Abstract
Objective: To compare anterior and posterior approaches for treating cervical spondylotic myelopathy (CSM) involving more than two levels, especially in regard to quality of life and cost effectiveness.
Methods: The authors studied 116 CSM patients who underwent decompressive surgery by either an anterior or a posterior approach with instrumentation. In the anterior group, 1–3 levels subtotal vertebrectomy was followed by bone graft and Orion anterior cervical locking plate fixation. In the posterior group, multilevel laminectomy with posterior screw‐rod fixation was performed. Follow‐up, which included radiographic assessment, clinical examination and documentation of length of any hospitalization and cost and incidence of complications, was performed 1 day before discharge, 6 months after leaving hospital, and at final follow‐up.
Results: Both groups had improved clinical outcomes. The anterior group showed greater satisfaction but lower visual analog scale scores than the posterior group, whereas SF‐36 emotional role and mental health scores were higher in the anterior group. There was no marked difference between the two groups in length of hospitalization and most of the costs of treating CSM, however treatment and examination fees were significantly higher in the posterior group.
Conclusions: Both anterior and posterior decompressions (with instrumentation) are effective procedures for improving the neurological outcomes of patients with CSM. However, although the two approaches have similar health care costs, anterior cervical corpectomy (with instrumentation) seems to be subjectively assessed by patients as better.
Keywords: Cervical spondylosis, Cost analysis, Decompression, Operative, Surgical procedures
Introduction
Cervical spondylotic myelopathy (CSM) is the commonest type of spinal cord dysfunction in patients older than 55 years and the commonest cause of acquired spastic paraparesis in the middle and later years of life, causing great disability to human health 1 . Numerous clinical and long‐term observations have shown that CSM is almost always characterized by progressive deterioration 2 , therefore it is essential to implement timely surgery when treating CSM in order to preserve or recover cervical spinal cord function.
Cervical spondylotic myelopathy can be treated by a variety of anterior, posterior, and combined surgical approaches 3 , 4 , 5 . There is continuing controversy about how to choose the optimal surgical strategy for each individual case. For CSM involving more than two vertebral body levels, there is so far no definitive evidence as to which surgical approach is better 6 . Especially where there is associated developmental stenosis of the cervical spinal canal, different surgeons advocate very different surgical approaches.
The aim of this retrospective database study was to compare the efficacy of multilevel anterior and posterior decompressive surgery of the cervical spine with instrumentation, focusing in particular on the patients’ subjective evaluations and analysis of the costs involved.
Materials and methods
Patient data
Criteria for patient inclusion were as follows: (i) clinical manifestations of cervical spinal cord compression, including clumsiness or numbness in the hands resulting in worsening of handwriting or difficulty in grasping or holding, limb pain, paresthesias, sensations of walking on cotton, feelings of fatigue in the chest and back; (ii) imaging findings indicating cervical spinal cord compression including straightening of cervical lordosis, protrusion of cervical disc with compression of spinal cord at the involved levels, spinal canal stenosis, and other abnormalities; (iii) disease at more than two levels treated by anterior corpectomy followed by placement of titanium surgical mesh (TSM)‐bone graft composite with/without discectomy or laminectomy followed by posterior screw‐rod fixation; and (iv) exclusion of the diagnoses of amyotrophic lateral sclerosis, spinal cord tumors, spinal cord injury, multiple peripheral neuritis, and secondary adhesive arachnoiditis.
Criteria for patient exclusion were as follows: (i) CSM involving only one or two levels; (ii) decompression by a combined approach; (iii) one or more co‐existing diseases that greatly affect outcomes; (iv) patient in a generally weakened condition; and (v) failure to attend for follow up.
Between June 2005 and January 2010, 154 patients underwent multilevel (more than two levels) decompressive surgery for CSM. According to the inclusion and exclusion criteria above, 131 patients were eligible. However, 12 patients were lost to follow‐up and 3 patients died. Thus, the eventual number of patients included in the study was 116: 71 in the anterior and 45 in the posterior group. There were 74 men (44 anterior, 30 posterior group) and 42 women (27 anterior, 15 posterior group). The patients’ ages at operation ranged from 29 to 76 years (mean 55.2 years), the difference between the anterior group (53.9 ± 10.7 years) and the posterior group (57.1 ± 10.4 years) not being significant. The interval between onset of symptoms and undergoing surgery ranged from 6 days to 10 years (mean 28.8 months), the difference between the anterior (27.6 ± 46.4 months) and the posterior group (33.5 ± 34.6 months) was not statistically significant.
