Abstract
Objective: To evaluate functional outcomes and complications of reconstruction of the proximal humerus after intra‐articular tumor resection.
Methods: Twenty‐five patients who underwent Malawer I type resection and reconstruction of the proximal humerus for treatment of malignant or invasive benign tumors from August 1999 to August 2005 were evaluated. A variety of reconstructive procedures, including modular tumor prosthesis, osteoarticular allograft, and allograft‐prosthetic composite (APC), were performed after resection of tumor. Oncological and radiographic parameters were evaluated. The modified Musculoskeletal Tumor Society (MSTS) evaluation system was used to assess limb functional outcome.
Results: The study group consisted of 10 male and 15 female patients, among which there were 20 malignant and 5 benign tumors. Restoration of shoulder function was achieved with a prosthesis in 6 patients, osteoarticular allograft in 12, and allograft‐prosthesis composite in 7. At a mean of 48 months follow‐up, 2 patients had died of disease. Two patients had local recurrence and 2 had metastatic disease. On the basis of the modified MSTS functional evaluation, the mean scores were 22.50 in the modular prosthesis group, 24.58 in the osteoarticular allograft group, and 27.00 in APC group, respectively. Joint instability and subluxation were serious complications affecting shoulder function in 10 patients.
Conclusion: Reconstruction of the proximal humerus is an option that provides good relief of pain and preserves manual dexterity. Functional outcomes are better for APC and allograft than for modular prosthesis, due to retention of the rotation cuff. Complications in the APC group were less than in the allograft one.
Keywords: Humerus; Bone neoplasms; Transplantation, homologous; Joint prosthesis
Introduction
Intra‐articular proximal humeral resection is type I shoulder‐girdle resection in the Malawer surgical classification 1 . Options for reconstruction after intra‐articular resection of the proximal humerus include tumor prostheses, osteoarticular allograft, and allograft‐prosthetic composite, each has merits and demerits. In this retrospective study, we reviewed the functional outcomes and complications associated with these three reconstructive procedures, with the aim of providing a research‐based basis for choosing the most appropriate reconstructive technique and minimizing complications after intra‐articular proximal humeral resection.
Materials and methods
Patients
From August 1999 to August 2005, 25 patients with primary malignant tumor or invasive benign tumor of the proximal humerus were treated by intra‐articular proximal humeral resection. Of the 25 patients, there were 10 male and 15 female patients, aged from 8 to 62 years (average age, 32 years). The pathological classifications were as follows: six patients were diagnosed as having chondrosarcoma, five osteosarcoma, six giant cell tumor (five benign and one malignant), three metastatic carcinoma (two thyroid carcinoma and one breast cancer), one lymphoma, two Ewing sarcoma, and two malignant fibrous histiocytoma. As confirmed by preoperative magnetic resonance imaging (MRI), 14 patients had intra‐articular tumors, and 11 extra‐articular tumors. Reconstruction was done with osteoarticular allograft in 12 patients, tumor prostheses in 6, and APC in 7.
Surgical technique
In all patients, proximal humeral resection was performed through a deltopectoral approach. The length of humerus that were resected ranged from 7 to 19 cm (average, 11 cm), depending on the extent of preoperative tumor invasion as shown on MRI. Type I resection in the Malawer classification (intra‐articular proximal humeral resection) was adopted. Bone marrow specimens obtained from the remaining portion of the humeral diaphysis were found to be free of tumor cells in all patients.
Allografts were provided by the bone bank of the Orthopedic Institute of Xijing Hospital affiliated to the Fourth Military Medical University. A particular allograft was chosen for each patient on the basis of estimations of the bone size made from preoperative radiographs. A humeral head of equal or slightly smaller size than the host bone was selected. The allograft was secured to host bone with an intramedullary nail in five patients, an intramedullary nail with a four‐hole small bone plate in three, and an intramedullary nail with bone cement in four. For APC patients it was attached to the proximal humerus using a bone cement prosthesis through the medullary cavity of the allograft.
