Abstract
This observational study describes trends in emergency department visits and admission rates among US acute care hospitals using data from the National Emergency Department Survey.
Hospital-based care accounts for approximately one-third of US health expenditures, and increasingly, most hospitalizations originate from emergency departments (ED).1,2,3 Value-based payment programs have focused on decreasing avoidable ED visits and hospitalizations. We describe trends in ED visits and admission rates among US acute care hospitals from January 1, 2006, through December 31, 2014.
Methods
We performed a retrospective observational study of the National Emergency Department Survey, using sampling weights and strata to generate national estimates. We examined patient-level characteristics, including age, sex, insurance, median income of patient zip code, and Elixhauser comorbidity score. Admission rate from the ED was defined as the number of admissions originating in the ED divided by the number of ED visits. We excluded visits of those 18 years or younger; those who left without being seen or against medical advice, transferred, or died on arrival in the ED; and those missing disposition. Data were analyzed from January 1, 2006, through December 31, 2014. Use of this publicly available dataset does not constitute human subjects research, and therefore did not require review by our institution’s review board.
Results
From 2006 through 2014, annual ED visits increased by 18.4%, from 89.6 to 106.0 million, and total ED hospitalizations increased by 6.8%, from 17.4 to 18.6 million. During the same period, ED admission rates fell from 19.4% to 17.5%, a 9.8% relative decline.
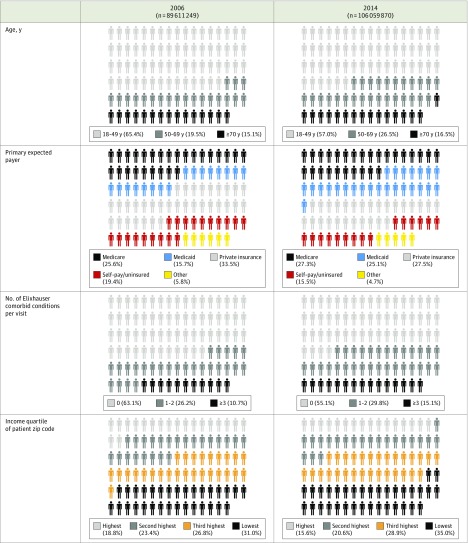
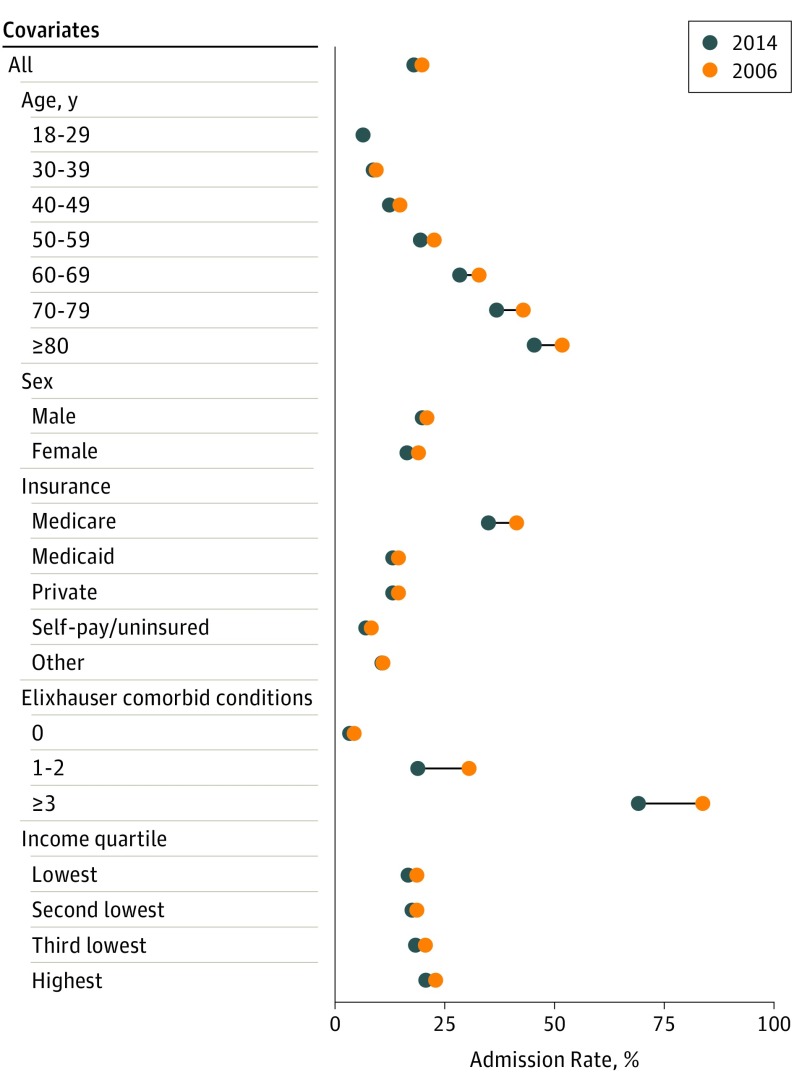
The proportion of ED visits by patients older than 50 years, with Medicare or Medicaid insurance, with 1 or more comorbid Elixhauser conditions, and from lower income areas increased from 2006 to 2014 (Figure 1). Patients of increasing age experienced larger reductions in ED admission rates, and ED admission rates decreased the most among Medicare-reimbursed ED visits relative to other insurance types (Figure 2). Patients with the most comorbid illness experienced the largest magnitude decrease in admission rates from the ED—by 15% among patients with at least 3 comorbid Elixhauser conditions, and by 11% among patients with 1 to 2 comorbid Elixhauser conditions.
