Key Points
Question
What are the attitudes of older Americans toward deprescribing?
Findings
In this population-based study of a nationally representative sample of older Medicare beneficiaries, 92.0% reported being willing to stop taking 1 or more of their medicines if their physician said it was possible, and 66.6% wanted to reduce the number of medicines that they were taking. Characteristics of older adults that were related to these attitudes included number of medications taken and number of medical conditions.
Meaning
Physicians should be reassured that most older patients are open to deprescribing their medications within the framework of patient-centered care and shared decision making.
This population-based survey study uses data from the US National Health and Aging Trends Study to describe the attitudes of older Medicare beneficiaries toward deprescribing and whether individual characteristics are associated with these attitudes.
Abstract
Importance
Use of harmful and/or unnecessary medications in older adults is prevalent. This can lead to avoidable harms such as adverse drug reactions, falls, hospitalization, and mortality. Primary care physicians report that patient resistance to discontinuing medication use is a significant barrier to deprescribing.
Objective
To describe the attitudes of older adults toward deprescribing and to determine whether individual characteristics are associated with these attitudes.
Design, Setting, and Participants
For this population-based survey study of US Medicare beneficiaries 65 years and older, data were obtained from the Medication Attitudes module fielded through in-person interviews in round 6 of the National Health and Aging Trends Study (weighted response rate of round 6 was 88.5%). The questions in this module were drawn from the Patients’ Attitudes Towards Deprescribing questionnaire and its revised version. The Medication Attitudes module was fielded to a random one-third (n = 2124) of the National Health and Aging Trends Study participants (weighted response rate of this module was 94.8%).
Main Outcomes and Measures
Responses to 2 statements (“If my doctor said it was possible, I would be willing to stop one or more of my regular medicines” and “I would like to reduce the number of medicines I am taking”) were the main outcomes of interest.
Results
Of the 1981 Medicare beneficiaries included in the study, 1149 (55.2%, weighted) were women, and the majority (n = 715 [54.6%, weighted]) were 65 to 74 years old. A total of 1752 (92.0%, weighted) older adults reported being willing to stop taking 1 or more of their medicines if their physician said it was possible, and 1241 (66.6%, weighted) older adults wanted to reduce the number of medicines that they were taking. Older adults taking 6 or more medications had greater odds than those taking fewer than 6 medications of being willing to stop taking 1 or more of their medicines (adjusted odds ratio, 2.90; 95% CI, 1.74-4.82) and wanting to reduce the number of medicines that they were taking (adjusted odds ratio, 2.31; 95% CI, 1.71-3.13).
Conclusions and Relevance
Physicians considering deprescribing as part of comprehensive, patient-centered care should be reassured that a majority of older Americans are open to having 1 or more of their medicines deprescribed if their physician says it is possible, and more than two-thirds want to reduce the number of medicines that they are taking.
Introduction
Polypharmacy, often defined as use of 5 or more medications by an individual, is common and is increasing in older adults in the United States and internationally. Approximately 50% of people 65 years or older are taking 5 or more medications.1,2,3,4 Polypharmacy can be appropriate and necessary in some patients, but even when medications are recommended for individual conditions (ie, in clinical practice guidelines), they may not be effective or safe in the context of multiple conditions.5,6 Use of potentially inappropriate medications, in which the risks of medication use are likely to outweigh the benefit, is also common in older adults and is associated with polypharmacy.4,7 Inappropriate medication use can result from starting inappropriate treatment or a reduction of benefits and increase of risks as the individual ages and undergoes changes in their condition, other medications, and care goals.8 Polypharmacy and inappropriate medication use have been associated with harms including adverse drug reactions, hospitalization, reduced quality of life, and mortality.4,9,10
The term deprescribing describes the physician-supervised process of discontinuation of an inappropriate medication. The goal of deprescribing is to minimize the risks associated with inappropriate medications and improve health and quality-of-life outcomes.11,12,13
Patient involvement in health care decision making is a central aspect of patient-centered care, and a majority of older adults report wanting to be involved in decision making about their health care.14,15,16 Physicians report patient resistance or unwillingness to stop taking medications as 1 of the main factors that prevents deprescribing.17,18,19 Although patient engagement is critical in safe and effective medication use,20 nationally representative data regarding patient perspectives on medication use and willingness to consider discontinuation of medication use are notably absent.
The aim of this study was to explore the attitudes of older US adults toward deprescribing. Additionally, we sought to understand whether clinical and demographic characteristics were associated with these attitudes.
Methods
Data Sources and Study Sample
This study draws on round 6 of the National Health and Aging Trends Study (NHATS),21 a nationally representative study of Medicare beneficiaries 65 years and older that aims to understand disability trends and trajectories in the United States. Details of the methods have been previously described.22 Data collection involves annual in-person interviews with participants (or a proxy if the participant is unable to respond) and includes demographics; physical and cognitive capacity; living, social, and technological environment; and economic status. The weighted response rate in round 6, fielded in 2016, was 88.5% (sampling weights take into account survey nonresponse and differential probabilities of selection). With weighting, this sample represents approximately 33.4 million Medicare beneficiaries (≥65 years old) living in the United States.23
Medication Attitudes Module
This study relies on responses to the NHATS Medication Attitudes module,24 which was fielded to a random sample of one-third of respondents (unweighted, n = 2124). This module had a weighted response rate of 94.8%; 119 participants responded as “don’t know” or “refused” to all questions in this module.
