Abstract
Objective
The hypothesis of this study is that pelvic obliquity (PO) is associated with specific patterns of degenerative scoliosis.
Methods
This study was a retrospective case series of consecutive patients undergoing fusion for lumbar conditions (degenerative scoliosis or spondylolisthesis). The discrepancy in the iliac crest height, coronal L1‐S1 endplate angles, distance from L1 coronal bisector to the sacral center, number of degenerative scoliosis curves, and individual curve angulations were measured.
Results
Limb length discrepancy was present in 87% of patients with a degenerative scoliosis. There were 116 patients with a single curve > 5° and PO > 2 cm. Of the patients with a single curve, the apex of scoliosis was opposite the high iliac crest side in 79% patients. There were 338 patients with a double curve. The apex of scoliosis was opposite the high iliac crest side in 48% of patients.
Conclusion
There were distinct patterns of limb length discrepancy corresponding to degenerative scoliotic curve morphology. In patients with single degenerative scoliotic curves, PO most commonly appeared to counteract the scoliotic curve and result in an overall decrease in trunk shift. This occurred because the high iliac crest was observed most commonly on the convex side of the scoliotic curve. This effect was not observed in double lumbar degenerative scoliotic curves.
Keywords: Hip spine syndrome, Lumbar deformity, Pelvic obliquity, Scoliosis
Introduction
Degenerative scoliosis is a common condition in elderly patients. According to one study, the incidence of degenerative scoliosis among the elderly is 35.5%1. The degenerative deformity may occur due to disk space obliquity, bony deformity, and/or lateral listhesis. Several authors have proposed rotary subluxation as the inciting event in the induction of de‐novo scoliosis2, 3. However, it is unknown why some patients develop isolated spondylosis without deformity and other patients develop degenerative scoliosis.
Leg length discrepancy is a frequent condition, present in 3%–15% of the population, and in most cases, its cause is unknown4. In a study done on children aged 5–17 years, it was shown that even a slight primary leg length discrepancy (LLD) can cause functional scoliosis during growth, and may require equalization treatment to prevent postural deterioration4. In the adult population, elderly patients often develop secondary limb length discrepancy during the course of development of hip osteoarthritis. In most cases, limb length discrepancies less than 2.5 mm are considered to be asymptomatic.
The hypothesis of this study was that degenerative scoliosis is a compensatory deformity secondary to pelvic obliquity (PO). Specifically, we sought to identify: (i) the incidence of PO in patients undergoing lumbar fusion; (ii) the relationship of PO to overall coronal spine alignment; and (iii) whether PO corresponds to scoliosis in a defined relationship (e.g. PO complements deformity in single curves but not double lumbar degenerative curves). To determine whether PO counteracted or exacerbated coronal imbalance from degenerative scoliosis, patients with degenerative scoliosis were grouped into single and two degenerative scoliotic curve categories (Fig. 1). Curve patterns were further described as to whether the high iliac crest side was on the concave or convex sides of the degenerative scoliotic curve (Fig. 2). In double lumbar curves, the patients were classified according to whether the high side was on the concave or convex side of the lower curve (Fig. 3).
Figure 1.
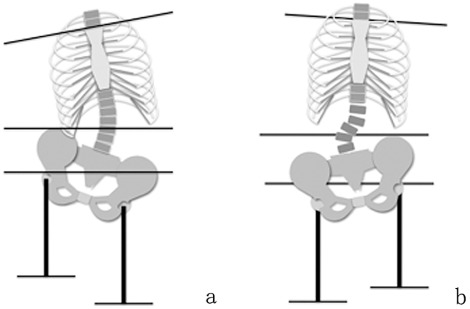
(a) Single degenerative scoliotic curve. This demonstrates a left apex of curvature, high right iliac crest, high right acetabulum, and horizontal line at superior surface of manubrium to further illustrate upper torso side bending due to scoliotic curve. Lines drawn perpendicular to the ground up to the acetabulum represent the whole leg to foot appendage, each line was made as a duplicate so as to prevent differences in length when drawing each leg to foot appendage (left image). (b) Double degenerative scoliotic curve. This demonstrates a right lower apex lumbar curve and a left upper apex lumbar curve, high left iliac crest, high left acetabulum.
