Abstract
Debridement, spinal canal decompression, deformity correction, bone graft fusion and internal fixation are commonly used in the surgical treatment of spinal tuberculosis. A complete surgical plan for patients with spinal tuberculosis may include all or some of these five surgical procedures that involve both removing tuberculous lesions and re‐establishing spinal stability and function. All five procedures can be carried out via an anterior or posterior approach or a combination of these two approaches. A combined posterior–anterior approach is becoming a preferred choice for treating spinal tuberculosis. However, this procedure requires two incisions and two rounds of surgeries, which the associated extensive surgical trauma. Thus, a simple anterior or posterior approach may be preferable. Each of these approaches has its own advantages and disadvantages that must be considered during the clinician's evaluation. Selection of the most appropriate of these three approaches is vital to achieving cure of spinal tuberculosis. Spinal surgeons should comprehensively consider each patient's characteristics, the manifestations of their lesions and how familiar the surgeon is with the required surgical procedure(s). The primary consideration should be the potential outcome: the effectiveness of debridement is the key determinant of the surgical outcome.
Keywords: Selection surgical procedures, Spinal tuberculosis, Thoracic and lumbar
Introduction
Continuing improvements resulting from basic research on spinal surgery have refined the surgical procedures for treating spinal tuberculosis1, 2, 3. Debridement, spinal canal decompression, deformity correction, bone graft fusion and internal fixation are commonly used in the surgical treatment of spinal tuberculosis4. A complete surgical plan for patients with spinal tuberculosis may include all or some of these five surgical procedures, the fundamental goal of which is to remove foci of spinal tuberculosis, the secondary yet important goals being achieving postoperative spinal stability and functional recovery5, 6, 7.
All five procedures listed above can be carried out via an anterior or posterior approach or a combination of these approaches. Because most spinal tuberculosis lesions are located in the anterior and middle columns of the spine, optimal surgical treatment of spinal tuberculosis should include anterior debridement, spinal canal decompression and bone graft fusion, posterior deformity correction and internal fixation. This makes a combined posterior–anterior approach the top choice for treatment of spinal tuberculosis. However, this procedure requires two incisions and two rounds of surgeries, with the associated extensive surgical trauma. Therefore, a simple anterior or posterior approach may be preferable. Spinal tuberculosis is most commonly located in the thoracic and lumber portions of the spine. In this course, we focus on appropriate selection of procedure(s) for the surgical treatment of thoracic and lumbar spinal tuberculosis.
Anterior Approach
The term “anterior approach surgery” refers to a systemic surgical procedure for treating spinal tuberculosis that specifically includes debridement, spinal canal decompression, deformity correction, bone graft fusion and internal fixation via an anterior spinal approach. Debridement of spinal tuberculosis has conventionally been performed via an anterior approach8. However, this approach has had the shortcoming of providing limited exposure of the affected vertebral body. During surgery, a bone fistula or abscess is often used as the main marker and the lesion is probed digitally or by guiding a curette, neither of which have exposed the lesion sufficiently in the past. Inadequate exposure of the affected vertebra has meant that the surgeon cannot perform complete debridement, accurate decompression and bone grafting. In addition, deformity correction and internal fixation could not be readily achieved. Therefore, the overall therapeutic outcome has often been unsatisfactory. With gradual improvements in anterior spinal surgery and continuing development of related surgical techniques, better surgical exposure and a wider field of vision can be achieved via an anterior approach. These factors allow the physician to perform surgery under direct vision, which makes the surgery safer and greatly improves outcomes9. In general, modern anterior approaches to surgery for treating spinal tuberculosis should sufficiently expose the anterior and lateral sides of the vertebrae inferior and superior to the affected intervertebral disc space. The upper and lower 1–2 normal vertebrae should be exposed according to the range of internal fixation; however, normal vertebrae distal to these vertebrae should not be exposed.
After the lesion has been exposed, the reactive bone of the affected vertebrae should be preserved as much as possible while completely removing the lesion. With multisegment spinal tuberculosis, each intervertebral disc space should be cleaned up step‐by‐step. Several small defects may be left after debridement. Bone grafting of any such small defects facilitates bony healing because of the large contact area and good blood supply. Surgeons should avoid breaking several affected vertebrae because formation of a large defect not only makes it difficult to select the size of the bone graft, but also reduces the contact area of a long‐segment bone graft, prejudicing graft healing. Strut grafts should be selected as often as possible because they provide intervertebral support for the anterior and middle columns, thus decreasing the biomechanical load on the posterior column and making the intervertebral fixation more solid.
Indications for Anterior Approach Surgery
This procedure is suitable for spinal tuberculosis with intact spinal accessories when fewer than two consecutive intervertebral disc spaces are damaged10 or the surgical procedure involves fewer than three intervertebral disc spaces. In cases where spinal tuberculosis has caused serious destruction, the lesion may invade the pedicle and even the superior articular process, the inferior articular process, and the lamina from one side or both sides of the vertebral body, inducing tissue granulation and abscess formation posterior to the spine. Lesions in the spinal accessories cannot be removed via an anterior approach and must be completely removed via a posterior approach. When the disease involves two consecutive intervertebral disc spaces, three consecutive vertebrae are affected. Whether the disease involves one intervertebral disc space or two consecutive intervertebral disc spaces, two internal fixation methods are available for implanting vertebral screws depending on how much of the affected vertebral body remains after complete debridement and bone graft fusion. The first method is internal fixation between the affected vertebrae. Screws can be directly inserted into an affected vertebral body that is more than two‐thirds the height of a normal vertebral body. This fixation method fixes two intervertebral spaces and three vertebral bodies and is the best choice for lesions that involve two intervertebral disc spaces. The second method is short‐segment fixation. An affected vertebral body that is less than two‐thirds the height of a normal vertebral body cannot hold two screws with 14 mm spacing between the upper and lower lateral margins; thus, in such cases the screws must be placed in the adjacent normal vertebrae, crossing superior and inferior normal intervertebral disc spaces. This fixation method requires fixing three or four intervertebral disc spaces in patients with two affected intervertebral disc spaces; thus, four or five vertebrae are involved. Although this method fixes one superior and one inferior normal intervertebral disc space, it is still an acceptable fixation method. However, more than two upper or lower normal intervertebral disc spaces are often fixed in clinical practice, which is not acceptable.