The Medication Attitudes module contained 10 questions from the Patients’ Attitudes Towards Deprescribing (PATD) questionnaire and revised PATD (rPATD) questionnaire (older adults’ version). The PATD and rPATD were designed to assess individuals’ attitudes, beliefs, and experiences regarding their medications, and the potential withdrawal of 1 or more of their medications. The questionnaires have established face, content, criterion, construct, and internal validity, as well as test-retest reliability in Australian older adults.25,26 The results are self-reported attitudes, are not medication specific, and are hypothetical in relation to intentions. To date, the PATD has been used in 6 studies internationally (3 in Australia, and 1 each in Italy, Canada, and Singapore).27,28,29,30,31,32 The participant populations have included outpatients,27 inpatients,28,29 care-facility residents,30 and community-dwelling older adults.31,32
Rating-scale statements were included from each of the 4 domains (burden, appropriateness, concerns about stopping, and involvement) of the rPATD, as well as a global statement from the PATD and rPATD (“If my doctor said it was possible, I would be willing to stop one or more of my regular medicines”).26 These 8 statements had response categories of “strongly agree,” “agree,” “disagree,” and “strongly disagree.” The final 2 questions in the module were from the PATD and asked participants “About how many different regular medicines do you take?” and “What is the maximum number of pills that you would be comfortable taking daily?” (with a series of 6 photographs of an increasing number of pills as response options).
The data used in this analysis are publicly available and have no unique identifiers. This study was deemed exempt from review by the Johns Hopkins Medicine Institutional Review Board. Written informed consent was obtained from participants when they were recruited to NHATS.
Statistical Analysis
This study is limited to those who self-reported responses to the Medication Attitudes module (n = 1981) owing to our interest in assessing what is an inherently subjective topic (143 proxy respondents [5.1% of the population, weighted] were excluded). All analyses were conducted with sampling weights and were performed using Stata (StataCorp), version 12.1. Participant responses to the questions in the Medication Attitudes module are reported as proportions. We chose a priori to focus on 2 of the rating-scale statements as the main outcomes of interest because they provided an overview of the person’s attitudes toward deprescribing. The statements, “If my doctor said it was possible, I would be willing to stop one or more of my regular medicines” and “I would like to reduce the number of medicines I am taking,” are hereafter referred to as “willingness to stop” and “wanting to reduce,” respectively. The responses to these 2 statements were converted to a binary outcome of agree (strongly agree or agree) and disagree (disagree or strongly disagree), which was then examined using logistic regression to assess unadjusted associations between the 2 main statements and respondents’ demographic and clinical characteristics. Multivariate regression models were then used to examine the likelihood of willingness to stop and wanting to reduce medicine use after adjusting for the demographic and clinical characteristics. Significance was set at P < .05.
Results
Absolute numbers reported may not reflect the reported percentages, because all reported percentages are weighted.
Older Adults’ Characteristics
Of the older adults whose responses were included in the study, 54.6% (n = 715) were 65 to 74 years old, 33.5% (n = 829) were 75 to 84 years old, and 12.0% (n = 437) were 85 years and older. Women made up 55.2% (n = 1149) of the respondents, 57.0% (n = 1065) reported beyond high school education, and 70.5% (n = 1484) had 2 or more chronic medical conditions (Table 1).33
Table 1. Characteristics of Older Adults, Stratified by Attitudes About Deprescribinga.