Figure 2.
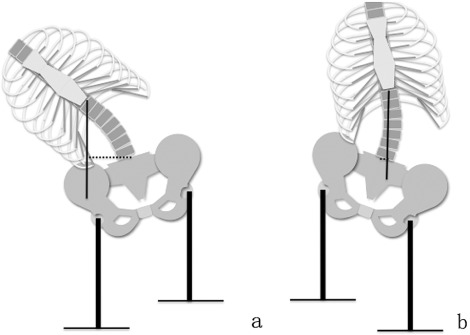
(a) Uncompensated single curve. Here the pelvic obliquity exacerbates trunk shift created by the degenerative scoliotic curve. Single curve with high left pelvic side ipsilateral to the single left apex lumbar curve, horizontal line demonstrating distance from center sacral line to L1 coronal bisector. (b) Compensated single curve. The pelvic obliquity counteracts the effect of trunk shift that would be created by the degenerative scoliotic curve. Single curve with high right pelvic side contralateral to the single left apex lumbar curve, horizontal line demonstrating distance from center sacral line to L 1 coronal bisector.
Figure 3.
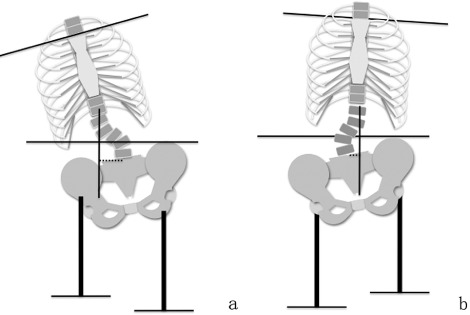
(a) Uncompensated double curve. Here the pelvic obliquity exacerbates trunk shift created by the degenerative scoliotic curve. Double curve with high left pelvic side ipsilateral to the lower left apex lumbar curve and contralateral to the upper right apex lumbar curve. (b) Compensated double curve. The pelvic obliquity counteracts the effect of trunk shift that would be created by the degenerative scoliotic curve. Double curve with high left pelvic side contralateral to the lower right apex lumbar curve and ipsilateral to the upper left apex lumbar curve.
Materials and Methods
The eligible population was a retrospective series of 2562 consecutive patients with lumbar deformity. Inclusion criteria were patients who underwent lumbar fusion from January 1, 2010 to December 31, 2010 for degenerative scoliosis or degenerative spondylolisthesis. Patients were selected using ICD‐9 coding from billing records of an orthopedic‐spine practice. Ultimately, there were 741 eligible patients. Patients with prior lumbar surgery or lower extremity surgery [hip replacement, hip open reduction (with) internal fixation (ORIF), femur ORIF] or incomplete data (such as incomplete radiographs) were excluded (85 patients). Ultimately, there were 656 patients who constituted the study population.
Lumbar deformity was measured on all patients (Fig. 4). The L1‐S1 Cobb endplate angles, distance from L1 coronal bisector to center sacral vertical line, number of degenerative scoliotic curves, and, if more than one curve was present, individual curve Cobb angle of each curve (such as L4‐S1) were measured. The trunk alignment was measured using the distance from the L1 coronal bisector to the center sacral vertical line.
Figure 4.
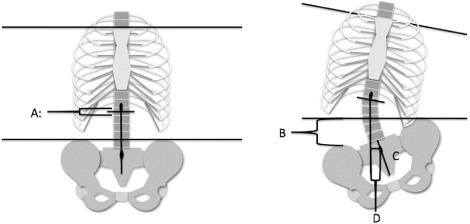
Demonstration of measurement parameters (measurements made upon X‐rays for respective subject) A: L 1 coronal bisector, drawn from T 12 spinous process perpendicular to the floor (left image); B: Difference in iliac crest height, measured by using horizontal line as baseline for measurement of height differences; C: Center sacral vertical line, drawn perpendicular to the S 1 end‐plate through the S 1 spinous process to the coccygeal tip; D: Distance between coronal bisector and “posterior” S 2 spinous process, measured by drawing horizontal line perpendicular to L 1 coronal bisector (A) to the center sacral vertical line intersection with the S 1 spinous process (C).
