Key Points
Question
Do schoolchildren treated for attention-deficit/hyperactivity disorder have worse education and health outcomes than their peers?
Findings
In this population-based cohort study, 766 244 singleton children attended Scottish schools between 2009 and 2013. The 7413 children receiving medication for attention-deficit/hyperactivity disorder had worse education outcomes (unauthorized absence, exclusion, special educational need, lower academic attainment, left school earlier, and higher unemployment) and health outcomes (hospitalizations overall and for injury).
Meaning
Even with medication, children with attention-deficit/hyperactivity disorder fare worse than their peers across a wide range of outcomes relating not only to education but also health.
Abstract
Importance
Attention-deficit/hyperactivity disorder (ADHD) affects 39 million people worldwide; in isolation, it doubles annual health care costs and, when associated with comorbid mental health problems, it quadruples the costs.
Objective
To compare the education and health outcomes of schoolchildren treated for ADHD with their peers.
Design, Setting, and Participants
In this population-based cohort study, individual-level record linkage was performed of 8 Scotland-wide administrative databases covering dispensed prescriptions, admissions to acute and psychiatric hospitals, maternity records, annual pupil census, examinations, school absences and exclusions, and unemployment. The study cohort comprised 766 244 children attending Scottish primary, secondary, and special schools at any point between September 21, 2009, and September 18, 2013. Data analysis was performed from June 1, 2015, to December 6, 2016.
Exposures
Medication approved solely for ADHD treatment.
Main Outcomes and Measures
Special educational needs, academic attainment, unauthorized absence, exclusion, age at leaving school, unemployment after leaving, and hospitalization. Outcomes were adjusted for potential sociodemographic, maternity, and comorbidity confounders.
Results
Of the 766 244 schoolchildren, 7413 (1.0%) were treated for ADHD; 6287 (84.8%) were male. These children had higher rates of unauthorized absence (adjusted incidence rate ratio [IRR], 1.16; 95% CI, 1.14-1.19) and exclusion (adjusted IRR, 5.79; 95% CI, 5.45-6.16), more commonly had a record of special educational need (adjusted odds ratio [OR], 8.62; 95% CI, 8.26-9.00), achieved lower academic attainment (adjusted OR, 3.35; 95% CI, 3.00-3.75), were more likely to leave school before age 16 years (1546 [64.3%] vs 61 235 [28.4%]), and were more likely to be unemployed (adjusted OR, 1.39; 95% CI, 1.25-1.53). Children with ADHD were more likely to require hospitalization overall (adjusted hazard ratio [HR], 1.25; 95% CI, 1.19-1.31) and for injury (adjusted HR, 1.52; 95% CI, 1.40-1.65).
Conclusions and Relevance
Even while receiving medication, children with ADHD fare worse than their peers across a wide range of outcomes relating not only to education but also to health.
This population-based cohort study examines educational and health outcomes in children with attention-deficit/hyperactivity disorder compared with their unaffected peers.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a relatively common psychiatric condition characterized by persistent inattention, hyperactivity, and impulsivity. Pooled estimates from meta-analyses suggest that ADHD affects approximately 5.3% of the general population (6.5% of children) and is 4 times more common in boys.1 In 2013, the World Health Organization estimated that 39 million people worldwide are affected.2 Attention-deficit/hyperactivity disorder is associated with comorbid conditions, including low self-esteem, mood disorders, substance abuse, learning disabilities, and disruptive behavior disorders.3,4,5 Compared with the costs for unaffected children, the health care costs for children with ADHD are double—quadruple among those with comorbid mental health disorders.6 The annual health- and work-related costs of ADHD in the United States total $32 billion.7 No cure has yet been identified, but symptoms can be managed using medication: methylphenidate hydrochloride, dexamphetamine sulfate, lisdexamphetamine dimesylate, atomoxetine, and guanfacine hydrochloride. Children with ADHD are more prone to difficulties with reading, writing, and executive function,8,9,10,11 but medication may improve concentration by controlling impulsivity and promoting calmness.12
In the United Kingdom, ADHD medication use increased 34-fold between 1992 and 200813 owing to greater awareness of the condition, more positive perception of medicine, longer maintenance of treatment, and increased use in girls.14,15 Use of the medication plateaued thereafter following publication of UK recommendations suggesting that medication should not be used as first-line treatment in children with mild to moderate ADHD.16 This recommendation is contrary to guidelines from the American Academy of Pediatrics, which recommends medication for all affected children.17
Previous studies comparing the outcomes of children with ADHD with those of their unaffected peers have been relatively small (most <500 participants), and we are unaware of any previous national studies of educational outcomes. The present study linked, at an individual level, all relevant Scotland-wide administrative databases from the health and education sectors to undertake a large-scale, general population cohort study. We hypothesized that children treated for ADHD would have worse education and health outcomes than their unaffected peers.
Methods
Databases
We linked individual-level data from 4 Scotland-wide health databases, held by the Information Services Division of the National Health Service, and 4 Scotland-wide education databases, held by the Scottish Exchange of Educational Data (ScotXed). The linkage methodology has been described in detail previously.18 The study was approved by the National Health Service National Services Scotland Privacy Advisory Committee. A data processing agreement was drafted between Glasgow University and the Information Services Division and a data sharing agreement between Glasgow University and ScotXed. Data were deidentified. Both the health and education data operate on the basis of nonwritten informed consent, and have been determined to be consistent with the uses and agreements to which patients, pupils, and parents had consented.