| Respondent Characteristics | Total (n = 1981) (Weighted %) | If My Doctor Said It Was Possible, I Would Be Willing to Stop One or More of My Regular Medicines (n = 1917) (Weighted %)b | I Would Like to Reduce the Number of Medicines I Am Taking (n = 1911) (Weighted %)c | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Strongly Agree | Agree | Disagree | Strongly Disagree | Strongly Agree | Agree | Disagree | Strongly Disagree | ||
| Age, y | |||||||||
| 65-74 | 715 (54.6) | 324 (48.5) | 308 (42.5) | 37 (4.8) | 24 (4.3) | 202 (31.9) | 266 (36.2) | 156 (20.9) | 70 (11.0) |
| 75-84 | 829 (33.5) | 329 (44.8) | 410 (48.2) | 41 (4.3) | 23 (2.6) | 201 (25.4) | 325 (40.4) | 218 (26.1) | 61 (8.1) |
| ≥85 | 437 (12.0) | 171 (41.6) | 210 (49.0) | 29 (6.6) | 11 (2.8) | 91 (22.8) | 156 (38.4) | 139 (32.5) | 26 (6.3) |
| Sex | |||||||||
| Men | 832 (44.8) | 365 (48.9) | 381 (43.6) | 39 (4.7) | 22 (2.8) | 229 (30.2) | 329 (40.7) | 193 (21.2) | 58 (7.9) |
| Women | 1149 (55.2) | 459 (44.4) | 547 (46.5) | 68 (5.0) | 36 (4.1) | 265 (27.4) | 418 (35.6) | 320 (26.3) | 99 (10.7) |
| Race | |||||||||
| White, non-Hispanic | 1415 (79.6) | 633 (49.0) | 648 (44.2) | 63 (3.8) | 34 (2.9) | 358 (28.6) | 557 (39.3) | 348 (22.4) | 111 (9.6) |
| Black, non-Hispanic | 384 (7.9) | 133 (38.9) | 192 (48.3) | 29 (9.1) | 14 (3.7) | 87 (26.4) | 140 (37.2) | 109 (28.3) | 27 (8.1) |
| Other | 182 (12.6) | 58 (33.9) | 88 (50.0) | 15 (8.8) | 10 (7.4) | 49 (30.5) | 50 (28.7) | 56 (31.6) | 19 (9.3) |
| Education | |||||||||
| Below high school | 395 (15.5) | 122 (33.3) | 204 (54.2) | 36 (8.7) | 18 (3.8) | 70 (20.6) | 153 (40.1) | 128 (33.0) | 30 (6.3) |
| High school | 489 (24.5) | 187 (40.9) | 253 (49.9) | 23 (4.9) | 15 (4.3) | 119 (28.2) | 187 (38.0) | 134 (24.7) | 38 (9.1) |
| Beyond high school | 1065 (57.0) | 506 (52.8) | 457 (40.8) | 46 (3.6) | 23 (2.7) | 300 (31.1) | 399 (37.7) | 241 (21.1) | 85 (10.1) |
| No. of different regular medicines | |||||||||
| ≤5 | 1115 (56.1) | 449 (44.4) | 508 (44.2) | 74 (6.1) | 47 (5.3) | 227 (23.6) | 380 (33.7) | 347 (29.6) | 125 (13.1) |
| ≥6 | 831 (39.8) | 372 (49.4) | 411 (46.5) | 32 (3.1) | 11 (1.1) | 264 (35.9) | 365 (44.1) | 161 (15.9) | 30 (4.1) |
| No. of chronic medical conditionsd | |||||||||
| 0-1 | 497 (29.6) | 197 (44.7) | 210 (40.9) | 26 (5.5) | 37 (8.9) | 98 (23.5) | 152 (29.4) | 149 (29.1) | 72 (18.0) |
| 2-3 | 1048 (52.3) | 437 (46.7) | 516 (47.5) | 54 (4.5) | 11 (1.2) | 261 (29.4) | 425 (41.2) | 266 (23.2) | 64 (6.2) |
| >3 | 436 (18.2) | 190 (48.2) | 202 (45.2) | 27 (4.7) | 10 (1.9) | 135 (34.6) | 170 (41.6) | 98 (18.4) | 21 (5.4) |
| Health | |||||||||
| Excellent/very Good | 812 (45.2) | 386 (52.7) | 334 (39.4) | 31 (3.0) | 28 (4.9) | 199 (27.4) | 262 (31.6) | 225 (26.5) | 91 (14.5) |
| Good | 732 (36.9) | 280 (42.9) | 369 (49.6) | 46 (5.3) | 16 (2.2) | 173 (28.8) | 310 (42.6) | 184 (23.1) | 43 (5.4) |
| Fair/poor | 435 (17.9) | 157 (38.0) | 225 (50.6) | 29 (8.3) | 14 (3.1) | 122 (31.4) | 174 (43.8) | 104 (19.7) | 22 (5.1) |
| Recent fall | |||||||||
| Yes | 208 (9.4) | 69 (40.4) | 110 (50.0) | 18 (6.8) | 7 (2.7) | 56 (31.0) | 84 (41.4) | 47 (22.6) | 13 (5.0) |
| No | 1773 (90.6) | 755 (47.0) | 818 (44.7) | 89 (4.6) | 51 (3.6) | 438 (28.4) | 663 (37.5) | 466 (24.1) | 144 (9.9) |
| Probable dementiae | |||||||||
| Yes | 150 (5.0) | 46 (34.8) | 73 (53.3) | 15 (9.9) | 5 (1.9) | 29 (22.1) | 37 (30.5) | 56 (35.4) | 14 (12.0) |
| No | 1831 (95.0) | 778 (47.0) | 855 (44.8) | 92 (4.6) | 53 (3.6) | 465 (29.0) | 710 (38.2) | 457 (23.5) | 143 (9.3) |
| Any drug coverage | |||||||||
| Yes | 1784 (89.8) | 758 (46.6) | 849 (45.5) | 92 (4.7) | 46 (3.2) | 454 (28.8) | 689 (38.6) | 459 (23.3) | 139 (9.4) |
| No | 158 (8.3) | 55 (42.2) | 70 (44.2) | 12 (6.1) | 12 (7.6) | 33 (26.9) | 51 (31.3) | 48 (31.8) | 15 (10.1) |
Numbers reported refer to the unweighted number of respondents to the Medication Attitudes module.
Weighted proportion of participants who agreed or strongly agreed to this question, 91.6%; 95% CI, 89.5% to 93.4%; unweighted, 91.4%; 95% CI, 90.1%-92.6%.
Weighted proportion of participants who agreed or strongly agreed to this question, 66.6%; 95% CI, 63.6% to 69.4%; unweighted, 64.9%; 95% CI, 62.8%-67.1%).
Chronic medical conditions refer to the number of self-reported physician diagnoses of heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, cancer, and hip fracture.