In the anterior group, 5 cases had associated degenerative kyphosis, 21 ossification of the posterior longitudinal ligament, and 17 stenosis of the cervical spinal canal. The disease involved three levels in 39 cases, four in 28 cases, and five in 4 cases. In the posterior group, 33 had associated ossification of the posterior longitudinal ligament and 28 cervical spinal canal stenosis. The disease involved three levels in 15 cases, four in 24 cases, and five in 6 cases.
The selection of surgical procedure depended on two main factors: the direction from which the spinal cord was compressed and the preoperative cervical alignment. However, it is very likely that CSM patients with the same conditions were operated on via different approaches, because the surgeons involved had different policies.
Surgical technique
In the anterior group, all patients underwent corpectomy followed by placement of TSM‐bone graft composite and internal fixation. The responsible vertebrae and the two adjacent intervertebral discs were removed to expose the posterior longitudinal ligament, a trapezoidal bone groove was created, and then titanium surgical mesh‐bone graft composite (PYRAMESH titanium mesh fusion apparatus, Medtronic Sofamor Danek, Memphis, TN, USA) was placed in position. In addition, in cases with associated independent intervertebral disc pathology, discectomy was followed by placement of a cage (CSR fusion apparatus, Medtronic Sofamor Danek). Appropriate internal fixation (ORION anterior cervical locking plate system fixation, Medtronic Sofamor Danek) was used with the aim of achieving immediate stability.
In the posterior group, laminectomy followed by posterior instrumentation with a screw‐rod was performed. A bone rongeur was used to remove the target spinous processes, a suitable posterior screw‐rod system (axis posterior cervical fixation system, Medtronic Sofamor Danek) was inserted, and then the responsible laminae removed to decompress the spinal cord.
Postoperatively, diuretics and corticosteroid were routinely used for 3–5 days and external orthotics advised for 3 months. Hemostasis, antibiotics, neurotrophic and other general treatments were used as indicated. All patients were asked to desist from heavy physical activities until fusion has been established.
Follow‐up
The follow‐up times used in this study were 1 day before discharge, 6 months after discharge, and final follow up (range 12–70 months, mean 31.2 months). At these times cervical plain radiographs and CT scan or MR imaging films were taken and assessed; Japanese Orthopedic Association (JOA) scores and Visual Analogue Scale (VAS) scores of neck pain obtained; complications noted; patient satisfaction assessed (an immediate positive reply was classified as “yes”, other replies as “no”); quality of life assessed using a 36‐item short‐form health survey, SF‐36) 7 , and the cost of medical care, including total costs and the separate costs of treatment, examination, surgery, medication and instruments, calculated.
Treatment costs included expenses incurred by various clinical procedures, such as dressing changes, suture removal, nursing care, and preoperative lumbar punctures. Examination costs included expenses incurred during all clinical examinations, such as X‐rays, CT scans, MR imaging, various blood tests, and electrocardiograms. Surgical costs were the cost of the actual surgery, instrument costs the cost of instruments used during surgery and medication costs the cost of all medications, including treatment drugs and narcotics.
Statistical analysis
The χ2 test, nonparametric Mann‐Whitney U‐test, and Student's t‐test were used for statistical analysis of data. Results were considered significant at a P‐value < 0.05. The analyses were performed using SPSS statistical software, version 13 (SPSS Chicago, IL, USA).
Results
In the anterior group, corpectomies were performed at the C4 level in 12 cases, C5 in 36, C6 in 16, C7 in 1, and at multiple levels (C4‐5 in 1 case and C5‐6 in 5 cases) in 6 cases. The follow up time was 12–68 months (mean 33 months). There were no surgical complications. In one case the site of internal fixation was adjusted on the 6th post‐operative day because of an unfavorable position.
In the posterior group, laminectomy was performed at multiple levels: four levels in 42 cases (C3–6 in 37 cases and C4–7 in 5 cases), and five levels in 3 cases (C3–7). The follow up time of this group was 12–70 months (mean 30 months). There were well no surgical complications. One patient developed postoperative paralysis and underwent re‐operation 10 months post‐operatively.
