Abstract
Rupture of the medial head of the gastrocnemius, known as “tennis leg”, typically occurs when the muscle has been overstretched by dorsiflexion of the ankle with full knee extension. The classic clinical presentation is a middle‐aged person who complains of sports‐related acute pain in the mid portion of the calf, associated with a snapping sensation. Magnetic resonance imaging (MRI) or ultrasound is often required to evaluate patients with this condition. This injury is usually managed non‐operatively, surgical treatment rarely being indicated according to published reports. One case of longstanding and one of recent rupture of the musculotendinous junction of the medial head of the gastrocnemius that were successfully treated by surgical repair are presented here and the MRI characteristics and indications for surgery are discussed.
Keywords: Gastrocnemius, Magnetic resonance imaging, Rupture, Surgical repair
Introduction
Rupture of the distal musculotendinous junction (MTJ) of the medial head of the gastrocnemius, also called “tennis leg”, is a relatively common clinical condition. It occurs mainly when the muscle has been overstretched, either during sporting activities or during common daily activities, and those affected are frequently middle‐aged, physically active patients1, 2, 3. The initial diagnosis is made based on a careful history and clinical examination and is confirmed by MRI or ultrasound. Surgical treatment is rarely described in published reports because the mainstay of treatment is conservative4. In this report, we present our experience of surgical repair of ruptures of the medial head of the gastrocnemius and the good clinical results that we achieved. The relative importance of, and indications for, surgical repair are also discussed. Our patients were informed that data concerning their cases would be submitted for publication and gave their consent for this.
Cases Reports
Case 1
Whilst playing basketball, a 37‐year‐old man experienced acute pain in the posterior aspect of his left calf subsequent to a lay‐up shot and experienced immediate difficulty in walking. Swelling and ecchymosis developed within a few hours. The patient was examined in our hospital 6 days after the injury. Physical examination revealed a palpable defect in the medial head of the gastrocnemius just above the MTJ with marked tenderness and mild edema. Furthermore, the patient could not toe stand on the left because of weakness of plantar flexion. MRI showed a hematoma at gastrocnemius MTJ and retraction of muscle fibers consistent with complete gastrocnemius rupture (Fig. 1). Because his symptoms did not improve as expected with acute conservative treatment, surgical repair was performed 10 days after the injury (Figs 2, 3). Two months after the operation, the patient could walk without pain and had a full range of motion in the ankle.
Figure 1.
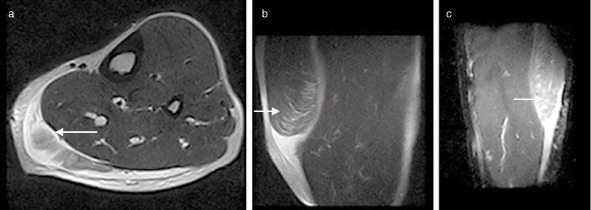
(a) Axial T2W, (b) coronal T2W and (c) sagittal fat‐saturated images demonstrating hyperintensity at the MTJ due to a complete tear with diffuse edema and intermuscular hematoma (arrows).
Figure 2.
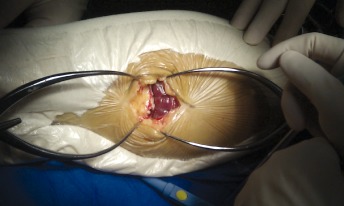
Complete rupture at the MTJ with visualization of dehiscence and retraction of the proximal gastrocnemius muscle.
Figure 3.

Intermuscular hematoma; the underlying soleus muscle is intact.
Case 2
Whilst playing badminton, a 43‐year‐old woman felt sudden pain in the posterior aspect of her left calf as if she had been struck by a ball or racket, followed by a feeling of weakness in the limb and subsequent ecchymosis and swelling. At a local hospital she was diagnosed as having muscle strain and treated conservatively with rest and analgesics. However, 7 months after the injury, she came to our hospital requesting surgical treatment because of persistent pain in her left leg that was exacerbated by walking and stair climbing. Clinical examination revealed a palpable defect and localized soreness in the medial head of the gastrocnemius just above the MTJ (Fig. 4) and an objective loss of power in ankle dorsiflexion and plantarflexion. A tennis leg was suspected and MRI requested. MRI revealed complete rupture at the MTJ and retraction of proximal muscle fibers with scar tissue formation (Fig. 5). Because of her ongoing disability, surgical exploration was undertaken (Fig. 6). 10 months after the surgery, the patient noted only mild ache after prolonged walking and her leg strength was comparable with that on the right.
