Introduction
Lipomas are the most common benign musculoskeletal tumors, comprising 50% of musculoskeletal soft tissue tumors. Intermuscular lipomas are occur deep within muscle compartments and comprise 0.3% of all lipomas1. As with other deep lipomas, they are often asymptomatic, being identified only when they have reached a large size or are compressing local neurovascular structures or both2. Deep lipomas are most commonly found in the lower limbs, and in decreasing order of frequency affect the trunk, shoulders and arms; the intermuscular subtype has a particular predilection for the abdominal wall3, 4.
We here report a rare case of giant intermuscular lipoma involving the brachialis, coracobrachialis and triceps muscles, traversing between the anterior and posterior compartments along the course of the radial nerve.
Case Report
A 58‐year‐old woman with type 2 diabetes presented with a three year history of a gradually enlarging mass in her right upper arm. The swelling had initially been asymptomatic; however, over the preceding year it had started to cause non‐radiating pain deep in the anterolateral aspect of her arm. The pain was not related to any specific movement and occurred during periods of both rest and activity; however, direct pressure on the mass tended to cause pain. She denied any sensory disturbance or weakness of the arm, forearm or fingers. On examination she had asymmetry of her right upper arm with a palpable soft mass over its anterolateral aspect, palpation of which caused pain over the mass itself, particularly over the region of transition between the posterior and anterior compartments of the arm. She underwent MRI, which revealed a 5.7 cm × 3.2 cm × 10.8 cm lobulated deep lipoma involving the brachialis, coracobrachialis and triceps muscles with extension along the intermuscular planes (Fig. 1). Although it lay against the lateral humeral cortex no underlying periosteal reaction was apparent. The mass had an hourglass appearance as it traversed between the anterior and posterior compartments through the hiatus for the radial nerve in the lateral intermuscular septum (Fig. 2). The mass was compressing the radial nerve against the septum.
Figure 1.
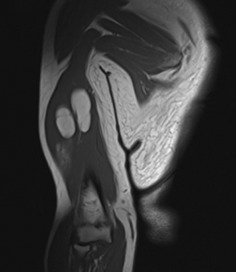
Coronal T1 MRI showing a lipoma involving the anterior and posterior compartments of the right upper arm.
Figure 2.
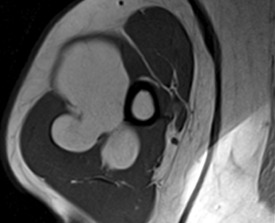
Axial T1 MRI showing lipoma traversing between the anterior and posterior compartments through the intermuscular septum.
Because of her symptoms, the patient was brought in for elective excision of the lipoma as a day case procedure. She was placed in a supine position with the right arm over an arm table with the elbow flexed and the shoulder abducted and internally rotated to 90°. A lateral approach between the brachialis and the lateral intermuscular septum was used to reach the mass. This approach was chosen because it enabled identification and protection of the radial and posterior cutaneous nerves of the arm distally, dissection of the mass in the anterior compartment, release of the lateral intermuscular septum from the humerus and removal of the mass from the posterior compartment. Because the radial nerve was in close proximity to the mass, great care was taken intraoperatively to assess the relationship between the mass and this nerve.
The waist of the lipoma was constricted as it traversed the lateral intramuscular septum, following the course of the radial nerve from the posterior to the anterior compartment of the upper arm. Rather than relying on sharper instruments, finger dissection was performed to remove the lipoma. After dissecting the mass anteriorly, the lateral intermuscular septum was identified and elevated from the humerus and the hiatus for the radial nerve enlarged. The nerve was then protected and the mass removed by finger dissection en masse from the posterior compartment and sent for histopathological analysis (Fig. 3). Post excision the cavity was checked to ensure the radial and posterior cutaneous nerves of the arm remained intact (Fig. 4). The patient made a good recovery post‐operatively with no features of radial nerve palsy and normal sensation over the distribution of posterior cutaneous nerve of the arm. Histopathology confirmed a 97 g lipoma measuring 8.0 cm × 7.5 cm × 3.0 cm, with no atypical features on microscopy.
Figure 3.

Macroscopic appearance of the lipoma after excision.
Figure 4.

Residual cavity after excision of the lipoma showing an intact radial nerve (yellow arrow) resting on the humerus and posterior cutaneous nerve of the arm (blue arrow).
The patient made a full postoperative recovery with complete resolution of her arm pain, a return to normal function and no recurrence of the mass or neurological symptoms at her six month follow‐up.