The prescribing information system collects information on all prescriptions dispensed to Scottish residents by community pharmacies or primary care. The Scottish Morbidity Record 02 (SMR02) maternity database collects data on maternal, obstetric, and child factors; SMR01 and SMR04 record admissions to acute and psychiatric hospitals, respectively, including dates of admission and discharge, and the main and secondary diseases are recorded using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10).
The pupil census is conducted annually by all local authority-run primary, secondary, and special schools. The information includes whether the child has a special educational need and, if so, its type. Approved and unapproved absences and exclusions are collected prospectively and appended at the end of each school term. The Scottish Qualifications Authority (http://www.sqa.org.uk/sqa/70972.html) collects examination attainment data for all Scottish schoolchildren. The School Leaver database (http://www.gov.scot/Topics/Statistics/Browse/School-Education/RollsByStage) collects information on the status of pupils 6 months after leaving school: paid/voluntary employment, higher/further education, training, or unemployment.
Inclusion Criteria, Definitions, and Outcomes
We excluded individuals whose age was recorded as younger than 4 years or older than 19 years in the pupil census. For multiple births involving offspring of the same sex, it is not possible to be certain that the correct child has been linked; therefore, this study was restricted to singleton children. We used prescribing information system data to identify children who had been dispensed 1 or more medication approved solely for the treatment of ADHD on at least 1 occasion over the same pupil census year: methylphenidate, dexamphetamine, atomoxetine, or lisdexamphetamine. Therefore, the exposed group comprised singleton children who attended a Scotland school at some point between September 21, 2009, and September 18, 2013, and received at least 1 medication for ADHD during that time. The comparison group was the same except that the children did not receive ADHD medication.
We studied 6 educational outcomes: total number of days of unauthorized absence, total number of exclusions, any record of special educational need, type of special educational need, academic achievement, and unemployment. Analyses of the latter 2 outcomes were restricted to the subgroup of pupils who left school during the study period. In addition, absence and exclusion data were available only for 2009, 2010, and 2012.
Special educational need is defined as being unable to benefit fully from school education without help beyond that normally given to schoolchildren of the same age. We included special educational need attributed to intellectual disabilities, dyslexia, physical or motor impairment, language or speech disorder, autistic spectrum disorder, and social, emotional, and behavioral difficulties. A child could be recorded as having more than 1 of these types of need. Academic achievement was derived from the number of awards attained at each level of the Scottish Credit Qualifications Framework and converted into an ordinal variable: low attainment (≥1 at level 2, <5 at level 3, or <2 at level 4), basic attainment (≥5 at level 3, ≥2 at level 4, or ≤4 at level 5), broad general attainment (>7 at level 4, >5 at level 5, or <3 at level 6), and high attainment (>1 at level 7 or ≥3 at level 6). Leaver destination was collapsed into a dichotomous variable of education/employment/training or unemployment. We studied 2 health outcomes: any hospital admission and hospital admission due to injury (ICD-10 codes S00-T98). Data on acute and psychiatric hospital admissions were available until September 21, 2014, providing a mean follow-up period of 3.81 years (range, 1 day to 5 years).
The pupil census provided data on the child’s ethnicity and age. Area socioeconomic deprivation was derived from postcode of residence using the Scottish Index of Multiple Deprivation 2012 (SIMD) (http://www.gov.scot/Topics/Statistics/SIMD/BackgroundMethodology), and children were allocated to general population quintiles. The SIMD is derived from 38 indicators across 7 domains (income, employment, health, housing, geographic access, crime and education, and skills and training) using information collected for data zones of residence (median population, 769). Retrospective linkage to SMR02 provided data on maternal age at delivery, parity, maternal smoking, gestational age at delivery, mode of delivery, and 5-minute Apgar score. We also derived sex- and gestation-specific birthweight centiles as a measure of intrauterine growth. Comorbid diabetes, asthma, epilepsy, and depression were ascertained from relevant dispensed medication: insulin, corticosteroid inhalers, antiepileptic medication, and antidepressants. All of the above factors were treated as potential confounders. We also explored age, sex, and deprivation as potential effect modifiers. We tested for statistical interactions and, where significant, undertook subgroup analyses.
Statistical Analysis
The characteristics of children receiving ADHD medication were compared with their peers using χ2 tests for categorical data and χ2 tests for trend for ordinal data. Leaver status and academic attainment were analyzed using binary and multinomial logistic regression analyses. Special educational need, absences, and exclusions were analyzed using generalized estimating equations to adjust for correlations between repeated observations relating to the same pupil across different census years. The user-written quasi-likelihood under the independence model criterion (QIC) statistic was used to compare different correlation structures. The structure with the lowest trace QIC was selected as being the most appropriate. The number of days absent and number of exclusions were modeled using univariate and multivariable longitudinal generalized estimating equations analyses with a negative binomial distribution and log link function. The total number of possible attendances recorded within each census year was used as an offset variable to adjust for exposure time for each pupil. Special educational need was modeled using generalized estimating equation analyses with a binomial distribution and logit link.