Figure 4.

Visible local dehiscence and proximally displaced muscle head in the left posterior calf.
Figure 5.
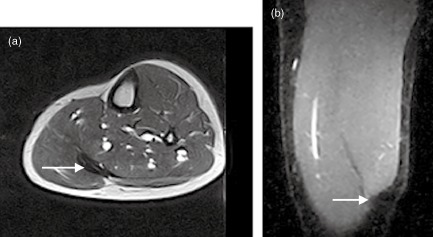
(a) Axial T2W and (b) sagittal fat‐saturated images demonstrating an area of nodular hypointensity with focal tendon thickening and scar tissue formation (arrows), the chronic changes of a complete tear at the MTJ.
Figure 6.
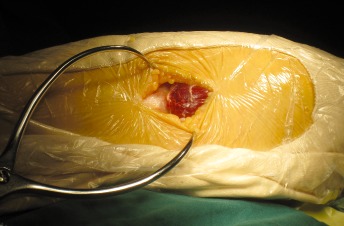
Complete rupture at the MTJ with visualization of the gap and bulging of the proximal retracted muscle.
Characteristics on Magnetic Resonance Imaging
Magnetic resonance imaging should consist of T1 and T2 series in addition to fluid sensitive fat suppressed sequences. Characteristic findings include a feathered appearance indicating edematous changes involving the MTJ, intramuscular hematoma, intermuscular fluid collections, and complete rupture with retraction of the proximal muscle fibers, typically characterized by indistinctness of the tapering distal MTJ, which is often bunched up so as to appear rounded. In chronic cases, MRI may detect macroscopic foci of scar tissue along with focal tendon thickening and peritendinous muscular atrophy.
Surgical Treatment
A single longitudinal incision is centered over the middle of the defect. After evacuation of hematoma, an oblique rupture of the medial head of the gastrocnemius at the MTJ accompanied by a visible gap and muscle contracture can be confirmed. The retracted proximal muscle fibers protrude as a bundle and should be loosened and reattached to the distal end using absorbable and non‐absorbable sutures with the foot held in plantar flexion. According to our experience, sutures should engage healthy contractile muscle tissue to achieve proper reattachment, especially in chronic injury, in which scar tissue should be excised first.
After surgery, the patient is immobilized for 3 weeks in a long leg cast with the knee flexed 60° and the ankle plantar flexed 20°–30° and then for an additional 3 weeks in a below‐knee cast with ankle plantar flexion. After removal of the cast, the patient can start range of motion exercises with progressive weight‐bearing.
Discussion
The pathogenesis of Tennis leg has been debated since Powell first described it in 1883. Initially, it was attributed to rupture of the plantaris tendon. However, surgical and imaging studies eventually clarified that the most common lesion underlying tennis leg is an avulsion injury of the gastrocnemius rather than the plantaris3, 5. The gastrocnemius is at high risk for injuries because it crosses two joints (the knee and ankle) and possesses a high proportion of type two fast twitch muscle fibers, reflective of its function in rapid locomotion such as jumping and running6, 7. Because the gastrocnemius muscle spans two joints, the injury typically occurs during full extension of the knee with simultaneous forced dorsiflexion of the ankle, which implies sudden and maximal overstretching of the gastrocnemius. However, it can also occur during active ankle plantar flexion when the knee is in full extension. The attempt to contract in an already lengthened state leads to tearing of the muscle8, 9.
Although frequently ignored or misdiagnosed, the signs and symptoms of gastrocnemius rupture are characteristic. The patient generally reports a sudden pain in the calf, which may be accompanied by a popping or tearing sensation as though someone has kicked the back of his or her leg, and subsequent difficulty walking. Sometimes there is prodromal aching in the calf before rupture4, 10. Subsequently, swelling and ecchymosis may be visible. Rarely, the swelling is so extensive that it causes an acute compartment syndrome11, 12, 13. Physical examination reveals local swelling and tenderness and sometimes a defect in the mid portion of the calf. Depending on the severity of the tear, the patient may be unable to sustain toe standing with the affected extremity and have decreased plantar flexion power.
The history and clinical examination are sometimes enough to make this diagnosis and MRI or ultrasound should be utilized to confirm it, evaluate the extent of injury, and exclude other pathologies, such as ruptured Baker's cyst, proximal Achilles tendon tear and deep vein thrombosis1, 3, 8, 14. MRI is the imaging modality preferred by the authors because it provides a global and extensive view of injuries and even the ability to detect relatively small signal intensity changes. Also, MRI provides anatomical detailed information such as correct assessment of the amount of muscle retraction, which is important information for preoperative planning7, 15.
