Key Points
Question
Is trauma of hospitalization, which is characterized by patient-reported disturbance in sleep, mobility, nutrition, and mood, associated with a greater risk of 30-day readmission or emergency department visit after hospital discharge?
Findings
In this cohort study of 207 medical inpatients, disturbances in sleep, mobility, nutrition, and mood were common, and most participants reported experiencing a disturbance in multiple domains. These disturbances were associated with greater risk of readmission or emergency department visit.
Meaning
Trauma of hospitalization was common among medical inpatients and may be associated with a greater risk of unplanned return to the hospital or emergency department within 30 days of discharge.
Abstract
Importance
Trauma of hospitalization refers to the depersonalizing and stressful experience of a hospital admission and is hypothesized to increase the risk of readmission after discharge.
Objectives
To characterize the trauma of hospitalization by measuring patient-reported disturbances in sleep, mobility, nutrition, and mood among medical inpatients, and to examine the association between these disturbances and the risk of unplanned return to hospital after discharge.
Design, Setting, and Participants
This prospective cohort study enrolled participants between September 1, 2016, and September 1, 2017, at 2 academic hospitals in Toronto, Canada. Participants were adults admitted to the internal medicine ward for more than 48 hours. Participants were interviewed before discharge using a standardized questionnaire to assess sleep, mobility, nutrition, and mood. Responses for each domain were dichotomized as disturbance or no disturbance. Disturbance in 3 or 4 domains (the upper tertile) was considered high trauma of hospitalization, and disturbance in 0 to 2 domains (the lower 2 tertiles) was considered low trauma.
Main Outcome and Measures
The primary outcome was readmission or emergency department visit within 30 days of discharge. The association between trauma of hospitalization and the primary outcome was examined using logistic regression, adjusted for age; sex; length of stay; Charlson Comorbidity Index Score; Laboratory-Based Acute Physiology Score; and baseline disturbances in sleep, mobility, nutrition, and mood.
Results
A total of 207 patients participated, of whom 82 (39.6%) were women and 125 (60.4%) were men, with a mean (SD) age of 60.3 (16.8) years. Among the 207 participants, 75 (36.2%) reported sleep disturbance, 162 (78.3%) reported mobility disturbance, 114 (55.1%) reported nutrition disturbance, and 48 (23.2%) reported mood disturbance. Nearly all participants (192 [92.8%]) described a disturbance in at least 1 domain, and 61 participants (29.5%) had high trauma exposure. A statistically significant 15.8% greater absolute risk of readmission or emergency department visit was found in participants with high trauma (37.7%; 95% CI, 25.9%-51.1%) compared with those with low trauma (21.9%; 95% CI, 15.7%-29.7%), which remained statistically significant after adjusting for baseline characteristics (adjusted odds ratio, 2.52; 95% CI, 1.24-5.17; P = .01) and propensity score matching (odds ratio, 2.47; 95% CI, 1.11-5.73; P = .03).
Conclusions and Relevance
Disturbances in sleep, mobility, nutrition, and mood were common in medical inpatients; such trauma of hospitalization may be associated with a greater risk of 30-day readmission or emergency department visit after hospital discharge.
This cohort study examines patient reports and implications of difficulties with sleep, movement, eating, and anxiety or depression during hospitalization for at least 48 hours and the association with subsequent readmission or emergency department visits.
Introduction
Improving patient experience1 and reducing readmissions2 are priorities for health care practitioners, patients, and policymakers. A growing body of evidence suggests that patient experience in hospital may be associated with posthospital outcomes and the risk of readmission.3,4,5 Krumholz6 hypothesized that the stress of hospitalization results in physiologic disturbances that leave patients vulnerable to developing new or recurrent illnesses after discharge. Krumholz6 termed this condition posthospital syndrome and suggested that it increased the probability of unplanned return to hospital and readmission.7 Detsky and Krumholz8 later identified aspects of inpatient care that contribute to the posthospital syndrome, including sleep deprivation, immobility, nutritional disturbance, and anxiety and stress induced by the unpredictable and depersonalizing hospital environment. Detsky and Krumholz8 called the cumulative effect of these disturbances the trauma of hospitalization.
Evidence supports the hypothesis of trauma of hospitalization. Sleep disturbances are common in hospitalized patients because of acute illness, reduced physical activity, medication adverse effects, light, and noise.9,10,11,12,13 Mobility declines in hospital, and this change is associated with a loss of independence, persistent functional decline, and increased readmission.14,15,16,17 Poor nutritional status is associated with adverse clinical outcomes and worsens in hospital for reasons that include poor meal experience, increased catabolism, and physical barriers to accessing food.18 Anxiety is common among intensive care unit survivors but is not well described in medical inpatients.19 Depression may develop after hospitalization for common medical conditions such as pneumonia and heart failure.20,21 Although its components have been studied individually to varying degrees, the trauma of hospitalization has not been examined as a coherent framework.
In this prospective study, we measured the frequency of patient-reported disturbances in 4 domains of the trauma of hospitalization: sleep, mobility, nutrition, and mood. We examined whether these disturbances were associated with a greater risk of 30-day readmission to hospital or emergency department (ED) visit after hospital discharge.
