Abstract
Objective: To investigate the effect of treatment of osteoporotic proximal humeral fractures in elderly patients with a proximal humeral internal locking system (PHILOS) and minimally invasive injectable graft (MIIG).
Methods: Patients who conformed to the inclusion criteria were randomly divided into two groups: group A (21 cases) were treated with PHILOS alone and group B (29 cases) were treated with PHILOS augmentation plus minimally invasive injectable graft (MIIG) X3 Hivisc. Postoperative follow‐up was performed regularly to check for complications, reduction loss and fracture healing by imaging. Shoulder joint function was scored and clinical results evaluated according to the Neer scoring system.
Results: All patients were followed‐up and achieved fracture healing. The complication rate in group A (six cases) was greater than in group B (one case), the differences being statistically significant. The reduction loss in group A (2.9 ± 0.4 mm) was greater than in group B (1.5 ± 0.3 mm), this difference also being statistically significant. According to the Neer system, the excellent and good rate was 76.2% in group A and 82.8% in group B.
Conclusion: PHILOS using MIPPO and augmented with MIIG X3 Hivisc produces satisfactory clinical results in aged patients with osteoporotic proximal humeral fractures and the method has advantages such as relatively minor trauma, stable fixation, fewer complications, and better joint function.
Keywords: Humeral fractures, Internal fixators, Minimally invasive, Osteoporosis, Surgical procedures
Introduction
Proximal humeral fractures, which have a high incidence in elderly patients, are most often caused by low‐energy injuries and are closely associated with osteoporosis. Some of proximal humeral fractures are non‐displaced or minimally displaced which are successfully treated non‐operatively with good functional results. However, it is difficult to achieve and maintain a good reduction for severely displaced and comminuted fractures by non‐surgical treatment. So surgical treatment are performed for complex and unstable fractures to optimize shoulder function. The treatment decisions of displaced proximal humeral fractures trend to humeral head preservation based on the related factors such as fracture classification, bone quality, age of patient, rotator cuff disease, and surgeon. We usually prefer to plate fixation rather than hemiarthroplasty. The advent of locking plate technology has extended fixation ability in osteoporotic fracture. The proximal humeral internal locking system (PHILOS) conform to the anatomy of the proximal humeral and become increasingly important in the treatment of proximal humeral fractures. The PHILOS produces satisfactory clinical outcomes in the treatment of osteoporotic comminuted proximal humeral fractures, but has the drawbacks of fixation loosening, fracture re‐displacement and other complications 1 . How to avoid or reduce those complications? Reports in the literature are few. In an attempt to solve these problems and increase the stability of fixation, we tried using minimally invasive injectable graft (MIIG) X3 Hivisc to strengthen the spongy bone and fill the bone defects. The purpose of this study was to evaluate the efficacy of osteoporotic proximal humeral fractures in elderly patients with PHILOS and minimally invasive injectable graft.
Materials and methods
Fifty cases of proximal humeral fractures in elderly patients that were treated in our institution from January 2007 to January 2010 met the inclusion criteria as follows. Among them, 21 cases were treated with PHILOS alone using minimally invasive percutaneous plate osteosynthesis (MIPPO), and the other 29 cases were treated with PHILOS, also using MIPPO, plus augmentation with MIIG X3 Hivisc.
Inclusion criteria
(i) age ≥ 60 years; (ii) osteoporosis and bone mineral density T‐value not greater than 2.5 SD; (iii) fractures due to falls, excluding pathological fractures; (iv) unstable fractures, excluding severely comminuted fractures of the humeral head of the Neer four‐part type. Fifty such patients were randomly divided into two groups: A and B.
General data
There were 21 cases in Group A, including 5 men and 16 women with an average age of 69.7 years (range, 60–82 years). Twelve cases were on the left side, and nine on the right. According to the Neer classification, ten were type two‐part, eight were type three‐part and three were type four‐part. There were 29 cases in Group B, including 9 men and 20 women with an average age of 70.4 years (range, 63–86 years). Ten cases were on the left side and 19 on the right. According to the Neer classification, nine cases were type two‐part, thirteen were type three‐part and seven were type four‐part. All patients had one or more associated medical conditions, such as diabetes, hypertension, coronary heart disease, lung infections and cerebrovascular accidents. Surgery was performed within 3–5 days of the traumatic event in all cases. There were no statistically significant differences (P > 0.05) in the general characteristics of the two groups. Plain radiographs were obtained preoperatively in all cases, and CT scans with 3D reconstruction in some, to interpret the geometry of the fractures and deepen the understanding of their pattern, displacement and angulation.
