Abstract
Chronic pancreatitis (CP) is an irreversible fibroinflammatory disorder of the pancreas. It presents with relapsing, remitting upper abdominal pain accompanied by features of malabsorption due to pancreatic exocrine insufficiency and endocrine deficiency with the development of diabetes mellitus. The associated increased hospitalisation and high economic burden are related to CP often presenting at advanced stage with irreversible consequences. Diagnosing CP at an early stage is still challenging and therefore CP is believed to be under-reported. Our understanding of this disease has evolved over the last few years with attempts to redesign the definition of CP. Better recognition of the risk factors and conditions associated with CP can lead to an earlier diagnosis and coupled with a multidisciplinary approach to treatment, ultimately reduce complications. This article reviews the epidemiology, risk factors, diagnosis and management of CP.
Keywords: chronic pancreatitis, exocrine pancreatic function, pancreatic enzymes, pancreatitis
Epidemiology and risk factors of CP
Chronic pancreatitis (CP) is a progressive condition characterised by irreversible fibrosis of pancreatic parenchyma, accompanied by calcification and dilatation of the pancreatic ducts.1 The global prevalence of CP is variable, with estimates between 13.5 and 52.4 per 100 000 population.2–5 The incidence of CP in the United Kingdom is estimated to be 8.6 per 100 000 population per year.6 There is an apparent mismatch that exists between incidence and prevalence of CP which may suggest CP is under-recognised. In a multicentre French survey, the expected prevalence of CP has been calculated at 120–143 per 100 000 of population based on an incidence of CP of 7.8 per 100 000 of population per year, assuming an average life expectancy of 20 years following diagnosis.3 The idea that CP is under-recognised is also supported by historical postmortem series reporting a significantly higher prevalence of 2.1%–13%.7 8
Fibrotic changes in the pancreas develop following multiple inflammatory insults and can be due to a variety of causes (box 1); however, alcohol accounts for up to 80% of cases in the Western World.3 The risk of CP increases with the amount of alcohol consumed (OR:1.33 for 25 g/day and OR:3.19 for 100 g/day) compared with non-alcohol drinkers.9 Cessation of alcohol following acute alcoholic pancreatitis decreases the risk of developing CP.10 Smoking is a independent, dose-related risk factor for CP,5 11 significantly increasing the risk of developing CP compared with non-smokers (OR:7.8).9
Box 1. Classification of CP: The ‘TIGAR-O’ classification summarised the causes of CP into six groups: toxin, idiopathic, genetic, autoimmune, recurrent and severe acute pancreatitis, and obstructive1 .
Toxic-metabolic
Alcohol
Tobacco smoking
Hypercalcaemia
Chronic renal failure
Medication (azathioprine, tetracycline, valproate and oestrogens)
Idiopathic
Early onset
Late onset
Tropical
Genetic
Autosomal dominant
Autosomal recessive (cystic fibrosis)
Autoimmune
Isolated autoimmune CP
Syndromic associations (Sjögren’s, inflammatory bowel disease and primary biliary cirrhosis)
Recurrent and severe acute pancreatitis
Post necrotic and severe acute pancreatitis
Post radiotherapy
Ischaemia
Obstructive
Pancreatic divisum
Duct obstruction (tumour or stones)
CP, chronic pancreatitis.
Clinical and genetic testing is advised for patients with acute recurrent pancreatitis or idiopathic CP presenting below 35 years. Hereditary pancreatitis is a rare cause of CP with a prevalence of 0.3/100 000 population, it is autosomal dominant and characterised by early onset with a detectable PRSS1 mutation.12 13
Pancreas divisum is thought to be a risk factor for CP. The congenital non-fusion of the ventral and dorsal pancreatic duct can be demonstrated by endoscopic ultrasound (EUS) (sensitivity 85%–95%) and MRI (sensitivity 59%–73%).14–16 The prevalence in general population is estimated to be 1%–10% but <10% of patients develop symptoms thought to be caused by dominant drainage through a minor papilla stenosis.14 17 18 Retrospective studies have shown that the presence of pancreas divisum has no impact on the natural history of CP14 but it can act as a cofactor which increases the frequency of the attacks of pancreatitis when compared with controls.19 20
Presentation of CP
The classical presentation of CP is dull pain in the epigastrium area which radiates to the back and flanks. The bouts of pain and duration may vary but can intensify as the disease progresses.21 Patients with CP can present insidiously and are challenging to diagnose especially in the early phases. Symptoms of upper abdominal pain, weight loss and loose stools are non-specific and can overlap with other conditions (box 2).22
Box 2. Differential diagnosis of CP58 .
Acute cholecystitis
Biliary colic
Acute pancreatitis
Irritable bowel syndrome
Functional abdominal pain
Peptic ulcer disease
Pancreatic cancer
Postherpetic neuralgia
Gastroparesis.
Intestinal obstruction, ischaemia or infarction
Abdominal aortic aneurysm
Thoracic radiculopathy
Myocardial infarction
CP, chronic pancreatitis
The pain felt with CP can be from local inflammation effects or from pancreatic duct obstruction due to strictures and stone formation. Jaundice or cholangitis can develop from biliary obstruction due to inflammation of the pancreas around the bile duct and formation of pancreatic pseudocysts can cause localised pain and gastric outlet obstruction (figure 1).
Figure 1.