Methods
Study Setting and Participants
This study was conducted at 2 academic hospitals in Toronto, Ontario, Canada: St Michael’s Hospital and Toronto Western Hospital, University Health Network. Both institutions are public hospitals that provide tertiary and quaternary care to a large and diverse urban population with universal health insurance coverage for physician and hospital services. The internal medicine ward consists of 70 beds at St Michael’s Hospital and 88 beds at Toronto Western Hospital. Study participants were recruited among patients admitted to the internal medicine ward at both institutions between September 1, 2016, and September 1, 2017. The study was approved by the Research Ethics Board of both St Michael’s Hospital and University Health Network. All participants provided written informed consent.
A trained research assistant worked with physicians and nurses to identify patients who had a plan for discharge home on the same or next day. Eligible study participants were adult medical inpatients who had been admitted for at least 48 hours, to ensure that participants had sufficient exposure to the experience of hospitalization. We excluded patients who were unable to answer questions because of limited English proficiency or cognitive impairment. Cognition was assessed using the Short Portable Mental Status Questionnaire,22 and patients with moderate-to-severe cognitive impairment (≥5 errors) were excluded from the study. In addition, we excluded patients who had been admitted to the intensive care unit because of the greater physiologic disturbances associated with critical care. We excluded patients who were discharged to a facility other than their home (such as a rehabilitation facility; patients discharged to a nursing home were included if they lived in that home prior to hospitalization); were terminally ill, with limited life expectancy; or were anticipated to be unable to complete the 30-day follow-up survey for any reason. The study sample size was determined by the number of participants who could be recruited over a 12-month period at the 2 institutions.
Exposures
The research assistant administered a survey at the participant’s bedside on either the day of discharge or the day prior to the planned discharge. The survey assessed 4 domains using standardized questionnaires: sleep, mobility, nutrition, and mood. Sleep was assessed using questions adapted from the Patient Reported Outcomes Measurement Information System (PROMIS) Short Form v1.0–Sleep Disturbance 4a.23,24 The context of the questions and text of some questions were modified to refer to the time in hospital or the time before hospitalization. Mobility was evaluated using a single item adapted from the Eastern Cooperative Oncology Group Scale of Performance Status screen and similar to the Saltin-Grimby Physical Activity Level Scale.25,26 Disturbances in nutrition were assessed using questions taken from the Patient Mealtime and Nutrition Care Survey.27 A single question from the Euro-Qol Five Dimensions Questionnaire was used to characterize depression and anxiety in hospital.28 These questionnaires were selected to provide a simple and pragmatic assessment of the 4 domains of interest. Participants were asked to consider the entirety of their hospital stay when responding to the survey questions. The resultant survey consisted of 10 questions (Table 1).
Table 1. In-Hospital Disturbance Survey.
| Domain | Source | Question | Response Choice | Disturbance Categorizationa |
|---|---|---|---|---|
| Sleep | Questions adapted from PROMIS Short Form v1.0–Sleep Disturbance 4a | In hospital, my sleep quality has been… | Very poor (5), poor (4), fair (3), good (2), very good (1) | Considered disturbance if score ≥13; cutoff reflects an overall score of less than average |
| In hospital, my sleep has been refreshing | Not at all (5), a little bit (4), somewhat (3), quite a bit (2), very much (1) | |||
| In hospital, I have had a problem with my sleep | Not at all (1), a little bit (2), somewhat (3), quite a bit (4), very much (5) | |||
| In hospital, I have had difficulty falling asleep | Not at all (1), a little bit (2), somewhat (3), quite a bit (4), very much (5) | |||
| Mobility | 1 Item adapted from the Eastern Cooperative Oncology Group Scale of Performance Status and similar to the Saltin-Grimby Physical Activity Level Scale | During my hospitalization, I was… |
|
Considered disturbance if confined to bed or chair for >50% of waking hours or totally confined to bed or chair |
| Nutrition | Patient Mealtime and Nutrition Care Survey | When I was eating, I was disturbed | Yes (1), no (2) | Considered disturbance if total score <8, suggesting that meals were disturbed or missed in the hospital |
| My meal times were interrupted by staff | Yes (1), no (2) | |||
| I missed meals because I was not available when they were served | Yes (1), no (2) | |||
| I missed meals because I had to avoid food for tests | Yes (1), no (2) | |||
| Mood (anxiety or depression) | 1 item from Euro-Qol Five Dimensions Questionnaire | Now, I am… |
|
Considered disturbance if moderately to extremely anxious or depressed |
These were prespecified cutoffs for disturbance according to clinical judgment.
Responses for each domain were dichotomized into disturbance or no disturbance. Prior to analysis, the cutoffs for each domain were prespecified on the basis of clinical judgment: Sleep disturbance was considered to be an overall score of less-than-fair sleep, mobility disturbance was considered to be confined to a bed or chair for more than 50% of waking hours, nutrition disturbance was present if meals were disturbed or missed, and mood disturbance consisted of moderate-to-extreme anxiety or depression (Table 1). We decided a priori to divide participants into tertiles according to the number of domains in which they experienced a disturbance. We considered those in the upper tertile to have experienced high trauma of hospitalization and hypothesized that these participants would be at greater risk of unplanned return to the hospital after discharge compared with participants in the lower 2 tertiles.
Outcomes
The primary outcome was readmission or ED visit to the same hospital within 30 days of discharge. Data on readmission and ED visit were collected through medical record review in the 2 hospitals by trained abstractors (including S. R.) who were blinded to the categorization of trauma of hospitalization. We performed medical record review and made telephone calls to participants to determine whether those who did not experience the primary outcome were alive at 30 days after discharge.