Treatment
In group A, patients were positioned in the beach chair position after brachial plexus or general anesthesia. Preoperative conventional traction was performed under fluoroscopy with a C‐arm X‐ray machine. The operative area was draped with sterile sheets after routine disinfection. The preferred approach was below the anterolateral acromion, making a longitudinal incision of 3 cm, and cutting skin, subcutaneous tissue and fascia. The anterolateral aspect of the deltoid was dissected longitudinally and folded to each side to expose the greater tuberosity of the humerus and fracture site. The assistant gently applied traction to the limb according to the direction of fracture displacement. The surgeon reduced displaced fractures and restored the normal anatomic position of the humeral head either manually or by levering with Kirschner wire or pulling with a bone hook. Fractures were fixed provisionally by Kirschner wire after X‐raying to confirm correct alignment of the humerus.
A tunnel was made under the deltoid and extended to the distal humerus. A PHILOS plate of the appropriate length was selected and fixed with a locking guide, then inserted from proximal to distal through the deltoid incision, and the position of plate adjusted. The plate was positioned directly behind the dorsal intertubercular sulcus and extended 5–10 mm to protect the humeral artery, and roughly 8 mm distal to the superior tip of the greater tuberosity to prevent rotator cuff attachment, subacromial impingement and to support the humerus. Next, an approximately 2 cm longitudinal incision was made to expose the distal plate and the plate fixed by Kirschner wire so that it was aligned with the greater tuberosity. Under further traction, the elbow was then kept in flexion and external rotation with correct retroversion (about 30°–40°) in order fix the humeral head in a normal anatomical position. Once appropriate fracture reduction and plate position had been confirmed, the proximal plate was drilled using an insertion guide, taking care not to drill through the articular surface of the humeral head, and screws were inserted into the humeral head (about 3–4 locking screws). A non‐locked screw was inserted into the distal humerus to achieve compression, then 2–3 locking screws were inserted into the distal humerus and fixed through both sides of the cortex. Finally, once appropriate fracture reduction and plate position had been confirmed by radiographs, passive motion of the shoulder was checked and then wound lavaged, bleeding stopped and the incision closed.
In group B, the surgery was the same as in group A. Both the powder and mixture of MIIG X3 Hivisc were stirred into a paste, put into a special syringe, and injected under pressure into the humeral head and neck. The wound was then lavaged, bleeding stopped and the incision closed. A typical case is shown in Figure 1.
Figure 1.
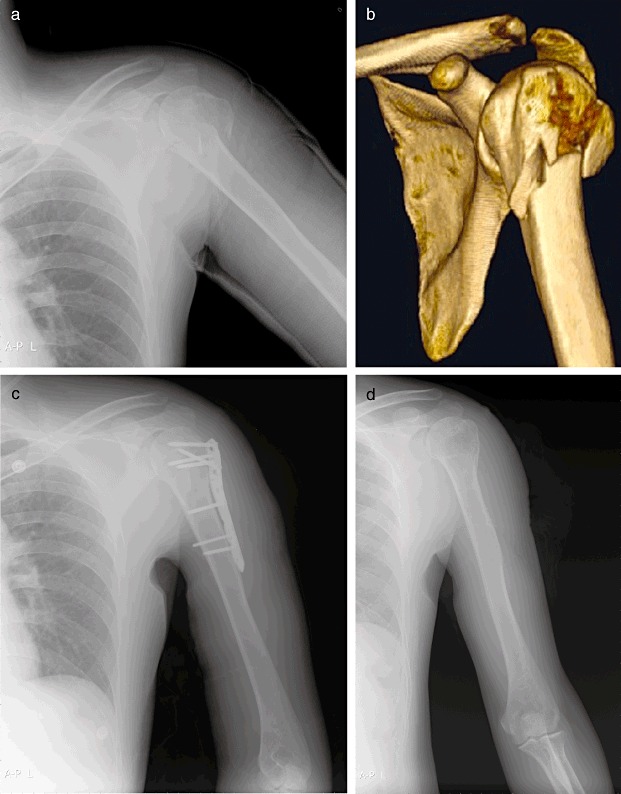
A 67 year‐old man with left proximal humeral fractures caused by a fall. (a) Preoperative X‐ray film and (b) CT scan showed left proximal humeral fractures. He was treated with PHILOS using MIPPO augmented by MIIG X3 Hivisc. (c) At 2 weeks postoperatively, an X‐ray film showed good reduction; and (d) at 12 months postoperatively, fixation was removed, and the X‐ray film showed fracture healing.