Figure 1. Patient Characteristics of Adult Emergency Department (ED) Visits, 2006 and 2014.
The proportion of ED visits by female patients was 56.7% in 2006 and 57.6% in 2014. Data are obtained from the National Emergency Department Survey, using sampling weights and strata to generate national estimates. Percentages of patients have been rounded and may not total 100. Each data marker represents 1% of US ED visits.
Figure 2. Emergency Department Admission Rate.
Data are obtained from the National Emergency Department Survey, using sampling weights and strata to generate national estimates.
Discussion
From 2006 to 2014, ED visits increased 18.4%, and ED admission rates decreased 9.8%. The increase in ED visits, outpacing population growth, underscores an unabating demand for acute, unscheduled care. Declining ED admission rates represent a significant reduction in hospital-based care that has received little attention to date.
Our findings are unlikely to be explained by lower acuity ED visits, given the increase in age and comorbidities. In fact, ED visits with the highest burden of comorbid illness experienced the largest reductions in ED admission rates. Decreasing ED admissions may be attributed to a combination of clinical factors, such as outpatient clinical pathways (eg, diagnostic protocols for chest pain), and policy factors, such as the 2010 Recovery Audit Contractor program and 2014 Two-Midnight Rule, which increased scrutiny of short-stay hospitalizations, and the 2009 Patient Protection and Affordable Care Act,4 which contributed to increased ED visits and improved access to follow-up care, likely reducing hospitalizations.5 Increases in non-ED admissions are also unlikely to explain our findings, given prior work demonstrating that, increasingly, most hospitalizations originate from the ED.2
Further research is needed to examine unintended consequences of reduced ED admissions, such as morbidity, mortality, readmissions, or ED revisits. Our findings are limited by our administrative data set, which lacks data on clinical factors and use of observation care; however, the 0.4% increase in observation care from 2006 to 2014 is less than the 1.9% reduction in hospitalization we observed.6 The increase in comorbid conditions per visit can be explained in part by more complete documentation, which has contributed to decreases in hospital readmission rates7; however, documentation likely does not explain the entire observed effect, given the increasing age among ED visits. Our findings highlight the major role EDs play in the shift from inpatient to outpatient care—a role that will expand as ED visits and the proportion of hospitalizations originating in the ED continue to increase.
References
- 1.Centers for Medicare & Medicaid Services National Health Expenditure Fact Sheet, 2015. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html Updated April 17, 2018. Accessed May 22, 2018.
- 2.Gonzalez Morganti K, Bauhoff S, Blanchard JC, et al. . The Evolving Role of Emergency Departments in the United States. Santa Monica, CA: RAND Corporation; 2013. [PMC free article] [PubMed] [Google Scholar]
- 3.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;367(5):391-393. doi: 10.1056/NEJMp1204431 [DOI] [PubMed] [Google Scholar]
- 4.McClelland M, Asplin B, Epstein SK, et al. . The Affordable Care Act and emergency care. Am J Public Health. 2014;104(10):e8-e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medicare Payment Advisory Committee Chapter 7: Hospital Short-Stay Policy Issues. June 2015. Report. http://www.medpac.gov/docs/default-source/reports/chapter-7-hospital-short-stay-policy-issues-june-2015-report-.pdf?sfvrsn=0. Accessed May 22, 2018.
- 6.National Center for Health Statistics National Hospital Ambulatory Medical Care Survey: 2014 Emergency Department Summary Tables. 2https://www.cdc.gov/nchs/data/nhamcs/web_tables/2014_ed_web_tables.pdf. 2014. Accessed May 22, 2018.
- 7.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of coded severity with readmission reduction after the hospital readmissions reduction program. JAMA Intern Med. 2018;178(2):290-292. doi: 10.1001/jamainternmed.2017.6148 [DOI] [PMC free article] [PubMed] [Google Scholar]