Composite dementia measure developed and validated for use in the National Health and Aging Trends Study.
Older Adults’ Beliefs and Attitudes Toward Deprescribing
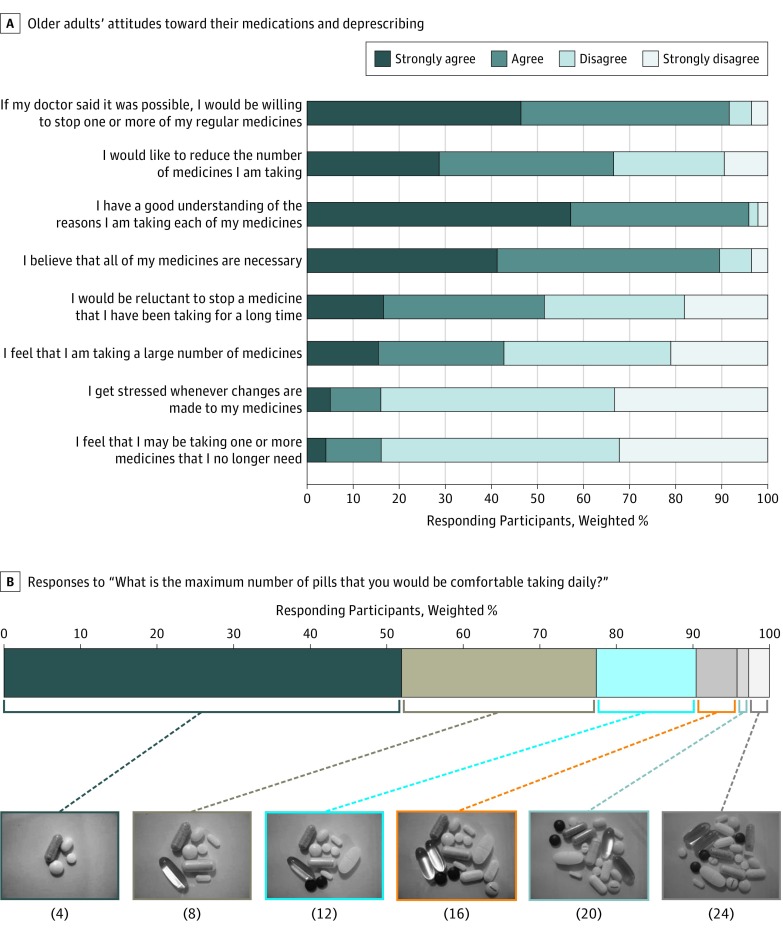
Using weighted percentages, 92.0% (n = 1752) of older adults in the United States agreed or strongly agreed that they would be willing to stop 1 or more of their medicines if their physician said it was possible (Figure). Two-thirds (66.6% [n = 1241]) of older adults reported that they would like to reduce the number of medicines they were taking, and nearly half (42.7% [n = 850]) agreed or strongly agreed that they felt they were taking a large number of medicines. In addition, 89.5% (n = 1702) agreed or strongly agreed that all of their medicines were necessary, and 16.1% (n = 333) agreed or strongly agreed that they were taking a medicine that they no longer needed.
Figure. Participant Responses to the Medication Attitudes Module Questions.
A, Participant level of agreement responses to the Medication Attitudes module. B, The number of pills in each photograph is shown in parentheses below the image. These numbers were not shown to participants.
When asked to select the maximum number of pills that they would be comfortable taking from a series of photographs, about half (51.9% [n = 973]) of older adults chose the option with 4 pills, which was the fewest, and about one quarter (25.4% [n = 486]) selected the second-lowest option of 8 pills (Figure). Thirteen percent of older adults chose an option in which the photograph depicted fewer medications than the number they reported taking.
Characteristics Associated With Willingness to Stop
Older adults’ characteristics stratified by responses to the 2 main outcomes are detailed in Table 1.
A number of demographic and clinical characteristics were associated with willingness to stop and wanting to reduce (Table 2).33 In the multivariate analysis, older adults taking 6 or more medications compared with fewer than 6 (adjusted odds ratio [aOR], 2.90; 95% CI, 1.74-4.82) and older adults with 2 to 3 (aOR, 2.87; 95% CI, 1.75-4.69) and more than 3 medical conditions (aOR, 2.87; 95% CI, 1.53-5.37) compared with fewer than 2 had almost 3 times greater odds of willingness to stop. Additionally, compared with non-Hispanic white respondents, non-Hispanic black respondents (aOR, 0.60; 95% CI, 0.37-0.96) and respondents of other races (aOR, 0.46; 95% CI, 0.24-0.89), and those reporting fair/poor health compared with excellent/very good health (aOR, 0.46; 95% CI, 0.24-0.86) had lower odds of willingness to stop.