Postoperative treatment
All patients' arms were immobilized in wide arm slings for 2 weeks postoperatively (the slings were removed during functional exercise), with active treatment for osteoporosis. The patients started early muscle contraction exercises of the shoulder and elbow one day postoperatively, and controlled active mobilization, such as climbing a wall with their fingers, circles and swings in the next 3 or 4 days. Active abduction, anterior flexion and posterior shoulder stretch exercises commenced 1 week postoperatively. Normal daily activities were resumed when fracture healing had been confirmed by radiography. Postoperatively the patients attended for regular follow‐up appointments after they had been discharged from the hospital.
Evaluation and follow‐up
Operative time and blood loss were recorded. Postoperatively, the patients attended for regular follow‐up appointments. Radiographs were taken regularly to check for fracture displacement, loosening of fixation, screw cutout or backout, humeral head necrosis, reduction loss after restoration and fracture healing. Shoulder joint function was evaluated according to the Neer scoring system at 12 months postoperatively. In this system there are a total of 100 points made up of 35 points for pain, 30 points for function, 25 points for mobilization range and 10 points for anatomical position; 90 to 100 points is excellent, 80 to 89 points is good, 70 to 89 is moderate, less than 70 points is poor.
Statistical methods
Statistical software SPSS14.0 was used for statistical analysis. Operative time, blood loss, fracture healing as assessed by imaging and loss of limb length were compared between the groups by Student's t‐test. Complication rates and excellent‐to‐good rates on the Neer score were compared between groups using the χ2 test. Significance was set at P < 0.05.
Results
Group A: The mean operative time was 65.8 ± 12.9 minutes (range, 40–95 minutes), and the mean blood loss 102.5 ± 12.1 mL (range, 50–145 mL). All patients were followed up for an average of 18 months (range, 12 to 25 months). All patients achieved fracture healing. The mean healing time was 12.7 ± 1.6 weeks (range, 8–16 weeks). In this group, one patient had varus redislocation; fracture fixation loosening occurred in two cases; two screws penetrated the humeral head; no instances of screw backout occurred; one patient had osteonecrosis of the humeral head and the average loss of limb length was 2.9 ± 0.4 mm. For the initial and final radiographs, two lines were drawn perpendicular to the shaft of the plate: one at the top of the plate and one at the top of the humeral head, and the distance between them measured as an indicator of loss of limb length 13 . At 12 months postoperatively, according to the Neer scoring system, the mean shoulder score was 75.5 (range, 60.1–89.8), the shoulder function was excellent in seven cases, good in nine, moderate in two and poor in three and the excellent‐to‐good rate was 76.2%.
Group B: The mean operative time was 70.7 ± 13.1 minutes (range, 45–110 minutes), and the mean blood loss 110.1 ± 13.7 mL (range, 75–157 mL). All patients were followed up for an average of 16 months (range, 11–22 months). All patients achieved fracture healing. The mean healing time was 12.1 ± 1.4 weeks (range, 9–16 weeks). In this group, none of the cases had displacement, loosening, screw cutout or backout; only one of them had osteonecrosis of the humeral head and the average loss of limb length was 1.5 ± 0.3 mm. At 12 months postoperatively, according to the Neer scoring system, the mean shoulder score was 83.7 (range, 62.3–92.2), the shoulder function was excellent in 12 cases, good in 12, moderate in 4 and poor in 1 and the excellent‐to‐good rate was 82.8%.
There were no statistical differences in operative time, blood loss, fracture healing time and the excellent‐to‐good rate according to Neer score between groups A and B (P > 0.05). However, the study did show statistical differences between the two groups (P < 0.05) in complication rate and loss of limb length (Table 1).
Table 1.