Covariates
Information on participants’ age, sex, and race/ethnicity were obtained through our predischarge survey. Hospital administrative data were used to measure length of stay; compute the Charlson Comorbidity Index (scored 0, 1, and ≥2)29; and determine the primary discharge diagnoses according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, codes. We calculated the Laboratory-Based Acute Physiology Score (LAPS; theoretical score range: 0-256 [although rarely reaching more than 100], with higher scores indicating a greater risk of in-hospital mortality), a validated measure of illness severity, using laboratory data extracted from electronic medical records.30,31 To estimate baseline disturbances in the domains of trauma of hospitalization, we asked participants to recall their sleep, mobility, and mood prior to hospitalization as well as their nutritional status over the past 6 months using PROMIS Short Form v1.0–Sleep Disturbance 4a, the Euro-Qol Five Dimensions Questionnaire, and the Canadian Nutrition Screening Tool (eTable 1 in the Supplement).32
Statistical Analysis
Disturbances in sleep, nutrition, mobility, and mood were reported using descriptive statistics, and the association between each individual domain and the primary outcome was tested using χ2 analysis. Unadjusted and adjusted logistic regression models were fit to examine the association between trauma exposure and the primary outcome. In the first adjusted model, we controlled for participant age, sex, Charlson Comorbidity Index, hospital length of stay, and LAPS. In the second adjusted model, we controlled for self-reported baseline disturbances in sleep, mobility, nutrition, and mood as separate covariates. These models were fit separately, because the sample size limited the number of variables that could be included in each model. Next, we performed a propensity score–matched analysis, in which each participant with high trauma exposure was matched to a participant with low trauma exposure. Propensity scores were derived from logistic regression models predicting the probability of high trauma by all baseline covariates. In addition, we examined the primary outcome in participants stratified by age (younger or older than 65 years) to explore whether the trauma of hospitalization differed by age subgroup. We also examined the relationship among hospital length of stay, trauma exposure, and the primary outcome by categorizing the study population into quartiles according to length of stay. Finally, to explore the implication of our inclusion and exclusion criteria, we compared the characteristics of the study population with all general internal medicine admissions over a 1-year period at the participating hospitals, using the data collected in a previous study.33
Participants who did not experience the primary outcome and could not be determined to be alive at 30 days were considered to be at risk of unrecorded death. If death is associated with trauma of hospitalization, then unrecorded deaths could potentially bias our findings. We used the Fisher exact test to assess the balance in the risk of unrecorded deaths across high and low trauma of hospitalization groups. Analyses were completed using R, version 3.3.2 (R Foundation for Statistical Computing).
Results
A total of 207 participants were enrolled in the study from September 1, 2016, to September 1, 2017 (eFigure in the Supplement). Of the 207 participants, 82 (39.6%) were women and 125 (60.4%) were men, with a mean (SD) age of 60.3 (16.8) years (Table 2); 110 (53.1%) of these patients were younger than 65 years. The mean (SD) hospital length of stay was 8.0 (6.7) days. The 5 most common primary discharge diagnoses were lower limb cellulitis, congestive heart failure, chronic obstructive pulmonary disease, gastrointestinal hemorrhage, and pneumonia. Complete follow-up data were available on 197 participants (95.2%), who either experienced the primary outcome or were alive at 30 days. The remaining 10 participants (4.8%) did not experience the primary outcome and could not be confirmed to be alive 30 days after discharge. The proportion of participants at risk of unrecorded death did not differ statistically significantly between high trauma and low trauma groups (n = 4 [5.5%] vs 6 [4.6%]; P = .74).
Table 2. Participant Characteristics.
| Characteristic | No. (%) | Standardized Differencec | P Valuec | ||
|---|---|---|---|---|---|
| Overall (N = 207) | Low Trauma (n = 146) | High Trauma (n = 61)b | |||
| Age, mean (SD), y | 60.3 (16.8) | 60.1 (17.6) | 60.6 (14.8) | 0.03 | .85 |
| Female sex | 82 (39.6) | 59 (40.4) | 23 (37.7) | 0.06 | .84 |
| Length of stay, mean (SD), d | 8.0 (6.7) | 7.5 (6.3) | 9.3 (7.5) | 0.26 | .08 |
| White race/ethnicity | 148 (71.8) | 98 (67.1) | 50 (82.0) | 0.36 | .09 |
| Charlson Comorbidity Index score | NA | NA | NA | 0.22 | .33 |
| 0 | 101 (48.8) | 75 (51.4) | 26 (42.6) | NA | NA |
| 1 | 42 (20.3) | 26 (17.8) | 16 (26.2) | ||
| 2+ | 64 (30.9) | 42 (30.8) | 19 (31.1) | ||
| LAPS, mean (SD)a | 14.6 (14.4) | 13.8 (13.7) | 16.3 (16.0) | 0.17 | .26 |
| Baseline | |||||
| Sleep disturbance | 99 (47.8) | 65 (44.5) | 34 (55.7) | 0.23 | .19 |
| Mobility disturbance | 122 (58.9) | 86 (58.9) | 36 (59.0) | <0.01 | >.99 |
| Nutrition disturbance | 68 (32.9) | 41 (28.1) | 27 (44.3) | 0.34 | .04 |
| Mood disturbance | 84 (40.6) | 57 (39.0) | 27 (44.3) | 0.11 | .59 |
Abbreviations: LAPS, Laboratory-Based Acute Physiology Score; NA, not applicable.