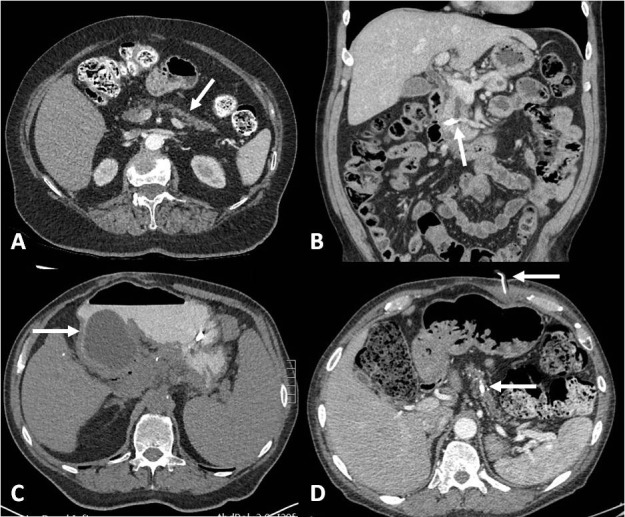
Complications of CP illustrated with CT: (A) Recurrent pancreatic inflammation results in atrophy with secondary PEI and diabetes (B) Dilated pancreatic duct containing a large (white) stone at the distal end resulting in pain and PEI. (C) A pseudocyst causing gastric outlet obstruction has developed with a nasogastic tube in situ. (D) Calcification in the pancreas parenchyma, recurrent inflammation adjacent to coeliac axis results in pain. In this patient, a gastroenterostomy feeding tube has also in situ for nutritional support. CP, chronic pancreatitis; PEI, pancreatic exocrine insufficiency.
Clinical distinction between CP and pancreatic cancer can be difficult. Urgent referral for investigation and discussion with multidisciplinary teams should be made where the possibility of underlying pancreatic cancer exists.23
Historically CP has a natural history divided into three phases with an early phase characterised by acute recurrent pancreatitis, pain and hospitalisations in first 5 years; a middle phase characterised by the presence of duct strictures and pancreatic calcifications; and a late phase after 10 years with development of complication such as diabetes mellitus and pancreatic exocrine insufficiency (PEI).24 However, it is now recognised that the timing of the development of symptoms from PEI (diarrhoea and malnutrition) and endocrine failure (diabetes) can vary significantly. It is also being recognised that PEI can precede the onset of pain and radiological morphological changes of CP in a number of patients.25 Although CP and PEI are closely linked, PEI can exist on its own or as a consequence of a number of other conditions. Pancreatic cancer causing ductal obstruction and altered anatomy following pancreatic and gastric surgery commonly results in PEI.26–28 Patients with type 1 diabetes and insulin treated type 2 diabetes have been shown high rates of significant PEI up to 22.9%.29 30
Diagnosis of CP
The diagnosis of CP is based on identifying morphological and/or functional abnormalities combined with clinical symptoms. Early diagnosis and treatment may help to halt the progress of the disease and prevent complications, however, diagnosing early stages of CP remains a challenge as these changes are often subtle.9
In patients with symptoms of CP, it is advisable to exclude other differentials (box 2). Clinical suspicion of CP alone is insufficient for diagnosis and a composite assessment is necessary. Symptoms and clinical history, cross-sectional imaging with CT and assessment of nutritional status are recommended (box 3).22 The gold standard diagnostic tool for CP is histology, but this is rarely performed due to its invasive nature, risk of complications and poor intraobserver agreement of CP features.1
Box 3. Investigative care bundle for patients with CP at diagnosis and follow-up22 38 51 80–83 .
New diagnosis CP—first consultation
Identify cause: CT has been performed to exclude differentials.
LFTs and abdominal ultrasound to exclude gallstones.
Consider MRI or EUS assessment for bile duct or pancreatic duct abnormalities.
Lifestyle modification: advice on cessation of smoking and alcohol.
Nutritional assessment: BMI or % body mass change if available prothrombin time, albumin, haematinics, vitamin D and E (if available), calcium, phosphate, magnesium.
Dietitian referral.
Test for exocrine and endocrine function
HbA1C and stool for FEL-1
Review pain control
Complications
Initial bone mineral density assessment
Follow-up (yearly)
Lifestyle modification: continued support on smoking and alcohol abstinence
Nutrition: BMI and % body mass change prothrombin time, albumin, haematinics, vitamin D and E (if available), calcium, phosphate, magnesium
Exocrine and endocrine function
HbA1C and stool for FEL-1.
Review enzyme replacement therapy dose and timing and consider acid suppression.
Pain
If uncontrolled consider pain team involvement or endoscopic or surgical intervention if dilated pancreatic duct on CT.
Complications
Liver function testing to exclude biliary obstruction developing.
CT scan if complications suspected (progressive weight loss, change in LFTs, new diabetes, worsening pain, vomiting).
Yearly CT scan in patients with hereditary pancreatitis.
Bone mineral density assessment (extend to 2 yearly if no other risk factors).
BMI, body mass index; CP, chronic pancreatitis; EUS, endoscopic ultrasound; FEL-1, faecal elastase-1; LFT, liver function test.
CT is the preferred diagnostic first line investigation, the sensitivity of CT exceeds that of ultrasound, (75%–90% vs 60%–70%) although the specificity is similar (CT 85% vs ultrasound 80%–90%).31 MRI is used for detailed ductal and cyst assessment and benefits from lack of radiation exposure. EUS is considered a highly sensitive method for diagnosing CP using certain criteria characterising parenchymal and ductal disease. Although it is can be subjective and intraobserver agreement variable when compared with histology as the gold standard, the sensitivity of EUS for the diagnosis of CP is >80%, with a specificity of 100%.32 It has also been shown to be a good correlation between the number of EUS criteria present and CP severity with respect to the histology.33
Serum tumour markers and amylase are not helpful in the diagnosis of CP and should not be performed, although amylase remains useful in diagnosing acute pancreatitis.34
Malnutrition is a major complication resulting from fat and protein malabsorption in addition to deficiencies of vitamins A, D, E and K.35 Up to 63% of patients with CP have fat-soluble vitamin deficiencies.35 36 Vitamin D deficiency exists in many patients with CP (and the general population) and although its presence is not diagnostic, deficiencies should be corrected.37 Several serum markers have been associated with the development of PEI including magnesium, haemoglobin, albumin, prealbumin and retinol binding protein.38 Vitamin E has been shown to be the single most useful level to check as a marker of malnutrition38 (box 3).