Published reports recommend routinely treating tennis leg non‐operatively by rest, ice packs, leg elevation, and anti‐inflammatory and analgesic medications followed by a stretching and strengthening program. Surgical treatment is reportedly indicated only when an associated compartment syndrome has complicated evolution of the symptoms and signs4, 16, 17, 18. However, it is common to find marked destruction of anatomical structures during surgery, the complete reconstruction of which is only possible by early surgical repair. In cases of complete rupture, the mass of contracted muscle and the gap between the divided ends tend to produce persistent pain and to preclude regaining of full strength. Furthermore, a severe muscle tear treated conservatively is likely to heal with fibrotic scar tissue, which absorbs forces differently, and is thus at increased risk of recurrent injury19, 20. Therefore, severe cases, which are identified largely on clinical grounds, require primary surgical repair. Dr. Miller believes that inability to stand on tiptoe or sustain body weight on the metatarsal heads of the involved leg alone is an indication for surgery10. Dr. Leach believed that a palpable defect that is not be closed by foot dorsiflexion and knee flexion should be surgically repaired. We believe that severe (grade III) tears or large intramuscular hematomas for indicating surgery (Table 1). Furthermore, we recommend consideration of surgical treatment in patients who complain of ongoing extension pain (duration > 4–6 months) with evidence of contracture, especially when an obvious defect and clear extension deficit accompany the pain. In such cases, formation of scar adhesions restricting the movement of the injured muscle should be suspected and surgical division of adhesions considered. We also recommend surgical repair in young patients who are actively involved in sports to facilitate rapid and complete return to normal function6, 21, 22. In addition, we suggest early surgery because it allows early functional rehabilitation and leaves a smaller defect. Early surgery is often easier than in chronic complete avulsions in which fatty degeneration and fibrous remodeling of the ruptured muscle tissue with consecutive atrophy are always present. However, even in chronic cases, surgery can achieve considerable improvement of symptoms. Despite the fact that the duration of the treatment is about the same, a better anatomical and functional result can be expected after surgical repair than after conservative treatment19, 23.
Table 1.
Grades of tennis leg
| Grade | Symptoms | Signs | Pathologic findings | Radiologic findings |
|---|---|---|---|---|
| Grade 1 (mild) | Sharp pain at time of injury or pain with activity. Usually able to continue activity | Mild pain and localized tenderness. Mild spasm and swelling. No or minimal loss of strength and range of motion | <10% muscle fibers disrupted | Bright signals on fluid‐sensitive sequences. Feathery appearance < 5% muscle fiber involvement |
| Grade 2 (moderate) | Unable to continue activity | Clear loss of strength and range of motion | 10%–50% disruption of muscle fibers | Change in myotendinous junction. Edema and hemorrhage |
| Grade 3 (severe) | Immediate severe pain, disability | Complete loss of muscle function. Palpable defect or mass | 50%–100% disruption of muscle fibers | Complete disruption of continuity of muscle. Extensive edema and hemorrhage. Wavy tendon morphology and retraction |
Conclusion
A common guideline regarding tennis leg injuries is non‐operative treatment. There are, however, certain highly specific indications in which surgical intervention might be beneficial, even though no evidence‐based treatment protocol is available for operative treatment of severe muscle ruptures. The authors propose consideration of surgery for complete rupture and for patients with prolonged (4–6 months) pain with evidence of contracture. Large intramuscular hematomas may impair clinical progress and are also indications for surgical referral. Furthermore, we suggest surgical repair in young patients who are actively involved in sports, to ensure strength for continued sports activity. Further studies are needed to evaluate who requires surgery, and at which point it should be considered.