Patients with spinal tuberculosis and an associated cold abscess require anterior approach surgery. When thoracic or lumbar spinal tuberculosis is associated with paraspinal, psoas or significant gravitation abscess(es) in the chest wall, iliac fossa or inguinal region, these abscesses should be removed completely under direct vision via the same incision or another additional small incision without changing the patient's position. Psoas and large gravitation abscesses should be removed via an anterior approach.
Patients with associated injuries in the spinal cord, cauda equina or nerve roots require anterior decompression. In most cases of spinal tuberculosis, compression of the spinal cord and nerve roots occurs from the anterior or anterolateral side of the spinal canal. Anterolateral decompression is the most rational and effective method of treating active spinal tuberculosis with minimal complications.
Anterior Surgical Approaches and Procedures
An anterolateral approach is often used to treat thoracic and lumbar spinal tuberculosis and includes the following variations. Because the anatomical structure of the cervicothoracic spine is complicated, a low anterior cervical or trans‐sternal approach can be selected for C7–T2 according to the location of the manubrium. For spinal tuberculosis in T2 –4, surgeons can use a mid‐sternal, trans‐manubrial or trans‐sternal approach with partial resection of the clavicle. A transthoracic extrapleural approach is the best choice for spinal tuberculosis in T4 –10 because there is little associated surgical trauma and it has few complications. If pleural adhesion is severe and the pleura cannot be detached from the thoracic wall, thoracotomy is required. In patients with thoracolumbar spinal tuberculosis (T11–L2), a combined thoracic and abdominal, supraphrenic, or the infraphrenic approach can be used. For spinal tuberculosis involving the lumbar (lower than L3) and lumbosacral spine, an extraperitoneal approach can be used (Fig. 1).
Figure 1.
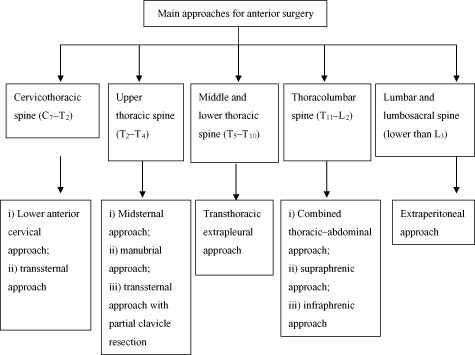
Main anterior surgical approaches for treating thoracic and lumbar spinal tuberculosis.
The main factors that should be considered when selecting an anterior approach are as follows: (i) selection of surgical approaches for the cervicothoracic (C7–T2) and upper thoracic spine (T2–T4) depends on the height of the manubrium; (ii) whether the bone lesion can be completely removed (site, severity, side and type of destruction,); (iii) whether or a cold abscess can be completely removed (size, number, origin, and side); (iv) whether decompression, deformity correction and bone grafting are likely to be effective; (v) minimizing the number of fixation segments, assuming stable internal fixation between affected vertebrae and short segments; and (vi) degree of difficulty of surgical approaches and the level of the surgeon's skill.
A combined thoracic and lumbar approach can be used in almost all patients with thoracolumbar spinal tuberculosis who require anterior spinal surgery. The anterolateral side of the spine superior to and including T12 can be reached via an extrapleural or transthoracic approach, whereas the anterolateral side of the spine inferior to and including L1 can be reached via an extraperitoneal approach. The attachments of the diaphragm to the spine and chest wall are then severed to connect the incisions in the chest and abdomen. This approach causes extensive surgical trauma and has many complications. If thoracic spinal tuberculosis and related surgical procedures do not involve the T12 vertebra or if lumbar spinal tuberculosis does not involve the L1 vertebra, the patient can be managed via a supradiaphragmatic or infradiaphragmatic approach, respectively, to reduce surgical trauma. However, a combined thoracic and lumbar approach is required if the spinal tuberculosis or surgical procedure involves T12–L1 (Fig. 2).
Figure 2.
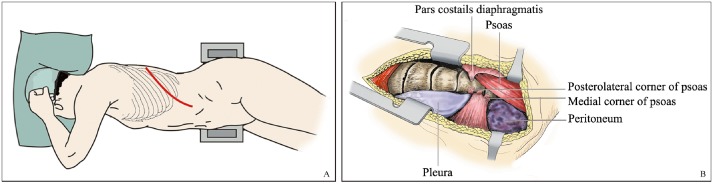
Combined thoracic‐abdominal approach. (A) The site of incision for removal of the 10th rib, suitable for treating spinal tuberculosis in T12–L1. (B) Via the above incision, the thoracic spine can be exposed via a transthoracic or extrapleural approach; below it, the lumbar spine can be exposed via an extraperitoneal approach; in the middle, the diaphragm can be cut open to connect the thoracic and lumbar segments.