Symptoms of PEI are variable but can include diarrhoea, offensive smelling stools, steatorrhoea, bloating, abdominal pain and weight loss. Clinical features of malnutrition and muscle wasting may also be present.39 Diagnosing PEI early can be challenging due to the non-specific nature of symptoms and potential absence of abnormalities on imaging. ‘Compensated exocrine insufficiency’ may exist in patients with mild to moderate PEI prior to the onset of steatorrhoea and malabsorption.40
Exocrine function can be assessed with faecal elastase-1 (FEL-1). This is an indirect test of pancreatic function using FEL-1 as a surrogate. Other methods to directly assess pancreatic function have been described but are highly invasive and not widely available. FEL-1 measurement is easily performed; patients collect a pea-sized amount of faeces for analysis. FEL-1 has recurrently shown high sensitivity in severe PEI (85%–100%) but more varied results in moderate (35%–100%) and mild (25%–67%) disease with most studies showing a specificity >93%.41 42 It is felt to be the most appropriate first line investigation for screening for PEI in at risk patients.42 False positive FEL-1 samples can occur with water contamination form stool specimen collection, therefore strict instruction or low threshold for repeating should be considered with FEL-1 testing.
Complications and mortality of CP
CP is a disabling disease with severe impact on quality of life and increased mortality. Patients with advanced CP have a 2-fold to 13-fold increase in mortality compared with general population, largely due to cardiovascular complications.43 A reduction in 10-year survival of between 20% and 30% is seen in CP compared with the general population,44 therefore continued follow-up is required. PEI has also been shown to be an independent risk factor for mortality in patients with CP.45
The complication of CP are summarised in box 4.46 The risk of developing pancreatic cancer has been shown to be 1.3%–1.8% at 10 years after diagnosis and 4% at 20 years after diagnosis,47 48 this risk is especially significant in hereditary pancreatitis with an estimated 69-fold increased risk of pancreatic cancer compared with a 13-fold increase for other causes.49 The development of diabetes secondary to pancreatic diseases including CP (and also following pancreatic surgery) is classified as type 3c diabetes mellitus according to the current classification of diabetes mellitus.50 Type 3c diabetes is found in 5%–10% patients with CP, it is a complex subtype of diabetes which leads to glucagon deficiency and brittle diabetes. Type 3 c diabetes is important to recognise due to comorbidities such as maldigestion, malnutrition, pancreatic cancer risk and subclinical PEI which may cause no gastrointestetinal symptoms but poor diabetic control.51
Box 4. Complications of CP46 .
Diabetes mellitus type 3c
Pancreatic exocrine insufficiency
Metabolic bone disease
Pancreatic cancer
Splenic vein thrombosis
Pseudocysts
Duodenal obstruction
Biliary obstruction
CP, chronic pancreatitis
Osteoporosis and high prevalence of low trauma fracture are seen in patients with CP with one meta-analysis reporting 65% of patients with CP affected by osteoporosis or osteopaenia.52 In addition to the reduction in bone mass, patients with CP have been shown to have significant reductions in lean body mass and fat mass despite normal body mass index scores (figure 1).36
Management of CP
International guidelines advocate a multidisciplinary approach to managing patients with CP.49 53 Treatment of CP is similar regardless of aetiology. Aims of therapy include pain control, management of exocrine and endocrine insufficiency and management of complications. Involvement from chronic pain teams, dietitians and diabetologists can be beneficial. Surgery may be indicated for selected patients. We have summarised the current management recommendations in a care bundle (box 3).
Medical management
Complete abstinence from alcohol and smoking is essential for all patients to slow progression of disease and improve pain.11 54 55 Chronic pain and burden of incurable disease affect social situations of patients with CP. They are prone to social isolation and support groups may be of benefit to enable sharing knowledge and experiences to boost coping strategies.21 Patients with psychosocial problems may struggle to attend clinics and comply with treatment, often presenting as emergencies which adds to the management challenges.
Pain can initially be managed with simple analgesia with the addition of a weak opioid if necessary. It is not uncommon for patients with CP to require rapidly increasing doses of strong opioids risking tolerance and hyperalgesic side effects. Adjuncts such as gabapentin tricyclic antidepressants have been shown to be beneficial.56 Care should be taken when prescribing to avoid polypharmacy and opioid dependence.
A trend toward significant pain relief benefit from improved nutrition and pancreatic enzyme replacement therapy (PERT) has been shown in one systematic review,57 however PERT is not recommended for pain alone in CP.58 In select cases, jejunal feeding has been shown to improve pain, although oral nutrition remains the preferred route.59
Nutritional management
Patients with evidence of malnutrition, malabsorption or PEI should be treated with PERT to improve symptoms, nutritional status and quality of life.56 60 61 In 80% of patient with CP, PEI can be managed with normal diet and PERT, with 10%–15% requiring nutritional supplementation and 5% requiring enteral tube feeding.62 Intervention providing balanced dietary advice has been shown to be as effective as providing supplements to optimise malnutrition in patients with CP so early dietician input is vital.63 The majority of patients can be managed with normal diet (30% fat content) and PERT, however if calorie intake is low, protein supplementation can be considered.62 Starting dose of PERT at 50 000 units with meals and 25 000 units with snacks recommended but may need increasing or gastric acid suppression with proton pump inhibitors or H2-receptor antagonists may be necessary to improve absorption.
