Abstract
Objectives: Exchange nailing (EN) for aseptic femoral shaft nonunion is currently a standard orthopaedic treatment modality. However, according to recent studies there is occasionally a high failure rate when EN is used. In the present study, augmentative locked plating and bone graft was used as an alternative method for treating such cases. The purpose of this study was to report the treatment outcomes of selected femoral diaphyseal nonunions that had initially been treated by nailing.
Methods: Thirteen patients with femoral diaphyseal nonunions underwent revision surgery with locked plate and bone graft. The inclusion criteria were: (a) nonisthmic nonunion; (b) atrophic/oligotrophic nonunion. All patients were managed by augmentative locked plating and bone graft.
Results: All patients were followed up for a mean of 1.2 years (range, 1–2 years). After revision surgery all nonunions achieved bony union, the average union time being 7.5 months (range, 6–12 months). No major complications were observed in this case series.
Conclusion: Augmentative locked plating is an effective and simple technique for treatment of femoral diaphyseal nonunion after nailing in selected cases.
Keywords: Bone plates, Bone transplantation, Femoral fractures, Fractures, ununited
Introduction
Due to its superior biomechanical and biological properties, intramedullary nailing of the femur has enjoyed wide spread acceptance in the management of femoral diaphyseal fractures. However, nonunion occasionally occurs secondary to malreduction, inaccurate implant placement and unfavorable fracture pattern 1 , 2 . Revision surgery is then generally indicated because of persistent pain and significant functional disability.
Exchange nailing (EN) for femoral shaft nonunion is known for its excellent rate of fracture healing and is currently a standard orthopaedic procedure 3 . However, a couple of recent studies have argued against its use in all femoral nonunion cases. Banaszkiewicz et al. 4 and Weresh et al. 5 have reported unfavorable results with closed EN, reporting success rates as low as 73% and 58%, respectively. Shroeder et al. demonstrated that atrophic/oligotrophic nonunions are risk factors which correlate significantly with an adverse outcome 3 . Park et al. compared the results of EN and plate augmentation and demonstrated that higher failure rates may occur when EN is used for nonisthmic femoral shaft nonunions 6 . These reports suggest that despite its high success rate, EN alone does not solve all the problems of femoral shaft nonunion. According to recent studies, nonisthmic femoral nonunion and atrophic/oligotrophic nonunion are susceptible to failure when EN is used.
Since March 2006, locked plating augmented with bone graft has been used for the treatment of selected femoral diaphyseal nonunion after failed nailing fixation in our trauma center. All cases were managed by the same senior doctor (the author for correspondence). The purpose of this study is to report the results of this treatment.
Materials and methods
Patients
This retrospective study included thirteen patients with femoral diaphyseal aseptic nonunion after nailing who were treated between March, 2006 and February, 2010. We defined diaphyseal nonunion as the main fracture line being located between the inferior border of the lesser trochanter and upper border of the transepicondylar width of the knee. The inclusion criteria were: (i) nonisthmic nonunion; and (ii) atrophic/oligotrophic nonunion.
Nonunion was defined as a clinically and radiographically unhealed fracture that required additional procedures to achieve union, as determined by the surgeon.
The case series included twelve men and one woman with an average age of 38.9 years (range, 28–55 years). All patients' data are shown in Table 1. All the fractures had initially been treated by nailing. Two had been fixed with a Gamma nail (Howmedica, Allendale, NJ, USA) and one with a retrograde nail. The remaining ten had been stabilized with antegrade interlocking nails with proximal locking into the region of the lesser trochanter. At the time of presentation, the cases had undergone one or two previous operations since the initial injury. The erythrocyte sedation rate and C‐reactive protein concentration of all patients were checked preoperatively to exclude any cases of occult septic nonunion.
Table 1.