Associations between ADHD medication use and unemployment (univariate and multivariable binary logistic regression model), academic attainment (univariate and multivariable ordinal logistic regression model), and time to hospital admission (univariate and multivariable Cox proportional hazards regression model) were investigated. All multivariable models were run adjusting for sociodemographic and maternity confounders and then rerun also adjusting for comorbid conditions. For academic attainment and unemployment, we reran the multivariable models including absenteeism to explore whether absenteeism was a mediator. For academic attainment and unemployment, we also reran the models excluding children with special educational needs. Tests for proportional hazards were conducted using the estat phtest command within Stata. All statistical analyses were undertaken using Stata MP, version 14.1 (StataCorp). Data analysis was performed from June 1, 2015, to December 6, 2016.
Results
Between 2009 and 2013, 766 244 singleton children attended Scottish schools; of these, 7413 (1.0%) received ADHD medication. Treated children were more likely to be male, socioeconomically deprived, and have a mother who was younger, parous, and smoked during pregnancy (Table 1). Children receiving ADHD medication were born at an earlier gestational age and had a lower sex- and gestation-specific birthweight centile and lower APGAR scores (Table 1). Children treated for ADHD were more likely to have a record of learning disability (959 [12.9%] vs 18 754 [2.5%]), autistic spectrum disorder (855 [11.5%] vs 7635 [1.0%]), or both (241 [3.3%] vs 2083 [0.3%]), and 1546 (64.3%) of these children left school before age 16 years compared with 61 235 (28.4%) of their peers.
Table 1. Characteristics of Schoolchildren by Presence or Absence of ADHD.
| Characteristic | No. (%)a | P Value | |
|---|---|---|---|
| No ADHD (n = 758 831) |
ADHD (n = 7413) |
||
| Sociodemographic Factor | |||
| Sex | |||
| Male | 384 003 (50.6) | 6287 (84.8) | <.001 |
| Female | 374 828 (49.4) | 1126 (15.2) | |
| Missing | 0 | 0 | |
| Deprivation quintileb | |||
| 1 (most deprived) | 171 399 (22.6) | 2395 (32.3) | <.001 |
| 2 | 151 765 (20.0) | 1804 (24.4) | |
| 3 | 146 585 (19.3) | 1339 (18.1) | |
| 4 | 148 409 (19.6) | 1114 (15.0) | |
| 5 (least deprived) | 140 084 (18.5) | 756 (10.2) | |
| Missing | 589 | 5 | |
| Ethnic group | |||
| White | 720 881 (96.2) | 7235 (98.9) | <.001 |
| Asian | 17 759 (2.4) | 18 (0.2) | |
| Black | 1959 (0.3) | 6 (0.1) | |
| Mixed | 6693 (0.9) | 35 (0.5) | |
| Other | 2055 (0.3) | 21 (0.3) | |
| Missing | 9484 | 98 | |
| Medication for comorbid conditions | |||
| Epilepsy | 5137 (0.7) | 177 (2.4) | <.001 |
| Depression | 5151 (0.7) | 191 (2.6) | <.001 |
| Asthma | 45 256 (6.0) | 644 (8.7) | <.001 |
| Diabetes | 3299 (0.4) | 31 (0.4) | .83 |
| Maternity Factors | |||
| Maternal age, y | |||
| ≤24 | 206 525 (27.2) | 3353 (45.2) | <.001 |
| 25-29 | 222 536 (29.3) | 2004 (27.0) | |
| 30-34 | 215 529 (28.4) | 1406 (19.0) | |
| ≥35 | 114 229 (15.1) | 650 (8.8) | |
| Missing | 12 | 0 | |
| Maternal smoking | |||
| No | 487 722 (72.5) | 3392 (51.4) | <.001 |
| Yes | 184 582 (27.5) | 3207 (48.6) | |
| Missing | 86 527 | 814 | |
| Parity | |||
| 0 | 342 365 (45.3) | 3300 (44.9) | <.001 |
| 1 | 261 846 (34.7) | 2296 (31.3) | |
| >1 | 150 820 (20.0) | 1750 (23.8) | |
| Missing | 3800 | 67 | |
| Mode of delivery | |||
| SVD | 511 105 (67.4) | 5114 (69.0) | <.001 |
| Assisted vaginal | 90 870 (12.0) | 787 (10.6) | |
| Breech vaginal | 2210 (0.3) | 23 (0.3) | |
| Elective CS | 57 821 (7.6) | 493 (6.7) | |
| Emergency CS | 96 661 (12.7) | 995 (13.4) | |
| Other | 162 (<0.01) | 1 (<0.01) | |
| Missing | 2 | 0 | |
| Gestational age, wk | |||
| <24 | 29 (<0.1) | 0 | <.001 |
| 24-27 | 1086 (0.1) | 39 (0.5) | |
| 28-32 | 6921 (0.9) | 137 (1.8) | |
| 33-36 | 35 063 (4.6) | 539 (7.3) | |
| 37 | 37 142 (4.9) | 477 (6.4) | |
| 38 | 94 939 (12.5) | 1053 (14.2) | |
| 39 | 157 241 (20.7) | 1499 (20.2) | |
| 40 | 228 451 (30.1) | 1979 (26.7) | |
| 41 | 169 751 (22.4) | 1442 (19.5) | |
| 42 | 26 891 (3.5) | 233 (3.1) | |
| 43 | 619 (0.1) | 11 (0.1) | |
| >43 | 139 (<0.01) | 1 (<0.01) | |
| Missing | 559 | 3 | |
| Sex-, gestation-specific birthweight centile | |||
| 1-3 | 31 077 (4.1) | 409 (5.5) | <.001 |
| 4-10 | 67 862 (9.0) | 784 (10.6) | |
| 11-20 | 90 383 (11.9) | 965 (13.0) | |
| 21-80 | 445 950 (58.8) | 4171 (56.3) | |
| 81-90 | 64 815 (8.6) | 548 (7.4) | |
| 91-97 | 40 848 (5.4) | 373 (5.0) | |
| 98-100 | 16 921 (2.2) | 158 (2.1) | |
| Missing | 975 | 5 | |
| 5-min Apgar score | |||
| 1-3 | 3645 (0.5) | 64 (0.9) | <.001 |
| 4-6 | 7192 (1.0) | 110 (1.5) | |
| 7-10 | 740 294 (98.6) | 7118 (97.6) | |
| Missing | 7700 | 121 | |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; CS, cesarean section; SVD, spontaneous vaginal delivery.
