This cluster-randomized clinical trial assesses whether a targeted electronic health record alert achieves similar advances to multicomponent interventions and safely reduces unnecessary monitoring.
Key Points
Question
Can an electronic health record (EHR) alert, targeted to the right physician at the right time, safely reduce unnecessary inpatient cardiac monitoring?
Findings
In a cluster-randomized clinical trial of 1066 hospitalizations, teams on a general medicine service received an EHR alert when a patient’s telemetry order exceeded the duration recommended for the monitoring indication. In response to the alert, physicians chose to discontinue monitoring 62% of the time, resulting in a reduction of monitoring duration per hospitalization with no increase in potential adverse events.
Meaning
A targeted EHR alert appears to safely reduce unnecessary cardiac monitoring without the need for human resources devoted to monitoring use or physician feedback.
Abstract
Importance
Physicians frequently use cardiac monitoring, or telemetry, beyond the duration recommended by published practice standards, resulting in “alarm fatigue” and excess cost. Prior studies have demonstrated an association between multicomponent quality improvement interventions and safe reduction of telemetry duration.
Objective
To determine if a single-component intervention, a targeted electronic health record (EHR) alert, could achieve similar gains to multicomponent interventions and safely reduce unnecessary monitoring.
Design, Setting, and Participants
This cluster-randomized clinical trial was conducted between November 2016 and May 2017 on the general medicine service of the Division of Hospital Medicine at the University of California, San Francisco Medical Center and included physicians of 12 inpatient medical teams (6 intervention, 6 control).
Interventions
The EHR alert was randomized to half of the teams on the general medicine service. The alert displayed during daytime hours when physicians attempted to place an order for patients not in the intensive care unit whose telemetry order duration exceeded the recommended duration for a given indication.
Main Outcomes and Measures
The primary outcome was telemetry monitoring hours per hospitalization, which was measured using time-stamped orders data from the EHR database. Physician responses to the alert were collected using EHR reporting tools. The potential adverse outcomes of rapid-response calls and medical emergency events were measured by counting the notes documenting these events in the EHR.
Results
Of the 1021 patients included in this study, in the intervention arm, there was a mean (SD) age of 64.5 (18.9) and 215 (45%) were women; in the control arm, there was a mean (SD) age of 63.8 (19.1) and 249 (46%) were women. The 12 teams were stratified to 8 house-staff teams and 4 hospitalist teams, with 499 hospitalizations analyzed in the intervention arm and 567 hospitalizations analyzed in the control arm. The alert prompted a significant reduction in telemetry monitoring duration (−8.7 hours per hospitalization; 95% CI, −14.1 to −3.5 hours; P = .001) with no significant change in rapid-response calls or medical emergency events. The most common physician response to the alert was to discontinue telemetry monitoring (62% of 200 alerts).
Conclusions and Relevance
A targeted EHR alert can safely and successfully reduce cardiac monitoring by prompting discontinuation when appropriate. This single-component electronic intervention is less resource intensive than typical multicomponent interventions that include human resources.
Trial Registration
ClinicalTrials.gov identifier: NCT02529176
Introduction
Cardiac monitoring, or telemetry, can provide early detection of sudden cardiac death, identification and monitoring of arrhythmias, and evaluation of ST segment and QT interval changes.1 Despite American Heart Association (AHA) indication–specific best practice standards, telemetry is overused, both in initiation and in duration of monitoring.1,2,3 This results in excess cost and “alarm fatigue,” a phenomenon of desensitization to alarms when they are frequently false or irrelevant.4,5,6 The American Board of Internal Medicine Foundation recommends a protocol to promote early telemetry discontinuation.7
Modifications to the electronic health record (EHR) can play an important role in attempting to reduce inappropriate telemetry use; however, studies analyzing this effect have been methodologically limited.8,9,10,11 Multicomponent interventions obscure the effect of a single EHR modification; single-armed studies are difficult to interpret without a control; and a lack of evaluation for potential adverse outcomes reduces confidence in the safety of the intervention. Thus, the safety and efficacy of a targeted EHR intervention is not known.
Herein, we report the results of a cluster-randomized clinical trial using AHA practice standard–concordant alerts in the EHR to safely reduce telemetry duration.
