Abstract
Objective: To investigate the outcome of a laminoplasty technique without additional instrumentation for fixation of laminae in the treatment of extramedullary intradural tumors in the thoracic and lumbar spine.
Methods: Twenty‐four patients (15 men and 9 women) with extramedullary intradural tumors in the thoracic and lumbar spine were included in our study. The average age was 36.2 years (range 18 to 61 years). The pathological diagnosis was neurofibroma in 13, ependymoma in 6, lipoma in 2 and teratoma in 3 cases. All patients underwent the same laminoplasty surgery as follows: the laminae were reattached to their original sites, the ligaments (including the supraspinal, interspinal and yellow ligaments) were conserved, and primary stability of the re‐attached laminae was achieved with silk or nylon sutures.
Results: Sixty‐six laminae were re‐implanted in 24 patients. The average length of follow‐up was 34.2 months (26.5 to 41 months). Fusion of the laminae was achieved in a mean of 4.5 months (3 to 6 months). Unilateral healing of the incision lines was observed in seven cases, including one with two‐level laminotomy, three with three‐level laminotomy and three with four‐level laminotomy. The other 17 cases underwent bilateral fusion.
Conclusion: Fixing the laminae, spinous processes and ligaments with sutures can achieve satisfactory primary stability and high fusion rates for resected laminae. Additional instrumentation may be necessary in greater than three‐level laminoplasty.
Keywords: Laminectomy, Spinal cord neoplasms, Treatment outcome
Introduction
The technique of laminoplasty, which has been widely used in thoracic and lumbar spinal surgery, especially in cases of intradural tumor and lumbar spinal canal stenosis (LSCS), can preserve the posterior arch of the spine, protect paraspinal muscles, and prevent postoperative instability, epidural adhesion and kyphotic deformities. Compared with LSCS, with laminoplasty after excision of intradural tumors it is relatively easy to preserve the osseous structure and obtain anatomical reconstruction of the posterior structure, because it is not necessary to enlarge the spinal canal or lateral recess, nor to excise the ligamentum flavum for decompression of the cauda equina and nerve roots. Moreover, considering that intradural tumors can recur, the technique of laminoplasty makes revision surgery much easier, as it is safer to expose the dura after this type of surgery than after traditional laminectomy, because it preserves a relatively normal posterior bony structure and there is no epidural scar; hence laminoplasty may be a suitable option for this type of patient.
Many reconstructive methods have been reported in the literature, such as transverse placement laminoplasty, restorative laminoplasty, inverse laminoplasty, en bloc laminoplasty, and expansive laminotomy 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 . In our study, the laminae were reattached to their original sites, the ligaments were conserved and fixation was achieved with sutures. We reported the five‐year clinical results of laminoplasty for the treatment of LSCS in 1995 6 . In the present study, we have retrospectively reviewed the medical records of twenty‐four patients with a greater than two‐year follow‐up who underwent laminoplasty for the treatment of extramedullary intradural tumors in the thoracic and lumbar spine.
Materials and methods
Twenty‐four patients (15 men and 9 women) with extramedullary intradural tumors in the thoracic and lumbar spine were included in our study. The average age was 36.2 years (range 18 to 61 years). Pathological examination revealed neurofibromas in 13, ependymomas in 6, lipomas in 2 and teratomas in 3 cases. The tumors occupied a single vertebral level in eight, extended to involve two levels in nine, three levels in six, and four levels in one case. All patients underwent routine X‐rays, CT and MRI before surgery. Twelve cases were located in the thoracic region (single level in two, two levels in three, three levels in six, and four levels in one case), seven cases (single level in three, and two levels in four cases) were in the lumbar region and five cases were in the thoracolumbar region (single level in three, and two levels in two cases).
