Introduction
Heterotopic ossification, a benign condition, results from normal lamellar bone formation in an abnormal location. Although the pathogenesis of this condition remains largely unknown, several causative factors have been identified since its description in children with myositis ossificans progressiva in 1692 by Patin1. The most commonly observed cause is trauma: either a single episode of severe trauma or repeated microtraumas2, 3. Although it is a self limiting condition which often resolves spontaneously, it can cause significant morbidity in the form of significant restriction in movements, especially when it occurs close to joints3, 4.
Heterotopic ossification commonly occurs around the hip joint, where it most often involves the abductor muscles. Involvement of the iliopsoas is uncommon, very few cases having been reported3, 4, 5, 6. All previously reported cases have been due to trauma or intramuscular hemorrhage. Moreover, few of these reported cases involved the psoas without involvement of the hip joint; those that did had a radically different presentation7, 8. Some recent reports have documented involvement of the psoas muscle after posterior spinal fusion surgery, especially when bone morphogenetic proteins have been used9. We present here a case of heterotopic ossification of the iliopsoas muscle without antecedent trauma or any other known cause. We further discuss and review published reports on this subject.
Case report
A 28‐year‐old man presented to our outpatient department with a history of gradual, progressive and painless restriction of movement of his left hip over the previous 10 months. There was no history of trauma, surgery or bleeding disorder. However, the patient described an acute febrile illness that had started 7–10 days prior to the onset of his local hip symptoms, which had consisted of pain and stiffness during the initial 2–3 weeks, following which painless stiffness of the hip joint progressively replaced these symptoms. His febrile illness, which ran a benign course over 10–15 days, had been managed at a local primary care centre on an outpatient basis. Further details of his treatment and investigations were not available, however the patient claimed to have taken a course of oral antibiotics. Despite increasing stiffness of his hip joint the patient continued to work, which at times involved heavy labor.
Local clinical examination revealed fullness in the left femoral triangle and a palpable, well‐defined, hard, bony mass in the femoral triangle, extending from the superior pubic ramus to the medial subtrochanteric level of the femur. Although the neurovascular bundle was displaced medial to the mass, there was no distal neurovascular deficit. The patient had significant restriction of hip flexion, internal rotation and adduction and wasting of his hip and thigh musculature. Radiological evaluation revealed an ossified mass lying anterior to the hip joint (Fig. 1) and extending from the level of the superior pubic ramus to the lesser trochanter. A CT scan revealed a well‐defined, trabeculated mass with peripheral mature lamellar bone and central immature bone (Fig. 2). The ossified mass measured approximately 16 cm in length.
Figure 1.
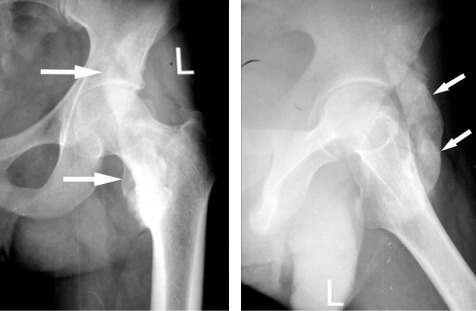
Anteroposterior and lateral radiographs of the left hip showing an ossified mass (arrows) extending from the level of superior pubic ramus to the lesser trochanter and lying anterior to the hip joint.
Figure 2.
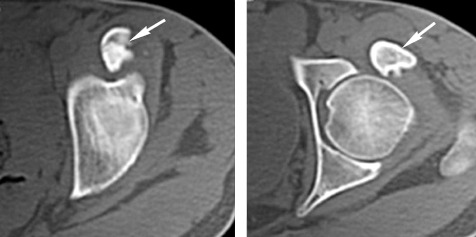
CT scan showing a well defined, trabeculated mass, with peripheral mature lamellar bone and immature central bone (arrows).
We discussed the treatment options with the patient after making a diagnosis of myositis ossificans, explaining the need for surgical excision and the appropriate timing of surgery. We prescribed indomethacin 75 mg orally in sustained release form. Having observed no change in the mass during serial checks over 4 months, we admitted the patient for open surgical excision of the ossified mass14 months from the onset of symptoms.