A supradiaphragmatic approach is suitable for patients with spinal tuberculosis or surgical procedures that involve only the thoracolumbar spine superior to the T12 vertebra. A transthoracic or an extrapleural approach can be used. Surgeons can expose the T12 vertebra by severing the attachment of the diaphragm to the anterolateral portion of the T12 vertebral body and pushing the diaphragm away with a periosteal elevator. During this procedure, the attachment of the diaphragm to the chest wall remains intact, which may reduce surgical trauma compared with the conventional combined thoracic and abdominal approach (Fig. 3). The diaphragm is sutured on completion of surgery.
Figure 3.
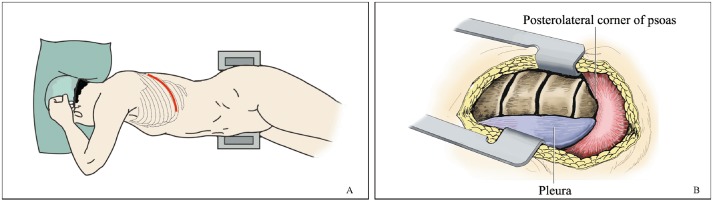
Supraphrenic approach. (A) The site of incision. The 10th rib is removed. (B) Exposure of the T12 vertebral body can be obtained by severing the attachment of the diaphragm from the anterolateral side of the vertebral body and pushing it inferiorly.
An infradiaphragmatic approach is suitable when the surgical procedure involves only the thoracolumbar spine inferior to the L1 vertebra. An extraperitoneal approach that removes the 12th rib can be used. After the L4 level has been reached, the crus of the diaphragm and the psoas muscle are severed from their attachments to the anterolateral portion of the L1 vertebra and pushed superiorly with a periosteal elevator. Extensive severing of the diaphragm's attachment to the chest wall should be avoided. Exposure of the supradiaphragmatic portion is not required; thus, the chest cavity and extrapleural space are not involved (Fig. 4). The crus of the diaphragm and the psoas muscle are sutured on completion of surgery.
Figure 4.
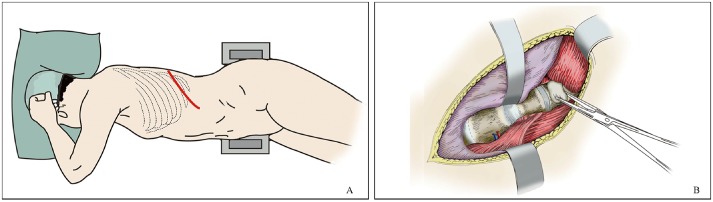
Infraphrenic approach. (A) The site of incision. The 12th rib is removed and an extraperitoneal approach chosen. (B) Exposure of the L1 vertebral body can be obtained by severing the crura of the diaphragm from the anterolateral side of the L1 vertebral body and pushing it superiorly.
Main Advantages of an Anterior Approach
Firstly, the lesion can be reached directly, and all five of the surgical procedures that may be required can be performed through the same incision, which simplifies the surgical process.
Secondly, complete debridement can be carried out. Debridement is the basis for and key point of the series of surgical procedures for spinal tuberculosis: failed debridement indicates an overall failure of surgical treatment. An anterior approach sufficiently exposes the anterolateral portion of the affected vertebra, allowing the surgeon to completely remove tuberculous bone lesions and cold abscesses in the paraspinal tissue, psoas muscle, iliac fossa and so on, leading to successful treatment.
Thirdly, spinal canal decompression can be safely and adequately performed. Because the spinal cord, cauda equina and nerve roots can be decompressed under direct vision, surgeons can remove the bone ridge, necrotic intervertebral disc, abscesses, granulation tissue, sequestrum and foci of caseous necrosis, thus achieving debridement and sufficient decompression while reducing interference with and accidental injury to the spinal cord and promoting functional recovery.
Fourthly, bone grafting is reliable, appropriate and associated with a high rate of healing. A graft bed suitable for the bone graft can be trimmed under direct vision. The bone graft can be tightly and properly embedded into the graft bed with moderate pressure to avoid undesirable situations such as poor bone‐to‐bone contact between the donor and recipient tissues, graft fracture and displacement and other complications, and to provide favorable conditions for bony fusion.
Main Disadvantages of an Anterior Approach
Firstly, relatively poor deformity correction is achieved. In patients with large‐angle kyphosis and active spinal tuberculosis or stationary kyphosis requiring osteotomy, an anterior approach cannot effectively correct the deformity and a posterior approach is required.
Secondly, the capacity to achieve internal fixation is limited. The length of the fixation segment should not be too long. In general, an anterior approach achieves a satisfactory outcome when the range of fixation is within three motion units; if the range of fixation is more than four motion units, standardized and reliable outcomes of fixation cannot be obtained by fixation devices that are currently available for anterior surgery. In addition, continuous dissection anterior to the spine and ligation of too many blood vessels can jeopardize blood supply to the spinal cord. To avoid this, posterior deformity correction and internal fixation should be carried out together with anterior debridement and bone graft fusion via a combined posterior–anterior approach2. When the T2 –4 and L5–S1 vertebrae are involved, the anterolateral structure is complicated, the exposure limited and achievement of internal fixation difficult. Some surgeons have reported trying new techniques; however, their results are not yet widely accepted3. The residual affected vertebra should be more than two‐thirds the height of a normal vertebra, otherwise the affected vertebra cannot accommodate currently available vertebral screws. If the fixation crosses the normal intervertebral spaces, the maximum span should not exceed one or two upper or lower segments adjacent to the affected vertebra in order to retain the normal motion units.
