Abstract
Objective
The purpose of this study was to compare the clinical results of percutaneous reduction and Steinman pin fixation for Sanders II calcaneal fractures with those of operative management through an extensile lateral approach.
Methods
Fifty‐three patients treated with standard open reduction and internal fixation (ORIF group) and 54 patients who had undergone percutaneous reduction and Steinman pin fixation (CRIF group) were retrospectively reviewed. There were no differences between the groups regarding sex, age or fracture classification. Pain and functional outcome were evaluated with a visual analogue scale (VAS) and American Orthopaedic Foot and Ankle Society (AOFAS) scores. Wound complications and radiological results were compared.
Results
At a mean follow‐up of 40.4 months (24 to 56 months), there were no differences between the two groups in mean AOFAS score, VAS score or radiologically determined variables. Two cases of deep infection and six of poor wound healing occurred in the ORIF group and none in the CRIF group. Subtalar and ankle motion was found to be better in the CRIF group.
Conclusions
Percutaneous reduction and Steinman pin fixation minimizes complications and achieves functional outcomes comparable to those of the open techniques in patients with Sanders II calcaneal fractures.
Keywords: Fracture fixation, internal, Intra‐articular calcaneal fracture, Minimal‐invasive surgery
Introduction
Intra‐articular fractures of the calcaneum remain among the most challenging of fractures for the orthopedic surgeon to manage effectively. Open reduction and internal fixation (ORIF) via an extensile L‐shaped approach has gained wide popularity because this procedure provides a powerful way of restoring anatomical alignment of the calcaneum and congruity of the posterior subtalar joint and stable osteosynthesis without joint transfixation, allowing early mobilization. However, even though there is some evidence that operative treatment has advantages over non‐operative treatment, ORIF with an extensile exposure is often plagued by soft tissue complications. These include deep and superficial infections and wound sloughs, which reportedly occur in 1.8% to 27% of patients. This high frequency of infection is likely attributable to the soft‐tissue envelope around the calcaneus being particularly thin and vulnerable over the lateral wall, which is exposed for surgery1, 2, 3. To avoid these potential complications, a wide variety of percutaneous fixation options have been employed throughout the history of calcaneal fracture treatment. Notably, the first to introduce a technique for percutaneous pin leverage reduction and subsequent plaster immobilization was Westheus in 19344. The technique was further developed and popularized by Gissane in the USA5. Essex‐Lopresti reported the minimally invasive technique was particularly useful for reduction of tongue type fracture fragments1, 6. Currently, the Essex‐Lopresti technique has been further modified to facilitate fixation of percutaneous screws7, 8, 9, percutaneous arthroscopically assisted methods10, 11 and external fixation12, 13. Such minimally invasive procedures have the advantage of minimizing soft tissue complications and potentially shorter hospital stays. However, a risk of inadequate reduction of the posterior facet with an inferior functional outcome is a major concern, especially with complex fracture patterns. It is imperative for surgeons to weigh the risks and benefits of open surgery versus minimally invasive surgery in the quest for perfect correction of the subtalar joint. We believe that percutaneous techniques are indicated for simple fracture patterns (Sanders II, Arbeitsgemeinschaft für Osteosynthesefragen‐Orthopaedic Trauma Association [AO‐OTA] 83‐C2 fractures). For Sanders type III and IV, AO‐OTA 83‐C3 and C4 fractures, ORIF with a standard extended lateral approach is preferred.
This article describes the results in a consecutive of patients with Sanders II calcaneal fractures that were stabilized by percutaneous Steinman pin fixation. The outcomes were compared with those of a control group of concurrent patients treated by traditional ORIF through a lateral extensile approach. We postulated that percutaneous fixation could provide comparable results to open repair in patients with Sanders II fracture in regard to accurate restoration of subtalar joint congruity and overall architecture of calcaneus and subsequent restoration of function with minimal wound complications.