Reconstruction of soft tissues surrounding the shoulder joint was achieved by restoration of the rotator cuff and binding of the deltoid muscles. In patients undergoing osteoarticular allograft or APC, the rotator cuff soft tissues were sutured to their anatomic insertion sites on the allograft, and the deltoid muscle end to the deltoid tuberosity of the humeral shaft, with nonabsorbable sutures. Holes were made in the bone substance, and repeated polydioxanone sutures were used to attach the soft tissue to the allograft. In most cases the soft tissues were attached to the lateral annulus of the allograft, while in recent years some of the allografts were designed with several holes around the surgical neck so that the rotator cuff could be attached to its anatomic insertion site on the allograft (Fig. 1).
Figure 1.
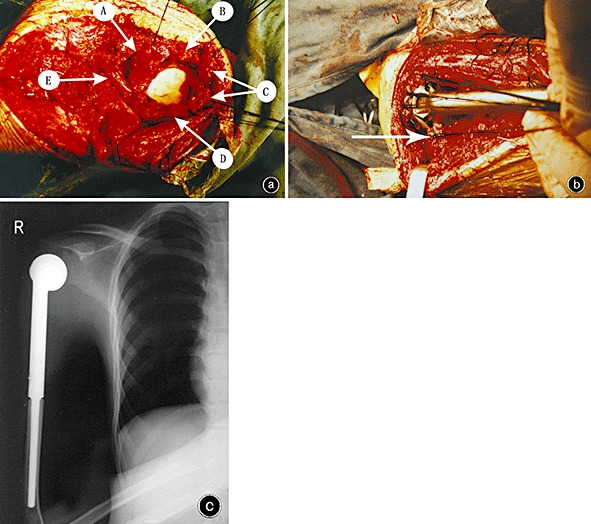
Anatomical reconstruction of the rotator cuff after resection of a proximal humerus tumor. (a) The structure surrounding the glenoid component. A, subscapularis muscle; B, supraspinous muscle; C, infraspinous muscle; D, teres minor muscle; E, axillary nerve. (b) The reconstructive insertion of the subscapularis muscle. Allograft fracture (arrow). (c) Postoperative X‐ray revealing that the humeral prothesis matches the glenoid component well.
Postoperative management
Postoperatively, patients were immobilized in a position of forward flexion and abduction with an orthosis for six weeks to facilitate union of the rotator cuff tissues, after which passive and active exercises were introduced.
Follow‐up and evaluation
The database included radiographs, operative records including photographs, and pathological reports. Functional evaluations were based on the modified MSTS system for the upper extremity, which assesses pain, functional restriction, emotional acceptance, positioning and dexterity of the hand, and lifting ability 2 . Functional evaluation was made at follow‐up and scores obtained at the most recent follow‐up were used in statistical analysis. The most recent evaluation data available was used for patients who had died. The extent of forward flexion and posterior extension of the shoulder joints were measured, while abduction was measured using an orthophoria X‐ray technique with the patient in maximal active glenoid abduction.
The oncological parameters which were studied included survival time, local recurrence and metastasis of tumors. Radiographic parameters included time to union, joint stability, allograft resorption and fracture, subchondral collapse, and loosening of prostheses and internal implants. For radiographic evaluation, fracture was defined as a discontinuity of allograft bone in the metaphyseal‐diaphyseal regions; subchondral fracture as fragmentation in the epiphyseal region; glenohumeral subluxation as incongruent placement of the humeral head in the glenoid; and glenohumeral dislocation as a complete lack of glenohumeral articulation.
The data were analyzed using SPSS10.0 software package (SPSS, Chicago, IL, USA). The χ2 test was used for count data. Functional evaluation scores were subjected to the Kolmogorov‐Smirnov test of normality and the Levene test for homogeneity of variance before analysis. If they satisfied the prerequisites for analysis of variance, they were analyzed using analyses of variances or Student's t‐test; otherwise they were analyzed using the Kruskal‐Wallis nonparametric test. The level of significance was considered to be α < 0.05.