LAPS theoretical score range: 0-256 (although rarely reaching more than 100), with higher scores indicating a greater risk of in-hospital mortality.
High trauma was defined as reporting disturbances in 3 or 4 domains, and low trauma was reporting disturbances in 2 or fewer domains.
Comparison of low trauma with high trauma groups.
Disturbance in Sleep, Mobility, Nutrition, and Mood
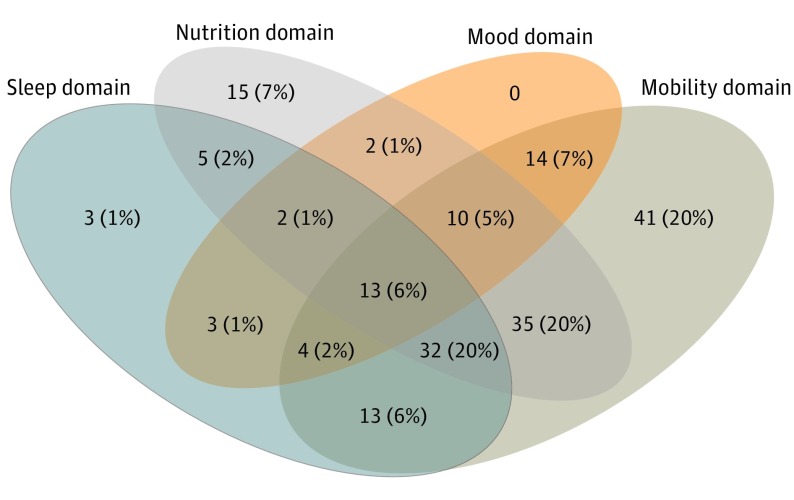
In our cohort, 75 participants (36.2%; 95% CI, 29.8%-43.2%) reported sleep disturbance, 162 (78.3%; 95% CI, 71.9%-83.6%) reported mobility disturbance, 114 (55.1%; 95% CI, 48.3%-61.7%) reported nutrition disturbance, and 48 (23.2%; 95% CI, 17.7%-29.7%) reported mood disturbance (Table 3). Nearly all participants (192 [92.8%]) described a disturbance in at least 1 domain. Only 15 participants (7.3%; 95% CI, 4.3%-11.9%) reported no disturbances, and 133 (64.3%; 95% CI, 57.3%-70.7%) reported disturbances in more than 1 domain (Figure). Participants were categorized into tertiles according to the number of domains with a disturbance. The upper tertile consisted of 61 participants (29.5%; 95% CI, 23.5%-36.3%) who reported disturbances in 3 or 4 domains, and these participants were considered to have experienced high trauma of hospitalization. The remainder were considered to have low trauma of hospitalization.
Table 3. Disturbances and 30-Day Readmission or Emergency Department Visit.
| Domain | Participants With Disturbance, No. (%) | Readmission, No./Total (%)a | Absolute Difference, % | Readmission Difference P Valuea | |
|---|---|---|---|---|---|
| Disturbance | No Disturbance | ||||
| Sleep | 75 (36.2) | 22/75 (29.3) | 33/132 (25.0) | 4.3 | .61 |
| Mobility | 162 (78.3) | 46/162 (28.4) | 9/45 (20.0) | 8.4 | .35 |
| Nutrition | 114 (55.1) | 34/114 (29.8) | 21/93 (22.6) | 7.2 | .31 |
| Mood | 48 (23.2) | 19/48 (39.6) | 36/159 (22.6) | 17.0 | .03 |
30-Day readmission or emergency department visit.
Figure. Overlapping Disturbances in Sleep, Mobility, Nutrition, and Mood Among Medical Inpatients.
This figure illustrates the number of participants who reported disturbances at the intersections of each trauma-of-hospitalization domain. For example, 13 participants (6%) were affected by disturbances in all 4 domains.
For each individual domain, the primary outcome occurred more commonly among participants who experienced disturbance than in those who had no disturbance, but the differences were statistically significant only for mood (Table 3).
Trauma of Hospitalization and Primary Outcome
Overall, 55 participants (26.6%; 95% CI, 20.8%-33.2%) experienced the primary outcome, 30 (14.5%; 95% CI, 10.1%-20.2%) were readmitted, and 25 (12.1%; 95% CI, 8.1%-17.5%) had an ED visit but were not readmitted. The primary outcome occurred in 15.8% more participants with high trauma (37.7%; 95% CI, 25.9%-51.1%) than with low trauma (21.9%; 95% CI, 15.7%-29.7%). High trauma exposure was associated with statistically significantly greater occurrence of the primary outcome in the unadjusted analysis (odds ratio [OR], 2.16; 95% CI, 1.12-4.13; P = .02); in the analysis adjusted for participant characteristics (adjusted OR, 2.52; 95% CI, 1.24-5.17; P = .01); and in the analysis adjusted for baseline disturbance in sleep, mobility, nutrition, and mood (adjusted OR, 2.19; 95% CI, 1.12-4.30; P = .02) (Table 4).
