Abstract
Objective
To identify the most effective treatment for application to high‐energy complex plateau fractures.
Methods
125 patients with closed high‐energy complex tibial plateau fractures who had been surgically treated between 2003 and 2010 were reviewed retrospectively. Five procedure methods were studied (e.g. four open reduction and internal fixations, and close reduction via a minimal incision with hybrid external fixation) in five surgical timings, with a control group. The incidence of wound complications after operative treatment in the five surgical timings and the clinical effects of the five surgical procedure options were evaluated statistically. A postoperative follow‐up ranging 26–110 months (mean, 36.5 months) was performed.
Results
Among the various groups, the respective overall wound complication incidences were 20.0%, 41.6%, 33.3%, 2.5%, and 16.7% within 4 hours, 4 hours to 3 days, 3–5 days, 5–8 days, and more than 8 days after injury. Failed fixation was clearly observed in Group 1 (23.1%, 6/26) and Group 5 (21.7%, 5/23) (P < 0.05). Significant differences were also found among Group 2 (92.6%), Group 3 (93.3%), and Group 5 (69.6%), in terms of the good and excellent rate of joint function according to the Rasmussen score (P < 0.05).
Conclusion
The optimal surgical timing is within 4 hours after trauma, for which no obvious swelling was observed in the limbs. This is followed by surgical timing within 5–8 days, after which trauma showed only subsided limb swelling. Dual plating provides the best stabilization option, as it allows early joint mobilization, cartilage regeneration, and joint remodeling, thus decreasing the risk of joint stiffness. Hybrid external fixation may provide relative stability to maintain fracture alignment without the need for massive soft tissue dissection, and also minimizes blood loss and potential soft tissue complications.
Keywords: Procedures, Surgical timing, Tibial plateau fractures
Introduction
Closed high‐energy complex (Schatzker V and VI1) tibial plateau fracture represents a treatment challenge with severe soft tissue damage2, which is usually further complicated by significant articular depression, multiple displaced condylar fracture lines, metadiaphyseal fracture extension and comminution, and considerable soft tissue injuries3.
Various methods for treating these complex injuries have been proposed, including double‐buttress plate fixation4, hybrid external fixation, internal fixation with locking plates, and the minimally invasive plate osteosynthesis (MIPO) technique5, solitary plate via one anterior incision6, and dual plating via a two‐incision technique7. Numerous studies have demonstrated that early knee movement is a critical factor affecting the outcome of surgery8. However, the surgical timing of high‐energy complex tibial plateau fractures remains controversial. Some authors believe that the surgical timing of severe tibial plateau fractures does not have an effect on the rate of infection9. Contrary to this belief, Koval and Helfet pointed out that the surgery timing and the handling of the soft tissue were critical to treatment success10. Operative procedures may result in various complications such as wound dehiscence, wound necrosis, superficial wound infection, deep wound infection, malunion, posttraumatic osteoarthritis, failed fixation, lower extremity deep vein thrombosis (DVT), pulmonary embolism, or even amputation7, 8. Therefore, when treating complex tibial plateau fractures, it is necessary to take into account the fracture and soft tissue injury. Although various procedure options for complex tibial plateau fractures have been recommended previously, there is a lack of data for comparing surgical timing and procedure options to closed high‐energy complex tibial plateau fractures.
The purpose of this study is to analyze the incidence of wound complications of closed high‐energy complex tibial plateau fractures after operative procedures in the study hospital. The authors wished to identify risk factors leading to these complications, and to determine which surgical procedure options would lead to the optimal operative effect.
Materials and Methods
The authors retrospectively reviewed 125 patients with closed high‐energy complex tibial plateau fractures, who had been surgically treated in the study hospital between 2003 and 2010. Thirteen patients could not be reached, thus only 112 patients participated in the follow‐up process. Only patients satisfying the following inclusion criteria were covered: closed high‐energy complex tibial plateau fracture, severe soft tissue injury of Tscherne and Oestern grades 2 and 3, Schatzker types V and VI, closed bicondylar plateau fracture, and aged 18–60 years. Exclusion criteria: complication with other fractures in the ipsilateral limb, open fracture, aged more than 60 years or less than 18 years, and complication with serious medical disorders (i.e. severe cardiovascular or cerebrovascular diseases, hemiplegia, etc.) which would affect limb functions. The patients included 66 males and 46 females, with a mean age of 35.2 years (ranging from 18 to 58 years). The fracture was on the left side of the body in 57 patients, and on the right side in 55 patients. Among the 112 fractures, there were 58 Schatzker V and 54 Schatzker VI injuries. Among these, 14 patients were complicated with life‐threatening head (4 patients), chest (6 patients), and abdominal (4 patients) injuries.