Table 2. Unadjusted and Adjusted Associations Between Older Adults’ Demographic and Clinical Characteristics and Their Attitudes Toward Deprescribing.
| Characteristic | If My Doctor Said It Was Possible, I Would Be Willing to Stop One or More of My Regular Medicines, OR (95% CI) | I Would Like to Reduce the Number of Medicines I Am Taking, OR (95% CI) | ||
|---|---|---|---|---|
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | |
| Age, y | ||||
| 65-74 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 75-84 | 1.33 (0.87-2.04) | 1.13 (0.73-1.75) | 0.90 (0.65-1.24) | 0.80 (0.56-1.13) |
| ≥85 | 0.96 (0.59-1.56) | 0.82 (0.45-1.49) | 0.74 (0.53-1.02) | 0.61 (0.43-0.86)b |
| Sex | ||||
| Women | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Men | 1.25 (0.84-1.86) | 1.52 (0.98-2.35) | 1.43 (1.13-1.80)b | 1.64 (1.27-2.11)b |
| Race | ||||
| White, non-Hispanic | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Black, non-Hispanic | 0.50 (0.31-0.80)b | 0.60 (0.37-0.96)b | 0.82 (0.59-1.16) | 0.84 (0.57-1.23) |
| Other | 0.38 (0.21-0.66)b | 0.46 (0.24-0.89)b | 0.68 (0.45-1.04) | 0.66 (0.38-1.15) |
| Education | ||||
| Below high school | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| High school | 1.41 (0.74-2.72) | 1.08 (0.55-2.13) | 1.27 (0.93-1.73) | 1.36 (0.94-1.97) |
| Beyond high school | 2.09 (1.22-3.57)b | 1.49 (0.84-2.64) | 1.43 (1.05-1.94)b | 1.56 (1.08-2.22)b |
| ≥6 Different regular medicines | 2.96 (1.80-4.86)b | 2.90 (1.74-4.82)b | 3.00 (2.27-3.96)b | 2.31 (1.71-3.13)b |
| No. of chronic medical conditionsc | ||||
| 0-1 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 2-3 | 2.77 (1.74-4.43)b | 2.87 (1.75-4.69)b | 2.14 (1.56-2.94)b | 1.80 (1.28-2.53)b |
| >3 | 2.38 (1.29-4.37)b | 2.87 (1.53-5.37)b | 2.85 (1.93-4.20)b | 2.00 (1.27-3.13)b |
| Health | ||||
| Excellent or very good | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Good | 1.06 (0.64-1.77) | 0.81 (0.50-1.32) | 1.74 (1.38-2.20)b | 1.52 (1.19-1.94)b |
| Fair or poor | 0.67 (0.38-1.16) | 0.46 (0.24-0.86)b | 2.21 (1.57-2.83)b | 1.68 (1.18-2.38)b |
| Recent fall | 0.85 (0.50-1.44) | 0.79 (0.46-1.38) | 1.36 (0.87-2.12) | 1.33 (0.79-2.24) |
| Probable dementiad | 0.66 (0.38-1.15) | 0.80 (0.43-1.49) | 0.54 (0.38-0.77)b | 0.47 (0.32-0.71)b |
| Any drug coverage | 1.84 (1.05-3.21)b | 1.39 (0.75-2.59) | 1.48 (0.95-2.31) | 1.13 (0.69-1.87) |
Abbreviation: OR, odds ratio.
Adjusted for age, sex, race, education, number of medications taken, number of chronic medical conditions, health, recent fall, probable dementia, and any drug coverage.
Significant association (P < .05).
Chronic medical conditions refer to number of self-reported physician diagnoses of heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, cancer, and hip fracture.
Composite dementia measure developed and validated for use in the National Health and Aging Trends Study.
Similarly, the odds of wanting to reduce were higher for those taking 6 or more medications compared with those taking fewer than 6 (aOR, 2.31; 95% CI, 1.71-3.13) and for those with 2 to 3 (aOR, 1.80; 95% CI, 1.28-2.53) and more than 3 medical conditions (aOR, 2.00; 95% CI, 1.27-3.13) compared with fewer than 2. Older adults 85 years and older compared with adults aged 65 to 74 years (aOR, 0.61; 95% CI, 0.43-0.86), and those with probable dementia compared with those without (aOR, 0.47; 95% CI, 0.32-0.71) had lower odds of wanting to reduce.
Discussion
To our knowledge, this is the first nationally representative study of attitudes toward deprescribing among older Medicare beneficiaries. We found that the majority of older adults were willing to have a medicine deprescribed if their physician said it was possible. This suggests that clinicians can be reassured about broaching the topic of deprescribing with their older patients. Additionally, we found that the majority of older adults do not report that they get stressed when changes are made to their medicines. Deprescribing, including the actual determination of whether the medication is suitable for trial withdrawal, is conducted within the framework of patient-centered care and shared decision making.11,34 Most older adults reported that their medicines were necessary, and a substantial proportion expressed concern about stopping a medicine that they had been taking for a long time. These seemingly contradictory beliefs (ie, being willing to have a medication deprescribed but also thinking that their medicines are necessary) may reflect a combination of traditional deference to physician recommendations coupled with a medical culture focused on prescribing and starting medications rather than deprescribing. Qualitative studies with older adults have previously reported this disconnect of wanting to reduce their medications while also believing that the medications are still necessary, as well as the strong influence that their physician can have on their attitudes toward medications and deprescribing.35,36,37 Therefore, in practice, discussion of these concepts will be essential for reaching an informed decision about deprescribing with older adults.