It has been suggested that baseline bone density assessment is performed in all individuals with CP given the high risk for osteoporosis, fractures and the associated morbidity and cost. In addition, advice regarding weight bearing exercise, smoking and alcohol cessation and dietary advice to maximise calcium and vitamin D intake should be provided as standard.64
Endoscopic management
Uncontrolled pain should trigger referral to a multidisciplinary assessment with physicians, surgeons and specialist pain clinics.22 As well as conventional analgesia, endoscopic therapy to dilate strictures, remove stones or drain pseudocysts can improve pain.34 EUS can be used to drain pseudocysts via the stomach if symptomatic or inject a coeliac plexus block. EUS-guided coeliac plexus blocks with steroid and local anaesthetic have been shown to be effective in just over half (55%) of patients with CP,65 but its duration is also limited meaning repeated procedures are required unless other interventions are planned.
Biliary obstruction can occur in 3%–23% of patients with CP for which endoscopic retrograde cholangio-pancreatography (ERCP) treatment for biliary strictures is effective.66 Covered self-expanding metal stents (SEMS) have been shown to be a safe and effective therapy in benign biliary stricture including those caused by CP.67 SEMS have a comparable success rate to plastic stents at 2 years of over 90%68 but they require less repeat interventions.69 70
In symptomatic patients with a pancreatic duct dilatation or strictures, immediate relief has been shown with plastic stent insertion in 65%–95% with longer term relief in 32%–68% of patients (follow-up 14–58 months).71 SEMS insertion in to a pancreatic duct stricture has also been shown to improve pain in 15/18 of patients after a follow-up of 47 months with no stent migration.72 Stones in the main pancreatic duct can be removed with ERCP but if ≥5 mm they are likely to require extracorporeal shock wave lithotripsy. Treatment for obstructive pancreatic duct pain with ERCP has been show to be possible with ERCP in up to 89% of patients73 however long-term outcomes for pancreatic stones seem better with surgical treatment.74 75
If a pancreatic divisum is thought to be the cause of CP, endotherapy (including minor papillotomy, stent placement and balloon dilatation of minor papilla) is possible and has better outcomes if recurrent pancreatitis attacks are occurring (76% vs 42%).17 76 Surgical options of a sphincteroplasty and pancreas head resection is also possible in cases of patients with CP and although surgical outcomes for pain relief seem to be favoured over endoscopic treatment (72%–74.9% vs 62.3%–69.4%)18 76 chosen methods are highly dependent on available expertise.
Surgical management
Surgery is beneficial for patients with obstructive CP from a dilated pancreatic duct (figure 1). Evidence generally favours surgery over endoscopy in terms of pain relief (75%–80% vs 32%–38%; p=0.042) with similar morbidity and mortality outcomes.74 75 77 Removing the diseased pancreas and creating a new pancreatic-jejunostomy to remove the obstruction (Frey’s procedure) with initial benefit is reported in up to 80% of patients, with 60% reporting benefit for >2 years78. Pancreatic resection is indicated in the presence of pain and small duct disease or enlargement of the pancreatic head, or if previous drainage procedures have failed21 (box 5).
Box 5. Indications for pancreatic resection21 .
Intractable resistant pain
Small duct disease
Enlargement of pancreatic head
Failure of previous drainage procedures
Suspicion of malignancy
Surgery for CP is a significant consideration with morbidity rates between 30% and 60% although mortality is <5%.79 Recovery includes readjustment to opioid dosing, pain from incisions and adjusting to life with insulin. Patients should be counselled extensively prior to undertaking surgery helping promote understanding of risks and benefits as well as the possibility that improvement is not guaranteed.21 Gastroenterosotmy (gastric bypass surgery) is also indicated for gastric outlet obstruction from chronic fibrotic compression of the duodenum once pancreatic cancer has been considered as an alternative cause.
Follow-up of CP
Patients should remain on yearly review where routine blood tests should be checked monitoring liver function tests and markers of malnutrition (box 3). If not already known to have PEI, stool testing for steatorrhoea with quantitative measures such as FEL-1should be used.80 Annual screening for diabetes mellitus with HbA1c should be offered.51 Additionally, 1–2 yearly osteoporosis screening should be considered for those with malnutrition or high-risk indicators (previous low trauma fracture).80 There is no role for routine pancreatic cancer screening, however, an urgent suspicious cancer pathway referral to gastroenterology or hepatobiliary surgery should be made for patients with unexplained progressive weight loss and a CT considered.81 American and UK guidelines advocate cancer screening only in those with hereditary pancreatitis and a PRSS1 mutation in patients with CP with a family history of pancreatic cancer53 82 when yearly CT should be performed.
Ongoing support in primary care is vital to help with smoking cessation, complete alcohol avoidance and treatment compliance. The management of this patient group is challenging especially in preventing opiate dependence.
Conclusion
CP develops due to multiple causes, the most common of which is alcohol. Patients present with severe pain among other features often including malnutrition and weight loss. Early identification of CP can be challenging and patients are at risk of complications such as osteoporosis, diabetes and pancreatic cancer. A clear diagnosis is vital for ongoing care with early multidisciplinary input to help guide treatment and manage complications.
Further reading
Lohr JM, Dominguez-Munoz E, Rosendahl J, Besselink M, Mayerle J, Lerch MM, et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterology Journal. 2017;5(2):153-99.