Methods
Setting and Participants
This study was conducted on the general medicine service of the Division of Hospital Medicine at the University of California, San Francisco (UCSF) Medical Center (Supplement 1). The general medicine service includes patients in the intensive care unit (ICU), but they were excluded from the study population because monitoring is often mandatory in patients with critical illness. This study also excluded patients who did not receive cardiac monitoring during their hospitalization. The study received institutional review board approval from the UCSF Human Research Protection Program (15-17527), waiving patient written informed consent. The trial is registered at ClinicalTrials.gov as NCT02529176.
Appropriate indications and duration for telemetry orders were already incorporated in the EHR (Hyperspace; Epic Systems Corporation) when this study was designed (Table 1). These were developed 5 years ago using 2 main sources: 2004 AHA practice standards12 and expert opinion from UCSF faculty in hospital medicine, cardiology, cardiac surgery, and neurology.13
Table 1. Telemetry Monitoring Indications and Recommended Duration.
| Duration | Indication/Event |
|---|---|
| 24 h | Critical electrolyte abnormality |
| Severe sepsis | |
| 48 h | Rule out myocardial infarction |
| Syncope | |
| Other (long QT syndrome, myocarditis, drug overdose, etc) | |
| 72 h | After cardiac arrest |
| Acute coronary syndrome or after percutaneous coronary intervention | |
| Acute pulmonary embolism | |
| Indefinitely | After stroke to rule out arrhythmia |
| Cardiothoracic or vascular surgery | |
| Pulmonary hypertension or advanced heart failure | |
| Arrhythmia as primary reason for hospitalization |
Randomization
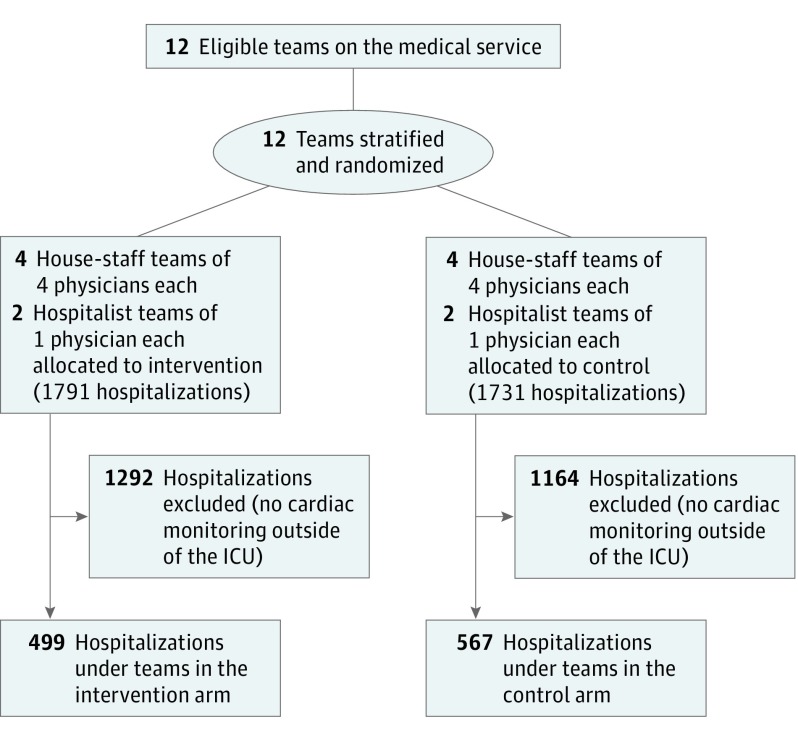
The general medicine service consists of 8 house-staff teams (designated A-H) and 4 attending, hospitalist-only teams (numbered 1-4). Patients admitted to the house-staff teams are assigned in the order they present to the hospital and can therefore be viewed as randomly distributed. A similar circumstance exists for the hospitalist-only teams. Patients on the house-staff teams are more similar to one another with regard to medical conditions and level of acuity than they are to patients on the hospitalist-only teams. Thus, to balance patient characteristics in the 2 arms of our study, we grouped teams A through D and 1 and 2 into 1 group and teams E through H and 3 and 4 into another group. Then we randomly assigned the former group to the intervention arm and the latter group to the control arm (Figure). Because patients cluster within teams, our intervention is cluster randomized.
Figure. Participant Enrollment Flowchart.
ICU indicates intensive care unit.
