the bone. Intensive debridement, proper use of antibiotics, appropriate bone grafting, and postoperative ankle function exercise can reduce the occurrence of complications.
Disclosure
This manuscript does not contain information about medical device(s)/drug(s). No benefits in any form have been, or will be, received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1. Wang YC. Fractures and Joint Injury, 4th edn. Beijing: People's Medical Publishing House, 2007; 1469. [Google Scholar]
- 2. Zhang B, Huang L, Wang MY, et al Surgical treatment of tibial pilon fracture (Chin). Zhonghua Gu Ke Za Zhi, 2001, 21: 403–407. [Google Scholar]
- 3. Craig S, Bartlett III, Lon S, et al Fracture of the tibial pilon In: Browner B, Jupiter J, Levine A, et al, eds. Skeletal Trauma, 3rd edn. Singapore: Elsevier, 2003; 2257. [Google Scholar]
- 4. Zhang JG, Lin FS, Yin SB, et al The prognostic relative factors in treatment of tibial pilon fracture. Zhonghua Gu Ke Za Zhi, 2004, 24: 44–47. [Google Scholar]
- 5. Lin MS, Lee HM, Hou YT, et al Treatment of tibial pilon fractures using the Link May Anatomic Bone Plate. J Chin Med Assoc, 2003, 66: 423–428. [PubMed] [Google Scholar]
- 6. Kalenderer O, Güneş O, Ozçalabi IT, et al Clinical results of tibial pilon fractures treated by open reduction and internal fixation. Acta Orthop Traumatol Turc, 2003, 37: 133–137. [PubMed] [Google Scholar]
- 7. Piper KJ, Won HY, Ellis AM. Hybrid external fixation in complex tibial plateau and plafond fractures: an Australian audit of outcomes. Injury, 2005, 36: 178–184. [DOI] [PubMed] [Google Scholar]
- 8. Golubović Z, Macukanović‐Golubović L, Stojiljković P. External fixation combined with limited internal fixation in the treatment of pilon tibia fractures. Vojnosanit Pregl, 2007, 64: 307–311. [DOI] [PubMed] [Google Scholar]
- 9. Leung F, Kwok HY, Pun TS, et al Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury, 2004, 35: 278–283. [DOI] [PubMed] [Google Scholar]
- 10. Endres T, Grass R, Biewener A, et al Advantages of minimally‐invasive reposition, retention, and Ilizarov‐(hybrid)fixation for pilon‐tibial‐fractures fractures with particular emphasis on C2/C3 fractures. Unfallchirurg, 2004, 107: 273–284. [DOI] [PubMed] [Google Scholar]
- 11. Rose R. Treatment of pilon fractures using the Ilizarov technique. Case reports and review of the literature. West Indian Med J, 2002, 51: 176–178. [PubMed] [Google Scholar]
- 12. Scalea TM, Boswell SA, Scott JD, et al External fixation as a bridge to intramedullary nailing for patients with multiple injuries and with femur fractures: damage control orthopedics. J Trauma, 2000, 48: 613–623. [DOI] [PubMed] [Google Scholar]
- 13. Haidukewych GJ. Temporary external fixation for the management of complex intra‐ and periarticular fractures of the lower extremity. J Orthop Trauma, 2002, 16: 678–685. [DOI] [PubMed] [Google Scholar]
- 14. Blauth M, Bastian L, Krettek C, et al Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma, 2001, 15: 153–160. [DOI] [PubMed] [Google Scholar]
- 15. Gardner MJ, Mehta S, Barei DP, et al Treatment protocol for open AO/OTA type C3 pilon fractures with segmental bone loss. J Orthop Trauma, 2008, 22: 451–457. [DOI] [PubMed] [Google Scholar]
- 16. Kilian O, Bündner MS, Horas U, et al Long‐term results in the surgical treatment of pilon tibial fractures. A retrospective study. Chirurg, 2002, 73: 65–72. [DOI] [PubMed] [Google Scholar]
- 17. Topliss CJ, Jackson M, Atkins RM. Anatomy of pilon fractures of the distal tibia. J Bone Joint Surg Br, 2005, 87: 692–697. [DOI] [PubMed] [Google Scholar]
- 18. Babis GC, Vayanos ED, Papaioannou N, et al Results of surgical treatment of tibial plafond fractures. Clin Orthop Relat Res, 1997, 341: 99–105. [PubMed] [Google Scholar]
- 19. Varsalona R, Liu GT. Distal tibial metaphyseal fractures: the role of fibular fixation. Strat Traum Limb Recon, 2006, 1: 42–50. [Google Scholar]
- 20. Williams TM, Marsh JL, Nepola JV, et al External fixation of tibial plafond fractures: is routine plating of the fibula necessary? J Orthop Trauma, 1998, 12: 16–20. [DOI] [PubMed] [Google Scholar]
- 21. Megas P, Panagiotopoulos E, Skriviliotakis S, et al Intramedullary nailing in the treatment of aseptic tibial nonunion. Injury, 2001, 32: 233–239. [DOI] [PubMed] [Google Scholar]
- 22. Wyrsch B, McFerran MA, McAndrew M, et al Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am, 1996, 78: 1646–1657. [DOI] [PubMed] [Google Scholar]