We placed the patient in a supine position with a sand bag under the ipsilateral hip. The skin incision curved over the iliac crest from the tuberosity to the anterior superior iliac spine, and then vertically distally for 8 cm (Fig. 3). We carried out deep dissection medial to the sartorius, which we retracted laterally. We then mobilized and retracted the rectus femoris laterally, which exposed the entire length of the iliopsoas tendon with the lower portion of the iliacus muscle. We could then feel the mass under the iliacus; at this stage, we identified the femoral nerve overlying the iliacus. We split the iliacus longitudinally over the mass and retracted it to completely expose the ossified mass (Fig. 4). We carefully isolated the 14 cm long bony mass with minimal bleeding, osteotomized it at each end, stripped it from the adherent soft tissue and removed it (Fig. 5). Intra‐operatively, we confirmed a full passive hip range of movement; achieved local homeostasis and closed the incision over a suction drain. Prophylactic indomethacin was started postoperatively and continued for 6 months. Histopathological examination of the excised mass confirmed the diagnosis of heterotopic ossification and revealed the zoning phenomenon that is pathognomonic of this condition. Postoperative radiographs confirmed that the entire mass had been excised (Fig. 6). The patient started a regimen of active and active assisted range of hip movements from the second postoperative day. He was able to sit cross‐legged and even squat by the fourth post‐operative day; he retained the range of motion achieved at surgery till his last follow‐up at 24 months.
Figure 3.

Photograph showing the surgical incision used.
Figure 4.
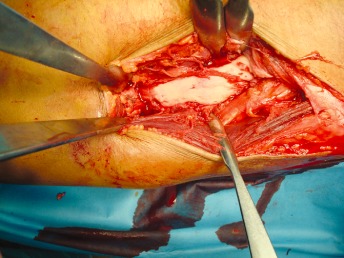
Photograph showing the mass after retracting both the sartorius and rectus muscles laterally.
Figure 5.

Photograph showing the excised mass of about 14 cm.
Figure 6.

Postoperative anteroposterior and lateral radiographs confirming excision of the mass.
Discussion
Heterotopic ossification around the hip joint commonly involves the abductor musculature; involvement of the iliopsoas has rarely been reported. Despite recognition of this entity for over 400 years, its exact pathogenesis remains elusive. Although trauma is the most frequently implicated cause, atraumatic causes are responsible in a significant number of cases6, 8, 10, 11. Heterotopic ossification around the hip joint frequently occurs following fractures/fracture‐dislocations or open surgical procedures12, 13, 14, 15, 16. Rare cases have been reported following hemorrhage into the muscle compartment in hemophiliacs5. Moreover, repeated microtrauma, for example in soccer players, can also lead to ossification at sites of injury2. In the present case, despite our best efforts, we were unable to establish a cause due to late presentation. However, occurrence of a febrile illness one week prior to the onset of symptoms may be relevant. Several febrile illnesses have reportedly caused bleeding abnormalities due to thrombocytopenia which, if sufficiently severe, can cause spontaneous intramuscular bleeding17. Furthermore, several antibiotics can cause a tendency to spontaneous bleeding, either due to a direct effect on platelet numbers or to an indirect effect on amounts of coagulation factor by inducing vitamin K deficiency due to changes in gut flora17, 18. It is possible that such intramuscular bleeding could present in a manner similar to the present case5, 19. Although we can only speculate about the inciting event, continuing vigorous physical activity and lack of adequate rest would definitely have contributed to the development of heterotopic ossification in the present case. Michelsson et al. have demonstrated that forcible manipulation induces heterotopic bone formation in rabbits20, 21. Gentle physiotherapy below the pain threshold, for example by means of continuous passive motion, maintains and even improves joint mobility and reduces spasticity, without causing bone formation22.
The principal disability in non‐progressive heterotopic ossification is usually mechanical and characterized by painless restriction of joint movements, the degree of limitation being dependent upon the amount and site of ossification. Patients usually regain a full active range of movement within a few days of excision of myositis ossificans masses3, 4.
The earliest radiologic change, that of a soft tissue mass, is apparent within 1 to 2 weeks and may be accompanied by faint periosteal new bone formation. By 3–4 weeks, floccular calcification appears in the soft tissue mass. By 6–8 weeks, a lacy pattern of new bone formation forms in the peripheral zone. By 5 to 6 months, the mass shrinks and maturation is complete8, 10. Three phase bone scintigraphy, the most sensitive investigation for early diagnosis of heterotopic ossification, becomes positive at 2–4 weeks23. Scintigraphy can further be used for follow up and to assess the maturity of the ossification process23. Although radiography, CT scan and MRI have low specificity in the early stages, in later stages these investigations can be diagnostic by showing normal lamellar bony architecture within a bony mass10, 11. Ultrasonography is also useful for early detection of bone formation, having high sensitivity and specificity for the early diagnosis of heterotopic ossifications 1 week after total hip arthroplasty24. In the present case, which presented 10 months after the onset of symptoms, we opted for routine radiography along with CT scan which showed clear lamellar bone with a cortex and medullary cavity.