Operative Technique
The Schatzker classifications were used to classify each fracture pattern based solely on the X‐rays1. Four patients with vascular injuries or compartment syndrome were operatively treated immediately. For the others, immobilization with plaster or calcaneal traction, topical application of ice packs, or raising the affected limb was performed after admission. The patients underwent resuscitation and treatment according to advanced trauma life support (ATLS) protocols, which involved treatment of life or limb threatening injuries. Decisions regarding the method of initial immobilization and timing of definitive fixation followed a specific treatment algorithm, which was based on the orthopaedic surgeon's experience and judgment. The negative pressure drainage was removed 24 to 48 hours and the sutures 10 days after operation. Patients were mobilized using a hinged knee brace which allowed 90° knee movement. They were advised to remain non‐weight bearing for six weeks and touch weight‐bearing for a further six weeks. The patients were then allowed to progress to full weight‐bearing by eighteen weeks. After general anesthesia, the patients also received 0.75 g of intravenous cefuroxime sodium as a prophylactic antibiotic. Postoperatively, all patients received an intravenous injection of cefuroxime sodium (0.75 g) in a 10 ml saline solution, three times a day for five days. Thromboprophylaxis with subcutaneous heparin was given to all patients during their stay at the hospital. The patients were divided into the following five groups.
Group 1 (open reduction and internal fixation with one plating via anterolateral incision): 26 patients. The operation was performed under general anesthesia with endotracheal intubation. The patients were placed in the supine position, and a routinely employed pneumatic tourniquet was used. The anterolateral incision was begun 2 cm lateral to the patella and extended distally over the Gerdy tubercle and 1 cm lateral to the crest of the tibia, for a total length of approximately 15 cm. The fracture was reduced and held temporarily with bone clamps. An adequate plate length of the AO locking compression plate (LCP) proximal tibial plate or locking plate was contoured to adapt to the lateral condyle. An autologous iliac bone was implanted when necessary. One patient underwent meniscectomy, and three received repair of the knee cruciate ligament.
Group 2 (open reduction and internal fixation with dual plating via anterolateral and posteromedial incisions): 27 patients. Anesthesia, body position, tourniquet and the anterolateral incision were performed in the same manner as Group 1. Based on the anterolateral incision, a posteromedial incision was made. Two vertical curved incisions >8 cm in width were made from the posteromedial to anterolateral. An incision was made 1 cm posterior to the posteromedial border of the tibial metaphysis, with dissection through the interval between the pes anserinus tendons and the medial head of the gastrocnemius. The fracture was reduced and a 3.5 mm reconstruction plate was fixed. Then, the lateral tibial condyle was exposed and fixed in the same manner as Group 1. One patient underwent meniscectomy, four received repair of the medial collateral ligament, and one received repair of the anterior cruciate ligament.
Group 3 (open reduction and internal fixation with dual plating via single midline incision): 30 patients. Anesthesia, body position and tourniquet were performed in the same manner as Group 1. An incision of the anterior midline was made in the center of the patella, from 2 cm above the patella via the medial patella and tibial tubercle insertion to the anterior crest of the top of the tibial shaft (18 cm in length). The incision was moderately dissected subperiosteally to expose the medial tibial plateau fracture ends, temporarily fixed by Kirschner wire, and stabilized by means of a reconstruction plate. Afterwards, the lateral tibial condyle was exposed and fixed in the same manner as Group 1. During surgery, three patients received repair of cruciate ligament injury, two received repair of the medial collateral ligament, and three underwent meniscectomy.