Surgical technique
After general anesthesia, patients were put in a prone position. Through a midline posterior approach, the paravertebral muscles were detached from the spinous processes and laminae, preserving the supraspinal and interspinal ligaments. The laminae were cut carefully in a trapezoid manner just medial to the facet joints on both sides. Osteotomy was performed with a micro‐saw and custom‐made thin osteotome to minimize bone loss from the laminae. The inferior half of the spinous process of the superior adjacent vertebra, superior half of the spinous process of the inferior adjacent vertebra and ligamentum flavum were removed. The laminae and spinous processes were carefully elevated en bloc from the caudal to the cranial side to expose the dura. After the tumors had been excised under microscopic magnification, the laminae were reattached to their original sites and fixed by suturing the detached yellow ligament (or with sutures passed through the bony holes at each edge of the laminae). The spinous processes were also fixed to the residual or adjacent spinous processes with sutures through holes. Finally, the supraspinous ligaments were also sutured to help keep the spinous processes and laminae in situ. Gauge 10# silk or nylon sutures were used in all procedures for fixation of the laminae and spinous processes (Fig. 1).
Figure 1.
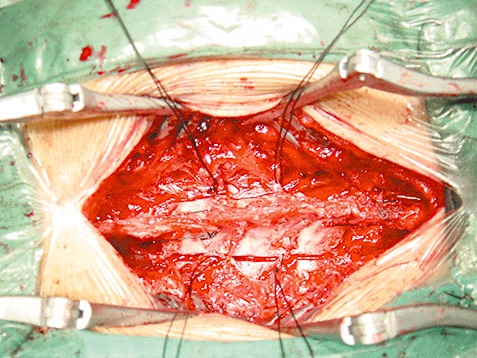
Intraoperative photograph showing the reattached laminae and spinous processes being fixed by 10# sutures.
After the operation, an external brace was used for two weeks in the case of thoracic surgery and four for lumbar surgery. Patients began ambulation with the brace one day after thoracic surgery and twelve days after lumbar surgery.
During postoperative follow‐up, the patients underwent X‐rays and/or MRI examination to monitor the alignment of spine, and to allow the Cobb angle to be measured pre‐operatively and at final follow‐up to evaluate sagittal alignment of the spine. The angle between intersecting lines drawn perpendicular to the top of the vertebra one‐level above the top vertebra, and the bottom of the vertebra one‐level below the bottom vertebra, was determined to be the Cobb angle. MRI and/or CT were used to assess fusion of the laminae, observe the epidural scar and exclude tumor recurrence. Bony fusion was defined as the incision lines in the laminae having disappeared and callus having formed at the unilateral or bilateral cut edges of the laminae. A 10 cm‐ visual analog scale (VAS) was used to assess the severity of back pain (0 indicates no pain and 10 represents the worst pain).
Statistical analysis
A SPSS 12.0 software package (SPSS, Chicago, IL, USA) was used for statistical analysis. To assess statistical significance, an unpaired t‐test was performed. A P value of <0.05 was considered significant.
Results
Sixty‐six laminae were re‐implanted in 24 patients (2.8 laminae on average). Two‐level laminotomy was performed in eight, three‐level in fourteen and four‐level in two patients. The average operative time was 137 min (range 90–205 min). Blood loss was 260–600 ml (mean 320 ml). Two cases had postoperative complication including cerebrospinal fluid (CSF) leakage in one case which was treated by lumbar CSF drainage; and recurrence in one case, who underwent revision surgery (Fig. 2).
Figure 2.
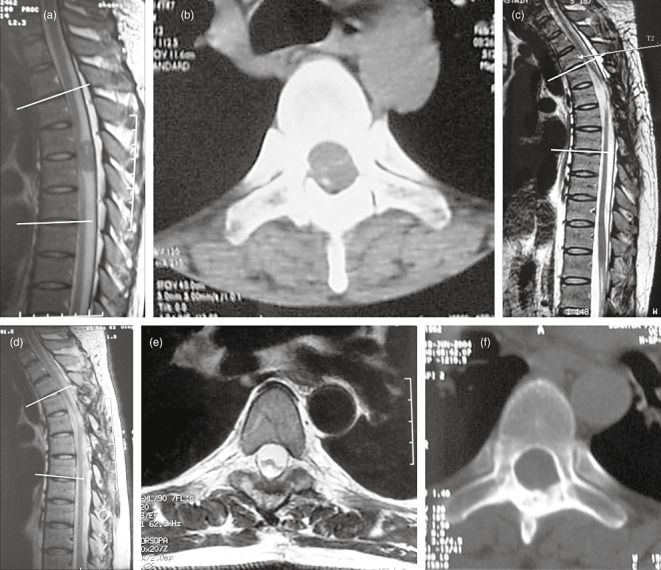
Thirty years old male patient. (a) Preoperative CT scan showing a neurofibroma at T4,5. The preoperative Cobb angle is 16.3°. (b) An immediately postoperative CT scan showing the laminae have been reattached to their original sites. (c) Ct scan showing recurrence of tumor one year after surgery, the Cobb angle is 28.9°. (d) Two years after the second surgery, the Cobb angle is 28.5°. (e) The cross‐sectional MRI showing the dura mater has a clearly defined boundary without epidural adhesion 2 years after revision surgery. (f) CT scan showing bilateral fusion of laminae.