Percentages determined using available data.
Determined using the Scottish Index of Multiple Deprivation.
The subgroup analyses of absences and exclusion included 702 210 children. Children receiving ADHD medication had more days of unauthorized absence (Table 2). There were significant interactions with age (χ2 = 69.22; P < .001) and deprivation (χ2 = 50.71; P < .001). The association was stronger among older and less deprived children (Table 2). The smaller relative effect on deprived children was due to higher levels of absence among deprived children not receiving ADHD medication (medians, 11.0 and 5.5 days in the most and least deprived quintiles, respectively). Among children receiving ADHD medication, absences were still more common in the most deprived quintile (medians, 12.0 vs 6.5 days).
Table 2. Association Between ADHD Medication and Unauthorized Absence From School .
| Characteristic | IRR (95% CI) | ||
|---|---|---|---|
| Univariate | Multivariablea | Multivariableb | |
| Overall | 1.37 (1.33-1.40) | 1.18 (1.16-1.21) | 1.16 (1.14-1.19) |
| Boys | 1.37 (1.34-1.41) | 1.18 (1.15-1.21) | 1.16 (1.13-1.19) |
| Girls | 1.43 (1.35-1.53) | 1.20 (1.13-1.27) | 1.15 (1.09-1.22) |
| Age, y | |||
| <11 | 1.24 (1.21-1.28) | 1.08 (1.05-1.11) | 1.07 (1.04-1.10) |
| 11-14 | 1.49 (1.44-1.54) | 1.27 (1.22-1.31) | 1.24 (1.20-1.28) |
| >14 | 1.42 (1.36-1.48) | 1.26 (1.21-1.32) | 1.23 (1.18-1.28) |
| Deprivation quintilec | |||
| 1 (most deprived) | 1.16 (1.11-1.20) | 1.10 (1.06-1.14) | 1.09 (1.05-1.13) |
| 2 | 1.27 (1.21-1.33) | 1.16 (1.11-1.21) | 1.14 (1.09-1.19) |
| 3 | 1.42 (1.35-1.51) | 1.27 (1.21-1.34) | 1.25 (1.19-1.32) |
| 4 | 1.28 (1.20-1.36) | 1.19 (1.12-1.26) | 1.16 (1.09-1.22) |
| 5 (least deprived) | 1.47 (1.36-1.59) | 1.31 (1.22-1.41) | 1.25 (1.17-1.34) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; IRR, incidence rate ratio.
Adjusted for age, sex, deprivation quintile and ethnic group, maternal age, maternal smoking, parity, mode of delivery, gestational age at delivery, and sex- and gestation-specific birthweight centile (as appropriate).
Also adjusted for comorbid conditions (ie, diabetes, asthma, epilepsy, and depression).
Determined using the Scottish Index of Multiple Deprivation.