Thirdly, because the anterior approach is complicated, associated surgical trauma extensive and blood loss massive, the procedure requires skilled surgeons who are familiar with this approach. Because of the complicated anatomical structures, exposure of the vertebrae is risky. Moreover, the required preoperative investigations are complicated. Most patients should be admitted to the intensive care unit postoperatively.
Fourthly, many serious complications can occur. During anterior spinal surgery, surgeons must pay close attention to prevent the catastrophic results of some complications. First, there may be adhesion or displacement of the blood vessels anterior and lateral to the spine (for example, the iliac vessels may be pushed to the thin muscle layer in the lower abdominal wall by a large abscess in the iliac fossa). In severe cases, the blood vessel wall may have become fragile because it has been invaded by tuberculosis. Blood vessel injury most often occurs anterior to the lumbosacral and sacral segments. Second, the nerve plexus and the nerve stem, which are often wrapped in cold abscess and scar tissue, may easily be injured by rough manipulation. Third, although surgeons may improve chronic paraplegia caused by persistent anterior compression by careful intraoperative manipulation without touching the spinal cord, immediate spinal cord decompression should be carried out in patients with acute paraplegia to prevent a poor outcome.
Posterior Approach
The posterior approach is a surgical technique that involves debridement, spinal canal decompression, deformity correction, fusion and internal fixation via a posterior spinal approach. Except for the conventional thoracic approach that involves removing the rib head and transverse process, the current posterior surgical procedure for the treatment of spinal tuberculosis has been developed gradually based on experience gained by performing posterior osteotomies, a procedure that has been successfully used to correct spine kyphosis during the past decade. Mehta and Bhojraj first reported this surgical procedure in 200111 and recent studies involving it have been reported10, 11, 12, especially from China13, 14. Because lesions in the anterior vertebral body are removed via a posterior approach during this procedure, normal structures posterior to the spine are extensively damaged. Therefore, application of this procedure is controversial.
Indications for a Posterior Approach
The first indication is tuberculosis in the paraspinal soft tissue which, in most cases, can be treated by posterior debridement. If there is severe destruction of the paraspinal tissue and spinal stability is affected, reconstructive spinal surgery should be performed via an anterior or posterior approach. When tuberculosis in the paraspinal soft tissue has originated from the vertebral body, the affected vertebral body should be managed by an anterior or posterior approach.
A second indication is when destruction of the vertebral body is mild (<50%), and the lesion is be located posterior to one side of the vertebral body and close to the endplate. Posterior surgery should be performed from the posterolateral side to the anterior part of the vertebra. The manipulation is relatively difficult, the surgical procedure being greatly limited by muscles and ribs around the incision on both sides. Lesions close to the intervertebral disc in the coronal and sagittal planes can be removed easily. In the horizontal plane, a unilateral approach is appropriate when the lesion is located in the ipsilateral half of the vertebral body, whereas a bilateral approach is suitable when the tuberculosis involves nearly all the vertebral body.
The third indication is when there are few affected segments (one to two). When the lesions in the anterior part of the vertebral body must be reached via the dural sac or when part or all of the lamina, pedicle, and facet joints must be removed bilaterally, internal fixation devices cannot be placed in the affected vertebrae. In such cases, implants are placed in the adjacent normal vertebrae. Therefore, this method is not suitable when a large number of segments are affected.
A fourth indication is when there is no associated gravitation abscess and any psoas or paraspinal abscess is small. Gravitation and psoas abscesses cannot be completely removed via a posterior approach and removal of paraspinal abscesses is also very difficult via such an approach.
A fifth indication is patients who are not candidates for an anterior approach because of high surgical risk or difficulty in reaching the lesion. In cases with spinal tuberculosis in the lumbar and sacral segments, the anatomy of the large blood vessels is complicated, and there may be severe adhesions between the blood vessels and peripheral granulation tissue. In such cases, it may be difficult to reach the bone lesion. In addition, if blood vessel injury occurs, surgery via an anterior approach must be suspended and a posterior approach implemented.
Posterior Surgical Approaches and Procedures
Posterior surgical approaches for thoracic and lumbar spinal tuberculosis include posterior laminectomy and surgical approaches similar to those used for posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF). A transpedicular approach, thoracic approach that involves removing the rib head and the transverse process, trans‐scapular inferolateral approach, lateral extrapleural approach and posterior approaches all allow extensive resection14, 15 (Fig. 5). The surgical approaches depicted in this figure proceed from superficial to deep with increased depth and width for better posterolateral exposure, allowing surgeons to perform debridement, spinal canal decompression and bone graft fusion via a posterior approach. The main factors that should be considered when selecting an approach are as follows: (i) whether the bone lesion can be completely removed (site, severity, side and type of destruction); (ii) whether any cold abscess can be completely removed (size, number, origin, and side); (iii) whether decompression, deformity correction and bone grafting can be effectively performed; (iv) minimizing the number of fixation segments, assuming stable internal fixation between affected vertebrae and short segments; and (v) degree of difficulty of surgical approaches and the level of the surgeon's skill.
Figure 5.
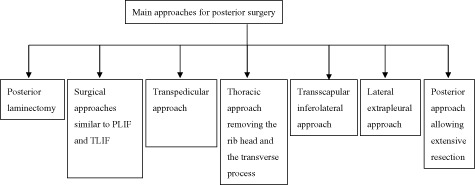
Main anterior surgical approaches for thoracic and lumbar spinal tuberculosis. From left to right, the surgical approaches range from superficial to deep with increased depth and width.