Drewes AM, Bouwense SAW, Campbell CM, Ceyhan GO, Delhaye M, Demir IE, et al. Guidelines for the understanding and management of pain in chronic pancreatitis. Pancreatology. 2017;17(5):720-31.
National Institute for Health and Care Excellence (NICE) Pancreatitis: diagnosis and management (including chronic). In development [GID-NG10015] Expected publication date: 05 September 2018. https://www.nice.org.uk/guidance/indevelopment/gid-ng10015. Last Accessed 28th January 2018.
Key points
Chronic pancreatitis (CP) is likely to be under-recognised.
When the diagnosis is considered it is important to exclude other causes of symptoms.
CP should be managed by a mutidiciplinary team with access to nutritional, medical, surgical and pain specialist support.
Continued follow-up should include support to reduce causes and check for the development of complications.
Footnotes
Contributors: MJ: drafted the original article analysis and interpretation of data. JAC and ADH: interpretation of data and approved the final version of the article to be published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Correction notice: This article has been corrected since it published Online First. Box 1 and figure 1 legends have been updated.
References
- 1. Etemad B, Whitcomb DC. Chronic pancreatitis: Diagnosis, classification, and new genetic developments. Gastroenterology 2001;120:682–707. 10.1053/gast.2001.22586 [DOI] [PubMed] [Google Scholar]
- 2. Wang LW, Li ZS, Li SD, et al. Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas 2009;38:248–54. 10.1097/MPA.0b013e31818f6ac1 [DOI] [PubMed] [Google Scholar]
- 3. Levy P, Barthet M, Mollard BR, et al. Estimation of the prevalence and incidence of chronic pancreatitis and its complications - A prospective survey in adults attending gastroenterologists in France. Gastroenterologie Clinique Et Biologique 2006;30(6-7):838–44. [DOI] [PubMed] [Google Scholar]
- 4. Hirota M, Shimosegawa T, Masamune A, et al. The sixth nationwide epidemiological survey of chronic pancreatitis in Japan. Pancreatology 2012;12:79–84. 10.1016/j.pan.2012.02.005 [DOI] [PubMed] [Google Scholar]
- 5. Domínguez-Muñoz JE, Lucendo A, Carballo LF, et al. A Spanish multicenter study to estimate the prevalence and incidence of chronic pancreatitis and its complications. Rev Esp Enferm Dig 2014;106:239–45. [PubMed] [Google Scholar]
- 6. Tinto A, Lloyd DA, Kang JY, et al. Acute and chronic pancreatitis–diseases on the rise: a study of hospital admissions in England 1989/90-1999/2000. Aliment Pharmacol Ther 2002;16:2097–105. 10.1046/j.1365-2036.2002.01367.x [DOI] [PubMed] [Google Scholar]
- 7. Akoojee SB. Pancreatitis in Natal. An autopsy study. S Afr Med J 1978;54:667–9. [PubMed] [Google Scholar]
- 8. Olsen TS. The incidence and clinical relevance of chronic inflammation in the pancreas in autopsy material. Acta Pathol Microbiol Scand A 1978;86A:361–5. 10.1111/j.1699-0463.1978.tb02057.x [DOI] [PubMed] [Google Scholar]
- 9. Yamabe A, Irisawa A, Shibukawa G, et al. Early diagnosis of chronic pancreatitis: understanding the factors associated with the development of chronic pancreatitis. Fukushima J Med Sci 2017;63:1–7. 10.5387/fms.2016-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kleeff J, Whitcomb DC, Shimosegawa T, et al. Chronic pancreatitis. Nat Rev Dis Primers 2017;3:17060 10.1038/nrdp.2017.60 [DOI] [PubMed] [Google Scholar]
- 11. Coté GA, Yadav D, Slivka A, et al. Alcohol and smoking as risk factors in an epidemiology study of patients with chronic pancreatitis. Clin Gastroenterol Hepatol 2011;9:266–73. 10.1016/j.cgh.2010.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Paolini O, Hastier P, Buckley M, et al. The natural history of hereditary chronic pancreatitis: a study of 12 cases compared to chronic alcoholic pancreatitis. Pancreas 1998;17:266–71. [DOI] [PubMed] [Google Scholar]
- 13. Rebours V, Boutron-Ruault M-C, Schnee M, et al. The natural history of hereditary pancreatitis: a national series. Gut 2009;58:97–103. 10.1136/gut.2008.149179 [DOI] [PubMed] [Google Scholar]
- 14. DiMagno MJ, Wamsteker EJ. Pancreas divisum. Curr Gastroenterol Rep 2011;13:150–6. 10.1007/s11894-010-0170-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kushnir VM, Wani SB, Fowler K, et al. Sensitivity of endoscopic ultrasound, multidetector computed tomography, and magnetic resonance cholangiopancreatography in the diagnosis of pancreas divisum: a tertiary center experience. Pancreas 2013;42:436–41. 10.1097/MPA.0b013e31826c711a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shen Z, Munker S, Zhou B, et al. The accuracies of diagnosing pancreas divisum by magnetic resonance cholangiopancreatography and endoscopic ultrasound: a systematic review and meta-analysis. Sci Rep 2016;6:35389 10.1038/srep35389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kanth R, Samji NS, Inaganti A, et al. Endotherapy in symptomatic pancreas divisum: a systematic review. Pancreatology 2014;14:244–50. 10.1016/j.pan.2014.05.796 [DOI] [PubMed] [Google Scholar]