Comparison of pre‐ and post‐operative radiological findings showed that almost all patients in the study had ideal outcomes (1, 2).
Figure 1.

A 45 year‐old man had 4‐years of intermittent, progressively worsening neck pain combined with weakness in all extremities for 1 year. (A) Preoperative MR imaging shows that the cervical discs have protruded at C3‐4, C4‐5, C5‐6, compressing the spinal cord at the involved levels. (B) A preoperative lateral radiograph shows straightening of cervical lordosis. (C, D) After performing 4‐levels laminectomy with posterior screw‐rod fixation, improvement in intervertebral height and cervical lordosis is apparent.
Figure 2.
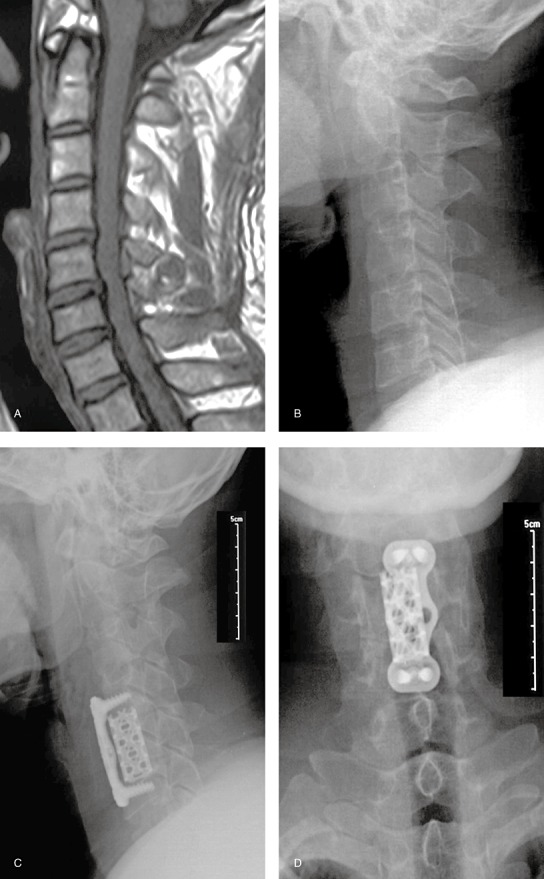
A 52 year‐old woman had had numbness and weakness in both hands for six months. (A) Preoperative MR imaging shows that the cervical discs have protruded at C4‐5, C5‐6, C6‐7, compressing the spinal cord at the involved levels. (B) A preoperative lateral radiograph shows straightening of cervical lordosis. (C, D) After performing C5 and C6 subtotal vertebrectomy followed by bone graft and fixation, improvement in intervertebral height and cervical lordosis is apparent.
Improvement of neurological function
Japanese Orthopedic Association scores were assessed pre‐operatively, 1 day before discharge, 6 months after discharge, and at last follow‐up in both groups. The results are shown in Table 1. The postoperative JOA scores were distinctly improved in both groups and, as time went on, these changes became even more marked. These findings indicate that both approaches are effective in improving spinal cord function. Preoperatively, the JOA scores of the two groups were not significantly different (P= 0.06), but at last follow‐up, the JOA scores were significantly higher in the anterior group (P= 0.007). This finding suggests that the JOA scores improved more in the anterior group, however this improvement was not statistically significant (P= 0.08). We concluded there was no significant difference between the anterior and the posterior groups in improvement in neurological function.
Table 1.
JOA scores at different follow‐up times
| Groups | Preop | Postop | 6 months | Last FU | JOA improvement (last FU‐preop)/(17‐preop)*100% | P value Last FU/Preop |
|---|---|---|---|---|---|---|
| Anterior | 10.5 ± 2.5 | 11.3 ± 1.8 | 14.4 ± 1.9 | 15.5 ± 1.6 | 77.0 ± 21.3 | <0.001 |
| Posterior | 9.5 ± 2.7 | 10.7 ± 2.0 | 14.1 ± 2.5 | 14.6 ± 1.7 | 68.1 ± 22.5 | <0.001 |
| P value | 0.06 | — | — | 0.007 | 0.08 | — |
Note: FU, follow‐up. Values given as mean ± SD.
