Abstract
This study analyzes electronic diagnostic test ordering habits of internal medicine resident physicians at an academic medical center and during academic year 2016-2017.
The Dartmouth Atlas of Health Care sheds light on wide variations in spending for Medicare beneficiaries in the 6 months before their death.1 That report has led to several efforts to better standardize patient care. High-value care has been defined as the seventh competency, with national efforts to educate physicians and physicians in training about how to deliver higher-quality care, while decreasing the cost of that care.2 Medical students and residents are particular targets for this effort because of the known “imprinting,” or sustained influence, that the training environment has on practice habits during a physician’s career.3 Kahneman and colleagues4 found that professionals express a much greater-than-expected degree of variability in the outcomes of their work, even when given the same data with which to base their conclusions. We are aware of 2 previous studies that showed a large degree of variability in resident patterns of test ordering. One study5 analyzed outpatient test ordering in 1987, and another,6 “practice intensity” in 2015.
Methods
We analyzed electronic diagnostic test orders placed in the inpatient medical record by internal medicine residents at an academic medical center (NewYork-Presbyterian/Weill Cornell Medical Center). Among 139 internal medicine residents in this study, we compared the aggregate profiles of each resident over the course of academic year (AY) 2016-2017 for the total number of tests each resident ordered and the mean number of tests each resident ordered per patient for whom he or she provided care. The Weill Cornell Medicine institutional review board approved this study and granted an exemption from human participant review because all data were deidentified.
Results
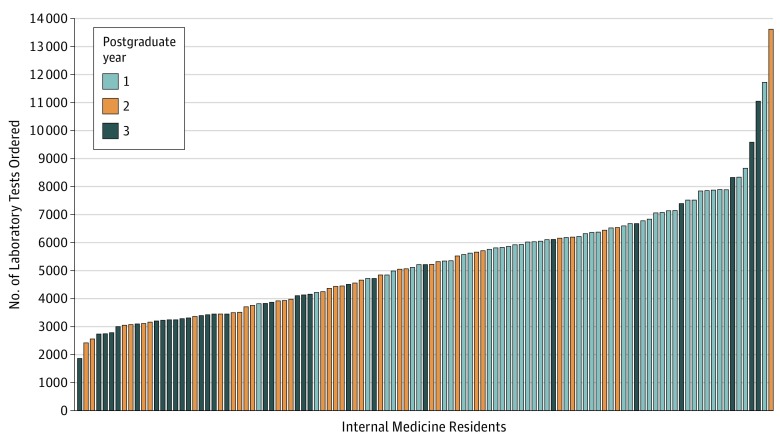
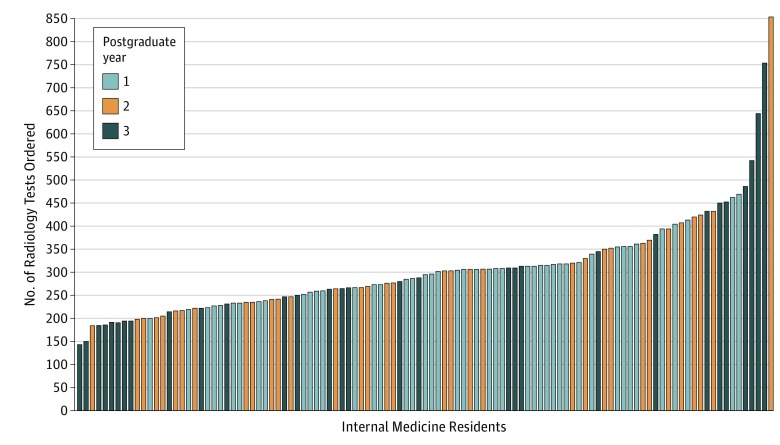
The residents in the New York-Presbyterian (Cornell Campus) internal medicine residency program ordered laboratory tests for 10 707 patients during 13 469 unique patient hospitalizations in AY 2016-2017. During these unique patient hospitalizations, the residents ordered 579 935 laboratory tests and 29 881 radiology tests. The resident who ordered the most laboratory tests (n = 13 604) ordered more than 7 times the tests than the resident who ordered the least (n = 1870) (interquartile range [IQR], 3509-6148) (Figure 1). The resident who ordered the most tests per unique patient hospitalization ordered 41.2 tests per patient compared with 9.0 tests per patient for the resident who ordered the least (IQR, 12.8-20.6), a 4.6-fold difference. The resident who ordered the most radiology tests (n = 826) ordered approximately 8 times the tests than the resident who ordered the least (n = 104) (IQR, 230-325) and approximately 3 times the tests per unique patient hospitalization (range, 1.6-5.0; IQR, 1.9-2.4) (Figure 2). Linear regression showed an association between postgraduate year (PGY) and the total number of laboratory tests ordered (R2 = 0.21; slope, −1187) and between PGY and the number of laboratory tests per patient (R2 = 0.19; slope, −3.2) but demonstrated no such associations for radiology testing (R2 < 0.01 for both). There was also a strong association between the total number of tests ordered and the mean number of tests per patient for both laboratory orders (R2 = 0.85; slope, 325) and radiology orders (R2 = 0.61; slope, 132).