The average time of follow‐up was 34.2 months (26.5–41 months). The preoperative American Spinal Injury Association (ASIA) impairment scale was A in two cases, B in two, C in seven, D in seven, and E in six. The postoperative ASIA impairment scale had improved from A to B in one case, A to C in one, B to C in one, B to D in one, C to D in four, and in all other cases to E. The pre‐ and post‐operative VAS for back pain was 5.1 ± 1.1 and 1.5 ± 1.2, respectively (P < 0.05). According to post‐operative X‐rays, MRI and/or CT, fusion of laminae was achieved in 3 to 6 months (mean 4.5 months). The pre‐operative and post‐operative Cobb angles were 16.5 ± 5.0 and 18.4 ± 11.4 respectively, and there was no significant difference (P > 0.05).
The healing style of incision liness in the laminae can be divided into two types: unilateral and bilateral fusion. The former was observed in seven cases, including one with two‐level laminotomy, three with three‐level and three with four‐level. The other 17 cases achieved bilateral fusion. There was no postoperative instability, adhesion between dura and re‐attached laminae or spinal cord compression caused by scar formation under the laminae according to follow‐up with X‐rays and MRI.
Discussion
The differences between laminoplasty techniques relate mainly to: (i) the range of laminotomy; (ii) the method of reconstructing the laminae, which include reattaching to the original site, and rotating or inversing the laminae to a certain degree; (iii) whether or not the supraspinal and interspinal ligaments are conserved; (iv) and the instrumentation used for fixation of the laminae, which include mini‐plates, sutures, screws or polylevolactide (PLLA) pins. In this study, the laminae were reattached the laminae to their original sites, ligaments were conserved and fixation was achieved with sutures. To our knowledge, there has thus far been no long time follow‐up report of this technique.
Hara et al. 2 and Kawahara et al. 4 have reported a similar method for laminotomy using a T‐saw. The disadvantage of this technique is that the range of osteotomy is larger and the facet capsules have to be removed. In the recent literature, the most popular method of osteotomy has been to make gutters just medial to the facet joints to avoid instability after surgery, and to remove the laminae in a trapezoid manner to prevent them sinking into the spinal canal7. In our cohort, we used the second method, which also provides good exposure of the tumors during the operation, and reduces the trauma.
We used sutures for fixation of the laminae. Hara et al. 2 and Kawahara et al. 4 reported no complications due to suture fixation. However, with this procedure it is necessary to wear a brace for longer than with mini‐plate or pins fixation. Hara et al. reported that their patients were instructed to wear a simple cervical collar or lumbar brace for 2 months when laminoplasty had been performed without internal fixation, while no brace was required if the patient underwent thoracic laminoplasty after the operation 2 . Kawahara et al. reported that their patients needed to wore an orthosis for 2 to 4 months while bone healing occurred 4 . In our institution, we gave patients only 2–4 weeks external fixation after surgery, yet also achieved good fusion of the laminae. Our results suggest that the re‐attached laminae can provide effective primary stability after fibrous healing between the incision lines in the laminae, and among the interfaces of the paraspinal musculature, laminae and spinous processes.