Group 4 (open reduction and internal fixation with dual plating via combined anterior and posterior approaches): 6 patients. After general anesthesia was performed, a pneumatic tourniquet was tied around the thigh at the prone position. First, for the posteromedial approach, a longitudinal posteromedial incision was made about 10 cm over the medial head of gastrocnemius. After opening the deep fascia, the interval between the medial head of gastrocnemius and semitendinosus was identified, and the medial head of gastrocnemius was retracted laterally, helping to protect the neurovascular structures11. The posterior aspect of the proximal tibia was then palpated, exposed, and reduced. The pre‐bending reconstruction plate was placed and internally fixed by screws. Then the patients were placed in the supine position, and the lateral tibial condyle was exposed and fixed in the same manner as Group 1. Two patients received repair of posterior cruciate ligament, one received anastomosis repair of the popliteal artery, and one received release and decompression by exploration of the common peroneal nerves.
Group 5 (close reduction/via a minimal incision with hybrid external fixation): 23 patients. The patients were placed in the supine position. A radiolucent operating table and fluoroscopy were used. The operations were performed under local anesthesia with lidocaine. An assistant aligned the fragments via simple manual traction. The condylar fragments were compressed with large tenaculum forceps12. Failure to reduce the articular fragments, or the presence of articular depression, often necessitated an open reduction through a small anteromedial or anterolateral approach, in order to elevate the articular surface. Six external fixing pins were inserted percutaneously at the proximal and distal fracture ends, and connecting rod and fixation clamps were placed (Constant, Wuhan, China). Three patients received spanning external fixation.
Follow‐ups were performed for all patients 1, 3, 6, and 12 months after surgery, and once per year thereafter. Radiographs were made during every follow‐up visit. The patients were examined at an orthopaedic clinic service center, and the clinical examinations were carried out by senior surgeons.
For each patient, the surgical timing, intraoperative blood loss, postoperative wound complications, fracture healing time and functional outcome scores were recorded. Functional outcome scores and visual analogue pain scales were recorded by a research nurse. The range of movement of the knee was measured using a goniometer. Valgus and varus instability were measured at 20° of knee flexion and compared with that on the uninjured side. Fracture union was clinically defined as a lack of pain and tenderness and the ability to ambulate without any aid; radiographically, it was defined as the bridging callus formation on both the anterior‐posterior and lateral views13. Fracture nonunion was defined as an absence in the progression of healing for more than 6–12 weeks in a fracture which was not radiographically healed. Fracture malunion was defined as healing of the fracture with <80° or >99° of the proximal medial tibial angle. Pain was assessed using a visual analogue scale and subsequently scored from one to ten, with ten being the most severe pain. The Rasmussen score system was used to evaluate function, and the SF‐36 questionnaire was used as a measure of general health outcome. These scores were assessed one year after operation14. Based on the various scores, the overall result was graded as excellent, good, fair, or poor. Wound complications included the following: (i) wound dehiscence: induced by hematoma formation, not fully healed skin and subcutaneous tissues, which should be treated by surgical dressings within 10 days of suture removal; (ii) superficial wound infection: infection of skin and subcutaneous tissues, generally occurring within 1 month after surgery, represented by locally red, hot, swollen, painful, or tender incision, purulent discharges in the superficial wound, and bacterial growth in cultured discharges around the incision; (iii) deep wound infection: clinically manifested by red, hot, swollen, painful, or tender incision, exudation, and positive bacterial cultures in the discharges around the incision. After additional surgical exploration, infection was confirmed to be present in the deep layer of deep fascia; (iv) wound necrosis: a variety of wound complications may also occur simultaneously. For instance, if a patient developed wound necrosis, wound dehiscence and infection would often occur as well. The most severe complications were extreme wound complications such as first infection, secondary wound necrosis, and wound dehiscence.
The data for the continuous variables were presented as means and ranges, whereas for the categorical variables, the data were presented as counts and percentages. Differences in proportions such as the presence of sex, fracture type, cause of injury, loss of reduction, and failed fixation were compared with the results of the Fisher exact test. Continuous variables were analyzed using the Student t test for data (such as age and surgical timing) with two levels of the nominal variable and analysis of variance when three or more levels were present for that variable.
Results
General Data
A total of 112 patients with complex tibial plateau fractures were treated by the same team of orthopedic surgeons in the study hospital during the study period, and follow‐ups were performed for at least one year after surgery (with an average of 36.5 months, and a range of 26–110 months, Figs 1, 2). No significant differences were found among the five surgical procedure methods in terms of age, sex, surgical timing, fracture type, and cause of injury for the patients (all P values > 0.05, Table 1).
Figure 1.