Figure 1. Total Number of Laboratory Tests Ordered by Each Internal Medicine Resident.
There was a much greater-than-expected degree of variability between the residents in terms of the total number of laboratory tests ordered over the course of a year in which their schedules contained roughly the same number and types of rotations. There was a strong, positive linear association between the total number of laboratory tests ordered and the mean number of laboratory tests ordered per unique patient hospitalization (R2 = 0.85; slope, 325).
Figure 2. Total Number of Radiology Tests Ordered by Each Internal Medicine Resident.
There is a shift where more upper-level residents are at the higher end of the ordering spectrum, perhaps reflecting their greater involvement in decision making regarding radiology testing. There was no linear association between postgraduate year (PGY) and the total number of radiology tests ordered or the mean number of radiology tests ordered per unique patient hospitalization. There was a positive linear association between the total number of radiology tests ordered and the mean number of radiology tests ordered per patient (R2 = 0.61; slope, 132).
Discussion
This study found that over the course of AY 2016-2017 some residents ordered 7 to 8 times more diagnostic tests than their peers. Even excluding outliers, we observed much more variation in diagnostic test ordering volume than expected given that there were minimal differences in resident schedules among each PGY cohort during the 1-year period. The residents in their first PGY residents tended to order more laboratory tests than the residents in their second or third PGY, likely because of a cultural norm in our urban teaching hospital (NewYork-Presbyterian/Weill Cornell Medical Center) where interns are responsible for ordering daily laboratory testing. Curiously, the top 3 residents by laboratory test ordering volume included individuals from each PGY.
The most significant limitation of this study is the inability to normalize test ordering frequency for patient acuity. We are also blind to the potential degree to which supervising physicians may directly or indirectly influence test ordering behavior.
Because residents are “imprinted” by their training environment, even small reductions in diagnostic test ordering habits during training could translate to years of higher-value care. Future research should evaluate the reasons for this variability.
References
- 1.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending, part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138(4):273-287. doi: 10.7326/0003-4819-138-4-200302180-00006 [DOI] [PubMed] [Google Scholar]
- 2.Weinberger SE. Providing high-value, cost-conscious care: a critical seventh general competency for physicians. Ann Intern Med. 2011;155(6):386-388. doi: 10.7326/0003-4819-155-6-201109200-00007 [DOI] [PubMed] [Google Scholar]
- 3.Asch DA, Nicholson S, Srinivas S, Herrin J, Epstein AJ. Evaluating obstetrical residency programs using patient outcomes. JAMA. 2009;302(12):1277-1283. doi: 10.1001/jama.2009.1356 [DOI] [PubMed] [Google Scholar]
- 4.Kahneman D, Rosenfield AM, Gandhi L, Blaser T. Noise: how to overcome the high, hidden cost of inconsistent decision making. https://hbr.org/2016/10/noise. Published October 2016. Accessed January 30, 2018.
- 5.O’Brien DK, Flood J, Wesley R. Resident test ordering patterns. Fam Pract Res J. 1987;7(1):42-50. [PubMed] [Google Scholar]
- 6.Dine CJ, Bellini LM, Diemer G, et al. Assessing correlations of physicians’ practice intensity and certainty during residency training. J Grad Med Educ. 2015;7(4):603-609. doi: 10.4300/JGME-D-15-00092.1 [DOI] [PMC free article] [PubMed] [Google Scholar]