Comparision of results in the two groups
| Group | Operative time (min) | Blood loss (mL) | Healing time (weeks) | Loss of limb length (mm) | Complications (number of cases) | Excellent‐to‐ good rate |
|---|---|---|---|---|---|---|
| Group A | 65.8 ± 12.9 | 102.5 ± 12.1 | 12.7 ± 1.6 | 2.9 ± 0.4 | 6 | 76.2% |
| Group B | 70.7 ± 13.1 | 110.1 ± 13.7 | 12.1 ± 1.4 | 1.5 ± 0.3 | 1 | 82.8% |
| P value | >0.05 | >0.05 | >0.05 | <0.01 | <0.05 | >0.05 |
Discussion
The principles of treatment for proximal humeral fractures include adequate correction that is maintained by stable fixation, the best possible restoration of the anatomical position of the proximal humerus, minimization of damage to the blood supply in order to preserve the humeral head, initiation of early and painless functional motion of the shoulder and optimization of postoperative shoulder function. The results of treating comminuted or unstable fracture nonsurgically are unsatisfactory. Traditional fixation has always had poor clinical efficacy because of its complications, including too much damage to soft tissue and impairment of blood supply, fixation instability or loosening, the requirement for lengthy postoperative immobilization and rotator cuff impairment. The thorny issue for treatment of osteoporotic proximal humeral fractures in elderly patients is how to achieve adequate reduction and stable fixation with a resetting and fixation method that involves minimal damage and maximizes humeral head preservation. Development of MIPPO, PHILOS and osteobiologics has provided new ways to solve the above‐mentioned issues.
Minimally invasive percutaneous plate osteosynthesis has obvious biological advantages. Its goals are to maximize preservation of blood supply, promote healing and reduce infection. The core of the treatment principles includes: (i) avoidance of direct exposure of the fracture site and provision of a good biological environment for healing, especially with respect to the blood supply around the fracture; (ii) use of traction of tendons, ligaments and soft tissue and indirect reduction techniques for fracture reduction; (iii) attempts to restore the axis and length and correct rotation, without forcing anatomic reduction; (iv) fracture reduction with the concept of “internal stent” and the use of ordinary or special plates for bridging fixation or elasticity fixation 2 .
The proximal humeral internal locking system is an angle stability fixture that was designed for osteoporotic proximal humeral fractures. The essence of PHILOS is the fixed‐angle relationship and mutual locking between the screws and plate, which not only guarantees that the screws are fixed in a three‐dimensional direction in the humeral head, but also reduces screw toggle, slide and pull‐out, and increases riveting and holding forces, improving the fixation effect on cancellous bone. The plate and screws form a rigid system with a strong load force and anti‐torsion effect that effectively prevents recurrence or displacement of the fracture. This system also reduces pressure on the bones and the destruction of blood supply, thus minimizing the risk of humeral head necrosis. Studies have shown that the locking plate can increase stability and healing, which is conducive to fixation of cancellous bone in proximal humeral fixation 3 . Koukakis et al. deemed that PHILOS is especially suitable for elderly patients with associated osteoporosis 4 .
Minimally invasive percutaneous plate osteosynthesis through an anterolateral subacromial approach minimizes, or even eliminates, the limitations of conventional fixation. With MIPPO, only two small incisions, at the proximal and distal ends of the fracture, are made. The plate can then be inserted through a tunnel established under the soft tissue and indirect restoration and elasticity fixation achieved. Gardner et al. 5 and Livani et al. 6 have reported that the axillary nerve can be stretched up to 1 cm from the humeral shaft without injuring it. Smith et al. consider that the minimally invasive deltoid splitting technique can be used without damage to the axillary nerve 7 . Hepp et al. found by analysis of the histomorphometry and microstructural architecture of the humeral head bone stock that trabecular thickness and density are greatest in the medial region 8 . Therefore, the best screw purchase is obtained by placing the superior screws into the medial subchondral bone. The fixation approach of locked screws in conjunction with non‐locked screws in the inferior holes achieves moderate compression and avoids concentration of local stress. Ahmad et al. found that a distance between the locked plate and bone of less than 2 mm maintains effective fixation 9 .
Some complications, such as delayed fracture healing, fixation loosening and fracture displacement occur postoperatively because of osteoporosis, postoperative metaphyseal defects and a poorly fixed humeral head. Some scholars have tried to reduce those complications by bone graft, and have obtained satisfactory results 10 . However, iliac grafts necessitate greater trauma and longer operation time, especially considering the limited quality and quantity of bone in these patients. The disadvantages of polymethacrylic acid bone cement are that high temperatures are produced by its curing, bone cement leakage can occur, it is not biodegradable in vivo and is not absorbed by the body 11 . Calcium phosphate cements produce less heat during curing but have some disadvantages, including poor shear strength, lack of osteoinductivity and slow resorption 12 . Therefore we selected minimally invasive injectable calcium sulfate implant to place in the fractures. This has the following characteristics: (i) plasticity, fast curing time (about 5 minutes) and curing without producing heat; (ii) strength similar to cancellous bone, therefore it augments bone support; (iii) filling of bone defects, thus blocking ingrowth of fibrous tissue, plus the absorption rate approaches the rate of new bone formation, thus it is eventually completely resorbed; (iv) osteoinductivity, stimulating new bone formation after degradation; (v) bone conduction, promoting healing; and (vi) because it is injectable, it is suitable for minimally invasive surgery.