Data of patients treated with augmentative locked plating and bone graft
| No. | Age (years) | Sex | Pattern of nonunion | Site | Operation times (hs) | Duration since injury (months) | First surgery | Last revision surgery | Bone graft | Time to union (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 34 | M | Atrophic (defect = 1.5 cm) | Isthmus | 1 | 15 | Antegrade nailing | LCP augmentation | Cancellous | 9 |
| 2 | 45 | M | Atrophic (defect = 1.3 cm) | Supra‐isthmus | 1 | 9 | Antegrade nailing | LCP augmentation | Cancellous | 12 |
| 3 | 36 | M | Atrophic (defect = 1.0 cm) | Subtrochanteric | 2 | 61 | Gamma nailing | PHLP | Fibula | 6 |
| 4 | 33 | M | Oligotrophic | Supra‐isthmus | 1 | 12 | Antegrade nailing | LCP augmentation | Cancellous | 6 |
| 5 | 44 | M | Atrophic (defect = 1.0 cm) | Isthmus | 2 | 13 | Antegrade nailing | LCP augmentation | Cancellous | 8 |
| 6 | 55 | M | Atrophic (defect = 1.2 cm) | Isthmus | 2 | 11 | Antegrade nailing | LCP augmentation | Cancellous | 8 |
| 7 | 28 | M | Atrophic (defect = 1.5 cm) | Isthmus | 2 | 16 | Antegrade nailing | LCP augmentation | Cancellous | 6 |
| 8 | 46 | F | Oligotrophic | Infra‐isthmus | 1 | 12 | Antegrade nailing | LCP augmentation | Cancellous | 6 |
| 9 | 36 | M | Atrophic | Infra‐isthmus | 1 | 13 | Antegrade nailing | LCP augmentation | Cancellous | 6 |
| 10 | 36 | M | Oligotrophic | Infra‐isthmus | 1 | 17 | Antegrade nailing | LCP augmentation | Cancellous | 8 |
| 11 | 42 | M | Atrophic (defect = 1.2 cm) | Subtrochanteric | 1 | 12 | Gamma nail | PHLP | Fibula | 8 |
| 12 | 32 | M | Atrophic | Infra‐isthmus | 1 | 14 | Retrograde nailing | LCP augmentation | Cancellous | 6 |
| 13 | 39 | M | Oligotrophic | Isthmus | 1 | 19 | Antegrade nailing | LCP augmentation | Cancellous | 8 |
Surgical management and follow‐up
The nonunion site was exposed through a lateral approach. Any dense fibrous tissue present was removed. Eleven cases were stabilized by additional locking compression plates (nine of them were manufactured by Synthes [Solothurn, Switzerland] and two by Chuang‐sheng [Changzhou, China]) placed at the lateral aspect of the femur with the nail left in place. Two high subtrochanteric nonunions were stabilized by proximal humeral anatomic locking plate (PHLP, Zimmer, Warsaw, IN, USA) placed at the anterolateral aspect of the proximal femur.
At least two unicortical locking screws were used on either side of the fracture site. Locking plates were of the same material as the nails, either stainless steel or titanium alloy. Stability was examined intraoperatively after fixation. There was visible movement at the fracture site in all cases before plate fixation; the movement disappeared in every case after plate fixation.
Eleven patients received autologous iliac‐crest cancellous bone grafts which were placed around the fracture site. Autologous nonvascularized fibular strut grafts were introduced at the medial cortex of the high subtrochanteric region in two cases. Two cortical screws were used to fix the free fibular bone graft in each case.
Tissue samples were collected for culture to rule out any hidden infection. Two tobacco users were asked to quit use of tobacco after treatment. Patients were kept non‐weight bearing until there was radiographic evidence of graft incorporation and advanced to full weight bearing when there was clinical and radiological evidence of healing.
The patients were followed up regularly at the outpatient clinic until their fractures had healed. Radiographic union was defined as bridging callus across three of four visible cortices on plain radiographs. Computed tomography was undertaken if necessary.
Results
All patients were followed up for a mean of 1.2 years (range, 1–2 years). The mean time to union was 7.5 months (range, 6–12 months) after the final revision surgery (Fig. 1a–c). All patients were ambulatory without pain at the fracture site during weight bearing at the final follow‐up. There were no major intra‐ or post‐ operative complications as infection or implant loosening. One patient complained of numbness in the anterior thigh region due to lateral femoral cutaneous nerve palsy after surgery; this symptom had disappeared completely 4 months later. There were no major donor site morbidities following resection of the fibula in the two fibular graft patients (Fig. 2a–c).