Intervention and Control Descriptions
We configured an EHR clinical decision support alert to trigger for patients admitted to the intervention teams (A-D and 1 and 2) in which a window would pop up on a physician’s computer screen when the following criteria were met: (1) the physician was logged into the EHR in their role on the general medicine service; (2) the patient was not in an ICU setting; (3) the patient had an active telemetry order; (4) the duration of the telemetry order had surpassed its indication-based recommended duration; (5) the current time was between 7 am and 5 pm; and (6) the physician was engaged in order entry. The time restriction was intended to maximize exposure of the alert to primary, rather than cross-covering, physicians. Similarly, the restriction to trigger during order entry was intended to minimize alert display to consultants.
The alert prompted physicians to write a telemetry discontinuation order, write a new telemetry order, or dismiss the alert. The study did not include an educational or audit and feedback campaign, although the goal of telemetry duration reduction had been communicated through prior initiatives.13 For teams in the control arm, no alerts pertaining to telemetry were displayed to physicians.
Outcomes
The primary outcome was telemetry hours per patient encounter. We measured the primary outcome via time stamps on telemetry orders in the EHR database.
We assessed potential adverse outcomes associated with discontinuation of telemetry via our secondary outcomes of rapid-response calls and medical emergency events. These measures were recorded in the EHR via templated notes that we acquired from the EHR database. This method of counting rapid responses and emergency events was verified to be accurate and complete by manual medical record review.
Power Calculation and Analysis
We performed a power calculation prior to the trial using data from a past telemetry-reduction campaign to estimate an anticipated 20% reduction in telemetry hours, from 50 hours (our baseline) to 40 hours.13 Assuming 75% of patients in the present study would have usable data, and assuming 204 discharges from the general medicine service each month, we calculated that this trial would need 6 months to accrue the necessary 1022 patients.
We used a team-level intervention but a patient-level primary outcome (telemetry hours), so we used generalized estimating equations with the Wald test and robust standard errors to analyze the difference in the mean of our primary outcome. We assessed the difference in the proportion of hospitalizations with a rapid-response event using the z test and the difference in the proportion of hospitalizations with a medical emergency event using Fisher exact test.
Results
Teams caring for patients in the intervention arm received the alert, when conditions were met to trigger it, from November 2016 to May 2017. There were 1066 hospitalizations that included non-ICU cardiac monitoring during the study period: 499 in the intervention arm and 567 in the control arm. These hospitalizations represented 1021 unique patients for which there was no significant difference in age, sex, race, marital status, primary language, or insurance status (Table 2).
Table 2. Characteristics of Patients in Intervention and Control Arms.
| Patient Characteristics | Intervention (n = 478) |
Control (n = 543) | P Value |
|---|---|---|---|
| Age, mean (SD), y | 64.5 (18.9) | 63.8 (19.1) | .54 |
| Women, No. (%) | 215 (45) | 249 (46) | .83 |
| Race, No. (%) | .74 | ||
| Asian | 113 (24) | 124 (23) | |
| Black or African American | 71 (15) | 94 (17) | |
| White | 219 (46) | 240 (44) | |
| Other/unknown | 75 (16) | 81 (15) | |
| Marital status, No. (%) | .57 | ||
| Married | 166 (35) | 205 (38) | |
| Single | 185 (39) | 209 (38) | |
| Widowed | 67 (14) | 74 (14) | |
| Other | 60 (13) | 55 (10) | |
| Primary language, No. (%) | .45 | ||
| English | 380 (79) | 427 (79) | |
| Chinese | 53 (11) | 53 (10) | |
| Russian | 14 (3) | 14 (3) | |
| Other | 31 (6) | 49 (9) | |
| Primary insurance status, No. (%) | .90 | ||
| Medicare | 279 (58) | 309 (57) | |
| Medicaid | 111 (23) | 137 (25) | |
| Commercial | 79 (17) | 88 (16) | |
| Other | 9 (2) | 9 (2) |
Two hundred clinical decision support alerts were generated in the intervention arm. The mean telemetry hours per hospitalization was 50.0 in the control group and 41.3 in the intervention group, which was a reduction of 17% (Table 3). Accounting for clustering at the team level, the intervention effect was −8.7 hours (95% CI, −14.1 to −3.5 hours; P = .001) per hospitalization. We estimated that the cumulative reduction in telemetry for the intervention arm relative to the control was approximately 8.7 × 499 = 4341 hours, or 181 days.
