Abstract
This study uses data from the Optum Clinformatics Data Mart to evaluate trends in outpatient prescription of opioids to persons 18 years or younger in the United States from 2004 to 2017.
Between 1997 and 2012, the rate of hospitalization due to opioid poisonings nearly doubled in US children and adolescents.1 Opioid use early in life is associated with a higher likelihood of opioid misuse in the future.2 Although recent reports suggest a deceleration and potentially a decrease in opioid prescribing in the overall population,3 little is known about contemporary opioid prescribing trends specifically in children and adolescents.
Methods
We evaluated trends in opioid prescriptions dispensed to individuals 18 years or younger between January 1, 2004, and March 31, 2017, in the Optum Clinformatics Data Mart. The database contains administrative pharmacy and medical claims for a large national, commercially insured population across all 50 US states, including approximately 2.5 million individuals 18 years or younger at a given time. The covered population has demographic characteristics similar to the US distribution for sex and age younger than 65 years. The Brigham and Women's Hospital Institutional Review Board waived the need for approval and also waived the need for patient informed consent.
We calculated the proportion of children and adolescents each month for whom an outpatient opioid prescription was dispensed and the proportion with long-term use, defined as 3 or more consecutive months with at least 1 opioid prescription.4 We considered all oral opioid products used for pain, excluding cough suppressants. Individuals with a health care claim associated with a cancer diagnosis code were excluded. We plotted the mean monthly prevalence of any and long-term opioid use in each year, stratified results by specific age ranges (ie, 0-5, 6-10, 11-14, and 15-18 years), and examined the relative proportion of all opioid prescriptions dispensed by individual opioid.
Results
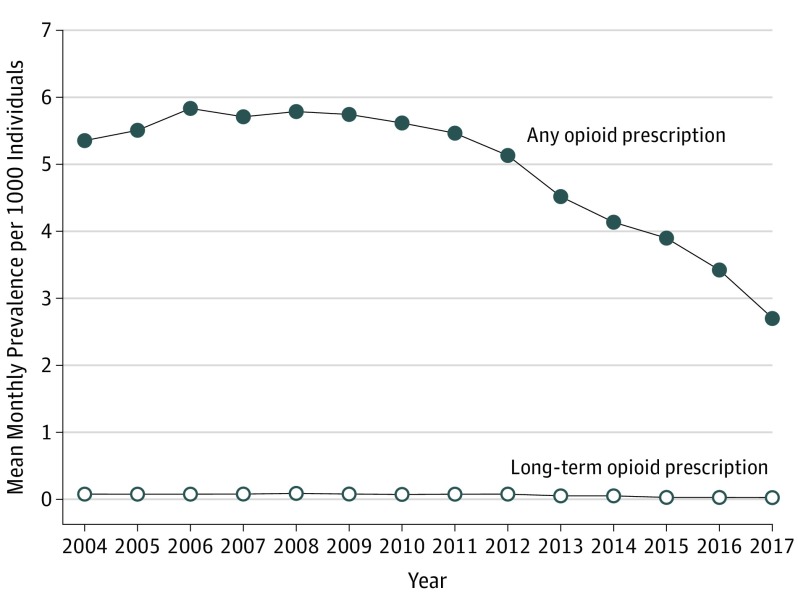
In 2004, a mean (SD) of 5.4 (0.7) of every 1000 children and adolescents received an outpatient opioid prescription in a given month (Figure). This increased by 7% to 5.8 (0.6) of every 1000 children and adolescents between 2006 and 2008 and then dropped to 2.7 (0.3) per 1000 children and adolescents at the beginning of 2017. A similar trend was observed for long-term opioid use. The decrease in any use was driven by a decrease in prescriptions of codeine and hydrocodone bitartrate, which was the most commonly dispensed opioid representing approximately half of all opioid prescriptions dispensed to children and adolescents. The mean (SD) number of hydrocodone prescriptions dispensed decreased from a high of 3.2 (0.5) per 1000 children and adolescents in 2011 to 1.4 (0.2) per 1000 in 2017. Dispensation of oxycodone was stable over time, not increasing after the 2015 US Food and Drug Administration (FDA) approval of extended-release oxycodone for children. Although the FDA did not restrict use of prescription codeine in children until 2017, non–cough suppressant codeine use decreased throughout the study period. Prevalence of both any and long-term opioid use increased with age, but patterns were similar for all ages.
Figure. Trends in Prevalence of Any and Long-term Opioid Prescriptions Dispensed to Children and Adolescents, January 1, 2004, to March 31, 2017.
Long-term use was defined as 3 or more consecutive months with at least 1 opioid prescription.
Discussion
A limitation of the analysis is that we used data from a single large commercial insurance provider, and opioid dispensing rates may differ in other populations and settings. However, the Clinformatics Data Mart includes data from beneficiaries of a large number of health plans that have different benefit structures and that serve geographically diverse populations. We focused on opioid use for pain and therefore excluded cough suppressants. As such, our results do not elucidate any changes potentially associated with the FDA’s restriction on codeine specifically for cough suppression. Our analysis also does not account for other sources of opioid exposure, such as opioids administered in the hospital or prescriptions to family members.
We found that prescription opioids dispensed to children and adolescents in a large commercially insured US population have been steadily decreasing since 2012. These findings are consistent with trends in adults that show a slight decline between 2011 and 20135 and with national trends observed in the overall US population from 2011 through 2015.3 Nevertheless, the frequency of opioid use remains high given the risks associated with these medications in children and adolescents.
References
- 1.Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170(12):1195-1201. doi: 10.1001/jamapediatrics.2016.2154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miech R, Johnston L, O’Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. 2015;136(5):e1169-e1177. doi: 10.1542/peds.2015-1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: changes in opioid prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697-704. doi: 10.15585/mmwr.mm6626a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85-92. doi: 10.7326/0003-4819-152-2-201001190-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dart RC, Severtson SG, Bucher-Bartelson B. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(16):1573-1574. [DOI] [PubMed] [Google Scholar]