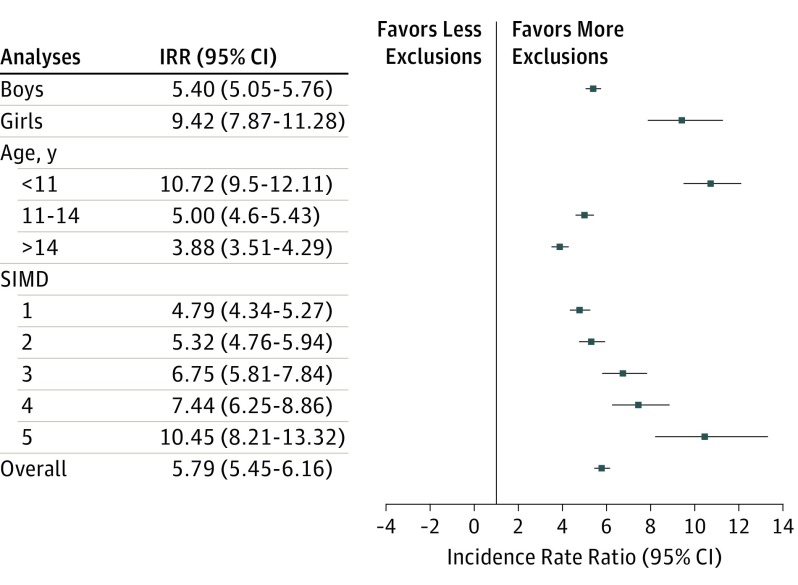
Use of ADHD medication was associated with higher numbers of exclusions from school in univariate (incidence rate ratio [IRR], 10.30; 95% CI, 9.73-10.90) analysis and adjusted for sociodemographic and maternity confounders; adjustment for comorbid conditions attenuated the association, but it remained (IRR, 5.82; 95% CI, 5.47-6.18; and IRR, 5.79; 95% CI, 5.45-6.16, respectively). There were significant interactions with sex (χ2 = 57.52; P < .001), age (χ2 = 286.98; P < .001), and deprivation (χ2 = 149.07; P < .001). The association was stronger in girls and affluent areas and decreased with age (Figure 1). Among children not receiving ADHD medication, 10 569 (6.7%) vs 1578 (1.2%) in the most and least deprived quintiles, respectively, were excluded. Among treated children, 780 (33.3%) vs 124 (17.4%) in the most and least deprived quintiles, respectively, were excluded.
Figure 1. Associations Between Attention-Deficit/Hyperactivity Disorder (ADHD) and School Exclusions by Sex, Age, and Area Deprivation Subgroup.
Outcomes were adjusted for age, sex, deprivation quintile and ethnic group, maternal age, maternal smoking, parity, mode of delivery, gestational age at delivery, sex- and gestation-specific birthweight centile, and comorbid conditions (ie, diabetes, asthma, epilepsy, and depression). IRR indicates incidence rate ratio; SIMD, Scottish Index of Multiple Deprivation: 1, most deprived; 5, least deprived.
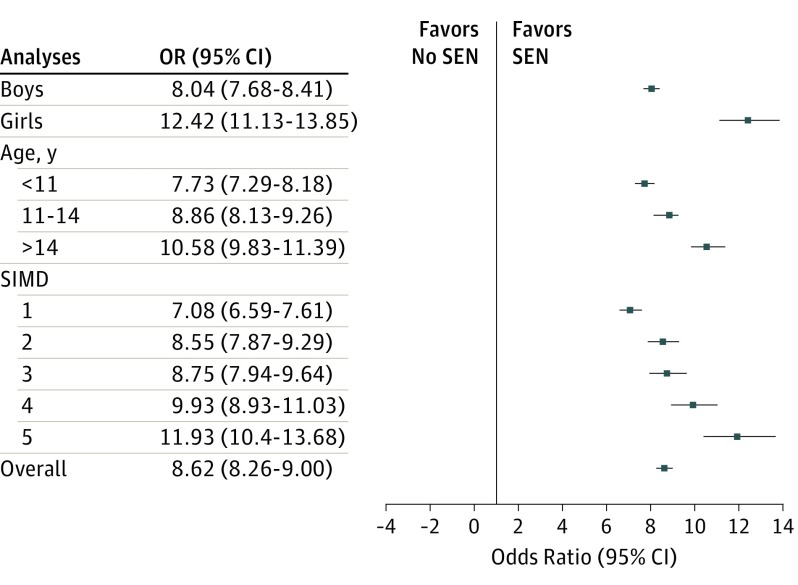
Children receiving ADHD medication had a higher risk of special educational needs on univariate analysis (odds ratio [OR], 12.38; 95% CI, 11.91-12.86). The association was attenuated slightly but remained strong after adjusting for socioeconomic and maternity (OR, 8.77; 95% CI, 8.40-9.15) and comorbid conditions (OR, 8.62; 95% CI, 8.26-9.00) confounders. There were significant interactions with sex (χ2 = 72.63; P < .001), age (χ2 = 53.27; P < .001), and deprivation (χ2 = 108.95; P < .001). The association between treated ADHD and special educational needs increased with age and was stronger in girls and less deprived children (Figure 2). Among children not treated for ADHD, 32 461 (18.9%) in the most deprived quintile had special educational needs compared with 14 185 (10.1%) in the least-deprived quintile. Among children receiving ADHD medication, 1841 (76.9%) in the most deprived quintile had special educational needs compared with 535 (70.8%) in the least-deprived quintile.
Figure 2. Association Between Attention-Deficit/Hyperactivity Disorder (ADHD) and Special Educational Needs by Sex, Age, and Deprivation Subgroup.
Outcomes were adjusted for age, sex, deprivation quintile and ethnic group, maternal age, maternal smoking, parity, mode of delivery, gestational age at delivery, sex- and gestation-specific birthweight centile, and comorbid conditions (ie, diabetes, asthma, epilepsy, and depression). OR indicates odds ratio; SEN, special educational need; SIMD, Scottish Index of Multiple Deprivation: 1, most deprived; 5, least deprived.