Discussion
Intermuscular lipomas are slow growing lesions that are referred to as giant lipomas when they exceed 5 cm in size. Due to the deep position of these lesions, they only come to clinical attention when they cause pain because of stretching or pressure on adjacent structures5. Although definitive diagnosis of a lipoma can only be made histologically, MRI remains the imaging modality of choice for their diagnosis. On MRI, lipomas appear as homogenous lesions with high fat signals on T1 or intermediate intensity on T2; however both ultrasound and CT may also be useful2. It is important to consider other differential diagnoses such as liposarcoma when diagnosing larger lesions. Although there are no CT or MRI features that distinguish between lipoma and liposarcomas, suspicious features such as large size, heterogeneity, irregular thickened septa, high degree of vascularity and low fat content all warrant initial biopsy6.
In our case, the radial nerve was intimately associated with the lipoma and compression against the lateral intermuscular septum could be seen on MRI. There are published case reports that describe peripheral nerve compression secondary to lipomas; these are considered rare sequelae. Flores et al. found that in patients with peripheral nerve compression, pain and sensory deficit were the most common symptoms7. Most reported cases have had nerve compression in the forearm; indeed, there have been reports of posterior interosseous and superficial radial nerve involvement, however involvement of the proximal radial nerve is rare2. In all reported cases, patients with compressive neuropathies secondary to lipomas experienced good resolution of symptoms, including pain, post‐resection7. Chaudhary et al. reported a case of a giant lipoma of the posterior compartment of the arm which was seen to be displacing the long head of the triceps along with the radial nerve and associated vessels; it was completely asymptomatic, which suggests that neurological symptoms may not be present initially8. Although our patient had no sensory or motor defects, pain was her main symptom. However, we believed that the proximity of the lipoma and the path through the tight lateral intermuscular septum left our patient at risk of developing further neurological symptoms.
Over a ten year study period, Elbardouni et al. assessed 13 cases of upper extremity deep‐seated lipomas, five of which were giant lipomas involving the triceps or brachialis muscles2. Unlike our case, none of the patients in their series presented with pain or compressive symptoms. To our knowledge, the specific pattern of a lipoma crossing from one muscular compartment to another has not previously been described in the upper arm. In our case, the decision to operate was made on the grounds of pain and the large size of the lesion. Other reported indications include cosmetic reasons, irregularity, subfascial location, increasing size and abnormal aspiration cytology9.
We here report a rare case of a large deep intermuscular lipoma that traversed along the course of the radial nerve from the posterior to the anterior compartment of the arm, presented with pain, and was successfully surgically removed. It is critical that extreme care be taken with the operative technique to ensure that neurovascular structures are carefully preserved, thus protecting the function of the affected limb.
Disclosure: All authors have no financial or personal relationships with other people or organizations that could inappropriately influence this work.
References
- 1. Fletcher CD, Martin‐Bates E. Intramuscular and intermuscular lipoma: neglected diagnoses. Histopathology, 1988, 12: 275–287. [DOI] [PubMed] [Google Scholar]
- 2. Elbardouni A, Kharmaz M, Salah Berrada M, Mahfoud M, Elyaacoubi M. Well‐circumscribed deep‐seated lipomas of the upper extremity. A report of 13 cases. Orthop Traumatol Surg Res, 2011, 97: 152–158. [DOI] [PubMed] [Google Scholar]
- 3. Lee JH, Do HD, Lee JC. Well‐circumscribed type of intramuscular lipoma in the chest wall. J Cardiothorac Surg, 2013, 8: 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bancroft LW, Kransdorf MJ, Peterson JJ, O'Connor MI. Benign fatty tumors: classification, clinical course, imaging appearance, and treatment. Skeletal Radiol, 2006, 35: 719–733. [DOI] [PubMed] [Google Scholar]
- 5. Balakrishnan C, Nanavati D, Balakrishnan A, Pane T. Giant lipomas of the upper extremity: case reports and a literature review. Can J Plast Surg, 2012, 20: e40–e41. [PMC free article] [PubMed] [Google Scholar]
- 6. Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors: distinction of lipoma and well‐differentiated liposarcoma. Radiology, 2002, 224: 99–104. [DOI] [PubMed] [Google Scholar]
- 7. Flores LP, Carneiro JZ. Peripheral nerve compression secondary to adjacent lipomas. Surg Neurol, 2007, 67: 258–263. [DOI] [PubMed] [Google Scholar]
- 8. Chaudhary RJ, Dube V, Bhansali C, Gupta A, Balwantkar S. Parosteal lipoma of humerus‐A rare case. Int J Surg Case Rep, 2013, 4: 1159–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Serpell JW, Chen RY. Review of large deep lipomatous tumours. ANZ J Surg, 2007, 77: 524–529. [DOI] [PubMed] [Google Scholar]