A 69‐year‐old man who had sustained a type V tibial plateau fracture caused by a motorcycle accident was treated with open reduction and internal fixation with one plate via anterolateral incision. (a) Preoperative coronal CT scan showed medial and lateral plateau fractures, including significant lateral plateau collapse. (b) Postoperative X‐ray film showed anatomical reduction and effective internal fixation in situ for tibial plateau fracture and the smooth articular surface. (c) The wound healed without wound dehiscence or necrosis. (d) One year after operation, bone healing and effective internal fixation in situ and the smooth articular surface were observed.
Figure 2.
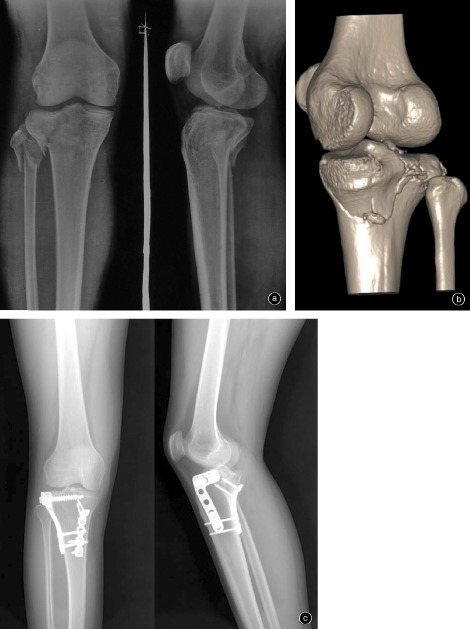
A 24‐year‐old man who had sustained a type V tibial plateau fracture caused by a motorcycle accident was treated with open reduction and internal fixation with dual plating via a combination of anterior and posterior approaches. (a) Preoperative anteroposterior and lateral views of a fracture‐dislocation of the knee. (b) Preoperative CT and 3D reconstruction showed a large posteromedial fragment. (c) One year later, X‐ray showed bone union with the smooth articular surface.
Table 1.
General data of the five groups
| Groups | Cases | Sex | Age | Surgical timing | Fracture type | Cause of injury | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | F | (mean ± s.d., years) | (mean ± s.d., d) | V | VI | Road‐traffic accident | Fall from height | Crushed by heavy object | ||
| Group 1 | 26 | 15 | 11 | 38.3 ± 12.7 | 4.3 ± 2.3 | 16 | 10 | 20 | 4 | 2 |
| Group 2 | 27 | 16 | 11 | 36.0 ± 9.1 | 5.7 ± 2.3 | 12 | 15 | 20 | 4 | 3 |
| Group 3 | 30 | 18 | 12 | 33.4 ± 9.5 | 6.0 ± 4.9 | 13 | 17 | 21 | 6 | 3 |
| Group 4 | 6 | 4 | 2 | 40.5 ± 7.8 | 5.0 ± 1.4 | 4 | 2 | 4 | 1 | 1 |
| Group 5 | 23 | 13 | 10 | 39.5 ± 9.9 | 5.0 ± 2.2 | 13 | 10 | 15 | 3 | 5 |
| Statistical value | 0.24 | 4.32 | 1.12 | 3.17 | 3.07 | |||||
| P value | 0.99 | 0.36 | 0.35 | 0.53 | 0.93 | |||||
Group 1: Open reduction and internal fixation with one plating via anterolateral incision; Group 2: Open reduction and internal fixation with dual plating via anterolateral and posteromedial incisions; Group 3: Open reduction and internal fixation with dual plating via single midline incision; Group 4: Open reduction and internal fixation with dual plating via combined anterior and posterior approaches; Group 5: Close reduction/via a minimal incision with hybrid external fixation.
Surgical Timing Associated with Wound Complications
No differences were found among the five surgical timing groups in terms of wound dehiscence and deep wound infection at the end of the follow‐up period. However, significant differences were found between the 3–5 day group (6.7%) and 5–8 day group (0%) in terms of wound necrosis; between the 4 hour <3 day group (16.7%) and 5–8 day group (0%) in terms of superficial wound infection (P less than 0.05); and among the <4 hour group (20.0%), 4 hour <3 day group (41.6%), 3–5 day group (33.3%) and 5–8 day group (2.5%) in terms of overall wound complication rate (P < 0.05, Table 2).