The PO was measured in all patients. Since full‐length lower extremity scanograms were not available, PO was measured as the difference in the heights of the iliac crests. The difference in iliac crest heights was measured using tangent lines to the left and right iliac crests (Fig. 4).
Statistics were calculated using SPSS 18.0. Pearson's correlation coefficient was used to determine the relationship between radiographic parameters. The association between high side and curve morphology (concave or convex side) in different curve patterns (single versus double curves) was compared using Fisher exact test.
Results
There were 656 patients in the study population (mean age, 58.77 years; 205 single curve and 451 double curve). Of these, there were 524 patients with degenerative scoliosis >5° (127 single scoliotic curve and 397 double scoliotic curve). The mean age of subjects meeting the exclusion criteria was 60.73 years old (85 patients). The population consistent was 43.5% male and 56.5% female.
The prevalence of PO in patients with a single degenerative scoliotic curve was 91% (116/127). Mean curvature was 10° (SD, 5°). The single curve population was 55% male and 45% female (Table 1). Mean age was 58.2 years. The high iliac crest side was on the concave curve side in 79% (92/116) of patients. The coronal bisector was on the concave curve side in 68% (79/116) of patients and on the low hemipelvis side in 49% (57/116) of patients. There was a weak correlation between Cobb angle and iliac crest height difference (r = −0.53, P < 0.05), Cobb and coronal bisector displacement (r = −0.32, P < 0.05), but not coronal bisector displacement and iliac crest height difference (r = −0.009, P > 0.05).
Table 1.
Single curve data of 205 cases (mean ± s.d.)
| Sex | Age (years) | Hip height (mm) | Acetabulum height (mm) | Total curvature (°) |
|---|---|---|---|---|
|
Male (114 cases) |
57.25 ± 12.93 | 8.86 ± 5.81 | 7.42 ± 5.38 | 7.85 ± 5.64 |
|
Female (91 cases) |
57.50 ± 13.58 | 7.67 ± 5.78 | 7.50 ± 5.40 | 7.59 ± 5.37 |
The prevalence of PO in patients with double scoliotic curves was 85% (338/397). The double curve population was 46% male and 54% female (Table 2). Mean age was 61 years. Mean curvature was 14° (SD, 9°). The high side was on the concave side of the lower degenerative scoliotic curve in 48% (161/338) of patients. The coronal bisector was on the concave side of the lower curve in 72% (244/338) of patients and on the low hemipelvis side in 71% (240/338) of patients. There was no significant correlation between iliac crest height difference and Cobb angle of lower curve (r = −0.007, P > 0.05). There was a significant correlation between the coronal bisector displacement and Cobb angle of lower curve (r = 0.29, P > 0.05) and between coronal bisector displacement and iliac crest height difference (r = 0.14, P > 0.05).
Table 2.
Double curve data of 451 cases (mean ± s.d.)
| Sex | Age (years) | Hip height (mm) | Acetabulum height (mm) | L1–4 curvature (°) | L4‐S1 curvature (°) |
|---|---|---|---|---|---|
|
Male (236 cases) |
57.78 ± 13.30 | 8.51 ± 5.60 | 7.42 ± 4.95 | 5.15 ± 4.63 | 9.20 ± 3.82 |
|
Female (215 cases) |
61.22 ± 13.64 | 7.07 ± 4.80 | 6.44 ± 4.84 | 7.41 ± 7.72 | 6.00 ± 4.89 |
There were statistically significant differences in the location of the curve apex versus PO in patients with single and double lumbar degenerative scoliotic curves. The high iliac crest side was significantly more likely to occur on the concave scoliotic curve side in patients with single curves (79%) versus double curves (48%, P = 0.001, Fisher exact test). Patients with double curves (72%) were significantly (P = 0.0001, Fisher exact test) more likely than patients with single curves (49%) to have the low iliac crest on the same side as the coronal bisector. There were no statistically significant differences in relationship of coronal bisector displacement and location on the concave side of curve between patients with single (68%) and double (71%) curves (P = 0.64, Fisher exact test).