Materials and Methods
This retrospective study was authorized by the local ethics committee and performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. A search was conducted of hospital perioperative records. All surgeries had been performed by trained trauma surgeons, all of whom used both the standard ORIF and percutaneous techniques. Both protocols were used contemporaneously based on surgeon preference. Inclusion criteria for the study included patients over the age of 18 years, fractures involving the posterior facet classified as type II and AO‐OTA 83‐C2 according to the Sanders14 and AO‐OTA fracture classification15, closed fractures and fractures that had been managed operatively. Patients aged less than 18 years, those with extra‐articular, Sanders type I, III or IV, AO‐OTA 83‐C1, C3 or C4 and open fractures, and those with fewer than 2 years of follow‐up were excluded from the study.
Between January 2007 and May 2009, 107 patients with 118 intra‐articular calcaneal fractures that met all inclusion criteria were found. These patients were allocated to the following two groups for comparative purposes. The ORIF group consisted of 53 patients with 58 feet treated with standard ORIF via a extensile lateral approach, whereas 54 patients (60 feet) who had undergone percutaneous reduction and Steinman pin fixation were allocated to the percutaneous group (CRIF). Seven of the 107 patients had additional trauma in other parts of the body, including six patients with vertebral fractures, one with a tibial plateau fracture and one with contralateral bimalleolar fractures. Charts and radiographic reviews were analyzed for each consenting patient. The interval between injury and operation, length of hospital stay, functional score, subtalar fusion and surgical complications requiring inpatient management or reoperation were recorded. Wound complications included deep infections, which were defined as those requiring operative debridement and intravenous antibiotics or both. Poor wound healing was defined as an effusion existing more than ten days postoperatively but with negative bacterial cultures.
Surgical Procedures
Under spinal anesthesia, all patients were placed in a lateral decubitus position on a radiotranslucent operating table with the injured limb uppermost.
In the CRIF group, the fractures were reduced by manipulating the fragments percutaneously fashion. With tongue type fractures, fluoroscopy was used to guide a percutaneously driven 4 mm Steinmann pin to purchase the dense subchondral bone under the posterior facet without violating the subtalar joint cavity. After ensuring proper placement, this Steinmann pin was maneuvered as a joystick to lower the calcaneal tuberosity and elevate the posterior facet. The foot was arched and placed in varus using the thumbs as a fulcrum on the plantar surface (like breaking a stick), followed by valgus stress. The goal of reduction was to reestablish the length and height of the calcaneus and reduce its varus. In so doing, deviations of Böhler angle were simultaneously addressed. Manual compression was then applied on both sides of the calcaneus with the palms of hands to achieve further reduction of the width and height of the calcaneus.
In fractures with a joint depression pattern, a distraction technique was also used for reduction. A 4 mm Steinmann pin was inserted from the medial side through the calcaneal tuberosity. Manual longitudinal axial distraction was applied to correct varus, lateral and anterior displacements of the tuberosity. The posterior facet fragment was elevated and aligned percutaneously with an additional Steinman pin inserted through the posterolateral aspect of the Achilles tendon.
After anatomical reduction had been documented fluoroscopically, a 2.5 mm Steinman pin was introduced percutaneously into the posterior and inferior aspect of the calcaneus and directed through the calcaneus and across the calcaneocuboid joint to settle securely in the cuboid, the purpose being to stabilize the fracture fragments in a reduced alignment. A second Steinman pin was placed in a paralleling fashion as described for the first one. Additional Steinman pins were sometimes used if necessary. Finally, these pins were cut off level with the skin and the soft pin sites lightly dressed with dry sterile dressings.
In the ORIF group, the fractures were treated with the extended lateral approach described in by Zwipp et al.16, Sanders et al.14 and Benirschke and Sangeorzan17. The reductions were evaluated by both fluoroscopy and direct visualization and the fractures stabilized with traditional screws and metal plates.