Results
Oncological results
The average length of follow‐up was 48 months (range, 16–80 months). One of the 22 patients with primary malignant tumors died of Ewing sarcoma, and one of the three patients with metastatic carcinoma died of the disease. Local recurrence was noted in two patients; specifically in one patient with malignant fibrous histiocytoma treated with local resection, and secondly in one of the patients with chondrosarcoma, who was treated by extensive resection twice and finally underwent amputation of the pectoral girdle to control local recurrence. One patient with breast cancer and one with malignant fibrous histiocytoma remained alive with tumors.
Functional results
Manual dexterity was preserved in all patients, and pain relieved in the majority of patients. The APC group scored highest according to the MSTS system (27.00 ± 1.53), followed by the osteoarticular allograft group (24.58 ± 1.38) and the tumor prosthesis group (22.50 ± 1.64). There were statistical differences between the three groups (F, 15.03; P, 0.00). It was evident that APC was superior to osteoarticular allograft or tumor prosthesis in terms of shoulder function (Fig. 2). Similarly, APC was better than osteoarticular allograft, and the latter was better than tumor prosthesis in regard to positioning of the hand and functional activities, the differences being statistically significant. However, as shown in Table 1, there was no difference between the three reconstructive procedures with respect to pain, emotional acceptance, manual dexterity, or lifting ability of the upper extremity.
Figure 2.
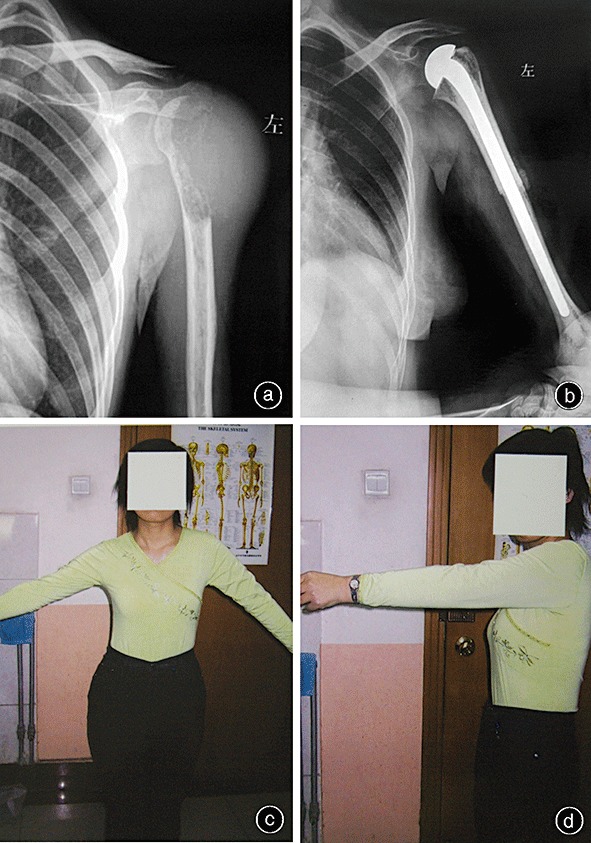
APC reconstruction following resection of a giant cell tumor of the proximal humerus. (a) Preoperative X‐ray film. (b) Postoperative X‐ray film. (c) Abduction of the glenohumeral joint to 50°. (d) Anteflexion of the glenohumeral joint to 90°.
Table 1.
Results of MSTS functional evaluation (Average rank)
| Groups | Pain | Functional activities | Emotional acceptance | Hand positioning | Manual dexterity | Lifting ability |
|---|---|---|---|---|---|---|
| Tumor prosthesis | 12.42 | 7.50 | 10.67 | 5.17 | 12.92 | 9.83 |
| Osteoarticular allograft | 12.42 | 12.75 | 12.17 | 13.42 | 12.92 | 11.79 |
| APC | 12.50 | 18.14 | 16.43 | 19.00 | 13.21 | 17.79 |
| χ2 value | 1.273 | 7.880 | 2.740 | 13.245 | 0.020 | 5.456 |
| P value | 0.529 | 0.019 | 0.254 | 0.001 | 0.990 | 0.065 |
APC produced the greatest abduction, followed by osteoarticular allograft and tumor prosthesis, and the difference was statistically significant (F= 15.401; P= 0.000). Similarly, APC and osteoarticular allograft were also better than tumor prosthesis in terms of forward flexion of the shoulder (F= 9.285; P= 0.001). Least significant difference revealed no difference between the APC and osteoarticular allograft groups (P= 0.604), but significant differences between the osteoarticular allograft and APC groups and the osteoarticular allograft and tumor prosthesis groups (P= 0.001 and P= 0.001, respectively). As shown in Table 2, there was no difference between the three groups in posterior extension of the shoulder joint (F= 3.293; P= 0.056).