It has been noted that increasing public awareness about deprescribing is a necessary step toward changing the culture around prescribing, which currently encourages continuation of medications and maintaining the status quo.17,34,38,39 A recent nationwide survey of older Canadians found that fewer than 10% were aware of the term deprescribing, although 41% reported previously initiating a conversation with their physician about medication withdrawal.38 Encouraging older adults to ask their physicians whether all of their medications are still appropriate aligns with the current international Choosing Wisely campaigns that aim to educate health care professionals and the public that “less is more.”40 Based on the results of the present study, public education campaigns should inform why medications may no longer be necessary (ie, that benefits and risks can change over time) and encourage older adults to discuss concerns they have about their medications with their physicians or other health care professionals. However, increasing public awareness of deprescribing does not replace the physician’s responsibility for appropriate use of medications.
The finding that more than 90% of older adults are willing to have a medicine deprescribed is consistent with previous investigations internationally (71%-93%).27,28,29,30,31,32 More than half of older adults reported that the photograph with 4 pills is the maximum that they would be comfortable taking. It is interesting that this result corresponds with research showing that the cutoff of 5 different medications is associated with increased risk of several harms, including falls, frailty, and mortality.41 However, this may simply demonstrate that most people picked the smallest option, rather than public awareness of the harms of polypharmacy. We found that 13% of older adults selected a photograph with fewer pills than the number of medications they reported taking, which is to say they were taking more medications than they would be ideally comfortable with. However, there was an imbalance in response options for number of medications (eg, 1-2, 3-5, 6-10) vs the photographs (eg, 4, 8, 12, 16). Additionally, number of different regular medications and number of pills taken daily may not be equivalent because many medications are taken more than once a day. Given that two-thirds of older adults wanted to reduce the number of medications that they were taking, the true result may be greater than 13%.
Several participant characteristics were associated with willingness to stop taking 1 or more of their medicines. Previous studies have identified some, but not all of these associations, likely owing in part to limitations of small sample size.27,28,29,30,31,32 Taking 6 or more medications was the greatest predictor of willingness to deprescribe and was associated with nearly 3 times greater odds of agreeing to deprescribe relative to those taking fewer than 6 medications. This finding may reflect the burden of polypharmacy experienced by these individuals. As number of medications increases, the likelihood of taking an inappropriate medication also increases, as does the risk of medication-induced harm.4,41 Therefore, this finding may indicate an understanding by these individuals that 1 or more of their medications may be inappropriate and, thus, suitable for deprescribing.35,36,42
In the unadjusted analyses, those with any drug coverage had greater odds of being willing to stop taking a medicine; however, this association was attenuated and no longer statistically significant in the adjusted analyses. Further research is required into the impact of cost of medications and socioeconomic status on attitudes toward medications and deprescribing, in particular to inform systems to ensure equal access to appropriate medications.43
Limitations
There are several limitations to this study. First, because of time limitations for the Medication Attitudes module, only a subset of the rPATD questions were used and, therefore, creating factor scores was not possible. Additionally, the questions were originally developed and validated in Australia and were not formally validated in the United States. However, many of the questions have been used in studies internationally and have not required adaptation, and no language translation was required for the United States.
Second, the statements within the rPATD are hypothetical and do not ask about specific medications. The statement about willingness to have a medicine stopped has not yet been externally validated for predictive ability.26 Therefore, it is unclear whether these results would translate to respondents actually being willing to have 1 of their medications deprescribed in practice. It is unknown what the actual rate of acceptance of deprescribing recommendations by patients and their families is in practice, and it likely varies depending on the type of medication.11 A study in Australia44 reported a patient acceptance rate of 95% for deprescribing recommendations, while another study in the United States45 reported a combined physician-patient acceptance rate of only 33%. Acceptance rates in studies may be biased by individuals who are willing to consent to study participation (ie, those who did not consent may have done so because they did not want their medications changed).
Third, number of medications and number of medical conditions is based on self-report, which may not be entirely accurate. Finally, results are weighted to the population of older Medicare beneficiaries, which is approximately 96% of all adults 65 years and older living in the United States.23 As there are pharmaceutical care services available to Medicare beneficiaries (such as Medication Therapy Management), it is possible that those enrolled in Medicare may have different attitudes than those who are not.
This study has filled an important knowledge gap in the field of deprescribing by providing nationally representative data of patient attitudes toward deprescribing. However, this new knowledge must be placed within the context of the wider fields of deprescribing and appropriate prescribing, such as the potential benefits and harms of deprescribing, determining which medications are appropriate to deprescribe in the individual, how physicians can be supported in deprescribing, and how the wider health care system and governing policies can be used to optimize medication use in older Americans.5,12,46
Conclusions
Physicians considering deprescribing as part of comprehensive, patient-centered care should be reassured that a majority of older Americans are open to having 1 or more of their medicines stopped if their physician said it was possible, and two-thirds want to reduce the number of medicines that they are taking.