Table 3. Primary Outcome and Potential Adverse Outcomes.
| Per Hospitalization | Intervention (n = 499) | Control (n = 567) | Effect Size (95% CI) | P Value |
|---|---|---|---|---|
| Telemetry hours, mean (SD) | 41.3 (40.2) | 50.0 (51.7) | −8.7 (−14.1 to −3.5) | .001 |
| Rapid-response call, No. (%) | 30 (6.0) | 32 (5.6) | 0.004 (−0.01 to 0.01) | .90 |
| Medical emergency event, No. (%) | 2 (0.4) | 2 (0.4) | 0.0005 (−0.5 to 0.9) | > .99a |
Fisher exact test.
There was no significant difference in proportion of hospitalizations with a rapid-response call or medical emergency event between the arms of the trial (Table 3).
Physician responses to the telemetry alert are presented in Table 4. Of 200 alerts, 62% (n = 124) of the time physicians discontinued the current telemetry order; 21% (n = 41) of the time they reordered telemetry; and 7% (n = 14) of the time they dismissed the alert without taking action. In the remaining 11% (n = 21) of cases, physicians acknowledged the alert but chose to maintain their current orders.
Table 4. Physician Responses to Expired Telemetry Alert.
| Action | Alerts (n = 200), No. (%) |
|---|---|
| Dismissed the alert with no action taken | 14 (7) |
| Continued the current telemetry order | 21 (11) |
| Discontinued current order and did not reorder | 124 (62) |
| Reordered telemetry with a new indication | 41 (21) |
Discussion
In this cluster-randomized trial at a large academic medical center, a targeted alert prompting physicians to discontinue telemetry when the recommended duration had expired resulted in a significant reduction in hours of monitoring. This reduction was achieved without a concomitant educational or audit and feedback campaign, without human resources dedicated to monitoring telemetry use, and without an increase in adverse events as measured by rapid-response or medical emergency activation.
A prior study with a before-after design by Dressler and colleagues8 demonstrated that changes to EHR orders and nurse assessments could safely reduce telemetry duration hours by 43%. Another before-after study by Edholm and colleagues10 included a modification of the EHR that caused telemetry orders to expire after a duration determined by the order’s indication. The multicomponent intervention group in that study demonstrated a reduction of 65%.
The present study extends the prior studies in important ways. First, we demonstrate that an EHR alert targeted to the right clinicians (primary team physicians), at the right time (daylight hours, while the physician is writing orders), with the right clinical context (telemetry exceeds recommended duration) can succeed without an associated educational or audit and feedback campaign. Second, we demonstrated this in a randomized trial that minimized the effects of secular trends or unmeasured confounders. Finally, we were able to demonstrate that when physicians were shown these targeted alerts, their majority behavior was to act in a practice standard–concordant way.
The reduction in telemetry hours in this study is notably smaller than in the study by Dressler and colleagues8 and smaller than the multicomponent intervention group in the study by Edholm and colleagues.10 However, both of these studies included interventions outside of a pure EHR modification. The 17% reduction in the present study is close to the reduction seen in the nonhospitalist, EHR-only intervention group in the study by Edholm and colleagues.10 It therefore appears that the effect size from making changes only to the EHR is smaller than what can be expected from including other elements typical of quality improvement interventions, such as educational and audit and feedback, but the EHR-only intervention is less costly and more scalable.
We chose to randomize the intervention by team, rather than patient or individual physician. Randomization by patient would have resulted in a given physician seeing the alert for some of the patients and not for others. Seeing alerts for some patients could prompt the physician to change their monitoring practices on all patients, including those randomized to control. This creates a “bleed over” of the effect of the intervention into the control arm, which would reduce the power of the intervention. Randomization by individual physician would result in some members of a team receiving the alert while others do not. This could lead to a bleed-over effect within the team because physicians in the intervention arm would likely tell their teammates in the control arm about the alerts they see.
With respect to team-level randomization, it is possible that, during the study period, a physician could have worked on an intervention team and then a control team, thus resulting in a bleed over of their telemetry reduction practice. However, this scenario is unlikely. First, both residents and attending physicians at UCSF Medical Center perform a variety of clinical services at a variety of locations, so being scheduled for repeated ward shifts in the same location in a 6-month period is uncommon. Second, to create interteam bleed over, the physician would have to coincidentally work first on an intervention team and then later on a control team because the other 3 possibilities, such as control to intervention or intervention to intervention, would have created no opportunity for the physician to bring their changed practice to a control team. Finally, the EHR alert would have to create such a lasting impression on the physician’s practice that it continued to have an effect weeks or months later when the physician was back on service and no longer seeing the alert.