- 18. Hafezi M, Mayschak B, Probst P, et al. A systematic review and quantitative analysis of different therapies for pancreas divisum. Am J Surg 2017;214:525–37. 10.1016/j.amjsurg.2016.12.025 [DOI] [PubMed] [Google Scholar]
- 19. Bertin C, Pelletier AL, Vullierme MP, et al. Pancreas divisum is not a cause of pancreatitis by itself but acts as a partner of genetic mutations. Am J Gastroenterol 2012;107:311–7. 10.1038/ajg.2011.424 [DOI] [PubMed] [Google Scholar]
- 20. Choudari CP, Imperiale TF, Sherman S, et al. Risk of pancreatitis with mutation of the cystic fibrosis gene. Am J Gastroenterol 2004;99:1358–63. 10.1111/j.1572-0241.2004.30655.x [DOI] [PubMed] [Google Scholar]
- 21. Goulden MR. The pain of chronic pancreatitis: a persistent clinical challenge. Br J Pain 2013;7:8–22. 10.1177/2049463713479230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Duggan SN, Ní Chonchubhair HM, Lawal O, et al. Chronic pancreatitis: a diagnostic dilemma. World J Gastroenterol 2016;22:2304–13. 10.3748/wjg.v22.i7.2304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adsay NV, Bandyopadhyay S, Basturk O, et al. Chronic pancreatitis or pancreatic ductal adenocarcinoma? Semin Diagn Pathol 2004;21:268–76. 10.1053/j.semdp.2005.08.002 [DOI] [PubMed] [Google Scholar]
- 24. Lévy P, Domínguez-Muñoz E, Imrie C, et al. Epidemiology of chronic pancreatitis: burden of the disease and consequences. United European Gastroenterol J 2014;2:345–54. 10.1177/2050640614548208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hopper AD, Campbell JA, Sanders DS. Improving Outcomes of Chronic Pancreatitis: Is Isolated Pancreatic Exocrine Insufficiency an Early Marker to Identify Modifiable Risks? Am J Gastroenterol 2017;112:813–4. 10.1038/ajg.2017.59 [DOI] [PubMed] [Google Scholar]
- 26. Löhr JM, Oliver MR, Frulloni L. Synopsis of recent guidelines on pancreatic exocrine insufficiency. United European Gastroenterol J 2013;1:79–83. 10.1177/2050640613476500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Frulloni L, Falconi M, Gabbrielli A, et al. Italian consensus guidelines for chronic pancreatitis. Dig Liver Dis 2010;42(42 Suppl 6):S381–406. 10.1016/S1590-8658(10)60682-2 [DOI] [PubMed] [Google Scholar]
- 28. Friess H, Böhm J, Müller MW, et al. Maldigestion after total gastrectomy is associated with pancreatic insufficiency. Am J Gastroenterol 1996;91:341–7. [PubMed] [Google Scholar]
- 29. Hardt PD, Krauss A, Bretz L, et al. Pancreatic exocrine function in patients with type 1 and type 2 diabetes mellitus. Acta Diabetol 2000;37:105–10. 10.1007/s005920070011 [DOI] [PubMed] [Google Scholar]
- 30. Nunes AC, Pontes JM, Rosa A, et al. Screening for pancreatic exocrine insufficiency in patients with diabetes mellitus. Am J Gastroenterol 2003;98:2672–5. 10.1111/j.1572-0241.2003.08730.x [DOI] [PubMed] [Google Scholar]
- 31. Issa Y, Kempeneers MA, van Santvoort HC, et al. Diagnostic performance of imaging modalities in chronic pancreatitis: a systematic review and meta-analysis. Eur Radiol 2017;27:3820–44. 10.1007/s00330-016-4720-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Albashir S, Bronner MP, Parsi MA, et al. Endoscopic ultrasound, secretin endoscopic pancreatic function test, and histology: correlation in chronic pancreatitis. Am J Gastroenterol 2010;105:2498–503. 10.1038/ajg.2010.274 [DOI] [PubMed] [Google Scholar]
- 33. Varadarajulu S, Eltoum I, Tamhane A, et al. Histopathologic correlates of noncalcific chronic pancreatitis by EUS: a prospective tissue characterization study. Gastrointest Endosc 2007;66:501–9. 10.1016/j.gie.2006.12.043 [DOI] [PubMed] [Google Scholar]
- 34. Conwell DL, Lee LS, Yadav D, et al. American Pancreatic Association Practice Guidelines in Chronic Pancreatitis: evidence-based report on diagnostic guidelines. Pancreas 2014;43:1143–62. 10.1097/MPA.0000000000000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Duggan SN, Smyth ND, O’Sullivan M, et al. The prevalence of malnutrition and fat-soluble vitamin deficiencies in chronic pancreatitis. Nutr Clin Pract 2014;29:348–54. 10.1177/0884533614528361 [DOI] [PubMed] [Google Scholar]
- 36. Haaber AB, Rosenfalck AM, Hansen B, et al. Bone mineral metabolism, bone mineral density, and body composition in patients with chronic pancreatitis and pancreatic exocrine insufficiency. Int J Pancreatol 2000;27:21–8. 10.1385/IJGC:27:1:21 [DOI] [PubMed] [Google Scholar]