Laminectomy
Laminectomy exposes only the posterior part of the epidural space: the area anterolateral or anterior to the spinal cord cannot be reached by this approach. When the anterior part of the vertebral body is severely destroyed, laminectomy results in more serious spinal instability, aggravates pain, worsens kyphosis and induces secondary neurological damage. Therefore, laminectomy is appropriate mostly in cases of simple paraspinal tuberculosis and posterior spinal cord compression.
Surgical Approaches Similar to PLIF and TLIF
These surgical approaches provide satisfactory posterior exposure of the thoracic and lumbar spine and are especially suitable for lumbar spinal tuberculosis surgery12, 16. A conventional posterior midline incision is often used, and the erector spinae muscle is dissected routinely. Because lumbar spinal tuberculosis requires bilateral internal fixation, a posterior midline incision or bilateral incisions on each side of the spinous process are required for the Wiltse approach. After the muscle layer has been reached, manipulations can be performed on both sides of the spinous process and dissection performed between the longissimus and multifidus muscles to expose the transverse process and facet.
An approach similar to PLIF requires removing some parts of the spinous process, lamina and facet joint. In general, one‐half to three‐fourths of both facet joints should be removed; total facet joint resection is not recommended. Intervertebral space distraction is achieved using pedicle screws, after which debridement of the anterior lesion and bone grafting are performed. Because it is difficult to dissect the origins of the iliopsoas muscle from the L1 vertebra and diaphragm with this approach, it is usually reserved for lesions located inferior to the L2 vertebra.
There is a transforaminal approach similar to TLIF that reaches the affected vertebra(e) using a method similar to that of the PLIF approach. The difference is that the posterior surgical approach is more distal from the midline. Either one or both facet joints are removed. This procedure not only reduces muscle dissection during surgery but also reduces interference with nerves when surgeons expose the vertebrae and manage the intervertebral disc17. Thus, this approach is less likely to damage the spine and is relatively safe for nerves.
A transpedicular approach is suitable for thoracolumbar spinal tuberculosis with bilateral paraspinal abscesses together with serious kyphosis and posterior sinus formation when the intervertebral destruction is significantly asymmetrical. With this procedure one or both pedicles are removed posteriorly to reach the affected vertebra. Unilateral pedicle resection exposes the ipsilateral half or a little more than half of the affected vertebra, whereas bilateral pedicle resection exposes the whole vertebral body. Because of the rib and back muscles, it is difficult to implant a large iliac crest strut graft or a large cage via a transpedicular approach. Therefore, this approach is not suitable for patients who require a wide range of spinal reconstruction procedures because of severe vertebral body destruction18.
A unilateral transpedicular approach is suitable mainly for patients with unilateral vertebral body destruction with mild kyphosis. Only limited debridement can be carried out via this approach and wide‐range vertebral body reconstruction is not possible. When there is extensive bone destruction in the intervertebral disc and there is neurological dysfunction or obvious kyphosis associated with its upper and lower vertebrae, a bilateral transpedicular approach is needed19.
A thoracic approach that involves removing the rib head and transverse process is suitable for treating thoracic spinal tuberculosis that involves only one or two segments. It was initially used to drain paraspinal abscesses in patients with thoracic spinal tuberculosis. During the procedure, the medial 4 cm of rib and the rib head are removed to provide a better pathway for reaching the anterior vertebral body. Because of the large posterolateral space, it is easy to place the bone graft into the anterior defect. Debridement, nerve decompression, deformity correction and bone graft fusion can be performed through one simple incision. However, in patients with more severe destruction, the ribs and transverse processes should be removed bilaterally to sufficiently expose the anterior vertebral body, especially when the lesion is in the thoracic spine.
The trans‐scapular inferolateral approach was developed after 1964, when Hodgson reported a trans‐scapular low‐thoracic approach that involves removing the third rib and exposing the C7–T3 vertebrae posterior to the pleura20. The incision starts from the spinous process, extends around the posterior angle of the scapula, and moves forward along the fifth intercostal space. Some parts of the second to fifth ribs and muscles are severed transversely and raised to expose the thoracic spine. On the lateral side of the vertebral body, this approach can expose C3–T10 vertebrae by cephalic and caudal dissection.
A lateral extrapleural approach can be used for multi‐segmental thoracic and thoracolumbar spinal tuberculosis associated with severe deformity and spinal cord compression, especially when the lesion is in the thoracic spine. This approach involves a lateral expansion of the thoracic approach and removal of the relevant rib heads and transverse processes. Starting from the midline, 10–12 cm of the relevant ribs is removed. This approach provides a wide posterolateral space because removal of three to four consecutive ribs from the lateral side exposes the anterolateral sides of three to four vertebrae, making their en bloc resection possible; it also provides sufficient space for the placement of a strut graft. This procedure was initially used for debriding spinal tuberculosis. However, it is now used mainly to correct spinal deformity in patients with severe kyphosis and reconstruct spinal stability. Because there are few muscles on the anterolateral side of the thoracic spine and the intercostal nerves can be sacrificed, this approach is useful for exposing the thoracic spine. However, the presence of the scapula makes this approach unsuitable for spinal tuberculosis that involves the upper thoracic spine above T4.