Figure 1.
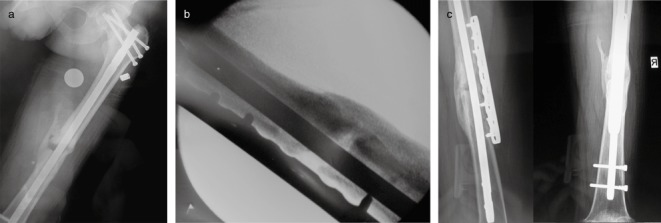
A 34‐year‐old male patient with femoral shaft fracture treated by intramedullary nailing. (a) Preoperative radiograph showing nonunion 15 months after the initial fracture management. (b) Intraoperative radiograph showing fixation with an augmentative locked plate and cancellous bone graft. (c) Radiograph at nine months after the revision surgery showing that the fracture nonunion has healed.
Figure 2.
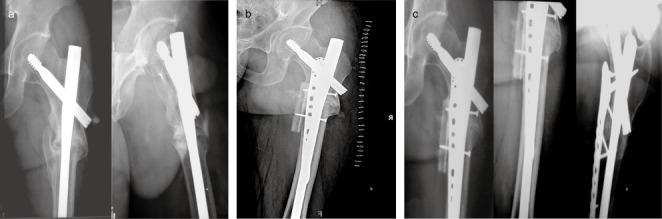
A 36‐year‐old male patient with high subtrochanteric fracture treated with long Gamma nail. Ten months after the initial surgery, dynamization was used because of deficient callus formation. Twenty‐three months after the initial surgery, distal locking was used again and autologous cancellous bone graft, performed because of failed dynamization. (a) Preoperative radiograph showing that, 42 months after the initial surgery, a high subtrochanteric nonunion has persisted in spite of bone graft. (b) Postoperative radiograph showing fixation with additional PHLP and autologous nonvascularized fibular bone graft. (c) Radiograph at 6 months after the third revision surgery showing that the nonunion has healed.
Discussion
The mechanism of femoral shaft nonunion is multifactorial. Nonunions usually occur secondary to unfavorable fracture patterns, poor reduction, and excessive soft tissue stripping or suboptimal position of internal fixation devices. Once nonunion has been detected, a successful treatment strategy should be based on the following three main goals: (i) achieving mechanical stability of the bone fragments; (ii) augmenting the potential for bone healing; and (iii) correcting any alignment deformity 7 .
Exchange nailing has been reported to be a very successful method for managing aseptic noncomminuted diaphyseal femoral nonunion after failure of nailing fixation, the bony union rate ranging from 72% to 100% 3 , 8 , 9 . However, some authors have reported higher failure rates when EN is used for the treatment of femoral nonunions that are not located in the diaphysis 4 , 5 . Shroeder et al. demonstrated that atrophic/oligotrophic nonunion correlates significantly with an adverse outcome 3 . In a recent study, results of EN and plate augmentation with a nail left in situ for nonisthmal femoral shaft nonunions after nailing were compared. In this study, all 11 cases in the additional plating group achieved osseous union, whereas 5 of 7 nonisthmic femoral shaft nonunions treated by EN failed to achieve bony union 6 .
The technique of augmentative plating for the treatment of femoral diaphyseal nonunion was first reported in 1997 by Ueng et al. 10 The plate provides additional stability when there is excessive motion at the nonunion site. The retained nail acts as a load‐sharing device, neutralizing shear forces on the nonunion site and maintaining alignment of the fracture. The internal fixator construct is strong enough to allow the patients to bear full weight and start vigorous rehabilitation immediately after the operation 10 . However, the procedure requires bicortical screw purchase through plate holes to achieve sufficient stability, which is often difficult to perform when the nail is left in place, especially when the nonunion site is at femoral isthmus.
The locked plate, a newly designed internal fixator, has gained wide popularity in recent years. The property of unicortical fixation of the locked plate may facilitate screw insertion. The complication of screws loosening reported by Choi and Kim can thus be prevented 11 . In addition, the fixed‐angle device preserves the periosteal blood supply, which is of paramount importance in the healing of nonunion. Locked plating is also especially useful for patients with the poor bone quality that is frequently encountered in nonunion cases. The main advantages provided by the locked plate method are the rigorous stability achieved in osteopenic bone and superior biomechanical environment for fracture healing 12 , 13 .