- 37. Lindkvist B, Phillips ME, Domínguez-Muñoz JE. Clinical, anthropometric and laboratory nutritional markers of pancreatic exocrine insufficiency: Prevalence and diagnostic use. Pancreatology 2015;15:589–97. 10.1016/j.pan.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 38. Lindkvist B, Domínguez-Muñoz JE, Luaces-Regueira M, et al. Serum nutritional markers for prediction of pancreatic exocrine insufficiency in chronic pancreatitis. Pancreatology 2012;12:305–10. 10.1016/j.pan.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 39. Lindkvist B. Diagnosis and treatment of pancreatic exocrine insufficiency. World J Gastroenterol 2013;19:7258–66. 10.3748/wjg.v19.i42.7258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut 2005;54:1–28. 10.1136/gut.2005.065946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Löser C, Möllgaard A, Fölsch UR. Faecal elastase 1: a novel, highly sensitive, and specific tubeless pancreatic function test. Gut 1996;39:580–6. 10.1136/gut.39.4.580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Domínguez-Muñoz JE, D Hardt P, Lerch MM, et al. Potential for Screening for Pancreatic Exocrine Insufficiency Using the Fecal Elastase-1 Test. Dig Dis Sci 2017;62:1119–30. 10.1007/s10620-017-4524-z [DOI] [PubMed] [Google Scholar]
- 43. Bang UC, Benfield T, Hyldstrup L, et al. Mortality, cancer, and comorbidities associated with chronic pancreatitis: a Danish nationwide matched-cohort study. Gastroenterology 2014;146:989–94. 10.1053/j.gastro.2013.12.033 [DOI] [PubMed] [Google Scholar]
- 44. Seicean A, Tantau M, Grigorescu M, et al. Mortality risk factors in chronic pancreatitis. Journal of Gastrointestinal and Liver Diesase 2006:21–6. [PubMed] [Google Scholar]
- 45. de la Iglesia-Garcia D, Vallejo-Senra N, Iglesias-Garcia J, et al. Increased Risk of Mortality Associated With Pancreatic Exocrine Insufficiency in Patients With Chronic Pancreatitis. J Clin Gastroenterol 2017. [DOI] [PubMed] [Google Scholar]
- 46. Ramsey ML, Conwell DL, Hart PA. Complications of Chronic Pancreatitis. Dig Dis Sci 2017;62:1745–50. 10.1007/s10620-017-4518-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lowenfels AB, Maisonneuve P, Cavallini G, et al. Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N Engl J Med 1993;328:1433–7. 10.1056/NEJM199305203282001 [DOI] [PubMed] [Google Scholar]
- 48. Hao L, Zeng XP, Xin L, et al. Incidence of and risk factors for pancreatic cancer in chronic pancreatitis: A cohort of 1656 patients. Dig Liver Dis 2017;49:1249–56. 10.1016/j.dld.2017.07.001 [DOI] [PubMed] [Google Scholar]
- 49. Löhr JM, Dominguez-Munoz E, Rosendahl J, et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterol J 2017;5:153–99. 10.1177/2050640616684695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003;26:S5–20. 10.2337/diacare.26.2007.S5 [DOI] [PubMed] [Google Scholar]
- 51. Ewald N, Hardt PD. Diagnosis and treatment of diabetes mellitus in chronic pancreatitis. World J Gastroenterol 2013;19:7276–81. 10.3748/wjg.v19.i42.7276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Duggan SN, Smyth ND, Murphy A, et al. High prevalence of osteoporosis in patients with chronic pancreatitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2014;12:219–28. 10.1016/j.cgh.2013.06.016 [DOI] [PubMed] [Google Scholar]
- 53. DiMagno EP, Reber HA, Tempero MA. AGA technical review on the epidemiology, diagnosis, and treatment of pancreatic ductal adenocarcinoma. Gastroenterology 1999;117:1464–84. 10.1016/S0016-5085(99)70298-2 [DOI] [PubMed] [Google Scholar]
- 54. Olesen SS, Juel J, Graversen C, et al. Pharmacological pain management in chronic pancreatitis. World J Gastroenterol 2013;19:7292–301. 10.3748/wjg.v19.i42.7292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Talamini G, Bassi C, Falconi M, et al. Smoking cessation at the clinical onset of chronic pancreatitis and risk of pancreatic calcifications. Pancreas 2007;35:320–6. 10.1097/mpa.0b013e31812e965e [DOI] [PubMed] [Google Scholar]
- 56. D’Haese JG, Ceyhan GO, Demir IE, et al. Treatment options in painful chronic pancreatitis: a systematic review. HPB 2014;16:512–21. 10.1111/hpb.12173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Taylor JR, Gardner TB, Waljee AK, et al. Systematic review: efficacy and safety of pancreatic enzyme supplements for exocrine pancreatic insufficiency. Aliment Pharmacol Ther 2010;31:57–72. 10.1111/j.1365-2036.2009.04157.x [DOI] [PubMed] [Google Scholar]
- 58. Yagil Y, Goldenberg I, Arnon R, et al. Serologic testing for celiac disease in young adults–a cost-effect analysis. Dig Dis Sci 2005;50:796–805. 10.1007/s10620-005-2576-y [DOI] [PubMed] [Google Scholar]
- 59. Stanga Z, Giger U, Marx A, et al. Effect of jejunal long-term feeding in chronic pancreatitis. JPEN J Parenter Enteral Nutr 2005;29:12–20. 10.1002/j.1941-2444.2005.tb04840.x [DOI] [PubMed] [Google Scholar]
- 60. Sandhu BS, Sistrun SN, Naniwadekar A, et al. M1377 Good nutrition, as measured by mynutritionindex, in chronic pancreatitis patients improves clinical outcome. Gastroenterology 2010;138:S-392 10.1016/S0016-5085(10)61801-X [DOI] [Google Scholar]
- 61. de la Iglesia-García D, Huang W, Szatmary P, et al. Efficacy of pancreatic enzyme replacement therapy in chronic pancreatitis: systematic review and meta-analysis. Gut 2017;66:1354.1–5. 10.1136/gutjnl-2016-312529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Meier R, Ockenga J, Pertkiewicz M, et al. ESPEN Guidelines on Enteral Nutrition: Pancreas. Clin Nutr 2006;25:275–84. 10.1016/j.clnu.2006.01.019 [DOI] [PubMed] [Google Scholar]