Table 2.
Comparison of wound complications in different surgical timing (cases [%])
| Surgical timing | Wound dehiscence | Wound necrosis | Superficial wound infection | Deep wound infection | Overall complication rate |
|---|---|---|---|---|---|
| <4 h (10 cases) | 1 (10.0) | 1 (10.0) | 0 (0) | 0 (0) | 2 (20.0) |
| 4 h–3 d (12 cases) | 2 (8.3) | 1 (8.3) | 2 (16.7) | 0 (0) | 5 (41.6) |
| 3–5 d (15 cases) | 2 (6.7) | 1 (6.7) | 1 (6.7) | 1 (6.7) | 5 (33.3) |
| 5–8 d (40 cases) | 1 (2.5) | 0 (0) | 0 (0) | 0 (0) | 1 (2.5) |
| >8 d (12 cases) | 1 (8.3) | 0 (0) | 1 (8.3) | 0 (0) | 2 (16.7) |
| Statistical value | 3.56 | 4.77 | 9.18 | 4.99 | 14.13 |
| P value | 0.47 | 0.31 | 0.06 | 0.29 | 0.01 |
Surgical Procedure Options Associated with Wound Complications
No differences were found among the five surgical procedure methods in terms of wound dehiscence, wound necrosis, superficial wound or deep wound infection at the end of the follow‐up period (all P values > 0.5). However, significant differences were found among Groups 2 (22.2%), 3 (16.7%), 4 (16.7%) and 5 (0%) in terms of overall wound complication rate (P < 0.05, Table 3).
Table 3.
Comparison of wound complications of the five procedure options
| Groups | Cases | wound dehiscence | wound necrosis | superficial wound infection | deep wound infection | Overall complication rate (cases [%]) |
|---|---|---|---|---|---|---|
| Group 1 | 26 | 1 | 1 | 1 | 0 | 3 (11.5) |
| Group 2 | 27 | 3 | 1 | 1 | 1 | 6 (22.2) |
| Group 3 | 30 | 2 | 1 | 2 | 0 | 5 (16.7) |
| Group 4 | 6 | 1 | 0 | 0 | 0 | 1 (16.7) |
| Group 5 | 23 | 0 | 0 | 0 | 0 | 0 (0) |
| Statistical value | 3.27 | 1.73 | 0.83 | 2.52 | 5.78 | |
| P value | 0.51 | 0.79 | 0.93 | 0.64 | 0.22 |
Surgical Procedure Options Associated Clinical Effect
No significant differences were observed among the five surgical procedure methods in terms of imperfect reduction. Anatomical reduction was obtained for 90/112 fractures, with satisfactory reduction (slight loss of reduction: <3 mm) for 16 patients, and imperfect reduction (secondary loss of reduction: >3 mm) for six patients. However, significant differences were seen among Groups 2, 3, and 5 in terms of loss of reduction and intraoperative blood loss at the end of the follow‐up period (P < 0.05). Significant differences also were seen between Groups 1, 2, and 3 in terms of failed fixation at the end of the follow‐up period (P < 0.05), as well as between Groups 3 and 5. Significant differences were also found among Groups 2 (92.6%), 3 (93.3%), and 5 (69.6%) in terms of the good and excellent rates of joint function (P < 0.05). Finally, significant differences were also found among Groups 2 (85.5 ± 2.9), 3 (86.2 ± 3.2), 4 (87.3 ± 2.7) and 5 (72.6 ± 6.3) (P < 0.05) in terms of SF‐36 (Table 4).
Table 4.