Table 2.
Range of shoulder movement as a function of the reconstructive options
| Groups | Anterior flexion | Posterior extension | Abduction |
|---|---|---|---|
| Tumor prosthesis | 45.00°± 4.15° | 41.33°± 3.50° | 42.17°± 4.49° |
| Osteoarticular allograft | 53.08°± 3.65° | 46.50°± 4.72° | 48.25°± 5.29° |
| APC | 54.14°± 5.08° | 46.71°± 4.39° | 58.00°± 5.72° |
As shown in Table 3, the range of postoperative shoulder movements was related to the site of the tumors. There was a significant difference in shoulder abduction (t= 5.400; P= 0.000), yet no difference in anterior flexion (t= 0.938; P= 0.358) or posterior extension (t= 1.333; P= 0.196), between patients with intra‐articular as opposed to extra‐articular tumors.
Table 3.
Range of shoulder movement as a function of intra‐articular or extra‐articular tumors
| Groups | Anterior flexion | Posterior extension | Abduction |
|---|---|---|---|
| Intra‐articular | 52.36°± 5.37° | 46.43°± 4.54° | 54.57°± 6.02° |
| Extra‐articular | 50.27°± 5.71° | 43.91°± 4.89° | 43.09°± 4.11° |
Complications
Early postoperative complications included superficial exudation and wound dehiscence, these were observed in two patients and healed through debridement and drainage. No deep infection developed in our study.
Late postoperative complications included joint instability, subluxation, delayed union of host bone with the allografts, allograft resorption and fracture. As shown in Fig. 3, shoulder instability after reconstruction, mainly in the forms of anterior subluxation and proximal migration, occurred in ten patients (40%), including four who had undergone prosthetic reconstruction, four osteoarticular allograft, and two APC, but the differences between the three groups in shoulder instability were not significant. However, there was a significant difference between patients with benign and those with malignant tumors in shoulder instability after reconstruction (20% vs. 36%; χ2= 1.000; P= 0.317); patients who underwent intra‐articular tumor resection had a higher incidence of shoulder instability than those who underwent extra‐articular tumor resection (64% vs. 21%; χ2= 4.390, P= 0.036); however there was no overall difference between the three reconstructive procedures in the incidence of shoulder instability (χ2= 2.286; P= 0.319).
Figure 3.
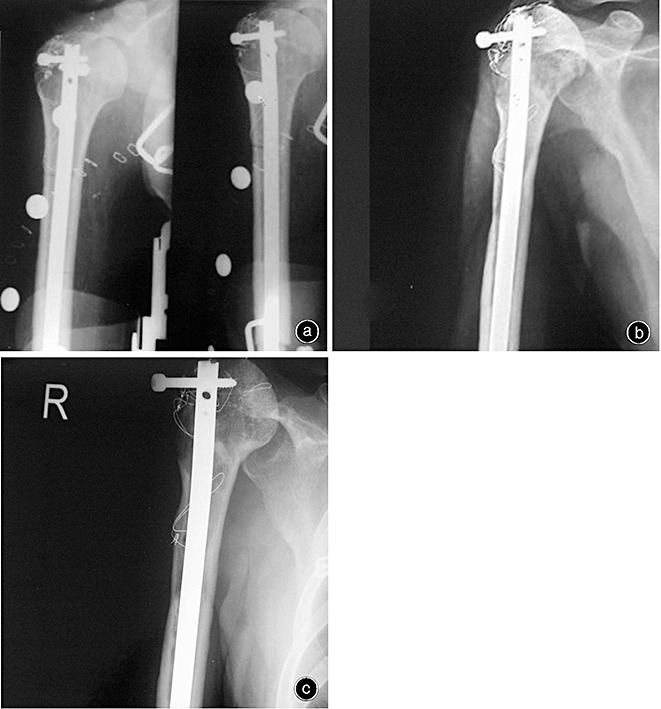
APC reconstruction following resection of proximal humerus osteosarcoma. (a) Postoperative X‐ray films showing good alignment of the glenohumeral joint. (b) X‐ray film showing upward subluxation of the humeral head 3 years postoperatively. (c) X‐ray film 7 years postoperatively.