The approach of using minimally invasive injectable calcium sulfate MIIG X3 Hivisc to intensify PHILOS fixation for the treatment in elderly patients is simple and feasible: it did not significantly increase operative time and blood loss in group B. In group B, the patients started early active mobilization postoperatively, the complications of postoperative fracture displacement, fixation loosening and loss of limb length were significantly reduced and shoulder joint function was better than in group A according to the Neer scoring system. Unsatisfactorily, MIIG X3 Hivisc does not prevent loss of limb length in proximal humeral fractures. Gardner et al. reported that mechanical support of the medial region is important for maintenance of reduction when proximal humerus fractures are treated with locking plates 13 . Medial support is considered to be necessary when the medial cortex has been anatomically reduced, the proximal fragment has impacted laterally on the distal shaft fragment, or an oblique locking screw has been positioned inferomedially in the proximal humeral head fragment 13 .
In the present study, we found that, with careful preoperative preparation and skilled surgical techniques, use of PHILOS in the treatment of osteoporotic proximal humeral fractures in elderly patients with MIPPO has positive results. Using MIIG X3 Hivisc to fill and strengthen can enhance the healing rate and decrease the incidence of fixation loosening and other complications. Of course, further study, long‐term follow‐up of a large number of cases and subsequent prospective controlled studies are necessary to confirm our findings.
Disclosure
The authors did not receive any outside funding or grants in support of the research for, or preparation of, this work. Neither they nor a member of their immediate families received payments or other benefits, or a commitment or agreement to provide such benefits, from a commercial entity.
References
- 1. Kettler M, Biberthaler P, Braunstein V, et al Treatment of proximal humeral fractures with the PHILOS angular stable plate. Presentation of 225 cases of dislocated fractures. Unfallchirurg, 2006, 109: 1032–1040. [DOI] [PubMed] [Google Scholar]
- 2. Ji F, Tong D, Tang H, et al Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop, 2009, 33: 543–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fankhauser F, Boldin C, Schippinger G, et al A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res, 2005, 430: 176–181. [DOI] [PubMed] [Google Scholar]
- 4. Koukakis A, Apostolou CD, Taneja T, et al Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res, 2006, 442: 115–120. [DOI] [PubMed] [Google Scholar]
- 5. Gardner MJ, Griffith MH, Dines JS, et al The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res, 2005, 434: 123–129. [DOI] [PubMed] [Google Scholar]
- 6. Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury, 2004, 35: 587–595. [DOI] [PubMed] [Google Scholar]
- 7. Smith J, Berry G, Laflamme Y, et al Percutaneous insertion of a proximal humeral locking plate: an anatomic study. Injury, 2007, 38: 206–211. [DOI] [PubMed] [Google Scholar]
- 8. Hepp P, Lill H, Bail H, et al Where should implants be anchored in the humeral head? Clin Orthop Relat Res, 2003, 415: 139–147. [DOI] [PubMed] [Google Scholar]
- 9. Ahmad M, Nanda R, Bajwa AS, et al Biomechanical testing of the locking compression plate: when does the distance between bone and implant significantly reduce construct stability?. Injury, 2007, 38: 358–364. [DOI] [PubMed] [Google Scholar]
- 10. Gerber C, Werner CM, Vienne P. Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br, 2004, 86: 848–855. [DOI] [PubMed] [Google Scholar]
- 11. Maestretti G, Cremer C, Otten P, et al Prospective study of standalone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J, 2007, 16: 601–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ladd AL, Pliam NB. Use of bone‐graft substitutes in distal radius fractures. J Am Acad Orthop Surg, 1999, 7: 279–290. [DOI] [PubMed] [Google Scholar]
- 13. Gardner MJ, Weil Y, Barker JU, et al The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma, 2007, 21: 185–191. [DOI] [PubMed] [Google Scholar]