Comparison of clinical effects of the five procedure options
| Groups | Cases | Blood loss (mean ± s.d., ml) | Imperfect reduction (cases) | Loss of reduction (cases) | Failed fixation [cases (%]) | Good and excellent rate of joint function (cases [%]) | SF‐36 (mean ± s.d.) |
|---|---|---|---|---|---|---|---|
| Group 1 | 26 | 265.7 ± 125.0 | 2 | 5 | 6 (23.1)†, ‡ | 20 (76.9) | 75.8 ± 5.6 |
| Group 2 | 27 | 373.7 ± 137.3* | 0 | 1 | 1 (3.7) | 25 (92.6) | 85.5 ± 2.9* |
| Group 3 | 30 | 308.4 ± 120.5† | 1 | 1 | 1 (3.3) | 28 (93.3) | 86.2 ± 3.2* |
| Group 4 | 6 | 461.7 ± 90.4*, ‡ | 0 | 0 | 0 (0) | 6 (100) | 87.3 ± 2.7* |
| Group 5 | 23 | 95.6 ± 31.6*, †, § | 3 | 6†, ‡ | 5 (21.7)‡ | 16 (69.6)†, ‡ | 72.6 ± 6.3*, †, ‡, § |
| Statistical value | 18.32 | 5.07 | 10.61 | 10.07 | 9.45 | 44.16 | |
| P value | 0.00 | 0.28 | 0.03 | 0.04 | 0.05 | 0.00 |
*Comparison with Group 1, P < 0.05; †Comparison with Group 2, P < 0.05; ‡Comparison with Group 3, P < 0.05; §Comparison with Group 4, P < 0.05.
Discussion
High‐energy complex tibial plateau fractures are severe injuries, and may result in considerable morbidity. Recommendations regarding optimal surgical timing cannot be concluded from the results of current studies. It has previously been clearly stated that high‐energy complex tibial plateau fractures must be surgically treated on a delayed basis15, 16, and currently there is an increasing level of awareness concerning wound complications associated with high‐energy complex tibial plateau fractures. Complications associated with definitive open reduction and internal fixation have led most surgeons to adopt a suitable surgical timing to treat severe injuries. Benirschke et al. stated that immediate internal fixation is warranted to protect the soft tissues from further damage17. However, it is not possible to complete imaging examinations in time. Furthermore, this method is not able to provide a satisfactory preoperative plan without consummate imaging examinations (such as CT or MRI); therefore the authors do not recommend emergency operation for a closed high‐energy complex fracture of the tibial plateau. Although no significant differences were found in the wound dehiscence between the <4 hour and 5–8 day groups, the wound dehiscence rate for these two groups was quite high (10.0%). Emergency operation should only be taken in case of vascular or compartment syndrome injury. The authors do not recommend rather late surgical timing (>8 days), as earlier timing may decrease the overall wound complication rate at the end of the follow‐up period (16.7%). The authors recommend that the open reduction and internal fixation should be taken in 5–8 days after injury when the soft tissue swelling subsides, as this timing may decrease wound complications (such as the wound dehiscence, necrosis, and infection rate).
The radiologic results showed that the reduction was excellent for two‐incision methods (e.g. anterolateral or combined anterior and posterior) performed immediately after operation. Furthermore, the height of the plateau was maintained at the grade of excellent, and the loss of reduction one year after operation was 3.7% for Group 2, and 3.3% for Group 3. The study results indicate that dual plating via anterolateral and posteromedial incisions, single midline incision or combined anterior and posterior approaches provides a significantly greater reduction in displacement for complex tibial plateau fractures, in comparison to other surgical procedures. A single incision via anterolateral is commonly used18. However, for some patients it is difficult to gain adequate exposure, especially for the internal fixation of the bicondylar tibial plateau or posterior fragments. Therefore some researchers have recommended two‐incision methods4, such as anterolateral and posteromedial or combined anterior and posterior11. Theoretically, two‐incision approaches enable the surgeon to sufficiently visualize and reduce tibial condyles and apply dual plates if desired, avoiding soft tissue complications associated with anterior midline exposure. However, if the knee joint cavity requires exploration, single midline incision may be selected. The advantages of knee anterior midline incision are that it enables the surgeon to sufficiently visualize the bicondylar tibial plateau and the joint cavity, as well as the menisci and cruciate ligaments, with no direct exposure of the internal fixator below the incision. Its main disadvantage is the unsatisfactory exposure of posterior fragments.