In none of the patients was loosening of the prosthesis observed. Five patients had experienced allograft resorption by three‐year or longer follow‐up, which, as shown in Fig. 4, was in the form of bone end resorption in three patients and bone segment resorption in two. No allograft fracture occurred in patients who underwent APC. As shown in Fig. 5, of the 12 patients treated by prosthetic reconstruction, three (25%), whose prostheses were fixed without compound bone cement, had fractures, of whom two had subchondral fractures confirmed by routine radiographic reexaminations at 55‐ and 62‐month after surgery, respectively. However, because they were clinically asymptomatic, these two received no treatment. The third one had metaphyseal fracture at 46‐month follow‐up and was treated with a second osteoarticular allograft. No allograft fracture occurred in the patients who underwent bone cement fixation and APC. Six patients experienced delayed bone union, four of whom received no special treatment apart from prolongation of fixation time, while the remaining two patients were treated by bone grafting.
Figure 4.
X‐ray film showing absorption of an allograft.
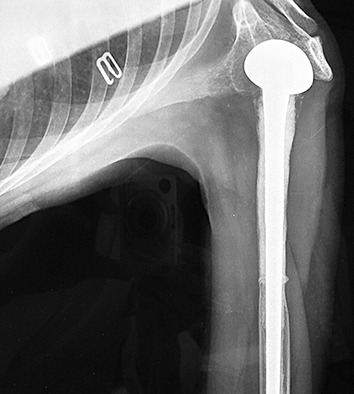
Figure 5.

X‐ray film showing metaphyseal fracture of an allograft 3 years postoperatively.
Discussion
Reconstruction of the proximal humerus following an intra‐articular tumor resection can be achieved by arthrodesis or arthroplasty 3 , 4 . At present arthroplasty mainly includes osteoarticular allograft, prosthetic reconstruction, and APC. Prosthetic reconstructions have the advantages of providing immediate stabilization of the distal humerus, having no influence on preoperative chemotherapy, and a low infection rate in comparison to osteoarticular allografts 5 . However, prostheses can fail at a later stage when surrounding stable structures become insufficient. Compared with prosthetic reconstruction, osteoarticular allografts allow the remaining deltoid muscle and rotator tendons to be attached to the soft tissue of the allograft, which provides better potential for maintaining shoulder stability and recovering its functions. Thus APC, which incorporates the advantages of both prosthetic reconstruction and osteoarticular allograft reconstruction, is thought to offer patients the optimal reconstructive option because it is effective in facilitating soft tissue union on the one hand, and avoiding complications associated with prosthetic replacement, such as collapse of the articular surface and fracture, on the other hand 6 , 7 .
Functional results
According to the MSTS system, the APC group scored highest, followed by the osteoarticular allograft group and the tumor prosthesis group. More specifically, there was no difference between the different reconstructive methods in pain relief, manual dexterity, or emotional acceptance. However, MSTS scores on functional activities and positioning of the hand varied dramatically from one reconstructive procedure to the next. There was no significant difference between the three groups in posterior extension of the shoulder joint. However APC and osteoarticular allografts were better than tumor prostheses in terms of forward flexion of the shoulder joint, which might be due to the functional loss of the deltoid muscles associated with tumor prosthesis. Abduction is an important function for the shoulder joint. The shoulder joint is a kind of third class lever, with its force bearing point located between the fulcrum and the weight. In our reviews, we found that abduction varied dramatically as a function of the reconstructive procedures and site of tumors: the APC group had the best abduction, followed by the osteoarticular allograft group and the tumor prosthesis group, and these differences were statistically significant. Abduction was less in patients with extra‐articular tumor as compared to those with intra‐articular tumors, possibly because more rotator cuff tissues have to be resected in the case of extra‐articular tumors. Therefore, the indications for reconstructions following proximal humeral resection are as follows: tumor prostheses are the preferred choice for those whose abduction cannot be preserved, whereas APC or osteoarticular allografts should be selected for those whose abduction can be preserved. Given that restoration and reconstruction of abduction will eventually affect the range of shoulder movement and functional outcomes, osteoarticular allografts or APC reconstruction provide a better anatomical basis for late recovery of shoulder functions. On the other hand, tumor prostheses do not provide intrinsic soft tissue stability, even though rotator cuff tissues are partially preserved, with the result that subsequent functional recovery is compromised.