In China, a posterior approach with extensive resection is commonly used to treat spinal tuberculosis. One or both spinous processes, laminas, transverse processes, facet joints, and pedicles can be removed to widely expose the dura mater via this approach. Debridement can be performed after the anterior part of the vertebral body has been reached via the pedicle; thus, deformity correction, decompression, bone grafting and internal fixation also can be carried out via this approach (Fig. 6). Most surgeons believe that this approach requires removing all the normal posterior structures and that the range of exposure is too large. Further studies are needed to identify ways of reducing surgical trauma.
Figure 6.
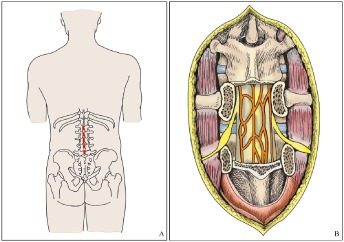
Posterior–lumbar approach with extensive resection. (A) A posterior midline incision is made, exposing two posterior structures of two adjacent affected vertebrae. (B) The accessories of two adjacent vertebrae are removed and the affected vertebrae reached via a posterior approach.
Main Advantages of Posterior Surgery
A one‐step surgical procedure including debridement, spinal canal decompression, bone graft fusion, deformity correction and internal fixation can be performed via a posterior approach, which simplifies the surgical process. Posterior internal fixation provides better biomechanical stability than can be achieved via an anterior approach. Therefore, posterior surgical correction is preferred over an anterior approach and the resultant fixation is more solid. If multisegment fixation is needed, the range of internal fixation can be extended superiorly and inferiorly. The anatomical structures accessed via a posterior approach are not as complicated as those accessed via an anterior approach, and the main structures are therefore less easily injured. Internal fixation devices can be easily removed after healing. Thoracic approaches that involve removing the rib and transverse process and lateral extrapleural approaches are extrapleural procedures that are more suitable for patients with pulmonary tuberculosis. Surgical trauma is relatively mild and the complications of thoracic and abdominal surgeries can be avoided.
Main Disadvantages of Posterior Surgery
Debridement, spinal canal decompression and bone graft fusion cannot be performed under direct vision during posterior surgery except for when a lateral extrapleural approach is used; this affects the outcome of surgery to some extent.
Second, the lesion cannot be completely removed. Both the unilateral and bilateral approaches make manipulation of the anterior part of the vertebral body difficult and the surgeon cannot accurately determine whether the bone lesion should be removed or preserved. Psoas, paraspinal and gravitation abscesses cannot be removed completely, and bone lesions and cold abscesses may be missed.
Third, appropriate and moderate bone graft fusion cannot be achieved and placement of strut grafts is relatively difficult.
Fourth, the required internal fixation may be too long to achieve via this approach. If too many adjacent pedicles and facet joints are removed, internal fixation cannot be performed over the affected vertebrae and adjacent normal segments. In addition, normal segments distal to the affected vertebra may require interventions, resulting in long‐segment internal fixation across multiple normal motion units. This inevitably affects the normal motion of the spine and sometimes exacerbates adjacent segment degeneration.
Fifth, surgical procedures on consecutive elements of multi‐segment spinal tuberculosis become more difficult. It is difficult to control relatively massive bleeding originating from blood vessels around the vertebra and within the spinal canal.
Current issues regarding posterior surgery include the following: the surgical indications are too extensive; the outcomes are poor; and internal fixation involves excessively long segments. More effective and reasonable surgical procedures should be further investigated.
Combined Posterior–Anterior Surgery
During combined posterior–anterior surgery, deformity correction and internal fixation are performed via a posterior approach, after which debridement, spinal canal decompression and bone graft fusion are performed via an anterior approach. Combined posterior–anterior surgery takes advantage of both the posterior approach for deformity correction and internal fixation and the anterior approach for debridement, decompression and bone graft fusion16, 21, 22. Moreover, this procedure avoids the disadvantages of both the anterior and the posterior approach. Because this technique is more rational and effective, it is commonly used in clinical practice. Approximately 98% of surgeries for spinal tuberculosis are performed via a combined posterior–anterior approach23.
Indications for Combined Posterior–Anterior Surgery
There is a broad range of indications for combined posterior–anterior surgery: this approach is suitable for most patients with spinal tuberculosis24, 25, 26. This procedure is especially suitable where long segments are involved or lesions have caused severe destruction, secondary surgery and cases that cannot be effectively treated by simple anterior or simple posterior surgery.
Approaches and Procedures for Combined Posterior–Anterior Surgery
During combined posterior–anterior surgery, selection of a one‐stage or two‐stage procedure depends mainly on the patient's nutritional status, general condition, presence of associated diseases in the vital organs, and whether the patient can tolerate general anesthesia. A precise and detailed surgical plan should be formulated before embarking on combined posterior–anterior surgery. The main issues that should be clarified preoperatively include the following: range of debridement and amount of reactive bone and intervertebral space that can be preserved; approximate length of the bone graft and segments to be crossed; lesions to be removed for decompression and their ranges; site, length, quantity and methods for placing internal fixation devices; and the methods for and desired outcomes of deformity correction. Successful performance of this procedure relies on sufficient preoperative preparation.
Because the pedicles are intact in most patients with spinal tuberculosis, a pedicle screw–rod system is commonly used for posterior internal fixation, which can be performed by open or minimally invasive surgery. If pedicle screw insertion is not possible, a posterior hook–rod internal fixation system can be selected. In patients with active spinal tuberculosis, deformity correction can be carried out by a procedure that combines postural reduction, manual reposition and instrumentation; a satisfactory outcome can be obtained in most cases. A few patients with active spinal tuberculosis and associated fusion of the affected vertebrae and patients with static kyphosis can be treated by posterior osteotomy.