Limitations
There are several important limitations to this study. First, it is a single-center study at a large academic medical center, so the findings may not generalize to other settings. Second, the indication-specific recommendations for duration of telemetry were in part informed by local expert opinion and are more permissive than national practice standards.1 For example, we included indications beyond these standards, such as acute pulmonary embolism and severe sepsis. Finally, the preintervention mean telemetry hours at the UCSF Medical Center general medicine service was already lower than the baseline in prior studies,8,9 which may have limited the effect size of this intervention.
Conclusions
This study demonstrates a safe reduction in unnecessary cardiac monitoring using a simple, targeted EHR intervention without the need for intensive human resources or nonenduring educational campaigns.
Study Application (Version 1.0)
Data Sharing Statement
References
- 1.Sandau KE, Funk M, Auerbach A, et al. ; American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Cardiovascular Disease in the Young . Update to practice standards for electrocardiographic monitoring in hospital settings: a scientific statement from the American Heart Association. Circulation. 2017;136(19):e273-e344. doi: 10.1161/CIR.0000000000000527 [DOI] [PubMed] [Google Scholar]
- 2.Svec D, Ahuja N, Evans KH, et al. Hospitalist intervention for appropriate use of telemetry reduces length of stay and cost. J Hosp Med. 2015;10(9):627-632. doi: 10.1002/jhm.2411 [DOI] [PubMed] [Google Scholar]
- 3.Najafi N, Auerbach A. Use and outcomes of telemetry monitoring on a medicine service. Arch Intern Med. 2012;172(17):1349-1350. doi: 10.1001/archinternmed.2012.3163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atzema C, Schull MJ, Borgundvaag B, Slaughter GR, Lee CK. ALARMED: adverse events in low-risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department: a pilot study. Am J Emerg Med. 2006;24(1):62-67. doi: 10.1016/j.ajem.2005.05.015 [DOI] [PubMed] [Google Scholar]
- 5.Graham KC, Cvach M. Monitor alarm fatigue: standardizing use of physiological monitors and decreasing nuisance alarms. Am J Crit Care. 2010;19(1):28-34. doi: 10.4037/ajcc2010651 [DOI] [PubMed] [Google Scholar]
- 6.Benjamin EM, Klugman RA, Luckmann R, Fairchild DG, Abookire SA. Impact of cardiac telemetry on patient safety and cost. Am J Manag Care. 2013;19(6):e225-e232. [PubMed] [Google Scholar]
- 7.Bulger J, Nickel W, Messler J, et al. Choosing wisely in adult hospital medicine: five opportunities for improved healthcare value. J Hosp Med. 2013;8(9):486-492. doi: 10.1002/jhm.2063 [DOI] [PubMed] [Google Scholar]
- 8.Dressler R, Dryer MM, Coletti C, Mahoney D, Doorey AJ. Altering overuse of cardiac telemetry in non-intensive care unit settings by hardwiring the use of American Heart Association guidelines. JAMA Intern Med. 2014;174(11):1852-1854. doi: 10.1001/jamainternmed.2014.4491 [DOI] [PubMed] [Google Scholar]
- 9.Rizvi W, Munguti CM, Mehta J, Kallail KJ, Youngman D, Antonios S. Reducing over-utilization of cardiac telemetry with pop-ups in an electronic medical record system. Cureus. 2017;9(5):e1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edholm K, Kukhareva P, Ciarkowski C, et al. Decrease in inpatient telemetry utilization through a system-wide electronic health record change and a multifaceted hospitalist intervention. J Hosp Med. 2018;13(8):531-536. [DOI] [PubMed] [Google Scholar]
- 11.Boggan JC, Navar-Boggan AM, Patel V, Schulteis RD, Simel DL. Reductions in telemetry order duration do not reduce telemetry utilization. J Hosp Med. 2014;9(12):795-796. doi: 10.1002/jhm.2264 [DOI] [PubMed] [Google Scholar]
- 12.Drew BJ, Califf RM, Funk M, et al. ; American Heart Association; Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young . Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation. 2004;110(17):2721-2746. doi: 10.1161/01.CIR.0000145144.56673.59 [DOI] [PubMed] [Google Scholar]
- 13.Najafi N, Bowman C, Diaz M, Zapata J, Mourad M. A resident-led campaign to reduce telemetry waste on a teaching service [abstract]. https://www.shmabstracts.com/abstract/a-residentled-campaign-to-reduce-telemetry-waste-on-a-teaching-service/. Accessed October 24, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Study Application (Version 1.0)
Data Sharing Statement