Postoperative complications
Exudation
The early complications of local exudation and wound dehiscence occurred only in the osteoarticular allograft group, and healed through debridement and local drainage. Occurrence of these complications may have been related to the early removal of drainage devices, which should routinely be kept in place for three weeks and removed on the basis of the volume of drainage fluid.
Allograft resorption and fracture
Allograft resorption, occurring by the creeping substitution process, was observed in five patients at three‐year or longer follow‐up in the form of bone end resorption in three patients and bone segment resorption in the other two. Allograft fracture is thought to be caused mainly by a dramatic decrease in bone strength as a result of consistent bone resorption 7 , 8 .
In line with the reported incidence of allograft fracture, which ranges from 12% to 27% 9 , three of the twelve patients (25%) treated by prosthetic reconstruction developed fractures. More specifically, two patients had subchondral fractures, for which they received no treatment because they were clinically asymptomatic, and the other one had a metaphyseal fracture which was treated by a second osteoarticular allograft.
We initially used bone plates, intramedullary nails, or both, to fix the allografts during reconstruction of the proximal humeri. Because compound bone cement has been reported to have the potential to strengthen allografts and decrease the incidence of fracture, later we used compound bone cement to fix the allografts. We found that, of the patients who underwent APC or osteoarticular allografts, those with compound bone cement fixation remained free of allograft fractures (n= 11), while three of the eight patients in whom compound bone cement was not used developed allograft fractures to varying extents. Therefore the incidence of allograft fracture might be related to the use of compound bone cement 10 , 11 . However since it has also been reported that compound bone cement compromises final union of the allograft and the host bone, we try to minimize the amount of bone cement between the allograft and the autogenous bone, and perform bone grafting where the ends make contact.
Delayed union of allograft
The complications of nonunion and delayed union of allograft and autogenous bone were seen in the prosthetic replacement and APC groups. In our review, six patients were found to have delayed union, but none had bony nonunion. Delayed union occurred only in patients who underwent surgery before 2002, which might be because the amount and extent of bone grafting was insufficient. Therefore after 2002 we performed extensive bone grafting around the contacting ends.
Joint instability
The incidence of shoulder joint instability following tumor resection has been reported to be as high as 55%. This may be related to the loss of a stable structure to support the shoulder due to resection of the shoulder cuff and joint capsule 5 , 12 . The incidence of shoulder joint instability was 40% in this study, mainly taking the forms of anterior subluxation and proximal migration. It has been noted that shoulder instability tends to be progressive and debilitating. In our cases of shoulder joint instability, the glenohumeral joint was noted to be only slightly ptotic during the immediate postoperative period. However it appears that, with time, attempted flexion of the shoulder recruits the long head of the triceps, the short head of the biceps, and the coracobrachialis muscles. Contraction of these muscles, progressive attenuation of the rotator cuff tendons, and lack of an anterior aspect of the deltoid together result in the humeral head being driven anteriorly and proximally. This dynamic deformity can be corrected passively if treated early, but with time it becomes permanent.