Postoperative Care
The postoperative protocol for the two groups was similar. The foot was immobilized with removable splints. Rehabilitation exercises began on the second postoperative day. Progressive weight bearing was allowed until 12 weeks after surgery, when evidence of bone healing was radiographically present. The Steinman pins were removed at 8–12 weeks in the CRIF group and the plates and screws routinely removed 9 to 12 months postoperatively in ORIF group.
Outcome Measures
Clinical and radiological assessments were performed immediately after surgery and every 4 weeks until full fracture healing had been achieved, after which the patients were regularly followed up every 6 months in the outpatient clinic. Functional outcome was evaluated by using the American Orthopaedic Foot and Ankle Society (AOFAS) ankle‐hindfoot scale18. The AOFAS Ankle‐Hindfoot score assesses pain (40 points), function (50 points) and alignment (10 points). An excellent score is 90 to 100 points; good is 75 to 89 points, fair is 50 to 74 points, and poor is fewer than 50 points. A visual analog scale (VAS) pain score was used to assess residual pain postoperatively from a scale of 0 (no pain) to 10 (worst possible pain). The ranges of motion of the ankle and subtalar joint were measured according to the Association for Osteosynthesis (AO) neutral zero method. Clinical assessment was performed by a senior author (W.F.W) at regular follow‐up visits.
Preoperative evaluation included plain axial and lateral radiographs and CT scans of the foot in all patients. These imaging studies were used to determine the fracture pattern and plan surgery. Postoperative CT scans were only acquired occasionally and therefore were not reviewed systematically. Preoperative and postoperative Böhler's and Gissane's angles were also measured on the lateral views. Furthermore, on postoperative Broden radiographic views, the amount of posterior facet step‐off was measured in millimeters to assess posterior articular facet congruency. Joint surface displacement of less than two millimeters was considered a satisfactory outcome3, 19.
Statistical Methods
The data were compiled and analyzed using commercial software program, SPSS version 11.0 (SPSS, Chicago, IL, USA). Mean and standard deviation (SD) were calculated for all measured and calculated values. Data were analyzed with either Student's t‐test or the Pearson χ2 test. A significant result was taken as P < 0.05.
Results
The two groups were similar with respect to age, sex and fracture type according to the Essex‐Lopresti and Sanders classifications (Table 1). Falls, as a mechanism of injury, accounted for 83.3% (45/54) of CRIF group injuries, compared with 79.2% (42/53) in the ORIF group. The average time from day of injury to surgery was 7.9 days in the ORIF group and 5.3 days in the CRIF group (P = 0.01). The length of hospital stay was 19.7 days in the ORIF group and 10.5 days in the CRIF group (P = 0.01). Both these differences between the two groups are significant.
Table 1.
Patient demographic data
| Indexes | ORIF | CRIF | P value |
|---|---|---|---|
| Age (years) | 41 (22–58) | 39 (19–66) | 0.57 |
| Sex | 0.68 | ||
| Male | 49 | 51 | |
| Female | 4 | 3 | |
| Injured extremity | 0.78 | ||
| Unilateral | 48 | 48 | |
| Bilateral | 5 | 6 | |
| Essex‐Lopresti classification | 0.31 | ||
| Tongue type | 19 | 25 | |
| Joint depression | 39 | 35 | |
| Sander classification | 0.11 | ||
| IIA | 21 | 13 | |
| IIB | 28 | 30 | |
| IIC | 9 | 17 | |
| Interval between injury and surgery (days) | 7.9 (1–35) | 5.3 (1–10) | 0.01 |
| Length of hospital stay (days) | 19.7 (5–44) | 10.5 (3–22) | 0.01 |
ORIF, 53 patients (58 feet); CRIF, 54 patients (60 feet).
Satisfactory reduction of the posterior facet (a step‐off less than 2 mm) was noted in 48 feet in the ORIF group (82.8%) and 46 feet in the CRIF group (76.7%), this difference not being significant (P = 0.41). There was no loss of correction of the subtalar joint surface in either group. According to radiologic assessment, the Böhler's and Gissan's angles of the calcaneus were significantly improved after surgery in both groups (P < 0.01 for both). Both the initial condition and these postoperative improvements were similar (P > 0.05, Table 2). There was little change in Böhler's and Gissane's angles in both groups during the follow‐up period (Fig. 1).