Treated ADHD was associated with all types of special educational needs: mental health (fully adjusted OR, 52.85; 95% CI, 45.73-61.08); social, emotional, and behavioral (fully adjusted OR, 19.97; 95% CI, 18.95-21.05); autistic spectrum disorder (fully adjusted OR, 13.72; 95% CI, 12.61-14.92); learning disability (fully adjusted OR, 8.10; 95% CI, 7.47-8.78); physical health (fully adjusted OR, 6.97; 95% CI, 6.03-8.06); physical or motor impairment (fully adjusted OR, 6.28; 95% CI, 5.42-7.28); learning difficulty (fully adjusted OR, 5.44; 95% CI, 5.12-5.79); communication problems (fully adjusted OR, 4.78; 95% CI, 4.26-5.36); and sensory impairment (fully adjusted OR, 3.62; 95% CI, 2.93-4.46).
The subgroup analyses of academic attainment included 139 205 children. Those taking ADHD medication were at higher risk of low academic attainment (Table 3). There was a significant interaction with sex (χ2 = 13.9; P < .001); the association with poor attainment was stronger among girls (Table 3). The association remained after adjustment for absenteeism (fully adjusted OR, 4.03; 95% CI, 3.56-4.55) and when children with special educational needs were omitted (fully adjusted OR, 2.60; 95% CI, 2.19-3.08).
Table 3. Association Between ADHD Medication and Academic Attainment and Leaver Status.
| Characteristic | OR (95% CI) | ||
|---|---|---|---|
| Univariate | Multivariablea | Multivariableb | |
| Poorer Academic Attainment | |||
| Overall | 6.53 (5.90-7.22) | 3.45 (3.08-3.86) | 3.35 (3.00-3.75) |
| Boys | 5.58 (4.99-6.24) | 3.38 (2.99-3.82) | 3.28 (2.90-3.71) |
| Girls | 8.46 (6.58-10.88) | 5.38 (4.06-7.12) | 5.16 (3.90-6.84) |
| Deprivation quintilec | |||
| 1 (most deprived) | 5.40 (4.48-6.51) | 3.49 (2.83-4.30) | 3.40 (2.76-4.20) |
| 2 | 5.30 (4.36-6.44) | 3.13 (2.52-3.88) | 3.03 (2.45-3.76) |
| 3 | 6.57 (5.21-8.29) | 3.65 (2.84-4.69) | 3.57 (2.78-4.59) |
| 4 | 8.26 (6.26-10.90) | 4.55 (3.37-6.16) | 4.41 (3.26-5.97) |
| 5 (least deprived) | 5.93 (4.37-8.05) | 2.45 (1.75-3.43) | 2.36 (1.69-3.30) |
| Not in Employment, Education, or Training 6 mo After Leaving School | |||
| Overall | 2.58 (2.35-2.84) | 1.42 (1.28-1.57) | 1.39 (1.25-1.53) |
| Boys | 2.22 (2.00-2.47) | 1.43 (1.28-1.60) | 1.40 (1.26-1.57) |
| Girls | 3.17 (2.50-4.01) | 1.66 (1.30-2.12) | 1.59 (1.24-2.03) |
| Deprivation quintileb | |||
| 1 (most deprived) | 1.90 (1.62-2.23) | 1.31 (1.11-1.54) | 1.30 (1.10-1.53) |
| 2 | 1.99 (1.65-2.41) | 1.21 (0.99-1.47) | 1.18 (0.96-1.43) |
| 3 | 2.47 (1.96-3.13) | 1.43 (1.12-1.83) | 1.40 (1.09-1.78) |
| 4 | 3.78 (2.88-4.95) | 2.15 (1.62-2.85) | 2.06 (1.55-2.74) |
| 5 (least deprived) | 3.70 (2.62-5.23) | 2.07 (1.44-2.99) | 2.01 (1.40-2.90) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; OR, odds ratio.
Adjusted for age, sex, deprivation quintile and ethnic group, maternal age, maternal smoking, parity, mode of delivery, gestational age at delivery, and sex- and gestation-specific birthweight centile (as appropriate).
Also adjusted for comorbid conditions (ie, diabetes, asthma, epilepsy, and depression).
Determined using the Scottish Index of Multiple Deprivation.
In the subgroup analyses of 217 924 children, children with treated ADHD were at higher risk of unemployment (Table 3). There was a significant interaction with sex (χ2 = 7.25; P = .007), with the association being stronger in girls (Table 3). There was also a significant interaction with deprivation (χ2 = 28.3; P < .001) whereby the association was strongest among less deprived children. Again, this association was due to higher baseline unemployment among the most deprived children (7936 [16.8%] vs 2003 [4.9%]). Among children treated for ADHD, unemployment was still higher in the most deprived quintile (213 [27.7%] vs 39 [16.1%]). Children with treated ADHD remained at higher risk of unemployment after adjusting for absenteeism (fully adjusted OR, 1.42; 95% CI, 1.27-1.58) and after omitting children with special educational needs (fully adjusted OR, 1.28; 95% CI, 1.08-1.52).