References
- 1.Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015;314(17):1818-1831. doi: 10.1001/jama.2015.13766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qato DM, Wilder J, Schumm LP, Gillet V, Alexander GC. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176(4):473-482. doi: 10.1001/jamainternmed.2015.8581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elmståhl S, Linder H. Polypharmacy and inappropriate drug use among older people—a systematic review. Healthy Aging Clin Care Elder. 2013;5:1-8. doi: 10.4137/HACCE.S11173 [DOI] [Google Scholar]
- 4.Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345-351. doi: 10.1016/j.amjopharm.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 5.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716-724. doi: 10.1001/jama.294.6.716 [DOI] [PubMed] [Google Scholar]
- 6.Gurwitz JH. Polypharmacy: a new paradigm for quality drug therapy in the elderly? Arch Intern Med. 2004;164(18):1957-1959. doi: 10.1001/archinte.164.18.1957 [DOI] [PubMed] [Google Scholar]
- 7.Hill-Taylor B, Sketris I, Hayden J, Byrne S, O’Sullivan D, Christie R. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360-372. doi: 10.1111/jcpt.12059 [DOI] [PubMed] [Google Scholar]
- 8.Spinewine A, Schmader KE, Barber N, et al. Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet. 2007;370(9582):173-184. doi: 10.1016/S0140-6736(07)61091-5 [DOI] [PubMed] [Google Scholar]
- 9.Olsson IN, Runnamo R, Engfeldt P. Medication quality and quality of life in the elderly, a cohort study. Health Qual Life Outcomes. 2011;9:95. doi: 10.1186/1477-7525-9-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muhlack DC, Hoppe LK, Weberpals J, Brenner H, Schöttker B. The association of potentially inappropriate medication at older age with cardiovascular events and overall mortality: a systematic review and meta-analysis of cohort studies. J Am Med Dir Assoc. 2017;18(3):211-220. doi: 10.1016/j.jamda.2016.11.025 [DOI] [PubMed] [Google Scholar]
- 11.Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmacol. 2014;78(4):738-747. doi: 10.1111/bcp.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834. doi: 10.1001/jamainternmed.2015.0324 [DOI] [PubMed] [Google Scholar]
- 13.Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol. 2015;80(6):1254-1268. doi: 10.1111/bcp.12732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chi WC, Wolff J, Greer R, Dy S. Multimorbidity and decision-making preferences among older adults. Ann Fam Med. 2017;15(6):546-551. doi: 10.1370/afm.2106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chewning B, Bylund CL, Shah B, Arora NK, Gueguen JA, Makoul G. Patient preferences for shared decisions: a systematic review. Patient Educ Couns. 2012;86(1):9-18. doi: 10.1016/j.pec.2011.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolff JL, Boyd CM. A look at person- and family-centered care among older adults: results from a national survey [corrected]. J Gen Intern Med. 2015;30(10):1497-1504. doi: 10.1007/s11606-015-3359-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson K, Stowasser D, Freeman C, Scott I. Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open. 2014;4(12):e006544. doi: 10.1136/bmjopen-2014-006544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson K, Foster M, Freeman C, Luetsch K, Scott I. Negotiating “unmeasurable harm and benefit”: perspectives of general practitioners and consultant pharmacists on deprescribing in the primary care setting. Qual Health Res. 2017;27(13):1936-1947. doi: 10.1177/1049732316687732 [DOI] [PubMed] [Google Scholar]
- 19.Wallis KA, Andrews A, Henderson M. Swimming against the tide: primary care physicians’ views on deprescribing in everyday practice. Ann Fam Med. 2017;15(4):341-346. doi: 10.1370/afm.2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryan R, Santesso N, Lowe D, et al. Interventions to improve safe and effective medicines use by consumers: an overview of systematic reviews. Cochrane Database Syst Rev. 2014;4(4):CD007768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Health and Aging Trends Study Round 6 data. http://www.nhatsdata.org. Accessed September 20, 2017.
- 22.DeMatteis JM, Freedman VA, Kasper JD. National Health and Aging Trends Study (NHATS) development of round 6 survey weights: NHATS Technical Paper #18. https://www.nhats.org/scripts/documents/NHATS_Round6_WeightsTechnicalPaper_12_12_17.pdf. Published December 12, 2017. Accessed August 21, 2018.
- 23.Kasper JD, Freedman VA National Health and Aging Trends Study (NHATS) user guide: rounds 1-6 beta release. https://www.nhats.org/scripts/documents/NHATS_User_Guide_R1_R6.pdf. Published July 19, 2017. Accessed August 21, 2018.
- 24.National Health and Aging Trends Study Medication Attitudes module. https://www.nhats.org/scripts/instruments/038_MA_Round6.pdf. Accessed August 22, 2018.