The management of heterotopic ossifications begins with preventive measures, which include meticulous dissection during surgery, appropriate immobilization and physical therapy, indomethacin, and prophylactic radiation therapy22, 25, 26. Treatment for established heterotopic ossification includes appropriate immobilization for immature bone and physical therapy for a mature mass. Although bisphosphonates and radiation therapy have been used for treatment, their therapeutic efficacy is questionable and bisphosphonates can lead to a rebound effect on cessation of drug treatment27, 28. Surgery is reserved for residual restriction in movements after maturation of bone. The timing of surgery, intra‐operative dissection and measures taken to minimize recurrence all determine the ultimate outcome.
One issue of concern in non‐traumatic cases is that the differential diagnosis includes malignant conditions like osteosarcoma and chondrosarcoma, and other processes like infection, calcified psoas abscesses and hematomas6. Establishment of the diagnosis can involve unnecessary biopsies and premature surgical intervention. However, the characteristic radiological findings on X‐ray and CT scans of a well‐defined trabeculation pattern and mature peripheral lamellar bone should clarify the diagnosis and allow planning of an appropriately timed surgical intervention.
The principal indication for surgical excision is restriction of movement. Because of high recurrence rates, surgical excision has to be appropriately timed, the ideal time being after clinical and radiological maturation of the lesion; this ensures the best clinical outcomes3, 6. Maturation of a mass can take up to 6–12 months. It is important to delay surgical excision of myositis ossificans around the hip because premature surgical intervention can lead to recurrence3, 29.
Access to the Iliopsoas can be either through an ilioinguinal or iliofemoral approach. Before surgery, careful examination to localize the vascular structures is important, as these are usually displaced and therefore at increased risk. We also emphasize the importance of intra‐operative identification of the femoral nerve overlying the iliacus to reduce the risk of nerve injury due to distorted anatomy.
Attention to several intraoperative details reduces the risk of recurrence of the mass. Dissection in the intermuscular planes avoids formation of intramuscular hematomas that might lead to recurrence. Minimal periosteal stripping and achievement of good homeostasis before closure also reduce the incidence of local recurrence3, 29. Chemical prophylaxis with indomethacin further reduces the recurrence and incidence of myositis ossificans. Low dose radiotherapy can be used as an adjuvant, but the timing of surgery remains the most important factor in reducing recurrences.
Heterotopic ossification of the iliopsoas can develop without antecedent trauma; excision is possible via a modified anterior approach to the hip. Preoperative planning, surgical timing and meticulous technique, combined with post‐operative adjuvants like indomethacin, ensure a good result for treating this mechanical block to motion.
Disclosure: We received no financial support for presenting this report.
References
- 1. Geschickter CF, Maseritz IH. Myositis ossificans. J Bone Joint Surg Am, 1938, 20: 661–674. [Google Scholar]
- 2. Cetin C, Sekir U, Yildiz Y, et al Chronic groin pain in an amateur soccer player. Br J Sports Med, 2004, 38: 223–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCulloch PC, Bush‐Joseph CA. Massive heterotopic ossification complicating iliopsoas tendon lengthening: a case report. Am J Sports Med, 2006, 34: 2022–2025. [DOI] [PubMed] [Google Scholar]
- 4. Thorseth K. A case of traumatic myositis ossificans in the iliopsoas muscle. Acta Orthop Scand, 1968, 39: 73–75. [DOI] [PubMed] [Google Scholar]
- 5. Balkan C, Kavakli K, Karapinar D. Iliopsoas haemorrhage in patients with haemophilia: results from one centre. Haemophilia, 2005, 11: 463–467. [DOI] [PubMed] [Google Scholar]
- 6. Merchan EC, Sanchez‐Herrera S, Valdazo DA. Circumscribed myositis ossificans. Report of nine cases without history of injury. Acta Orthop Belg, 1993, 59: 273–277. [PubMed] [Google Scholar]
- 7. Kim SW, Choi JH. Myositis ossificans in psoas muscle after lumbar spine fracture. Spine, 2009, 34: E367–E370. [DOI] [PubMed] [Google Scholar]
- 8. Choi MN, Lee GK, Suh KJ. Myositis ossificans of the psoas muscle after compression fracture of lumbar spine: CT and MR imaging findings. J Korean Soc Radiol, 2010, 63: 75–78. [Google Scholar]