Table 2.
Radiographic data (mean ± SD, °)
| Groups | Böhler's angle | Gissane's angle | ||||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Follow‐up | Preoperative | Postoperative | Follow‐up | |
| CRIF group | 4.53 ± 14.65 | 27.53 ± 7.48 | 28.87 ± 7.59 | 152.08 ± 30.01 | 130.91 ± 12.54 | 128.84 ± 11.28 |
| ORIF group | 7.36 ± 15.55 | 28.93 ± 7.84 | 28.27 ± 6.94 | 147.12 ± 31.62 | 128.79 ± 16.31 | 127.54 ± 17.33 |
Note: Radiological data at the time of trauma, immediately postoperatively and at the most recent follow‐up visit.
Figure 1.
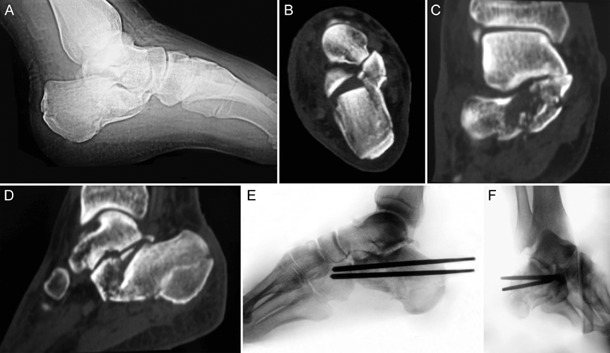
(A) Lateral radiograph, (B, C) coronal and (D) sagittal multiplanar reconstruction CT scans of an active 34‐year‐old man showing a Type IIC fracture of the right calcaneus sustained after falling from a ladder. After percutaneous reduction by the Essex‐Lopresti maneuver, fixation was achieved with Steinman pin. Restoration of the calcaneal shape posterior, facet congruity and adequate Steinman pin is apparent on (E) lateral and (F) Broden views.
The rates of wound complications differed significantly between the two groups. Two cases of deep infection and six of poor wound healing (13.79%) occurred in the ORIF group, whereas there were none in the CRIF group (P = 0.003). In the ORIF group, poor wound healing was resolved by local wound dressing. The deep infections were treated by operative debridement and intravenous antibiotics. The plates were removed after bone healing had been achieved, about 4 months after surgery, and the wounds healed by granulation. In the CRIF group, one case of drainage from the pin site that resolved after local wound care was documented. No patient developed osteomyelitis of the calcaneus. No patient underwent a subtalar fusion during the course of the observation period in either group.
Follow‐up for a minimum of 2 years after injury (range, 24–56 months; mean 40.4 months) was achieved in 48 (50 feet) of 54 patients in the CRIF group and 46 (49 feet) of 53 patients in the ORIF group. Thirteen patients were unable to be contacted and lost to follow up. At the follow‐up end point, the mean AOFAS score was 83.79 (range, 66 to 100) in the CRIF group and 81.09 (range, 44 to 100) in the ORIF group (P = 0.24). Excellent to good results were achieved in 36 of 48 patients (75.00%) in the CRIF group and 33 of 46 (71.74%) in the ORIF group. The VAS scores averaged 2.00 (range, 0 to 5) for patients in the ORIF group and 2.23 (range, 0 to 6) for those in the CRIF group (P = 0.48). These scores did not differ significantly between the two groups (Table 3).
Table 3.
Functional outcomes
| Groups | VAS | AOFAS | Excellent (%) | Good (%) | Fair (%) | Poor (%) |
|---|---|---|---|---|---|---|
| CRIF group | 2.23 (0–6) | 83.79 (66–100) | 16 (33.33) | 20 (41.67) | 12 (25.00) | 0 (0) |
| ORIF group | 2.00 (0–5) | 81.09 (44–100) | 12 (26.09) | 21 (45.65) | 11 (23.91) | 2 (4.35) |
AOFAS, American Orthopaedic Foot & Ankle Society score; VAS, visual analog score.