Table 4. Analyses of Association Between Trauma of Hospitalization and Primary Outcome.
| Variable | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Univariate modela | ||
| High trauma | 2.16 (1.12-4.13) | .02 |
| Multivariable I modela | ||
| High trauma | 2.52 (1.24-5.17) | .01 |
| Age | 0.97 (0.95-0.99) | .01 |
| Female sex | 2.02 (1.01-4.09) | .05 |
| Length of stay | 0.95 (0.89-1.01) | .16 |
| Charlson Comorbidity Index score = 1b | 1.03 (0.37-2.74) | .95 |
| Charlson Comorbidity Index score = ≥2 b | 3.96 (1.77-9.28) | .001 |
| LAPS | 1.02 (0.99-1.04) | .10 |
| Multivariable II modela | ||
| High trauma | 2.19 (1.12-4.30) | .02 |
| Baseline | ||
| Sleep | 1.05 (0.54-2.04) | .87 |
| Mobility | 1.97 (1.00-4.02) | .06 |
| Nutrition | 0.93 (0.46-1.82) | .83 |
| Mood | 1.24 (0.64-2.38) | .53 |
| Propensity score matching | ||
| High trauma | 2.47 (1.11-5.73) | .03 |
Abbreviation: LAPS, Laboratory-Based Acute Physiology Score.
Univariate and multivariable logistic regression models assessing the effect of high trauma of hospitalization on 30-d readmission or emergency department visit. High trauma was defined as experiencing disturbances in 3 or 4 domains.
Charlson Comorbidity Index was modeled as a categorical variable with 3 groups, and the reference category was Charlson score of 0.
Propensity score matching resulted in groups that were well balanced (standardized difference, ≤0.1) on all baseline characteristics except the LAPS (eTable 2 in the Supplement), which was higher among participants with low trauma. In the propensity-matched cohort, high trauma exposure was associated with statistically significantly greater occurrence of the primary outcome (37.7% vs 19.7%; OR, 2.47; 95% CI, 1.11-5.73; P = .03) (Table 4).
The primary outcome was more frequent among participants with high trauma exposure compared with participants with low trauma exposure in both age groups (≥65 years and <65 years). However, these differences were not statistically significant (eTable 3 in the Supplement).
High trauma was more common among patients with longer hospital length of stay, exhibiting a dose-response relationship. High trauma affected 20 (41.7%) of 48 participants (95% CI, 27.9%-56.7%) in the highest length-of-stay quartile compared with 15 (22.4%) of 67 participants (95% CI, 13.5%-34.5%) in the lowest length-of-stay quartile (eTable 4 in the Supplement). However, the primary outcome was not more frequent among participants with longer length of stay.
The study population, compared with all general internal medicine admissions over a 1-year period (N = 7862; eTable 5 in the Supplement), was younger (mean [SD] age, 60.3 [16.8] years vs 67.3 [18.7] years), included fewer women (82 [39.6%] vs 3755 [47.8%]), had fewer patients with high Charlson Comorbidity Index score (64 [30.9%] vs 3333 [42.4%]), had shorter length of stay (mean [SD] days, 8.0 [6.7] days vs 8.7 [17.4] days), and had lower LAPS (mean score, 14.6 [14.4] points vs 18.6 [15.9] points).
Discussion
In this prospective cohort study at 2 large urban hospitals, the trauma of hospitalization was common among medical inpatients, with most patients (64.3%) reporting disturbances in multiple domains of sleep, mobility, nutrition, and mood. Participants who experienced disturbance in 3 or 4 domains experienced a 15.8% greater absolute risk of 30-day readmission or ED visit. Making causal inferences is not possible in this observational study, but the association between the trauma of hospitalization and risk of unplanned return to hospital remained strong after propensity score matching and controlling for baseline characteristics, illness severity, and baseline disturbances in the trauma domains.
This study contributes to 2 growing areas of research: the relationship between patient experience and clinical outcomes as well as the associations between hospitalization and health status. Hospitals with higher patient ratings have been shown to have lower mortality and readmission rates.4,5,34 We extend this literature by describing important patient-level differences in 4 domains of hospital experience that were strongly associated with the risk of unplanned return to hospital. We used a simple 10-item questionnaire to assess sleep, nutrition, mobility, and mood, which are domains not found in most standardized patient experience surveys, such as the Hospital Consumer Assessment of Healthcare Providers and Systems.35 To our knowledge, this present study is the first to examine the association between the trauma of hospitalization and 30-day readmission and ED visit. Our findings support the hypothesis of the trauma of hospitalization, which offers a plausible mechanism to explain how negative patient experiences may be correlated with physiologic disturbances and subsequent adverse clinical outcomes.
The associations of hospitalization with health status are becoming increasingly apparent. Hospital-related disturbances in mobility and nutrition have been associated with a range of poor outcomes, including increased risk of readmission. Sleep disturbance has been reported among medical inpatients,36 although its correlation to health outcomes is not well described. Mood disturbance is more common among hospitalized patients than the general population,37,38,39,40 but the relationships among hospitalization, mood, and clinical outcomes are not well studied. We found similar rates of disturbance in mobility,15 sleep,10,36 nutrition,18 and mood19,39 as in previous reports from a wide range of hospitals and countries, strengthening our confidence in the generalizability of our findings.