Discussion
These results suggest that PO is a common compensatory phenomenon for degenerative scoliosis in some cases. The prevalence of PO in patients with degenerative scoliosis was 87% (454/524). There were distinct patterns of limb length discrepancy corresponding to degenerative scoliotic curve morphology. Patients with single curves were more likely (79%) to have compensatory PO opposite the apex of the curvature (Fig. 3b) that tended to reduce overall coronal imbalance compared to patients with double curves (48%). In patients with single curves, the curve Cobb angle corresponded to the degree of pelvic obliquity and the degree of trunk shift (coronal bisector displacement). In patients with double curves there was no clear pattern of PO and curve morphology. However, the coronal bisector was more likely to be on the low side in patients with double curves (Fig. 3a) suggesting that PO exacerbated coronal imbalance. These findings suggest that double curves are less likely to have a compensatory function and that PO has a significant role in trunk shift in these patients.
Given these findings, we speculate that single degenerative scoliotic curves are more rare and in fact may develop as compensatory mechanisms for PO (Fig. 5). Double curves may develop due to primary lumbar degenerative pathology independent of PO (Fig. 6). Previous studies have shown correlations between limb length discrepancy and spinal abnormalities. Specht and De Boer observed that either scoliosis or hypo‐hyper lordosis occurs in over half of patients who have leg length discrepancy (LLD) greater than 6 mm5. Correction of LLD through the use of under‐foot wedges has also been found to show significant postural improvements when used to treat patients with concurrent scoliosis6. The LLD observed in this study (2 mm) was significantly less than that considered to be clinically significant in previous investigations7, 8. However, as full length scanograms were not available in this study, we were only able to evaluate difference in iliac crest heights. This radiographic difference does not take into account hip or knee flexion contractures that may mimic limb length discrepancy8, 9, 10. However, whether or not such minimal discrepancies contribute to the development or perpetuation of spinal abnormalities has yet to be elucidated.
Figure 5.

Compensated single curve example. The patient has a 4.1 mm iliac crest height discrepancy (right side higher) that counteracts the effects of the 12.4° apex left degenerative scoliotic single curve.
Figure 6.

Uncompensated double curve. The patient has an 8.3 mm iliac crest height discrepancy (left side higher) that exacerbates the lower 9.4° apex left scoliotic curvature.
Hip‐spine syndrome is a common, poorly understood clinical phenomenon in which reconstruction of the hip or lumbar spine leads to the rapid development of symptomatic degeneration in the other organ. These findings, that suggest a relationship between degenerative lumbar pathology and pelvic parameters, may provide an explanation of the underlying mechanism of hip spine syndrome. Correction of PO (from a total hip replacement) or degenerative scoliosis (with a fusion) may upset the compensatory relationship between pelvic parameters and lumbar deformity. Based on these results, we recommend future studies to determine whether fixed PO is a risk factor for adjacent segment breakdown or development of sacroiliac joint pathology following lumbar fusion.
These results are consistent with previous studies on this topic that confirm an association between limb length discrepancy and scoliosis magnitude11. Previous studies on this topic have mostly evaluated PO in adolescent idiopathic curves. However, PO was not a significant factor corresponding to coronal balance (L1 coronal bisector to center sacral vertical line distance) in either single or double lumbar degenerative curves.