Better subtalar and ankle joint motion were noted in the CRIF group. The mean subtalar motion of the operated feet was 18.61° (range, 9° to 39°) in the ORIF group and 23.04° (range, 10° to 43°) in the CRIF group (P = 0.01). The average ankle motion was 49.30° (range, 20° to 75°) in the CRIF group and 45.06° (range, 20° to 70°) in the ORIF group (P = 0.09); this difference was not significant.
Discussion
The aims of surgical treatment of intra‐articular calcaneal fracture include anatomic reduction of the joint surface and restoration of the outer shape of the calcaneus. Although indirect, closed reduction and minimally invasive osteosynthesis have been proved to reconstruct the extra‐articular alignment to a similar degree as that achieved with ORIF with less wound complications, these techniques have been frowned upon because they have the disadvantage of achieving incomplete reduction of the subtalar facet3, 8. There is evidence from numerous studies that anatomic reconstruction of the subtalar joint is a major prognostic factor for displaced intra‐articular calcaneal fractures: even minor residual steps of about 2 mm in the posterior facet lead to a significant increase in the ratio of high‐pressure area to contact area in the subtalar joint according to biomechanical studies20, 21, they also have an adverse effect on functional outcome1, 11, 14, 16, 19. Furthermore, it is not possible to achieve anatomic articular reduction of comminuted fracture patterns in the posterior facet by closed methods. So the unanswered question is when to use percutaneous techniques in particular patients with particular fracture types.
The Essex‐Lopresti maneuver has recently been recommended for selected Sanders type IIC tongue‐type fractures and some Type 2B tongue‐type fractures in patients without comminution. Tornetta successfully used this method in 41 tongue‐type fractures, including 36 Type IIC and five Type IIB fractures. According to the Maryland Foot Score, good to excellent results were seen in 85% of the 41 patients followed up for an average of 3.4 years9. In 2010, Rammelt et al. combined percutaneous reduction and screw fixation of displaced calcaneus fractures with arthroscopic guidance. The quality of the reduction was confirmed arthroscopically in 33 of 61 patients with Sanders type IIA and IIB calcaneal fractures. With arthroscopic visualization of the reduction at the posterior facet, the risk of intra‐articular step‐off diminished10. Woon et al. reported that subtalar arthroscopy together with intraoperative fluoroscopy can aid in restoring congruence to the posterior calcaneal facet of the subtalar joint in all subtypes of Sanders type II fractures11. In our series, relatively simple fracture patterns (Sanders II, AO‐OTA 83‐C2 fractures); including both joint‐depression and tongue‐type fractures, were treated using percutaneous techniques. Both the extra‐articular anatomy and joint congruity were restored in most of our patients to a similar extent as in the ORIF group, resulting in 77.77% good to excellent long‐term results with shorter hospital stay and fewer problems in wound healing in the CRIF group. The clinical results of this technique compare favorably with those of patients treated by open reduction in the ORIF group. The findings of previous studies and this one prove that certain fracture patterns are amenable to effective management with minimally invasive osteosynthesis. Among them are Sanders II (AO‐OTA 83‐C2) fractures (in which only one fracture line crosses the posterior facet), whether tongue‐type or joint depression fractures. However, it is technically easier to reduce and maintain reduction in the former.
In our study, percutaneous reduction and fixation was performed an average of 5.3 days after the injury, therefore before fibrous union had begun, which made closed reduction efforts more difficult. There was a much longer interval between the trauma and surgery in the ORIF group, the aim being to prevent wound‐related complications. Operative fixation by an extensile lateral approach was postponed in patients with substantial swelling of the hind foot. Hospital stays were shorter in the CRIF than the ORIF group, which reflects an advantage of minimal invasive surgery. Of note, the relatively prolonged hospital stays in this study compared with reported studies from Western countries3, 7 related to our culture and the local Workers' Compensation policy.