This study’s findings add to the existing literature on the relationships among hospitalization, health status, and clinical outcomes. First, we measured multiple domains simultaneously to better characterize the implications of hospitalization. The most prevalent disturbances were mobility (78.3%) and nutrition (55.1%), with 43.5% of participants reporting disturbance in both domains, making this the most common pair of disturbances. The primary outcome appeared more common among patients who reported a disturbance in each individual domain, although the association was the largest and statistically significant only for mood. This finding suggests that individual disturbances may be associated with the risk of readmission or ED visit but that the cumulative effects of these disturbances are more pronounced. Second, we identified a dose-response relationship between hospital length of stay and rates of high trauma, further supporting the hypothesis that exposure to the hospital environment is a factor in the observed disturbances in multiple domains. Third, we addressed issues of confounding through the study’s design and multiple statistical analyses. Patients with more severe illness or greater baseline disability may be more likely to experience disturbance in sleep, mobility, nutrition, and mood and to be readmitted after discharge. Therefore, we excluded patients admitted to the intensive care unit or with baseline cognitive impairment. We used granular data from patient questionnaires, electronic health records, and hospital administrative records to control for factors associated with risk of readmission, such as age, comorbidity level, length of stay, and illness severity measured by the LAPS.30,31 We controlled for self-reported baseline disturbances in the 4 reported domains. Our findings were consistent across these analyses, including propensity score matching, which resulted in well-balanced groups. These results suggest a true association between the trauma of hospitalization and unplanned return to the hospital. Fourth, we included adults of all ages. Much of the existing literature in this area is focused on older adults, and less is known about younger populations. Approximately half (53%) of the participants in this study were younger than 65 years, and our findings suggest that hospitalization affects the health status of both younger and older adults. Finally, we linked in-hospital disturbances with postdischarge outcomes, highlighting the importance of further research into the implications of hospitalization for health status.
Limitations
This study has several limitations. First, it was conducted at 2 academic health centers and recruited patients on the day of or the day before their discharge. Because of this narrow recruitment window and because discharge is often unpredictable, we enrolled far fewer patients than the total number of internal medicine admissions, which was expected. Because we included only patients discharged to their home and excluded those with intensive care unit admission, cognitive impairment, and limited life expectancy, the study participants were younger, had fewer comorbidities, less severe illness, and shorter length of stay, compared with the broader internal medicine ward population. Thus, patients excluded from this study may have been at greater risk of the trauma of hospitalization, and we may have underestimated its prevalence. Nevertheless, our findings are consistent with existing literature in this area and our study population was diverse. Nearly 30% of participants identified as non-white, reflecting the multiethnic Toronto population, and patients were hospitalized for a wide range of conditions, consistent with the heterogeneity of general internal medicine.41 Thus, we believe these findings are likely to be generalizable to other hospitals. Second, although we conducted the study in a setting with universal hospital and physician insurance, we believe socioeconomic status and home supports may be potential confounders in our analysis, representing an opportunity for future research.
Third, we used a simple 10-question survey to measure the trauma of hospitalization, which included questions adapted from instruments that have not been validated in this population. The strength of our approach is that we drew on existing instruments to generate a pragmatic set of questions that could feasibly be administered to medical inpatients and we used prespecified cutoffs to dichotomize responses according to clinical judgment. Further research is required to validate the cutoffs we used to identify disturbances and to replicate our findings using these questions. Fourth, our measurement of baseline disturbances in the trauma domains was based on participant recall, which could have been biased by their present health status. If this were the case, we would expect more self-reported baseline disturbance among participants with high trauma, and this would bias our findings toward the null. Rates of baseline disturbance were high in our study, and tracing the trajectory of these disturbances before, during, and after hospitalization is an opportunity for future research. Fifth, because of sample size limitations, we were unable to adjust for all potential covariates simultaneously. However, our results were consistent across multiple sensitivity analyses and after propensity score matching, strengthening our confidence in the findings. Finally, we did not capture readmissions and ED visits to other hospitals. In the region around Toronto, Canada, where this study was conducted, 18% of readmissions occur in a hospital different from the site of the index admission.42 As a result, we have likely slightly underestimated the readmission rate. Choosing ED visit or readmission to the index hospital as the primary outcome allowed for high rates of follow-up (>95%) and was unlikely to bias the observed differences between those with and those without high trauma exposure.
Conclusions
These findings suggest that multiple physiologic and emotional domains are disrupted in hospital, raising the question of whether a multimodal intervention could be effective in reducing the trauma of hospitalization, which should be an important goal in promoting person-centered care. Furthermore, these findings suggest that such efforts may decrease readmissions. Multidimensional models of care, such as Enhanced Recovery After Surgery programs43 and Acute Care of the Elderly units,44 may offer lessons for improving care for all medical inpatients; however, neither of these models focus comprehensively on patient experience in hospital. Our study highlights an opportunity to develop and evaluate a multimodal intervention to reduce the trauma of hospitalization by improving sleep, mobility, and nutrition as well as minimizing stress from disruptions and surprises.
The trauma of hospitalization, characterized by disturbances in sleep, mobility, nutrition, and mood, was common among medical inpatients and appeared to be associated with a markedly greater risk of 30-day readmission or ED visit. Further study is required to validate these results and to develop and evaluate interventions aimed at reducing the trauma of hospitalization. These findings suggest that aspects of hospital care may hinder rather than help patients recover from illness.