This study provides a clinical effect assessment of five surgical procedures which may be used to stabilize high‐energy complex tibial plateau fractures. The study results suggest that the use of dual plating facilitates the surgical stabilization of complex tibial plateau fracture patterns (P < 0.05). Horwitz et al. demonstrated that lateral non‐locked plating alone was significantly less stable than a dual plating design19. However, stable fixation without compromising the soft‐tissue envelope is often difficult. Internal fixation via open reduction, despite the advantages of direct sufficient visualization and stable reduction of the articular surface, also presents large disadvantages, including skin or soft‐tissue necrosis caused by surgery being performed on an already damaged soft tissue envelope, as well as a high rate of infection, which may compromise the final result. Berkson and Egol recommended that complex tibial plateau fractures with severe soft tissue injury should be treated with closed reduction and stabilization with external fixation during the initial treatment16, 20. Comparing external to internal fixation, Mahadeva et al. concluded that hybrid external fixation possesses theoretical advantages in terms of soft tissue protection21. The Hybrid external fixator was applied for patients with complicated extensive soft tissue avulsion, blisters around the knee joint or ischemic necrosis, very high infection risk or severe underlying diseases, or intolerance to anesthesia. The authors of this study obtained rates of 16/23 (69.6%) good/excellent, and 30.4% fair/poor. The SF‐36 of these groups was significantly lower than that of other groups (P < 0.05) in type V and VI fracture series treated by hybrid external fixation. Catagni et al. reported excellent and good results in 30 (50.85%) and 27 (45.76%) patients22. Katsenis et al. presented excellent or good final clinical results in 36 patients (76%)23. The present study shows that hybrid external fixation may be a suitable alternative for the fixation of high‐energy complex tibia plateau fractures, avoiding the risk of skin or soft‐tissue necrosis caused by open reduction with internal fixations. Despite the use of posteromedial buttress plating, currently solitary lateral locked plating has become increasingly popular for application in the treatment of bicondylar tibial plateau fractures24.
The fundamental principles that must be followed by surgeons are as follows: (i) restore the smooth articular surface and stable anatomical structure; (ii) correct the rotation and angular deformity of the fracture, taking note to avoid varus25; (iii) maintain the original height and length; (iv) stable internal fixation and early mobilization; (v) repair the ligaments, meniscus, blood vessels, nerves in a timely manner; (vi) Create the necessary conditions for postoperative early painless functional exercise, and minimize muscle and periosteal damage; and (vii) CT scans were obtained for further investigation in order to identify the size and location of articular fragments26. MRI may show the pathological changes of bone contusion occurring in the knee, and accurately determine injuries in the ligaments around the joint and soft tissues27.
There are a number of limitations involved with this study. These include the retrospective nature of the review, the high percentage of patients who could not be contacted for follow‐up (10.4%), and the relatively small number of patients in Group 4 (dual plating via combined anterior and posterior approaches). In addition, the number of patients treated with single locked implants was very small and could not be compared with the other surgical procedure methods.
Acknowledgments
The authors would like to thank Yang Liang, BMS, the 98th Hospital of PLA, for his assistance with statistical analysis of the data.
Disclosure: Nanjing Military Region Foundation for Science and Innovation Program (No. 11MA009).
References
- 1. Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res, 1979, 138: 94–104. [PubMed] [Google Scholar]
- 2. Greiner P, Magnussen RA, Lustig S, Demey G, Neyret P, Servien E. Computed tomography evaluation of the femoral and tibial attachments of the posterior cruciate ligament in vitro. Knee Surg Sports Traumatol Arthrosc, 2011, 19: 1876–1883. [DOI] [PubMed] [Google Scholar]
- 3. Mills WJ, Nork SE. Open reduction and internal fixation of high‐energy tibial plateau fractures. Orthop Clin North Am, 2002, 33: 177–198. [DOI] [PubMed] [Google Scholar]