In the ORIF group, two patients developed infection and six had poor wound healing, whereas no such serious complications occurred in the patients who underwent percutaneous fixation. The significantly lower wound‐related complication rate in the CRIF group is comparable to those described in other studies in which minimally invasive techniques were used9, 11. Our results, moreover, support the notion that a less invasive approach can greatly reduce the risk of skin necrosis and wound infections compared with a extensile lateral approach.
It has been suggested that the use of a percutaneous technique avoids the large incisions and stripping required for formal open reduction, thus decreasing the amount of scar formation within the sinus tarsi and possibly residual stiffness, thus preserving the range of motion of the subtalar joint7, 8, 11. In our series, we were not surprised to find that subtalar and ankle motion was better in patients treated with closed reduction. It may be beneficial for the majority of affected patients because 80% to 90% of calcaneal fractures occur in young and middle‐aged male manual workers2, 22. Their working conditions and the nature of their work demand flexible subtalar joints to enable them to tolerate uneven surfaces.
Hardware was removed after bone healing had been achieved in all patients in both groups, regardless of the presence or absence of symptoms. Although rarely seen in Europe and America, in China removal of asymptomatic implants is a very common phenomenon, amounting to being an integral and routine component of orthopaedic procedures. For custom‐ and culture‐related reasons, for Chinese patients prefer to have extrinsic implants removed22. In the CRIF group, the percutaneous Steinman pins can be removed without local anesthesia in an outpatient clinic. Such simple removal of Steinman pins decreases patients' stress and medical costs, which is another advantage of this minimally invasive technique. It is also the reason we chose Steinman pins to stabilize the calcaneal fragments rather than the screws described by other surgeons7, 8, 9, 10, 11.
This preliminary study had some limitations. The first is its retrospective nature and the small size of the cohort. To determine whether this technique achieves better outcomes than open surgery in patients with Sanders II (AO‐OTA 83‐C2) fractures, a further larger, prospective, randomized study and longer follow‐up is necessary. The second limitation is radiographic evaluation of outcomes. To visualize the quality of anatomical reduction of the posterior facet, intraoperative fluoroscopy‐based 3‐D imaging or CT scanning should be performed, although these methods have not been widely used thus far22, 23.
Percutaneous reduction and Steinman pin can restore extra‐articular alignment of calcaneus and posterior facet congruity; minimizes complications and achieves functional outcome as comparable as the open techniques in Sanders II type of calcaneus fractures (AO‐OTA 83‐C2).
Disclosure: No funds were received in support of this work.
References
- 1. Epstein N, Chandran S, Chou L. Current concepts review: intra‐articular fractures of the calcaneus. Foot Ankle Int, 2012, 33: 79–86. [DOI] [PubMed] [Google Scholar]
- 2. Makki D, Alnajjar HM, Walkay S, Ramkumar U, Watson AJ, Allen PW. Osteosynthesis of displaced intra‐articular fractures of the calcaneum: a long‐term review of 47 cases. J Bone Joint Surg Br, 2010, 92: 693–700. [DOI] [PubMed] [Google Scholar]
- 3. Tomesen T, Biert J, Frölke JP. Treatment of displaced intra‐articular calcaneal fractures with closed reduction and percutaneous screw fixation. J Bone Joint Surg Am, 2011, 93: 920–928. [DOI] [PubMed] [Google Scholar]
- 4. Westhues H. Eine neue Behandlungsmethode der Calcaneusfrakturen. Arch Orthop Unfallchir, 1934, 35: 121 (in German). [Google Scholar]