eFigure. Study Flow Diagram
eTable 1. Baseline Disturbance Survey
eTable 2. Participant Characteristics in the Propensity-matched Study Cohort
eTable 3. Trauma of Hospitalization and 30-day Readmission or Emergency Department Visit, Categorized by Age of Participants
eTable 4. Trauma of Hospitalization and 30-day Readmission or Emergency Department Visit, Categorized by Hospital Length-of-Stay
eTable 5. Characteristics of Study Participants and All General Internal Medicine Admissions
eReferences
References
- 1.Tefera L, Lehrman WG, Conway P. Measurement of the patient experience: clarifying facts, myths, and approaches. JAMA. 2016;315(20):2167-2168. doi: 10.1001/jama.2016.1652 [DOI] [PubMed] [Google Scholar]
- 2.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374(16):1543-1551. doi: 10.1056/NEJMsa1513024 [DOI] [PubMed] [Google Scholar]
- 3.Carter J, Ward C, Wexler D, Donelan K. The association between patient experience factors and likelihood of 30-day readmission: a prospective cohort study [published online November 16, 2017]. BMJ Qual Saf. 2018;27(9):683-690. doi: 10.1136/bmjqs-2017-007184 [DOI] [PubMed] [Google Scholar]
- 4.Wang DE, Tsugawa Y, Figueroa JF, Jha AK. Association between the Centers for Medicare and Medicaid Services hospital star rating and patient outcomes. JAMA Intern Med. 2016;176(6):848-850. doi: 10.1001/jamainternmed.2016.0784 [DOI] [PubMed] [Google Scholar]
- 5.Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201-203. doi: 10.1056/NEJMp1211775 [DOI] [PubMed] [Google Scholar]
- 6.Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100-102. doi: 10.1056/NEJMp1212324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldwater DS, Dharmarajan K, McEwan BS, Krumholz HM. Is posthospital syndrome a result of hospitalization-induced allostatic overload [published online May 30, 2018]? J Hosp Med. 2018;13(5). doi: 10.12788/jhm.2986 [DOI] [PubMed] [Google Scholar]
- 8.Detsky AS, Krumholz HM. Reducing the trauma of hospitalization. JAMA. 2014;311(21):2169-2170. doi: 10.1001/jama.2014.3695 [DOI] [PubMed] [Google Scholar]
- 9.Young JS, Bourgeois JA, Hilty DM, Hardin KA. Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473-482. doi: 10.1002/jhm.372 [DOI] [PubMed] [Google Scholar]
- 10.Dobing S, Frolova N, McAlister F, Ringrose J. Sleep quality and factors influencing self-reported sleep duration and quality in the general internal medicine inpatient population. PLoS One. 2016;11(6):e0156735. doi: 10.1371/journal.pone.0156735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. doi: 10.7326/0003-4819-156-12-201208070-00472 [DOI] [PubMed] [Google Scholar]
- 12.Beveridge C, Knutson K, Spampinato L, et al. Daytime physical activity and sleep in hospitalized older adults: association with demographic characteristics and disease severity. J Am Geriatr Soc. 2015;63(7):1391-1400. doi: 10.1111/jgs.13520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wesselius HM, van den Ende ES, Alsma J, et al. ; “Onderzoeks Consortium Acute Geneeskunde” Acute Medicine Research Consortium . Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med. 2018;. 178(9):1201-1208. doi: 10.1001/jamainternmed.2018.2669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150(6):372-378. doi: 10.7326/0003-4819-150-6-200903170-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57(9):1660-1665. doi: 10.1111/j.1532-5415.2009.02393.x [DOI] [PubMed] [Google Scholar]
- 16.Brown CJ, Friedkin RJ, Inouye SK. Prevalence and outcomes of low mobility in hospitalized older patients. J Am Geriatr Soc. 2004;52(8):1263-1270. doi: 10.1111/j.1532-5415.2004.52354.x [DOI] [PubMed] [Google Scholar]
- 17.Brown CJ, Foley KT, Lowman JD Jr, et al. Comparison of posthospitalization function and community mobility in hospital mobility program and usual care patients: a randomized clinical trial. JAMA Intern Med. 2016;176(7):921-927. doi: 10.1001/jamainternmed.2016.1870 [DOI] [PubMed] [Google Scholar]
- 18.Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27(1):5-15. doi: 10.1016/j.clnu.2007.10.007 [DOI] [PubMed] [Google Scholar]
- 19.Nikayin S, Rabiee A, Hashem MD, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2016;43:23-29. doi: 10.1016/j.genhosppsych.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pederson JL, Majumdar SR, Forhan M, Johnson JA, McAlister FA; PROACTIVE Investigators . Current depressive symptoms but not history of depression predict hospital readmission or death after discharge from medical wards: a multisite prospective cohort study. Gen Hosp Psychiatry. 2016;39:80-85. doi: 10.1016/j.genhosppsych.2015.12.001 [DOI] [PubMed] [Google Scholar]
- 21.Pederson JL, Warkentin LM, Majumdar SR, McAlister FA. Depressive symptoms are associated with higher rates of readmission or mortality after medical hospitalization: a systematic review and meta-analysis. J Hosp Med. 2016;11(5):373-380. doi: 10.1002/jhm.2547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433-441. doi: 10.1111/j.1532-5415.1975.tb00927.x [DOI] [PubMed] [Google Scholar]
- 23.Yu L, Buysse DJ, Germain A, et al. Development of short forms from the PROMIS™ sleep disturbance and Sleep-Related Impairment item banks. Behav Sleep Med. 2011;10(1):6-24. doi: 10.1080/15402002.2012.636266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.PROMIS. Adult Sleep Disturbance Profile Short Form. A brief guide to the 4-item PROMIS Short Form v1.0–Sleep Disturbance 4a, the 6-item PROMIS Short Form v1.0–Sleep Disturbance 6a, and the 8-item PROMIS Short Form v1.0–Sleep Disturbance 8a. https://assessmentcenter.net/documents/PROMIS%20Scoring%20SF%20Sleep%20Disturbance%204a,%206a,%208a.pdf. Accessed April 23, 2018.