- 9. Shah RK, Moncayo VM, Smitson RD, et al Recombinant human bone morphogenetic protein 2‐induced heterotopic ossification of the retroperitoneum, psoas muscle, pelvis and abdominal wall following lumbar spinal fusion. Skeletal Radiol, 2010, 39: 501–504. [DOI] [PubMed] [Google Scholar]
- 10. Parikh J, Hyare H, Saifuddin A. The imaging features of post‐traumatic myositis ossificans, with emphasis on MRI. Clin Radiol, 2002, 57: 1058–1066. [DOI] [PubMed] [Google Scholar]
- 11. Sirvanci M, Ganiyusufoglu AK, Karaman K, et al Myositis ossificans of psoas muscle: magnetic resonance imaging findings. Acta Radiol, 2004, 45: 523–525. [DOI] [PubMed] [Google Scholar]
- 12. Dwyer AJ, John B, Singh SA, et al Complications after posterior dislocation of the hip. Int Orthop, 2006, 30: 224–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Guo JJ, Tang N, Yang HL, et al Impact of surgical approach on postoperative heterotopic ossification and avascular necrosis in femoral head fractures: a systematic review. Int Orthop, 2010, 34: 319–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ahrengart L, Lindgren U. Heterotopic bone after hip arthroplasty. Defining the patient at risk. Clin Orthop Relat Res, 1993, 293: 153–159. [PubMed] [Google Scholar]
- 15. Pennal GF, Davidson J, Garside H, et al Results of treatment of acetabular fractures. Clin Orthop Relat Res, 1980, 151: 115–123. [PubMed] [Google Scholar]
- 16. Matta JM, Mehne DK, Roffi R. Fractures of the acetabulum. Early results of a prospective study. Clin Orthop Relat Res, 1986, 205: 241–250. [PubMed] [Google Scholar]
- 17. Konkle BA. Disorders of platelets and vessel wall In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison's Principles of Internal Medicine, 17th edn New York: McGraw‐Hill, 2008; 718–724. [Google Scholar]
- 18. Conly J, Stein K. Reduction of vitamin K2 concentrations in human liver associated with the use of broad spectrum antimicrobials. Clin Invest Med, 1994, 17: 531–539. [PubMed] [Google Scholar]
- 19. Onodera M, Fujino Y, Inoue Y, et al Hematoma of the iliopsoas muscle due to thrombocytopenia resulting from the administration of a third‐generation cephalosporin. Ann Hematol, 2010, 89: 825–826. [DOI] [PubMed] [Google Scholar]
- 20. Michelsson JE, Rauschning W. Pathogenesis of experimental heterotopic bone formation following temporary forcible exercising of immobilized limbs. Clin Orthop Relat Res, 1983, 176: 265–272. [PubMed] [Google Scholar]
- 21. Michelsson JE, Granroth G, Andersson LC. Myositis ossificans following forcible manipulation of the leg. A rabbit model for the study of heterotopic bone formation. J Bone Joint Surg Am, 1980, 62: 811–815. [PubMed] [Google Scholar]
- 22. Linan E, O'Dell MW, Pierce JM. Continuous passive motion in the management of heterotopic ossification in a brain injured patient. Am J Phys Med Rehabil, 2001, 80: 614–617. [DOI] [PubMed] [Google Scholar]
- 23. Freed JH, Hahn H, Menter R, et al The use of the three‐phase bone scan in the early diagnosis of heterotopic ossification (HO) and in the evaluation of Didronel therapy. Paraplegia, 1982, 20: 208–216. [DOI] [PubMed] [Google Scholar]
- 24. Popken F, König DP, Tantow M, et al Possibility of sonographic early diagnosis of heterotopic ossifications after total hip‐replacement. Unfallchirurg, 2003, 106: 28–31. [DOI] [PubMed] [Google Scholar]
- 25. Banovac K, Williams JM, Patrick LD, et al Prevention of heterotopic ossification after spinal cord injury with indomethacin. Spinal Cord, 2001, 39: 370–374. [DOI] [PubMed] [Google Scholar]
- 26. Esenwein SA, Sell S, Herr G, et al Effects of single‐dose versus fractionated irradiation on the suppression of heterotopic bone formation—an animal model‐based follow‐up study in rats. Arch Orthop Trauma Surg, 2000, 120: 575–581. [DOI] [PubMed] [Google Scholar]
- 27. Banovac K. The effect of etidronate on late development of heterotopic ossification after spinal cord injury. J Spinal Cord Med, 2000, 23: 40–44. [DOI] [PubMed] [Google Scholar]
- 28. Sautter‐Bihl ML, Liebermeister E, Nanassy A. Radiotherapy as a local treatment option for heterotopic ossifications in patients with spinal cord injury. Spinal Cord, 2000, 38: 33–36. [DOI] [PubMed] [Google Scholar]
- 29. Specht LM, Gupta S, Egol KA, et al Heterotopic ossification of the quadriceps following distal femoral traction: a report of three cases and a review of the literature. J Orthop Trauma, 2004, 18: 241–246. [DOI] [PubMed] [Google Scholar]