Linkage to hospital records provided 2.92 million person-years of follow-up, with 157 475 pupils experiencing a total of 306 416 hospital admissions. Treatment for ADHD was associated with an increased risk of any hospital admission on univariate analysis (hazard ratio [HR], 1.47; 95% CI, 1.40-1.54) and following adjustment for sociodemographic and maternity confounders (HR, 1.33; 95% CI, 1.27-1.39) and other comorbid conditions (HR, 1.25; 95% CI, 1.19-1.31). There was a significant interaction with sex (P < .001), with the association being stronger in girls (fully adjusted HR, 1.49; 95% CI, 1.33-1.65) than boys (fully adjusted HR, 1.24; 95% CI, 1.18-1.31). The most common reason for hospital admission was injury, which accounted for 41 765 (13.6%) admissions. Treatment for ADHD was associated with an increased risk of hospital admission for injury on univariate analysis (HR, 2.06; 95% CI, 1.90-2.24) and following adjustment for sociodemographic and maternity confounders (HR, 1.60; 95% CI, 1.47-1.74) and other comorbid conditions (HR, 1.52; 95% CI, 1.40-1.65). Again, there was an interaction with sex (P = .02), with the association with hospital admission for injury being stronger in girls (fully adjusted HR, 1.83; 95% CI, 1.46-2.29) than boys (fully adjusted HR, 1.49; 95% CI, 1.37-1.63).
Discussion
Children treated for ADHD had worse educational outcomes: they left school at an earlier age, took more unauthorized absences, were more likely to be excluded from school, were at higher risk of special educational needs, performed more poorly in examinations, and were more likely to be unemployed after leaving school. Academic attainment was worse even among children treated for ADHD who did not have special educational needs, and the worse academic attainment and higher risk of employment were not simply due to higher absenteeism. These children also had worse health outcomes, being more likely to be hospitalized overall and specifically as a result of injury. All of these associations were independent of confounders relating to socioeconomic status, pregnancy, delivery, and comorbid conditions.
Although girls were less likely to be treated for ADHD, those who were treated fared worse than treated boys in association with exclusion, special educational needs, academic attainment, unemployment, and hospitalization. A previous review concluded that girls are more likely to present with inattention and boys with hyperactivity; girls have lower self-efficacy, poorer coping strategies, and higher rates of depression and anxiety.19 Girls are both less likely to be referred for treatment and less likely to use prescribed medication.19,20 The relative effect of treated ADHD on education was less in deprived areas. However, this finding was due to unaffected children living in deprived areas already having worse outcomes. Most notably, unemployment was comparable among affluent children treated for ADHD and deprived children not receiving ADHD medication (39 [16.1%] vs 7936 [16.8%]).
To our knowledge, this is the first nationwide study to compare educational outcomes of children with treated ADHD with their unaffected peers; with 7413 children treated for ADHD, this investigation is more than 20 times larger than previous studies reporting similar educational outcomes.21,22,23,24 The only previous national study of health outcomes that we are aware of focused on severe ADHD ascertained from psychiatric hospitalizations; linkage of 1.9 million Danish births to death records revealed an all-cause mortality ratio of 2.07, but no other health outcomes were studied.12 Smaller studies have reported higher rates of injury among children with ADHD.25,26,27
Strengths and Limitations
Ours was a large, nonselective study that included children across the entirety of Scotland. Because children were identified from school rather than health records, inclusion was not restricted to more severe cases. We were able to adjust for a range of potential confounders: sociodemographic, maternity, and comorbidities. However, as with any observational study, there is always a potential for residual confounding. The large size of the study provided sufficient power to test for statistical interactions and undertake subgroup analyses where appropriate. We were able to analyze a wide range of outcomes in the same study covering both the educational and health sectors. In Scotland, the childhood prevalence of ADHD is approximately 5%; however, the proportion diagnosed and treated ranges from 0.2% to 1.2% by region.28 Our study prevalence of 1% is consistent with these figures. However, the published figures suggest that 70% to 96% of Scottish children with ADHD do not receive medication. Therefore, our exposed group will have comprised children with more severe forms of ADHD, and the comparison group will have included some less severe and undiagnosed cases.
The study included only local authority–maintained schools; this should not have affected our findings since only 5% of children in Scotland attend private schools. According to the 2011 Scottish Census, 11% of Scottish residents aged 5 to 19 years were born outside of Scotland; this percentage is consistent with the 12.3% of Scottish children who could not be linked to Scottish maternity records in our study. The prevalence of ADHD medication was 0.86% in pupils who could not be linked and 0.97% in those who could be linked, suggesting that bias is unlikely. The study used existing administrative databases established for other purposes. However, these databases undergo regular quality assurance checks. The linkage of education and health records relied on probabilistic matching. A previous validation study demonstrated that this method was 99% accurate for singletons.22
Conclusions
Children treated for ADHD had worse outcomes in association with both education and health. Girls were less likely to be treated for ADHD, but those who were treated had worse outcomes than boys. The magnitude of the effect of ADHD was less among children living in deprived areas because children in these areas already had worse educational and health outcomes irrespective of whether they had ADHD.