Limitations of this study include the retrospective nature of the analysis. Furthermore, there is a possibility of selection bias as indications for lumbar fusion at our institution include coronal or sagittal deformity. Additionally, there is a possibility that patients may have false limb length discrepancy due to PO from hip or knee flexion contractures and not a true bony limb length discrepancy. Patients with degenerative scoliosis may develop compensatory hip flexion contractures, creating false PO to maintain coronal balance12. For the purposes of this study, however, we would argue that it is important that surgeons consider either structural or compensatory PO (due to a flexion contracture) prior to hip or spine reconstruction. As this was a retrospective analysis of patients selected to undergo lumbar fusion, it was not possible to evaluate full‐length lower extremity length with scanograms to distinguish true LLD from extremity flexion contracture. However, the lumbar spine radiographic technique includes evaluating patients in full extension of the hips and knees to remove the compensatory effect of PO.
In conclusion, there was a high incidence of PO in patients with degenerative scoliosis. Based on these results, we recommend that surgeons carefully consider the effect of PO and possible LLD prior to lumbar reconstruction since lumbar degenerative curves may serve a compensatory function due to PO. Additionally, future prospective studies should evaluate whether small limb length discrepancies previously considered to be clinically insignificant may actually contribute to the pathogenesis of degenerative lumbar scoliosis.
Disclosure: Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article. This work was approved by the institutional review board of Thomas Jefferson University. The manuscript submitted does not contain information about medical device(s)/drug(s). No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1. Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH. The prevalence and radiological findings in 1347 elderly patients with scoliosis. J Bone Joint Surg Br, 2010, 92: 980–983. [DOI] [PubMed] [Google Scholar]
- 2. Marty‐Poumarat C, Scattin L, Marpeau M, Garreau de Loubresse C, Aegerter P. Natural history of progressive adult scoliosis. Spine (Phila Pa 1976), 2007, 32: 1227–1234. [DOI] [PubMed] [Google Scholar]
- 3. Watanuki A, Yamada H, Tsutsui S, En‐yo Y, Yoshida M, Yoshimura N. Radiographic features and risk of curve progression of de‐novo degenerative lumbar scoliosis in the elderly: a 15‐year follow‐up study in a community‐based cohort. J Orthop Sci, 2012, 17: 526–531. [DOI] [PubMed] [Google Scholar]
- 4. Raczkowski JW, Daniszewska B, Zolynski K. Functional scoliosis caused by leg length discrepancy. Arch Med Sci, 2010, 6: 393–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Specht DL, De Boer KF. Anatomical leg length inequality, scoliosis and lordotic curve in unselected clinic patients. J Manipulative Physiol Ther, 1991, 14: 368–375. [PubMed] [Google Scholar]
- 6. D'Amico M, Roncoletta P, Di Felice F, Porto D, Bellomo R, Saggini R. Leg length discrepancy in scoliotic patients. Stud Health Technol Inform, 2012, 176: 146–150. [PubMed] [Google Scholar]
- 7. Offierski CM, MacNab I. Hip‐spine syndrome. Spine (Phila Pa 1976), 1983, 8: 316–321. [DOI] [PubMed] [Google Scholar]
- 8. Juhl JH, Ippolito Cremin TM, Russell G. Prevalence of frontal plane pelvic postural asymmetry–part 1. J Am Osteopath Assoc, 2004, 104: 411–421. [PubMed] [Google Scholar]
- 9. Aldegheri R, Agostini S. A chart of anthropometric values. J Bone Joint Surg Br, 1993, 75: 86–88. [DOI] [PubMed] [Google Scholar]
- 10. Hackenberg L, Hierholzer E, Bullmann V, Liljenqvist U, Götze C. Rasterstereographic analysis of axial back surface rotation in standing versus forward bending posture in idiopathic scoliosis. Eur Spine J, 2006, 15: 1144–1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Archer IA, Dickson RA. Stature and idiopathic scoliosis. A prospective study. J Bone Joint Surg Br, 1985, 67: 185–188. [DOI] [PubMed] [Google Scholar]
- 12. Kilshaw M, Baker RP, Gardner R, Charosky S, Harding I. Abnormalities of the lumbar spine in the coronal plane on plain abdominal radiographs. Eur Spine J, 2011, 20: 429–433. [DOI] [PMC free article] [PubMed] [Google Scholar]