The posterior internal fixation technique of posterior–anterior surgery differs from that of simple posterior surgery. During simple posterior surgery, pedicles and other attachments of the affected vertebra are removed for sufficient exposure. Thus, internal fixation devices cannot be placed in the affected vertebra; these devices must be implanted in the normal adjacent segments. However, posterior spine structures are not destroyed during posterior–anterior surgery, most pedicles of the affected vertebrae are intact and reliable internal fixation is possible. To date, the most taxing problem in internal fixation for spinal tuberculosis is the excessively long fixation range required. To ensure achievement of solid fixation, normal motion units should ideally not be fixed; if such fixation is deemed necessary, the number of fixed normal segments should be minimized. Thus, in patients with spinal tuberculosis, internal fixation should be carried out between as few affected vertebrae as possible. In those with simple‐segment or multisegment spinal tuberculosis, surgeons should treat the affected vertebrae after removing the lesion without interfering with normal motion units. Specifically, deformity correction is less effective in the thoracic than in the lumbar spine because the ribs are connected to the spine and sternum. Therefore, internal fixation should fix not only the affected vertebrae, but also one to two superior and inferior normal intervertebral spaces. In contrast, in the lumbar spine it is unnecessary to fix normal intervertebral spaces; only the affected intervertebral space should be fixed. This applies to both simple‐segment and multisegment spinal tuberculosis.
Regarding anterior debridement, spinal canal decompression and bone graft fusion, the procedure for the anterior component of the combined posterior–anterior approach is basically similar to that of simple anterior surgery. Because anterior fixation is not required, only the anterolateral side of the affected vertebra should be exposed; it is not necessary to expose normal intervertebral spaces and vertebrae.
During combined posterior–anterior surgery, removal of the lesion should be in accordance with the principle of complete debridement: Lesions should not only be removed as completely as possible in the conventional sense: the sclerotic wall, cavity and diseased bone bridge should also be removed. Spinal canal decompression and bone graft fusion should be carried out in the same manner as with simple anterior surgery.
Combined posterior–anterior surgery overcomes the disadvantages of simple anterior and simple posterior surgery: the design is rational, it is widely appropriate, being perhaps the most useful surgical procedure for treating spinal tuberculosis. This procedure characteristically has comprehensively good outcomes, including healing of lesions, bone graft fusion, deformity correction, functional recovery of the spinal cord and reduced duration of rehabilitation. The component of anterior debridement allows complete removal of lesions without removal of excessive amounts of reactive bone. Decompression under direct vision is safer and more complete. Preparation of the graft bed and bone grafting are more reliable, and falling off or tilting of the bone graft rarely occurs, which enhances bone healing. Further, posterior deformity correction can be achieved, as can reliable posterior internal fixation and fixation of the affected vertebrae, which together reduce the number of fixation segments, preserve normal spinal motion units, and prevent or decrease occurrence of adjacent segment degeneration. In addition, early ambulation and prompt rehabilitation are possible.
Disadvantages of Combined Posterior–Anterior Surgery
The required two incisions result in massive surgical trauma, high complication rates, and high medical costs. Further, two‐stage surgery prolongs the length of stay and requires a highly skilled surgeon. In some cases, the outcome of deformity correction is compromised because posterior deformity correction was performed before anterior debridement and loosening of the bone bridge.
Conclusions
When surgeons select surgical procedures for patients who present with thoracic and lumbar spinal tuberculosis, they should give comprehensive consideration to the patient's general condition and comorbidities, manifestations of the lesion(s) and their degree of familiarity with the surgical procedures that may be required27. Among the surgeon's considerations, the first should be the potential outcome: the effectiveness of debridement is the key to this because failed healing of the lesion undoubtedly means failure of the entire intervention. Anterior, posterior and a combination of posterior–anterior surgeries all have their own shortcomings that the clinician must evaluate. We should not expect one surgical procedure to be applicable all kinds of spinal tuberculosis28. In addition, we also should not believe that a certain kind of surgical procedure is better than others simply because a group of patients has been treated successfully with it—any comparisons of interventions should be verified by large, multicenter, prospective studies.
Disclosure: The submitted manuscript does not contain information regarding medical equipment. This work is not supported by any foundation and does not directly or indirectly have any formal relationships with business groups.