References
- 1.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):-. [DOI] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Study 2013 Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991;148(5):564-577. [DOI] [PubMed] [Google Scholar]
- 4.Pliszka SR. Comorbidity of attention-deficit/hyperactivity disorder with psychiatric disorder: an overview. J Clin Psychiatry. 1998;59(suppl 7):50-58. [PubMed] [Google Scholar]
- 5.Karande S, Kulkarni M. Poor school performance. Indian J Pediatr. 2005;72(11):961-967. [DOI] [PubMed] [Google Scholar]
- 6.Guevara J, Lozano P, Wickizer T, Mell L, Gephart H. Utilization and cost of health care services for children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108(1):71-78. [DOI] [PubMed] [Google Scholar]
- 7.Birnbaum HG, Kessler RC, Lowe SW, et al. Costs of attention deficit-hyperactivity disorder (ADHD) in the US: excess costs of persons with ADHD and their family members in 2000. Curr Med Res Opin. 2005;21(2):195-206. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez A, Järvelin M-R, Obel C, et al. Do inattention and hyperactivity symptoms equal scholastic impairment? evidence from three European cohorts. BMC Public Health. 2007;7(1):327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barry TD, Lyman RD, Klinger LG. Academic underachievement and attention-deficit/hyperactivity disorder: the negative impact of symptom severity on school performance. J Sch Psychol. 2002;40(3):259-283. [Google Scholar]
- 10.McConaughy SH, Volpe RJ, Antshel KM, Gordon M, Eiraldi RB. Academic and social impairments of elementary school children with attention deficit hyperactivity disorder. School Psych Rev. 2011;40(2):200-225. [Google Scholar]
- 11.Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry. 2005;57(11):1336-1346. [DOI] [PubMed] [Google Scholar]
- 12.Dalsgaard S, Nielsen HS, Simonsen M. Consequences of ADHD medication use for children’s outcomes. J Health Econ. 2014;37:137-151. [DOI] [PubMed] [Google Scholar]
- 13.Beau-Lejdstrom R, Douglas I, Evans SJW, Smeeth L. Latest trends in ADHD drug prescribing patterns in children in the UK: prevalence, incidence and persistence. BMJ Open. 2016;6(6):e010508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sayal K, Ford T, Goodman R. Trends in recognition of and service use for attention-deficit hyperactivity disorder in Britain, 1999-2004. Psychiatr Serv. 2010;61(8):803-810. [DOI] [PubMed] [Google Scholar]
- 15.Safer DJ, Zito JM, Fine EM. Increased methylphenidate usage for attention deficit disorder in the 1990s. Pediatrics. 1996;98(6, pt 1):1084-1088. [PubMed] [Google Scholar]
- 16.National Institute for Health and Clinical Excellence. Attention deficit hyperactivity disorder (ADHD): clinical guideline [CG72]. www.nice.org.uk/guidance/cg72. Updated February 2016. Accessed March 29, 2017.
- 17.Wolraich M, Brown L, Brown RT, et al. ; Subcommittee on Attention-Deficit/Hyperactivity Disorder; Steering Committee on Quality Improvement and Management . ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007-1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wood R, Clark D, King A, Mackay D, Pell J. Novel cross-sectoral linkage of routine health and education data at an all-Scotland level: a feasibility study. Lancet. 2013;382:S10. [Google Scholar]
- 19.Rucklidge JJ. Gender differences in attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2010;33(2):357-373. [DOI] [PubMed] [Google Scholar]
- 20.Lillemoen PK, Kjosavik SR, Hunskår S, Ruths S. Prescriptions for ADHD medication, 2004-08. Tidsskr Nor Laegeforen. 2012;132(16):1856-1860. [DOI] [PubMed] [Google Scholar]
- 21.Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Long-term school outcomes for children with attention-deficit/hyperactivity disorder: a population-based perspective. J Dev Behav Pediatr. 2007;28(4):265-273. [DOI] [PubMed] [Google Scholar]
- 22.Wu S-Y, Gau SS-F. Correlates for academic performance and school functioning among youths with and without persistent attention-deficit/hyperactivity disorder. Res Dev Disabil. 2013;34(1):505-515. [DOI] [PubMed] [Google Scholar]
- 23.Kent KM, Pelham WE Jr, Molina BS, et al. The academic experience of male high school students with ADHD. J Abnorm Child Psychol. 2011;39(3):451-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuriyan AB, Pelham WE Jr, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41(1):27-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hurtig T, Ebeling H, Jokelainen J, Koivumaa-Honkanen H, Taanila A. The association between hospital-treated injuries and ADHD symptoms in childhood and adolescence: a follow-up study in the Northern Finland Birth Cohort, 1986. J Atten Disord. 2016;20(1):3-10. [DOI] [PubMed] [Google Scholar]
- 26.van den Ban E, Souverein P, Meijer W, et al. Association between ADHD drug use and injuries among children and adolescents. Eur Child Adolesc Psychiatry. 2014;23(2):95-102. [DOI] [PubMed] [Google Scholar]
- 27.Pastor PN, Reuben CA. Identified attention-deficit/hyperactivity disorder and medically attended, nonfatal injuries: US school-age children, 1997-2002. Ambul Pediatr. 2006;6(1):38-44. [DOI] [PubMed] [Google Scholar]
- 28.Healthcare Improvement Scotland. Attention deficit and hyperkinetic disorders: services over Scotland; final report. Edinburgh, UK: NHS Scotland; 2012. http://www.healthcareimprovementscotland.org/our_work/mental_health/adhd_services_over_scotland/stage_3_adhd_final_report.aspx. Accessed 6 December 2016. [Google Scholar]