Improvement in subjective evaluation
Satisfaction: 83% of patients in the anterior and 73% in the posterior group were satisfied with the operation, satisfaction in the anterior group being higher than that in the posterior group (P < 0.05).
Visual analog scale: both in the anterior and the posterior groups, neck pain diminished significantly after surgery. Moreover, neck pain in the anterior group (1.4 ± 1.6) was significantly less than that in the posterior group (2.3 ± 2.4) (P= 0.02).
Short Form‐36 (SF‐36) questionnaire: at last follow‐up, the scores for all eight items in the SF‐36 were higher than before surgery, indicating that both surgical approaches can effectively improve life quality. Preoperatively, there was no marked difference between the SF‐36 scores of the two groups. However, at final follow‐up, the emotional role (ER) scores of the anterior group (70.9 ± 21.8) were significantly higher than those of the posterior group (57.5 ± 19.4) (P= 0.00), as were the mental health (MH) scores (71.2 ± 19.1 vs. 62.2 ± 21.6) (P= 0.02). The scores for other items were not significantly different (Table 2).
Table 2.
Scores of all the 8 terms of SF‐36 before operations and at last follow‐up
| Items | Preop | Last FU | ||||
|---|---|---|---|---|---|---|
| Anterior group | Posterior group | P value | Anterior group | Posterior group | P value | |
| PF | 31.2 ± 18.5 | 34.5 ± 20.0 | 0.31 | 74.1 ± 22.8 | 77.0 ± 20.7 | 0.49 |
| PR | 30.7 ± 25.3 | 27.8 ± 24.1 | 0.18 | 64.8 ± 23.4 | 60.0 ± 20.2 | 0.26 |
| BP | 43.6 ± 20.7 | 39.6 ± 18.8 | 0.09 | 82.0 ± 14.2 | 75.7 ± 21.3 | 0.08 |
| GH | 35.2 ± 14.5 | 32.9 ± 16.0 | 0.11 | 60.4 ± 20.6 | 55.0 ± 22.2 | 0.20 |
| VT | 32.3 ± 21.3 | 29.9 ± 17.7 | 0.23 | 67.1 ± 17.6 | 62.7 ± 16.1 | 0.20 |
| SF | 45.8 ± 14.6 | 41.3 ± 20.6 | 0.08 | 72.9 ± 18.2 | 66.6 ± 21.0 | 0.09 |
| ER | 42.4 ± 19.6 | 38.0 ± 21.2 | 0.09 | 70.9 ± 21.8 | 57.5 ± 19.4 | 0.00 |
| MH | 36.9 ± 17.3 | 35.4 ± 18.0 | 0.38 | 71.2 ± 19.1 | 62.2 ± 21.6 | 0.02 |
Values given as mean ± SD. BP, bodily pain; ER, emotional role; FU, follow‐up; GH, general health; MH, mental health; PF, physical function; PR, physical role; SF, social function; VT, vitality.
Costs of medical care
We analyzed the total cost, and each component of the cost, for both groups. In both groups, the cost of the implants was responsible for the largest proportion of the total costs, followed by medication, surgery, examination and treatment costs (Fig. 3).
Figure 3.
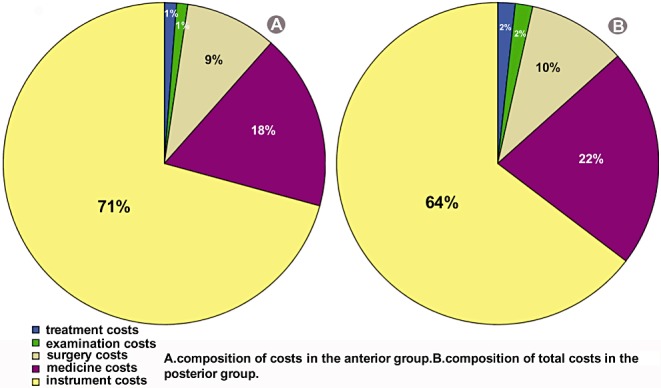
Pie chart showing composition of total costs (including costs of treatment, examination, surgery, medication, and instruments) in (A) the anterior group and (B) the posterior group.