In shoulder abduction the deltoid pull the humeral head upwards, and this is opposed by the downward pull on the humeral head provided by the infraspinous and the subscapularis muscles. At present reconstructive procedures for the rotator cuff stress reconstruction of the upper parts of the rotator cuff tissues, while ignoring the lower parts of these tissues. Therefore, the humeral head is progressively subjected to anterior subluxation and proximal migration in postoperative recovery exercises, and shoulder abduction becomes greatly limited without a stable force bearing point. Therefore reconstruction of the whole rotator cuff deserves attention in patients undergoing proximal humeral resection. In our early attempts at reconstruction, the soft tissues were attached to the lateral annulus of the allografts, which did not provide reconstruction of the rotator cuff tissues; reconstruction of the subscapularis muscle was also ignored in these early attempts, which might be an important reason for postoperative subluxation of the humeral head. Our review has confirmed that shoulder instability after reconstruction is not related to the nature of the tumors but rather to the site of those tumors (intra‐articular or extra‐articular). The incidence of shoulder instability was significant greater in those with extra‐articular tumor, because more rotator cuff tissue had to be resected. Our results suggest that reconstruction of the rotator cuff, well‐designed prostheses, recovery of the rotator cuff, and good local soft tissue balance techniques play key roles in improving function and stability of the shoulder joint.
References
- 1. Malawer MM, Meller I, Dunham WK. A new surgical classification system for shoulder‐girdle resections. Analysis of 38 patients. Clin Orthop Relat Res, 1991, 267: 33–44. [PubMed] [Google Scholar]
- 2. Enneking WF, Dunham W, Gebhardt MC, et al. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res, 1993, 286: 241–246. [PubMed] [Google Scholar]
- 3. Wittig JC, Bickels J, Kellar‐Graney KL, et al. Osteosarcoma of the proximal humerus: long‐term results with limb‐sparing surgery. Clin Orthop Relat Res, 2002, 397: 156–176. [DOI] [PubMed] [Google Scholar]
- 4. Shin KH, Park HJ, Yoo JH, et al. Reconstructive surgery in primary malignant and aggressive benign bone tumor of the proximal humerus. Yonsei Med J, 2000, 41: 304–311. [DOI] [PubMed] [Google Scholar]
- 5. Rödl RW, Gosheger G, Gebert C, et al. Reconstruction of the proximal humerus after wide resection of tumours. J Bone Joint Surg Br, 2002, 84: 1004–1008. [DOI] [PubMed] [Google Scholar]
- 6. Fuhrmann RA, Roth A, Venbrocks RA. Salvage of the upper extremity in cases of tumorous destruction of the proximal humerus. J Cancer Res Clin Oncol, 2000, 126: 337–344. [DOI] [PubMed] [Google Scholar]
- 7. Torbert JT, Fox EJ, Hosalkar HS, et al. Endoprosthetic reconstructions: results of long‐term follow up of 139 patients. Clin Orthop Relat Res, 2005, 438: 51–59. [DOI] [PubMed] [Google Scholar]
- 8. Getty PJ, Peabody TD. Complications and functional outcomes of reconstruction with an osteoarticular allograft after intra‐articular resection of the proximal aspect of the humerus. J Bone Joint Surg Am, 1999, 81: 1138–1146. [DOI] [PubMed] [Google Scholar]
- 9. Kassab M, Dumaine V, Babinet A, et al. Twenty nine shoulder reconstructions after resection of the proximal humerus for neoplasm with mean 7‐year follow‐up. Rev Chir Orthop Reparatrice Appar Mot, 2005, 91: 15–23. [DOI] [PubMed] [Google Scholar]
- 10. DeGroot H, Donati D, Di Liddo M, et al. The use of cement in osteoarticular allografts for proximal humeral bone tumors. Clin Orthop Relat Res, 2004, 427: 190–197. [DOI] [PubMed] [Google Scholar]
- 11. Taira H, Yoshida S, Takasita M, et al. Limb salvage for malignant bone and soft‐tissue tumours of the shoulder girdle. Int Orthop, 2003, 27: 136–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. O'Connor MI, Sim FH, Chao EY. Limb salvage for neoplasms of the shoulder girdle. Intermediate reconstructive and functional results. J Bone Joint Surg Am, 1996, 78: 1872–1888. [DOI] [PubMed] [Google Scholar]