- 63. Singh S, Midha S, Singh N, et al. Dietary counseling versus dietary supplements for malnutrition in chronic pancreatitis: a randomized controlled trial. Clin Gastroenterol Hepatol 2008;6:353–9. 10.1016/j.cgh.2007.12.040 [DOI] [PubMed] [Google Scholar]
- 64. Duggan SN, Conlon KC. Bone health guidelines for patients with chronic pancreatitis. Gastroenterology 2013;145:911 10.1053/j.gastro.2013.06.058 [DOI] [PubMed] [Google Scholar]
- 65. Gress F, Schmitt C, Sherman S, et al. Endoscopic ultrasound-guided celiac plexus block for managing abdominal pain associated with chronic pancreatitis: a prospective single center experience. Am J Gastroenterol 2001;96:409–16. 10.1111/j.1572-0241.2001.03551.x [DOI] [PubMed] [Google Scholar]
- 66. Varadarajulu S, Bang JY, Sutton BS, et al. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 2013;145:583–90. 10.1053/j.gastro.2013.05.046 [DOI] [PubMed] [Google Scholar]
- 67. Schmidt A, Pickartz T, Lerch MM, et al. Effective treatment of benign biliary strictures with a removable, fully covered, self-expandable metal stent: A prospective, multicenter European study. United European Gastroenterol J 2017;5:398–407. 10.1177/2050640616663757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Haapamäki C, Kylänpää L, Udd M, et al. Randomized multicenter study of multiple plastic stents vs. covered self-expandable metallic stent in the treatment of biliary stricture in chronic pancreatitis. Endoscopy 2015;47:605–10. 10.1055/s-0034-1391331 [DOI] [PubMed] [Google Scholar]
- 69. Devière J, Nageshwar Reddy D, Püspök A, et al. Successful management of benign biliary strictures with fully covered self-expanding metal stents. Gastroenterology 2014;147:385–95. quiz e15 10.1053/j.gastro.2014.04.043 [DOI] [PubMed] [Google Scholar]
- 70. Shen Y, Liu M, Chen M, et al. Covered metal stent or multiple plastic stents for refractory pancreatic ductal strictures in chronic pancreatitis: a systematic review. Pancreatology 2014;14:87–90. 10.1016/j.pan.2013.12.005 [DOI] [PubMed] [Google Scholar]
- 71. Dumonceau JM, Delhaye M, Tringali A, et al. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2012;44:784–800. 10.1055/s-0032-1309840 [DOI] [PubMed] [Google Scholar]
- 72. Oh D, Lee JH, Song TJ, et al. Long-term outcomes of 6-mm diameter fully covered self-expandable metal stents in benign refractory pancreatic ductal stricture. Dig Endosc 2018;30:508–15. 10.1111/den.13041 [DOI] [PubMed] [Google Scholar]
- 73. Guda NM, Partington S, Freeman ML. Extracorporeal shock wave lithotripsy in the management of chronic calcific pancreatitis: a meta-analysis. JOP 2005;6:6–12. [PubMed] [Google Scholar]
- 74. Cahen DL, Gouma DJ, Laramée P, et al. Long-term outcomes of endoscopic vs surgical drainage of the pancreatic duct in patients with chronic pancreatitis. Gastroenterology 2011;141:1690–5. 10.1053/j.gastro.2011.07.049 [DOI] [PubMed] [Google Scholar]
- 75. Cahen DL, Gouma DJ, Nio Y, et al. Endoscopic versus surgical drainage of the pancreatic duct in chronic pancreatitis. N Engl J Med 2007;356:676–84. 10.1056/NEJMoa060610 [DOI] [PubMed] [Google Scholar]
- 76. Liao Z, Gao R, Wang W, et al. A systematic review on endoscopic detection rate, endotherapy, and surgery for pancreas divisum. Endoscopy 2009;41:439–44. 10.1055/s-0029-1214505 [DOI] [PubMed] [Google Scholar]
- 77. Díte P, Ruzicka M, Zboril V, et al. A prospective, randomized trial comparing endoscopic and surgical therapy for chronic pancreatitis. Endoscopy 2003;35:553–8. 10.1055/s-2003-40237 [DOI] [PubMed] [Google Scholar]
- 78. Warshaw AL, Banks PA, Fernández-Del Castillo C. AGA technical review: treatment of pain in chronic pancreatitis. Gastroenterology 1998;115:765–76. 10.1016/S0016-5085(98)70157-X [DOI] [PubMed] [Google Scholar]
- 79. Ho CK, Kleeff J, Friess H, et al. Complications of pancreatic surgery. HPB 2005;7:99–108. 10.1080/13651820510028936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. NICE. Clinical knowledge summaries: pancreatitis- chronic, management of suspected chronic pancreatitis. London: National Institute for Clinical Excellence, 2016. [Google Scholar]
- 81. Ammann RW, Muellhaupt B. The natural history of pain in alcoholic chronic pancreatitis. Gastroenterology 1999;116:1132–40. 10.1016/S0016-5085(99)70016-8 [DOI] [PubMed] [Google Scholar]
- 82. National Institute for Health and Clinical Excellence guidelines. Pancreatic cancer in adults: diagnosis and management NICE guideline. 2018. nice.org.uk/guidance/ng85 (accessed 29 Jun 2018). [PubMed]
- 83. Mayerle J, Hoffmeister A, Werner J, et al. Chronic pancreatitis–definition, etiology, investigation and treatment. Dtsch Arztebl Int 2013;110:387–93. 10.3238/arztebl.2013.0387 [DOI] [PMC free article] [PubMed] [Google Scholar]