Autologous iliac‐crest cancellous bone graft was routinely used in our study and we found that it was sufficient to induce bone healing. Fibular bone grafts were introduced in two cases in which there was a gap on the medial side of the high subtrochantric region. We speculate that the high compressive and tensile forces across this specific region may pose great challenges to implant fixation, especially in cases with bone defects of the medial calcar 14 . Fibular cortical struts for reconstruction of bone defect on the medial side can provide additional mechanical support and offer an osteoinductive stimulus.
The main limitations of this study are the small number of cases, the retrospective methodology and the lack of a control group. However, on the basis of the satisfactory results, it can be safely concluded that augmentative locked plating is an effective and simple technique for the treatment of femoral diaphyseal nonunion after intramedullary nailing in selected cases.
Disclosure
This manuscript contains no information about medical device(s)/drug(s). The authors did not receive any outside funding or grants in support of the research for, or preparation of, this work. Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity.
References
- 1. Douglas L, Benson D, Seligson D. The incidence of nonunion after nailing of distal tibial and femoral fractures. Curr Orthop Pract, 2010, 21: 49–53. [Google Scholar]
- 2. Taitsman LA, Lynch JR, Agel J, et al Risk factors for femoral nonunion after femoral shaft fracture. J Trauma, 2009, 67: 1389–1392. [DOI] [PubMed] [Google Scholar]
- 3. Shroeder JE, Mosheiff R, Khoury A, et al The outcome of closed, intramedullary exchange nailing with reamed insertion in the treatment of femoral shaft nonunions. J Orthop Trauma, 2009, 23: 653–657. [DOI] [PubMed] [Google Scholar]
- 4. Banaszkiewicz PA, Sabboubeh A, McLeod I, et al Femoral exchange nailing for aseptic non‐union: not the end to all problems. Injury, 2003, 34: 349–356. [DOI] [PubMed] [Google Scholar]
- 5. Weresh MJ, Hakanson R, Stover MD, et al Failure of exchange reamed intramedullary nails for ununited femoral shaft fractures. J Orthop Trauma, 2000, 14: 335–338. [DOI] [PubMed] [Google Scholar]
- 6. Park J, Kim SG, Yoon HK, et al The treatment of nonisthmal femoral shaft nonunions with im nail exchange versus augmentation plating. J Orthop Trauma, 2010, 24: 89–94. [DOI] [PubMed] [Google Scholar]
- 7. Gao KD, Huang JH, Li F, et al Treatment of aseptic diaphyseal nonunion of the lower extremities with exchange intramedullary nailing and blocking screws without open bone graft. Orthop Surg, 2009, 1: 264–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brinker MR, O'Connor DP. Exchange nailing of ununited fractures. J Bone Joint Surg Am, 2007, 89: 177–188. [DOI] [PubMed] [Google Scholar]
- 9. Hak DJ, Lee SS, Goulet JA. Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma, 2000, 14: 178–182. [DOI] [PubMed] [Google Scholar]
- 10. Ueng SW, Chao EK, Lee SS, et al Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma, 1997, 43: 640–644. [DOI] [PubMed] [Google Scholar]
- 11. Choi YS, Kim KS. Plate augmentation leaving the nail in situ and bone grafting for non‐union of femoral shaft fractures. Int Orthop, 2005, 29: 287–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smith WR, Ziran BH, Anglen JO, et al Locking plates: tips and tricks. J Bone Joint Surg Am, 2007, 89: 2298–2307. [DOI] [PubMed] [Google Scholar]
- 13. Kubiak EN, Fulkerson E, Strauss E, et al The evolution of locked plates. J Bone Joint Surg Am, 2006, 88 (Suppl. 4): S189–S200. [DOI] [PubMed] [Google Scholar]
- 14. Haidukewych GJ, Berry DJ. Nonunion of fractures of the subtrochanteric region of the femur. Clin Orthop Relat Res, 2004, 419: 185–188. [DOI] [PubMed] [Google Scholar]