When we compared the two groups we found the following. The length of hospital stay was not significantly different (anterior group, 14.9 ± 5.3 days; posterior group, 16.6 ± 3.0 days; P= 0.122). The treatment costs were significantly less for the anterior (411.7 ± 257.6 renminbi [RMB]) than the posterior group (621.2 ± 369.5 RMB) (P= 0.012). The examination costs for the anterior (375.8 ± 245.3 RMB) were significantly less than for the posterior group (616.5 ± 436.3 RMB) (P= 0.012). There were no significant differences (Table 3) between the groups in surgery, medication, instrument, and total costs. In conclusion, treatment and examination costs were the only costs that differed significantly between the two groups; the other costs and the length of hospital stay were not significantly different.
Table 3.
Total costs and costs of each individual component for both groups
| Items | Anterior group | Posterior group | P value |
|---|---|---|---|
| Length of hospital stay (days) | 14.9 ± 5.3 | 16.6 ± 3.0 | 0.122 |
| Total costs (RMB) | 33655.4 ± 10763.4 | 35375.1 ± 9221.1 | 0.498 |
| Treatment costs (RMB) | 411.7 ± 257.6 | 621.2 ± 369.5 | 0.012 |
| Examination costs (RMB) | 375.8 ± 245.3 | 616.5 ± 436.3 | 0.011 |
| Surgery costs (RMB) | 3092.3 ± 621.8 | 3494.5 ± 1008.6 | 0.065 |
| Medication costs (RMB) | 5961.0 ± 3292.0 | 7772.9 ± 4494.5 | 0.075 |
| Instrument costs (RMB) | 23814.6 ± 8458.3 | 22870.0 ± 8230.8 | 0.653 |
Values given as mean ± SD.
Discussion
We started using surgery to manage CSM over 50 years ago. Anterior decompression, the most widely used and effective surgical approach, aims to thoroughly decompress the spinal cord and nerve tissues by removing protruded intervertebral discs, hyperplastic osteophytes and the ossified cervical posterior longitudinal ligament and rebuild the stability of the cervical spine by interbody fusion and/or internal fixation, thus restoring the normal curvature of the cervical spine and the intervertebral height 8 . More recently, some Japanese scholars have developed a posterior approach for treating CSM with developmental stenosis of the cervical spinal canal or pathology mainly located posteriorly. To date, the operative techniques of the posterior approach include corpectomy, laminectomy, and laminoplasty. The main aim of posterior surgery is to achieve decompression by expanding the spinal canal. Recently, a novel approach termed the combined approach has been developed for CSM; in which decompression is achieved via both anterior and posterior approaches. This approach is best suited for CSM where there is both ventral and dorsal compression 9 .
For CSM that involves only one or two vertebral body levels, almost all surgeons agree that anterior decompression is indicated 10 . However, for CSM that involve more than two vertebral body levels, the criteria for selecting the optimal surgical strategy remain controversial 11 , 12 . In cases involving multilevel disease with kyphosis, a combined approach including anterior release and reconstruction of lordosis as well as posterior decompression with instrumentation may be appropriate 9 .
In contrast to previous studies, the present retrospective study compared different multilevel CSM surgical approaches, focusing on the patients’ subjective evaluation and cost analysis. Very little similar data has been published.
We have here presented 116 patients who had undergone multilevel cervical decompression for CSM; 71 patients in the anterior group underwent corpectomy followed by placement of TSM‐bone graft composite and internal fixation and 45 patients in the posterior group underwent laminectomy followed by posterior screw‐rod fixation. There was no significant difference between the two groups in improvement in neurological function. Both procedures were effective in improving spinal cord function and appeared to result in equal neurological benefit.
Complete assessment of the effects of surgery system should include the patients’ subjective evaluation. In the present study, we assessed satisfaction, VAS and SF‐36 scores. The SF‐36 quality of life questionnaire assesses eight items, namely physical function, physical role, bodily pain, general health, vitality, social function, emotional role and mental health. The anterior group showed greater satisfaction but lower VAS scores than the posterior group, whereas the SF‐36 ER and MH scores were higher in the anterior group. We attribute these apparent discrepancies to the fact that multiple factors would affect patients' subjective evaluation, including objective results, improvement in symptoms, prior expectations, and mental state. Anterior decompression may have achieved better results in subjective feelings and mental state in our present research.