- 25.Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Development and validation of the Patients’ Attitudes Towards Deprescribing (PATD) questionnaire. Int J Clin Pharm. 2013;35(1):51-56. doi: 10.1007/s11096-012-9704-5 [DOI] [PubMed] [Google Scholar]
- 26.Reeve E, Low L-F, Shakib S, Hilmer SN. Development and validation of the revised Patients’ Attitudes Towards Deprescribing (rPATD) questionnaire: versions for older adults and caregivers. Drugs Aging. 2016;33(12):913-928. doi: 10.1007/s40266-016-0410-1 [DOI] [PubMed] [Google Scholar]
- 27.Reeve E, Wiese MD, Hendrix I, Roberts MS, Shakib S. People’s attitudes, beliefs, and experiences regarding polypharmacy and willingness to deprescribe. J Am Geriatr Soc. 2013;61(9):1508-1514. doi: 10.1111/jgs.12418 [DOI] [PubMed] [Google Scholar]
- 28.Qi K, Reeve E, Hilmer SN, Pearson S-A, Matthews S, Gnjidic D. Older peoples’ attitudes regarding polypharmacy, statin use and willingness to have statins deprescribed in Australia. Int J Clin Pharm. 2015;37(5):949-957. doi: 10.1007/s11096-015-0147-7 [DOI] [PubMed] [Google Scholar]
- 29.Galazzi A, Lusignani M, Chiarelli MT, et al. Attitudes towards polypharmacy and medication withdrawal among older inpatients in Italy. Int J Clin Pharm. 2016;38(2):454-461. doi: 10.1007/s11096-016-0279-4 [DOI] [PubMed] [Google Scholar]
- 30.Kalogianis MJ, Wimmer BC, Turner JP, et al. Are residents of aged care facilities willing to have their medications deprescribed? Res Social Adm Pharm. 2016;12(5):784-788. doi: 10.1016/j.sapharm.2015.12.004 [DOI] [PubMed] [Google Scholar]
- 31.Ng WL, Tan MZW, Koh EYL, Tan NC. Deprescribing: what are the views and factors influencing this concept among patients with chronic diseases in a developed Asian community? Proc Singapore Healthc. 2017;26(3):172-179. doi: 10.1177/2010105817699633 [DOI] [Google Scholar]
- 32.Sirois C, Ouellet N, Reeve E. Community-dwelling older people’s attitudes towards deprescribing in Canada. Res Social Adm Pharm. 2017;13(4):864-870. doi: 10.1016/j.sapharm.2016.08.006 [DOI] [PubMed] [Google Scholar]
- 33.Kasper JD, Freedman VA, Spillman B Classification of persons by dementia status in the National Health and Aging Trends Study: NHATS Technical Paper #5. https://www.nhats.org/scripts/documents/NHATS_Dementia_Technical_Paper_5_Jul2013.pdf. Published July 2013. Accessed August 21, 2018.
- 34.Jansen J, Naganathan V, Carter SM, et al. Too much medicine in older people? Deprescribing through shared decision making. BMJ. 2016;353(1):i2893. doi: 10.1136/bmj.i2893 [DOI] [PubMed] [Google Scholar]
- 35.Moen J, Bohm A, Tillenius T, Antonov K, Nilsson JLG, Ring L. “I don’t know how many of these [medicines] are necessary..”—a focus group study among elderly users of multiple medicines. Patient Educ Couns. 2009;74(2):135-141. doi: 10.1016/j.pec.2008.08.019 [DOI] [PubMed] [Google Scholar]
- 36.Linsky A, Simon SR, Bokhour B. Patient perceptions of proactive medication discontinuation. Patient Educ Couns. 2015;98(2):220-225. doi: 10.1016/j.pec.2014.11.010 [DOI] [PubMed] [Google Scholar]
- 37.Reeve E, Low L-F, Hilmer SN. Beliefs and attitudes of older adults and carers about deprescribing of medications: a qualitative focus group study. Br J Gen Pract. 2016;66(649):e552-e560. doi: 10.3399/bjgp16X685669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Turner JP, Tannenbaum C. Older adults’ awareness of deprescribing: a population-based survey. J Am Geriatr Soc. 2017;65(12):2691-2696. doi: 10.1111/jgs.15079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tannenbaum C, Farrell B, Shaw J, et al. An ecological approach to reducing potentially inappropriate medication use: Canadian Deprescribing Network. Can J Aging. 2017;36(1):97-107. doi: 10.1017/S0714980816000702 [DOI] [PubMed] [Google Scholar]
- 40.Levinson W, Kallewaard M, Bhatia RS, Wolfson D, Shortt S, Kerr EA; Choosing Wisely International Working Group . ‘Choosing Wisely’: a growing international campaign. BMJ Qual Saf. 2015;24(2):167-174. doi: 10.1136/bmjqs-2014-003821 [DOI] [PubMed] [Google Scholar]
- 41.Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65(9):989-995. doi: 10.1016/j.jclinepi.2012.02.018 [DOI] [PubMed] [Google Scholar]
- 42.Reeve E, To J, Hendrix I, Shakib S, Roberts MS, Wiese MD. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging. 2013;30(10):793-807. doi: 10.1007/s40266-013-0106-8 [DOI] [PubMed] [Google Scholar]
- 43.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94(10):1782-1787. doi: 10.2105/AJPH.94.10.1782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Potter K, Flicker L, Page A, Etherton-Beer C. Deprescribing in frail older people: a randomised controlled trial. PLoS One. 2016;11(3):e0149984. doi: 10.1371/journal.pone.0149984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams ME, Pulliam CC, Hunter R, et al. The short-term effect of interdisciplinary medication review on function and cost in ambulatory elderly people. J Am Geriatr Soc. 2004;52(1):93-98. doi: 10.1111/j.1532-5415.2004.52016.x [DOI] [PubMed] [Google Scholar]
- 46.Reeve E, Thompson W, Farrell B. Deprescribing: a narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. Eur J Intern Med. 2017;38:3-11. doi: 10.1016/j.ejim.2016.12.021 [DOI] [PubMed] [Google Scholar]