Disclosure: The authors declare no conflict of interest. No benefits in any form have been, or will be, received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1. Flecca D, Tomei A, Ravazzolo N, et al US evaluation and diagnosis of rupture of the medial head of the gastrocnemius (tennis leg). J Ultrasound, 2007, 10: 194–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yilmaz C, Orgenc Y, Ergenc R, et al Rupture of the medial gastrocnemius muscle during namaz praying: an unusual cause of tennis leg. Comput Med Imaging Graph, 2008, 32: 728–731. [DOI] [PubMed] [Google Scholar]
- 3. Delgado GJ, Chung CB, Lektrakul N, et al Tennis leg: clinical US study of 141 patients and anatomic investigation of four cadavers with MR imaging and US. Radiology, 2002, 224: 112–119. [DOI] [PubMed] [Google Scholar]
- 4. Campbell JT. Posterior calf injury. Foot Ankle Clin, 2009, 14: 761–771. [DOI] [PubMed] [Google Scholar]
- 5. Powel RW. Lawn tennis leg. Lancet, 1883, 2: 44. [Google Scholar]
- 6. Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf muscle injuries. Curr Rev Musculoskelet Med, 2009, 2: 74–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Koulouris G, Ting AY, Jhamb A, et al Magnetic resonance imaging findings of injuries to the calf muscle complex. Skeletal Radiol, 2007, 36: 921–927. [DOI] [PubMed] [Google Scholar]
- 8. Watura C, Harries W. Isolated tear of the tendon to the medial head of gastrocnemius presenting as a painless lump in the calf. BMJ Case Rep, 2009, 2009. pii: bcr01.2009.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Maehara H, Sakaguchi Y. Avulsion fracture of the medial head of the gastrocnemius muscle. A case report. J Bone Joint Surg Am, 2004, 86: 373–375. [DOI] [PubMed] [Google Scholar]
- 10. Miller WA. Rupture of the musculotendinous juncture of the medial head of the gastrocnemius muscle. Am J Sports Med, 1977, 5: 191–193. [DOI] [PubMed] [Google Scholar]
- 11. Straehley D, Jones WW. Acute compartment syndrome (anterior, lateral, and superficial posterior) following tear of the medial head of the gastrocnemius muscle. A case report. Am J Sport Med, 1986, 14: 96–99. [DOI] [PubMed] [Google Scholar]
- 12. Pai V, Pai V. Acute compartment syndrome after rupture of the medial head of gastrocnemis in a child. J Foot Ankle Surg, 2007, 46: 288–290. [DOI] [PubMed] [Google Scholar]
- 13. Russell GV Jr, Pearsall AW 4th, Caylor MT, et al Acute compartment syndrome after rupture of the medial head of the gastrocnemius muscle. South Med J, 2000, 93: 247–249. [PubMed] [Google Scholar]
- 14. Slawski DP. Deep venous thrombosis complicating rupture of the medial head of the gastrocnemius muscle. J Orthop Trauma, 1994, 8: 263–264. [DOI] [PubMed] [Google Scholar]
- 15. Menz MJ, Lucas GL. Magnetic resonance imaging of a rupture of the medial head of the gastrocnemius muscle. A case report. J Bone Joint Surg Am, 1991, 73: 1260–1262. [PubMed] [Google Scholar]
- 16. Kwak HS, Lee KB, Han YM. Ruptures of the medial head of the gastrocnemius (“tennis leg”): clinical outcome and compression effect. Clin Imaging, 2006, 30: 48–53. [DOI] [PubMed] [Google Scholar]
- 17. Millar AP. Strains of the posterior calf musculature (“tennis leg”). Am J Sports Med, 1979, 7: 172–174. [DOI] [PubMed] [Google Scholar]
- 18. Shields CL Jr, Redix L, Brewster CE. Acute tears of the medial head of the gastrocnemius. Foot Ankle, 1985, 5: 186–190. [DOI] [PubMed] [Google Scholar]
- 19. Dürig M, Schuppisser JP, Gauer EF, et al Spontaneous rupture of the gastrocnemius muscle. Injury, 1977, 9: 143–145. [DOI] [PubMed] [Google Scholar]
- 20. Renne JW, Davis PH. An unusual gastrocnemius muscle syndrome. Case report. J Bone Joint Surg Am, 1973, 55: 1294–1296. [PubMed] [Google Scholar]
- 21. Järvinen TA, Järvinen TL, Kääriäinen M, et al Muscle injuries: biology and treatment. Am J Sports Med, 2005, 33: 745–764. [DOI] [PubMed] [Google Scholar]
- 22. Almekinders LC. Results of surgical repair versus splinting of experimentally transected muscle. J Orthop Trauma, 1991, 5: 173–176. [DOI] [PubMed] [Google Scholar]
- 23. Järvinen TA, Järvinen TL, Kääriäinen M, et al Muscle injuries: optimising recovery. Best Pract Res Clin Rheumatol, 2007, 21: 317–331. [DOI] [PubMed] [Google Scholar]