- 4. Yu Z, Zheng L, Zhang Y, Li J, Ma B. Functional and radiological evaluations of high‐energy tibial plateau fractures treated with double‐buttress plate fixation. Eur J Med Res, 2009, 14: 200–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Biggi F, Di Fabio S, D'Antimo C, Trevisani S. Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury, 2010, 41: 1178–1182. [DOI] [PubMed] [Google Scholar]
- 6. Yoo BJ, Beingessner DM, Barei DP. Stabilization of the posteromedial fragment in bicondylar tibial plateau fractures: a mechanical comparison of locking and nonlocking single and dual plating methods. J Trauma, 2010, 69: 148–155. [DOI] [PubMed] [Google Scholar]
- 7. Zhang Y, Fan DG, Ma BA, Sun SG. Treatment of complicated tibial plateau fractures with dual plating via a 2‐incision technique. Orthopedics, 2012, 35: e359–e364. [DOI] [PubMed] [Google Scholar]
- 8. El‐Alfy B, Othman A, Mansour E. Indirect reduction and hybrid external fixation in management of comminuted tibial plateau fractures. Acta Orthop Belg, 2011, 77: 349–354. [PubMed] [Google Scholar]
- 9. Zura RD, Adams SB Jr, Jeray KJ, et al Timing of definitive fixation of severe tibial plateau fractures with compartment syndrome does not have an effect on the rate of infection. J Trauma, 2010, 69: 1523–1526. [DOI] [PubMed] [Google Scholar]
- 10. Koval KJ, Helfet DL. Tibial plateau fractures: evaluation and treatment. J Am Acad Orthop Surg, 1995, 3: 86–94. [DOI] [PubMed] [Google Scholar]
- 11. Georgiadis GM. Combined anterior and posterior approaches for complex tibial plateau fractures. J Bone Joint Surg Br, 1994, 76: 285–289. [PubMed] [Google Scholar]
- 12. Ariffin HM, Mahdi NM, Rhani SA, Baharudin A, Shukur MH. Modified hybrid fixator for high‐energy Schatzker V and VI tibial plateau fractures. Strategies Trauma Limb Reconstr, 2011, 6: 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu CC. Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch Orthop Trauma Surg, 2006, 126: 82–87. [DOI] [PubMed] [Google Scholar]
- 14. Rasmussen PS. Tibial condylar fractures: impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am, 1973, 55: 1331–1350. [PubMed] [Google Scholar]
- 15. Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high‐energy bicondylar tibial plateau fractures utilizing a two‐incision technique. J Orthop Trauma, 2004, 18: 649–657. [DOI] [PubMed] [Google Scholar]
- 16. Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high‐energy proximal tibia fractures (OTA types 41): the results of a prospective, standardized protocol. J Orthop Trauma, 2005, 19: 448–455. [DOI] [PubMed] [Google Scholar]
- 17. Benirschke SK, Agnew SG, Mayo KA, Santoro VM, Henley MB. Immediate internal fixation of open, complex tibial plateau fractures: treatment by a standard protocol. J Orthop Trauma, 1992, 6: 78–86. [PubMed] [Google Scholar]
- 18. Femino JE, Vaseenon T. The direct lateral approach to the distal tibia and fibula: a single incision technique for distal tibial and pilon fractures. Iowa Orthop J, 2009, 29: 143–148. [PMC free article] [PubMed] [Google Scholar]
- 19. Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma, 1999, 13: 545–549. [DOI] [PubMed] [Google Scholar]
- 20. Berkson EM, Virkus WW. High‐energy tibial plateau fractures. J Am Acad Orthop Surg, 2006, 14: 20–31. [DOI] [PubMed] [Google Scholar]
- 21. Mahadeva D, Costa ML, Gaffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: a systematic review of the literature. Arch Orthop Trauma Surg, 2008, 128: 1169–1175. [DOI] [PubMed] [Google Scholar]
- 22. Catagni MA, Ottaviani G, Maggioni M. Treatment strategies for complex fractures of the tibial plateau with external circular fixation and limited internal fixation. J Trauma, 2007, 63: 1043–1053. [DOI] [PubMed] [Google Scholar]
- 23. Katsenis D, Athanasiou V, Megas P, Tyllianakis M, Lambiris E. Minimal internal fixation augmented by small wire transfixion frames for high‐energy tibial plateau fractures. J Orthop Trauma, 2005, 19: 241–248. [DOI] [PubMed] [Google Scholar]
- 24. Nikolaou VS, Tan HB, Haidukewych G, Kanakaris N, Giannoudis PV. Proximal tibial fractures: early experience using polyaxial locking‐plate technology. Int Orthop, 2011, 35: 1215–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee JA, Papadakis SA, Moon C, Zalavras CG. Tibial plateau fractures treated with the less invasive stabilisation system. Int Orthop, 2007, 31: 415–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mustonen AO, Koivikko MP, Kiuru MJ, Salo J, Koskinen SK. Postoperative MDCT of tibial plateau fractures. AJR Am J Roentgenol, 2009, 193: 1354–1360. [DOI] [PubMed] [Google Scholar]
- 27. Ye DC, Qiu QD, Yin JC. MRI diagnosis of bone contusion on the knee and its clinical significance. Zhongguo Gu Shang, 2010, 23: 427–429. [PubMed] [Google Scholar]