- 5. Rammelt S, Amlang M, Barthel S, Zwipp H. Minimally‐invasive treatment of calcaneal fractures. Injury, 2004, 35 (Suppl. 2): SB55–63. [DOI] [PubMed] [Google Scholar]
- 6. Essex‐Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg, 1952, 39: 395–419. [DOI] [PubMed] [Google Scholar]
- 7. Schepers T, Schipper IB, Vogels LM, et al Percutaneous treatment of displaced intra‐articular calcaneal fractures. J Orthop Sci, 2007, 12: 22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. DeWall M, Henderson CE, McKinley TO, Phelps T, Dolan L, Marsh JL. Percutaneous reduction and fixation of displaced intra‐articular calcaneus fractures. J Orthop Trauma, 2010, 24: 466–472. [DOI] [PubMed] [Google Scholar]
- 9. Tornetta P 3rd. Percutaneous treatment of calcaneal fractures. Clin Orthop Relat Res, 2000, 375: 91–96. [DOI] [PubMed] [Google Scholar]
- 10. Rammelt S, Amlang M, Barthel S, Gavlik JM, Zwipp H. Percutaneous treatment of less severe intraarticular calcaneal fractures. Clin Orthop Relat Res, 2010, 468: 983–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Woon CY, Chong KW, Yeo W, Eng‐Meng Yeo N, Wong MK. Subtalar arthroscopy and flurosocopy in percutaneous fixation of intra‐articular calcaneal fractures: the best of both worlds. J Trauma, 2011, 71: 917–925. [DOI] [PubMed] [Google Scholar]
- 12. Magman B, Bortolazzi R, Marangon A, Marino M, Dall'Oca C, Bartolozzi P. External fixation for displaced intra‐articular fractures of the calcaneum. J Bone Joint Surg Br, 2006, 88: 1474–1479. [DOI] [PubMed] [Google Scholar]
- 13. Talarico LM, Vito GR, Zyryanov SY. Management of displaced intraarticular calcaneal fractures by using external ring fixation, minimally invasive open reduction, and early weightbearing. J Foot Ankle Surg, 2004, 43: 43–50. [DOI] [PubMed] [Google Scholar]
- 14. Sanders R, Fortin P, Di Pasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures: results using a prognostic computed tomography scan classification. Clin Orthop Relat Res, 1993, 290: 87–95. [PubMed] [Google Scholar]
- 15. Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma, 1996, 10 (Suppl. 1): v–ix. 1–154. [PubMed] [Google Scholar]
- 16. Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res, 1993, 290: 76–86. [PubMed] [Google Scholar]
- 17. Benirschke SK, Sangeorzan BJ. Extensive intraarticular fractures of the foot: surgical management of calcaneal fractures. Clin Orthop Relat Res, 1993, 292: 128–134. [PubMed] [Google Scholar]
- 18. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle‐hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int, 1994, 15: 349–353. [DOI] [PubMed] [Google Scholar]
- 19. Song KS, Kang CH, Min BW. Preoperative and postoperative evaluation of intra‐articular fractures of the calcaneus based on computed tomography scanning. J Orthop Trauma, 1997, 11: 435–440. [DOI] [PubMed] [Google Scholar]
- 20. Sangeorzan BJ, Ananthakrishnan D, Tencer AF. Contact characteristics of the subtalar joint after a simulated calcaneus fracture. J Orthop Trauma, 1995, 9: 251–258. [PubMed] [Google Scholar]
- 21. Mulcahy DM, McCormack DM, Stephens MM. Intra‐articular calcaneal fractures: effect of open reduction and internal fixation on the contact characteristics of the subtalar joint. Foot Ankle Int, 1998, 19: 842–848. [DOI] [PubMed] [Google Scholar]
- 22. Wang Q, Chen W, Su Y, et al Minimally invasive treatment of calcaneal fracture by percutaneous leverage, anatomical plate, and compression bolts–the clinical evaluation of cohort of 156 patients. J Trauma, 2010, 69: 1515–1522. [DOI] [PubMed] [Google Scholar]
- 23. Abdelgaid SM. Closed reduction and percutaneous cannulated screws fixation of displaced intra‐articular calcaneus fractures. Foot Ankle Surg, 2012, 18: 164–179. [DOI] [PubMed] [Google Scholar]