References
- 1. Ge Z, Wang Z, Wei M. Measurement of the concentration of three antituberculosis drugs in the focus of spinal tuberculosis. Eur Spine J, 2008, 17: 1482–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wang Z, Shi J, Geng G, Qiu H. Ultra‐short‐course chemotherapy for spinal tuberculosis: five years of observation. Eur Spine J, 2013, 22: 274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shi J, Wang Z, Li H, Yuan H. Diagnostic performance of the urinary deoxypyridinoline in spinal tuberculosis. Orthopedics, 2012, 35: e922–e926. [DOI] [PubMed] [Google Scholar]
- 4. Wang ZL, Wang Q. Operation strategy of spinal tuberculosis. Zhonghua Gu Ke Za Zhi, 2010, 30: 717–723 (in Chinese). [Google Scholar]
- 5. Wang ZL. Rational choice of operation approach for spinal tuberculosis. Zhongguo Ji Zhu Ji Sui Za Zhi, 2012, 22: 769–710 (in Chinese). [Google Scholar]
- 6. Bezer M, Kucukdurmaz F, Aydin N, Kocaoglu B, Guven O. Tuberculous spondylitis of the lumbosacral region: long‐term follow‐up of patients treated by chemotherapy, transpedicular drainage, posterior instrumentation, and fusion. J Spinal Disord Tech, 2005, 18: 425–429. [DOI] [PubMed] [Google Scholar]
- 7. Wang YN, Yang Y, Xiao W, et al Meta analysis of different operation approach for the treatment of adult thoracolumbar tuberculosis treatment. Zhonghua Gu Ke Za Zhi, 2013, 21: 658–662 (in Chinese). [Google Scholar]
- 8. Chen X, Yu FY, Ma YZ, et al One stage anterior operation for treatment of thoracic and thoracolumbar spinal tuberculosis. Ji Zhu Wai Ke Za Zhi, 2010, 8: 356–358. (in Chinese). [Google Scholar]
- 9. Shi JD, Wang ZL, Geng GQ, Niu NK. Intervertebral focal surgery for the treatment of noncontiguous multifocal spinal tuberculosis. Int Orthop, 2012, 36: 1423–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mehta JS, Bhojraj SY. Tuberculosis of the thoracic spine. A classification based on the selection of surgical strategies. J Bone Joint Surg Br, 2001, 83: 859–863. [DOI] [PubMed] [Google Scholar]
- 11. Luk KD. Commentary: instrumentation in the treatment of spinal tuberculosis, anterior or posterior? Spine J, 2011, 11: 734–736. [DOI] [PubMed] [Google Scholar]
- 12. Zaveri G. The role of posterior surgery in spinal tuberculosis. AEGOSpine News J, 2011, 23: 112–119. [Google Scholar]
- 13. Zhang HQ, Wang YX, Guo CF, et al One stage posterior debridement, fusion and internal fixation for the treatment of children thoracolumbar spinal tuberculosis with kyphosis: a preliminary report. Zhonghua Jiao Xing Wai Ke Za Zhi, 2011, 19: 31–35 (in Chinese). [Google Scholar]
- 14. Zhang H, Huang S, Guo H, et al A clinical study of internal fixation, debridement and interbody thoracic fusion to treat thoracic tuberculosis via posterior approach only. Int Orthop, 2012, 36: 293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kato S, Kawahara N, Murakami H, et al Extensive thoracolumbar spinal tuberculosis treated with two‐stage surgery using a minimally invasive posterior instrumentation. Eur J Orthop Surg Traumatol, 2011, 21: 407–409. [Google Scholar]
- 16. Lee SH, Sung JK, Park YM. Single‐stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: a retrospective case series. J Spinal Disord Tech, 2006, 19: 595–602. [DOI] [PubMed] [Google Scholar]
- 17. Garg B, Kandwal P, Nagaraja UB, Goswami A, Jayaswal A. Anterior versus posterior procedure for surgical treatment of thoracolumbar tuberculosis: a retrospective analysis. Indian J Orthop, 2012, 46: 165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jain AK, Dhammi IK, Jain S, Kumar J. Simultaneously anterior decompression and posterior instrumentation by extrapleural retroperitoneal approach in thoracolumbar lesions. Indian J Orthop, 2010, 44: 409–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. He B, Hu Z, Hao J, Liu B. Posterior transpedicular debridement, decompression and instrumentation for thoracic tuberculosis in patients over the age of 60. Arch Orthop Trauma Surg, 2012, 132: 1407–1414. [DOI] [PubMed] [Google Scholar]
- 20. Fang HS, Ong GB, Hodgson AR. Anterior spinal fusion: the operative approaches. Clin Orthop Relat Res, 1964, 35: 16–33. [PubMed] [Google Scholar]
- 21. Wang Z, Yuan H, Geng G, Shi J, Jin W. Posterior mono‐segmental fixation, combined with anterior debridement and strut graft, for treatment of the mono‐segmental lumbar spine tuberculosis. Int Orthop, 2012, 36: 325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Talu U, Gogus A, Ozturk C, Hamzaoglu A, Domanic U. The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis: experience of 127 cases. J Spinal Disord Tech, 2006, 19: 554–559. [DOI] [PubMed] [Google Scholar]
- 23. Wang Z, Wu Q, Geng G. Anterior debridement and bone grafting with posterior single‐segment internal fixation for the treatment of mono‐segmental spinal tuberculosis. Injury, 2013, 44: 253–257. [DOI] [PubMed] [Google Scholar]
- 24. Jin W, Wang Z. Clinical evaluation of the stability of single segment short pedicle screw fixation for the reconstruction of lumbar and sacral tuberculosis lesions. Arch Orthop Trauma Surg, 2012, 132: 1429–1435. [DOI] [PubMed] [Google Scholar]
- 25. Wang XB, Li J, Lü GH, Wang B, Lu C, Kang YJ. Single‐stage posterior instrumentation and anterior debridement for active tuberculosis of the thoracic and lumbar spine with kyphotic deformity. Int Orthop, 2012, 36: 373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hirakawa A, Miyamoto K, Masuda T, et al Surgical outcome of 2‐stage (posterior and anterior) surgical treatment using spinal instrumentation for tuberculous spondylitis. J Spinal Disord Tech, 2010, 23: 133–138. [DOI] [PubMed] [Google Scholar]
- 27. Pu X, Zhou Q, He Q, et al A posterior versus anterior surgical approach in combination with debridement, interbody autografting and instrumentation for thoracic and lumbar tuberculosis. Int Orthop, 2012, 36: 307–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br, 2010, 92: 905–913. [DOI] [PubMed] [Google Scholar]