- 25.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649-655. doi: 10.1097/00000421-198212000-00014 [DOI] [PubMed] [Google Scholar]
- 26.Grimby G, Börjesson M, Jonsdottir IH, Schnohr P, Thelle DS, Saltin B. The “Saltin-Grimby Physical Activity Level Scale” and its application to health research. Scand J Med Sci Sports. 2015;25(4)(suppl 4):119-125. doi: 10.1111/sms.12611 [DOI] [PubMed] [Google Scholar]
- 27.Canadian Malnutrition Task Force. Patient mealtime and nutrition care survey. http://www.nutritioncareincanada.ca/sites/default/uploads/files/Patient-Mealtime-Nutrition-Care-Survey_non-selective-menus_2014.pdf. Accessed April 23, 2018.
- 28.Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337-343. doi: 10.3109/07853890109002087 [DOI] [PubMed] [Google Scholar]
- 29.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676-682. doi: 10.1093/aje/kwq433 [DOI] [PubMed] [Google Scholar]
- 30.van Walraven C, Escobar GJ, Greene JD, Forster AJ. The Kaiser Permanente inpatient risk adjustment methodology was valid in an external patient population. J Clin Epidemiol. 2010;63(7):798-803. doi: 10.1016/j.jclinepi.2009.08.020 [DOI] [PubMed] [Google Scholar]
- 31.Escobar GJ, Greene JD, Scheirer P, Gardner MN, Draper D, Kipnis P. Risk-adjusting hospital inpatient mortality using automated inpatient, outpatient, and laboratory databases. Med Care. 2008;46(3):232-239. doi: 10.1097/MLR.0b013e3181589bb6 [DOI] [PubMed] [Google Scholar]
- 32.Laporte M, Keller HH, Payette H, et al. Validity and reliability of the new Canadian Nutrition Screening Tool in the ‘real-world’ hospital setting. Eur J Clin Nutr. 2015;69(5):558-564. doi: 10.1038/ejcn.2014.270 [DOI] [PubMed] [Google Scholar]
- 33.Verma AA, Guo Y, Kwan JL, et al. Patient characteristics, resource use and outcomes associated with general internal medicine hospital care: the General Medicine Inpatient Initiative (GEMINI) retrospective cohort study. CMAJ Open. 2017;5(4):E842-E849. doi: 10.9778/cmajo.20170097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48. [PubMed] [Google Scholar]
- 35.Centers for Medicare and Medicaid Services HCAHPS: Patients’ perspectives of care survey. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.html. Published 2017. Accessed February 28, 2018.
- 36.Arora VM, Chang KL, Fazal AZ, et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185-2186. doi: 10.1111/j.1532-5415.2011.03644.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arolt V, Driessen M, Dilling H. The Lübeck General Hospital Study, I: prevalence of psychiatric disorders in medical and surgical inpatients. Int J Psychiatry Clin Pract. 1997;1(3):207-216. doi: 10.3109/13651509709024728 [DOI] [PubMed] [Google Scholar]
- 38.Hansen MS, Fink P, Frydenberg M, Oxhøj M, Søndergaard L, Munk-Jørgensen P. Mental disorders among internal medical inpatients: prevalence, detection, and treatment status. J Psychosom Res. 2001;50(4):199-204. doi: 10.1016/S0022-3999(00)00230-0 [DOI] [PubMed] [Google Scholar]
- 39.Martucci M, Balestrieri M, Bisoffi G, et al. Evaluating psychiatric morbidity in a general hospital: a two-phase epidemiological survey. Psychol Med. 1999;29(4):823-832. doi: 10.1017/S0033291799008491 [DOI] [PubMed] [Google Scholar]
- 40.Silverstone PH. Prevalence of psychiatric disorders in medical inpatients. J Nerv Ment Dis. 1996;184(1):43-51. doi: 10.1097/00005053-199601000-00008 [DOI] [PubMed] [Google Scholar]
- 41.Verma AA, Guo Y, Kwan JL, et al. Prevalence and costs of discharge diagnoses in inpatient general internal medicine: a multi-center cross-sectional study [published online July 27, 2018]. J Gen Intern Med. 2018. doi: 10.1007/s11606-018-4591-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Staples JA, Thiruchelvam D, Redelmeier DA. Site of hospital readmission and mortality: a population-based retrospective cohort study. CMAJ Open. 2014;2(2):E77-E85. doi: 10.9778/cmajo.20130053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292-298. doi: 10.1001/jamasurg.2016.4952 [DOI] [PubMed] [Google Scholar]
- 44.Fox MT, Persaud M, Maimets I, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60(12):2237-2245. doi: 10.1111/jgs.12028 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure. Study Flow Diagram
eTable 1. Baseline Disturbance Survey
eTable 2. Participant Characteristics in the Propensity-matched Study Cohort
eTable 3. Trauma of Hospitalization and 30-day Readmission or Emergency Department Visit, Categorized by Age of Participants
eTable 4. Trauma of Hospitalization and 30-day Readmission or Emergency Department Visit, Categorized by Hospital Length-of-Stay
eTable 5. Characteristics of Study Participants and All General Internal Medicine Admissions
eReferences