Re‐attaching the laminae to the correct anatomical site may make it easier to reconstruct osteotomized spinous processes and detached ligaments, which are also very important in spinal mechanical stability and preventing postoperative epidural scarring. Moreover, it may be easier to get incision line fusion than with other methods. The fusion time of laminae ranges from 1.9 months to 5 months according to the literature. Yücesoy and Crawford reported that, using inverse laminoplasty, bony fusion of the incision line of the laminae was seen in only one third of patients who were monitored for more than 2 years 10 . Wiedemayer et al. reconstructed the laminar roof with miniplates to the anatomical site in 79 cases (laminae) 7 . In his follow‐up results, 11.3% laminae achieved unilateral fusion while 2.6% developed no osseous bridging of the osteotomy sites on either side. In our study, the time to achieve fusion of the laminae averaged 4.5 months, among our patients seven laminae (10.6%) achieved unilateral fusion of the incision line in the laminae, while in no case was bilateral nonunion observed.
During follow‐up, we found that unilateral fusion of the laminae occurred mainly in patients who had undergone laminoplasty at three or four levels. Unilateral fusion may have been due to bone deficits between the incision lines in the laminae and/or micro‐movement after surgery. As the laminae are connected by spinous processes and ligaments, unilateral fusion in one lamina may not affect the overall stability. These results may also demonstrate that the stability of laminae is reduced where laminoplasty has been performed at more than three levels, in which case additional instrumentation may be necessary. Another reason for us not using additional instrumentation is the poor economic circumstances of some Chinese patients.
Progressive neurological deficit and pain after laminectomy may be partly due to epidural scarring. Many materials and drugs have been used in an attempt to prevent scar formation; however some of them may cause infection and none of them has achieved a reliable outcome. With our method, we conserved both the laminae and ligamentum flavum. According to the follow‐up MRI in our cohort, we did not find adhesions between the dura and re‐attached laminae. The patients achieved good recovery of neurological function and had no, or only minor, pain after surgery. During the second surgery of the case in our cohort who developed a recurrence, we were easily able to expose and remove the laminae just as we had done during the primary surgery. We also did not find any adhesions between the laminae and dura, or between the ligamentum flavum and dura. The laminae and ligamentum flavum may be effective and safe at preventing epidural adhesions. All in all, this method may be better than those techniques in which only the posterior bony structure of the spine is reconstructed.
Papagelopoulos et al. reported 14‐year follow‐up results after multilevel lumbar or thoracolumbar total laminectomy for removal of benign intraspinal tumors 13 . Spinal column deformity occurred in 33% of the children and adolescents and in 8% of the young adults. Spondylolisthesis occurred in 16.6% of the children and adolescents and in 8% of the young adults. Yeh et al. found that laminectomy is associated with a worse alignment at the thoracic‐thoracolumbar region, while laminoplasty reduces this risk in children 9 . Hida et al. reported the results of a more than 2‐year follow‐up of transverse placement laminoplasty 3 . His report demonstrated that, compared with laminectomy, sagittal alignment was well conserved by laminoplasty. We consistently failed to find obvious developmental deformity during follow‐up of our cases, except in one patient who had a recurrence of tumor and underwent revision surgery. However, Wiedemayer's results show that laminoplasty does not prevent worsening of any pre‐existing deformity 7 . Pre‐operative kyphotic deformity tends to increase the risk of worsening alignment post‐operatively 14 , thus rigid internal fixation may be necessary for this type of case. In this series, the laminoplasty technique was used in four cases of thoracic extramedullary intradural tumors involving three or four levels, all of which achieved good sagittal alignment during postoperative follow‐up. This may be related to the relative stability of the thoracic region.
As the supraspinous and interspinal ligaments can provide a tethering or tension constraint during anterior flexion, and support for the lumbar muscles in all body positions, it may be useful to reconstruct posterior stability and thus prevent kyphotic deformity to some extent.
Another advantage of our technique is that we try to achieve fusion of the spinous processes instead of fibrosis fusion of the supraspinous and interspinal ligaments in the lumbar or thoracolumbar regions, which may provide more posterior stability of the spine, this possibility warrants further biomechanical investigation.