Because cost is a major consideration in clinical decision‐making, especially when medical resources are limited, cost effectiveness must be carefully considered. The present study showed that instrument/implants are responsible for the largest proportion of the total cost of CSM. Except for the costs of treatment and examination, other costs and the length of hospital stay did not differ significantly between the anterior and posterior groups. These data imply that the key to reducing health care costs may be to reduce implant costs. Nevertheless, the medical costs of the two different decompression procedures are about the same.
In conclusion, for CSM that involve more than two levels, both anterior corpectomy followed by instrumentation and internal fixation and posterior laminectomy followed by posterior screw‐rod fixation can achieve ideal clinical outcomes, these findings being supported by other published reports 13 , 14 . Anterior compression seems to result in better patients’ subjective evaluation with similar recovery of neurological function and medical costs. However, our study group is small and some biases may have been present. Thus, further prospective studies that include greater numbers of patients are needed.
Disclosure
The authors declare no conflict of interest. No benefits in any form have been, or will be, received from a commercial party related directly or indirectly to the subject of this manuscript.
Acknowledgments
The authors would like to thank funding from the Seven‐year Innovation Fund of Xi’an Jiaotong University. Furthermore, we thank all colleagues who participated in clinical care of the patients, and Kiran Gurung for technical support.
References
- 1. McCormick WE, Steinmetz MP, Benzel EC. Cervical spondylotic myelopathy: make the difficult diagnosis, then refer for surgery. Cleve Clin J Med, 2003, 70: 899–904. [DOI] [PubMed] [Google Scholar]
- 2. Tracy JA, Bartleson JD. Cervical spondylotic myelopathy. Neurologist, 2010, 16: 176–187. [DOI] [PubMed] [Google Scholar]
- 3. Abumi K, Shono Y, Taneichi H, et al Correction of cervical kyphosis using pedicle screw fixation systems. Spine, 1999, 24: 2389–2396. [DOI] [PubMed] [Google Scholar]
- 4. Callahan RA, Johnson RM, Margolis RN, et al Cervical facet fusion for control of instability following laminectomy. J Bone Joint Surg Am, 1977, 59: 991–1002. [PubMed] [Google Scholar]
- 5. Cattell HS, Clark GL Jr. Cervical kyphosis and instability following multiple laminectomies in children. J Bone Joint Surg Am, 1967, 49: 713–720. [PubMed] [Google Scholar]
- 6. Klineberg E. Cervical spondylotic myelopathy: a review of the evidence. Orthop Clin North Am, 2010, 41: 193–202. [DOI] [PubMed] [Google Scholar]
- 7. Li L, Wang HM, Shen Y. Chinese SF‐36 Health Survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health, 2003, 57: 259–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Emery SE, Bohlman HH, Bolesta MJ, et al Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen‐year follow‐up. J Bone Joint Surg Am, 1998, 80: 941–951. [DOI] [PubMed] [Google Scholar]
- 9. Mummaneni PV, Haid RW, Rodts GE Jr. Combined ventral and dorsal surgery for myelopathy and myeloradiculopathy. Neurosurgery, 2007, 60 (1 Supp1 1): S82–S89. [DOI] [PubMed] [Google Scholar]
- 10. DiAngelo DJ, Foley KT, Vossel KA, et al Anterior cervical plating reverses load transfer through multilevel strut‐grafts. Spine, 2000, 25: 783–795. [DOI] [PubMed] [Google Scholar]
- 11. Bapat MR, Chaudhary K, Sharma A, et al Surgical approach to cervical spondylotic myelopathy on the basis of radiological patterns of compression: prospective analysis of 129 cases. Eur Spine J, 2008, 17: 1651–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Houten JK, Cooper PR. Laminectomy and posterior cervical plating for multilevel cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: effects on cervical alignment, spinal cord compression, and neurological outcome. Neurosurgery, 2003, 52: 1081–1088. [PubMed] [Google Scholar]
- 13. Emery SE, Fisher JR, Bohlman HH. Three‐level anterior cervical discectomy and fusion: radiographic and clinical results. Spine, 1997, 22: 2622–2625. [DOI] [PubMed] [Google Scholar]
- 14. Kawakami M, Tamaki T, Iwasaki H, et al A comparative study of surgical approaches for cervical compressive myelopathy. Clin Orthop Relat Res, 2000, 381: 129–136. [DOI] [PubMed] [Google Scholar]