There are two shortcomings of this technique: (i) after laminoplasty, external fixation for an extended period of time is necessary, which prolongs the period of bed rest and prevents the patients from undergoing early mobilization and rehabilitation; (ii) multiple laminoplasty (at more than three levels) for the treatment of extramedullary intradural tumors should not be considered in patients with lumbar or cervical tumors, in order to avoid spinal instability, especially in young patients.
In this research, we investigated the outcome of a laminoplasty technique without additional instrumentation for fixation of laminae in the treatment of extramedullary intradural tumours in the thoracic and lumbar spine. Fixing the laminae, spinous processes and ligaments with sutures can achieve satisfactory primary stability and high fusion rates for resected laminae. Additional instrumentation may be necessary in greater than three‐level laminoplasty.
References
- 1. Adachi K, Futami T, Ebihara A, et al. Spinal canal enlargement procedure by restorative laminoplasty for the treatment of lumbar canal stenosis. Spine J, 2003, 3: 471–478. [DOI] [PubMed] [Google Scholar]
- 2. Hara M, Takayasu M, Takagi T, et al. En bloc laminoplasty performed with threadwire saw. Neurosurgery, 2001, 48: 235–239. [DOI] [PubMed] [Google Scholar]
- 3. Hida S, Naito M, Arimizu J, et al. The transverse placement laminoplasty using titanium miniplates for the reconstruction of the laminae in thoracic and lumbar lesion. Eur Spine J, 2006, 15: 1292–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kawahara N, Tomita K, Shinya Y, et al. Recapping T‐saw laminoplasty for spinal cord tumors. Spine, 1999, 24: 1363–1370. [DOI] [PubMed] [Google Scholar]
- 5. Mimatsu K. New laminoplasty after thoracic and lumbar laminectomy. J Spinal Disord, 1997, 10: 20–26. [PubMed] [Google Scholar]
- 6. Wang Y, Chen Z, Li M, et al. Extensive plasty of the lumbar canal: clinical application of laminae and spinous processes replantation(Chin). Zhonghua Gu Ke Za Zhi, 1995, 15: 644–647. [Google Scholar]
- 7. Wiedemayer H, Sandalcioglu IE, Aalders M, et al. Reconstruction of the laminar roof with miniplates for a posterior approach in intraspinal surgery: technical considerations and critical evaluation of follow‐up results. Spine, 2004, 29: E333–E342. [DOI] [PubMed] [Google Scholar]
- 8. Wiedemayer H, Schoch B, Stolke D. Osteoplastic laminotomy using titanium microplates for reconstruction of the laminar roof: a technical note. Neurosurg Rev, 1998, 21: 93–97. [DOI] [PubMed] [Google Scholar]
- 9. Yeh JS, Sgouros S, Walsh AR, et al. Spinal sagittal malalignment following surgery for primary intramedullary tumours in children. Pediatr Neurosurg, 2001, 35: 318–324. [DOI] [PubMed] [Google Scholar]
- 10. Yücesoy K, Crawford NR. Increase in spinal canal area after inverse laminoplasty: an anatomical study. Spine, 2000, 25: 2771–2776. [DOI] [PubMed] [Google Scholar]
- 11. Yücesoy K, Ozer E. Inverse laminoplasty for the treatment of lumbar spinal stenosis. Spine, 2002, 27: E316–E320. [DOI] [PubMed] [Google Scholar]
- 12. Zheng Y, Guan T, Liu X, et al. Thoracic laminoplasty for the treatment of tumor in spinal canal (Chin). Ji Zhu Wai Ke Za Zhi, 2004, 2: 193–195. [Google Scholar]
- 13. Papagelopoulos PJ, Peterson HA, Ebersold MJ, et al. Spinal column deformity and instability after lumbar or thoracolumbar laminectomy for intraspinal tumors in children and young adults. Spine, 1997, 22: 442–451. [DOI] [PubMed] [Google Scholar]
- 14. Zheng Y, Liu X, Du W, et al. The clinical value of Total laminotomy and re‐implantation for the treatment of ossification of the thoracic ligamentum flavum(Chin). Zhonghua Gu Ke Za Zhi, 2004, 24: 728–732. [Google Scholar]


