Abstract
Objective
To evaluate the clinical use of kinetic magnetic resonance imaging (kMRI) in spinal degenerative diseases.
Methods
A systematic search of PubMed, EMBASE and ISI databases for articles that had been published between January 1978 and February 2013 concerning patients who had undergone kMRI for spinal problems was performed. All selected patients had undergone kMRI in neutral, flexion, and extension weight‐bearing positions. Evaluation of cervical and lumbar degeneration by kMRI was analyzed. kMRI showed significant reduction of mobility in cervical segments of patients with severe disc degeneration; in addition, it was more severely reduced in patients with severe cord compression than in those without it. In the cervical spine, it was found that although disc height, translational motion, and angular variation were significantly affected at the level of disc herniation, no significant changes were apparent in adjacent segments. kMRI also showed that lumbar degeneration is closely associated with disc degeneration, facet joint osteoarthritis and the pathological characteristics of the interspinous ligaments, ligamentum flavum and paraspinal muscles.
Results
Eleven articles (4162 patients) fulfilled the inclusion criteria and were reviewed. It was found that kMRI is more specific and sensitive than conventional MRI regarding relating patients' symptoms to objective findings on imaging that demonstrate pathology and biomechanics. In the kinetic position, kMRI improves detection of disc herniation by 5.78%–19.46% and thus provides a new means of studying the biomechanical mechanism(s) in degenerative spines.
Conclusion
Kinetic MRI is effective for diagnosing, evaluating, and managing degenerative disease within the spine; however, it still has some limitations.
Keywords: Cervical degeneration, Kinetic magnetic resonance imaging, Lumbar degeneration, Spinal degeneration
Introduction
Spinal degeneration is increasingly common as a result of population aging. Degeneration in the intervertebral discs typically begins during the second decade of life in men and the third decade in women1. Degeneration then appears posteriorly in the facet joints, causing altered mechanical function of the disc and ultimately spinal instability and clinical symptoms2. Of the imaging techniques currently available, magnetic resonance imaging (MRI) provides the greatest range of information and most accurate delineation of soft‐tissue and osseous structures, enabling detection of subtle abnormalities with great sensitivity3. However, it provides only non‐weight‐bearing, static images, whereas spinal disorders, especially cervical and lumbar stenosis, are posture‐dependent. To overcome this limitation, radiographic studies of spinal kinematics have been reported.
Kinetic MRI (kMRI) can image patients in a weight‐bearing position (either standing up or sitting) and in flexed and extended positions, thus revealing abnormalities that are missed by traditional MRI studies4, 5, 6. It more thoroughly investigates each patient and facilitates better understanding of the the true nature of the pathology7. Imaging the spine in a weight‐bearing position with extension and flexion or placing the spine in the position of pain may increase the diagnostic accuracy for spine surgeons8. In this article, we review the use of kinetic MRI (kMRI) to assess spinal kinematics of patients in weight‐bearing positions with dynamic motion of the spine (Figs 1, 2).
Figure 1.

Cervical kMRI in a 56‐year‐old man. T2‐weighted sagittal kMRI images in the (A) neutral position, (B) flexion position and (C) extension position. (D) Axial image revealing disc herniation at C 4–5.
Figure 2.

Lumbar kMRI in a 40‐year‐old woman. T2‐weighted sagittal kMRI images in (A) the neutral position, (B) flexion position and (C) extension position. (D) Axial image revealing minor disc bulging at L 4–5.
Materials and Methods
Eligibility Criteria
Using the key words “magnetic resonance imaging”, “kinetic/kinematic magnetic resonance imaging”, “spinal degeneration”, “cervical degeneration” and “lumbar degeneration”, a comprehensive search of PubMed, EMBASE and ISI databases for articles with English language full texts that had been published between January 1978 and February 2013 was performed. All relevant articles were collected and their references reviewed. All the identified studies were reviewed by two independent investigators for content. Any study that did not mention kMRI or spinal degeneration was excluded from further assessment (Fig. 3).
Figure 3.
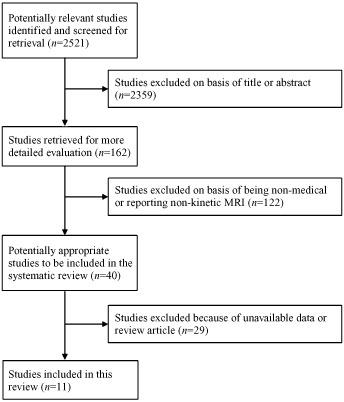
Flow diagram of selection of studies and specific reasons for exclusion.
Technical Parameters of Kinetic Magnetic Resonance Imaging
In the assessed studies, all of which originated from a single spine center in Los Angeles, CA, USA, kMRI scans of lumbar and cervical spines of symptomatic or asymptomatic patients in axially loaded, upright neutral, flexion, and extension positions were taken with a 0.6 Tesla kMRI scanner (Fonar, Melville, NY, USA) with a flexible surface coil. Imaging took 10 to 12 min to complete in each position. The imaging protocols included sagittal T1‐weighted spin‐echo sequences (repetition time [TR]/echo time [TE], 671/17 ms; slice thickness, 3.0 mm; field of view, 24 cm; matrix, 256 × 200; and number of excitations [NEX], 2) and T2‐weighted fast spin‐echo sequences (TR/TE, 3432/160 ms; slice thickness, 3.0 mm; field of view, 24 cm; and NEX, 2). All sequences were acquired without fat saturation. T2‐weighted mid‐sagittal images in the three positions were analyzed. Data were assessed using an MR analyzer.
Results
Evaluation of Cervical Degeneration by kMRI
In two of the selected studies, the patients had cervical disc degeneration that affected the mobility of this functional unit9, 10. In one of these studies, cervical kMRI was performed on 459 symptomatic patients. In normal cervical spines, most of the total angular mobility is attributable to C4–5 and C5–6; in this study cervical kMRI showed that mobility was significantly reduced in these segments in patients with severe disc degeneration10. In the other study, 1445 functional cervical units of 289 symptomatic subjects were examined by kMRI9. Cervical segmental mobility was significantly reduced in segments with severe cord compression compared with those with no cord compression. Morishita et al. postulated that the spinal cord is protected from dynamic mechanical cord compression restricting segmental motion and that the mechanisms of this are closely related to the intervertebral discs9.
Effects of Cervical Disc Herniation on Kinematics in Adjacent Vertebral Motion Segments
Another study reported using kMRI to evaluate 407 patients with neck pain and no prior history of surgery11. Although disc height, translational motion, and angular variation were significantly affected at the level of disc herniation, no significant changes were apparent in adjacent segments. These findings indicate that, regardless of the degree of disc degeneration or the size of disc herniation, herniated discs have no effect on range of motion in adjacent levels, suggesting that the natural progression of disc degeneration and adjacent segment disease may be separate, unrelated processes within the cervical spine11.
Changes in sagittal alignment of the cervical spine affect the kinematics and progress of cervical intervertebral disc degeneration, as shown by another series of 267 consecutive patients who underwent kMRI scans of the cervical spine12. Changes in sagittal alignment of the cervical spine were found to affect the kinematics and the contribution of each segment to total angular mobility. Consequently, there may be changes in overall motion when the segment is subjected to maximum load that accelerate its degeneration. Based on their findings, Miyazaki et al. recommended that cervical surgery such as cervical discectomy and fusion or artificial disc replacement should attempt to restore lordosis to prevent further degeneration and symptomatic deterioration12.
Relationship between Grade of Disc Degeneration and Motion Unit of the Cervical Spine
Dvir et al. used kMRI to evaluate164 patients with neck pain13. They found that the degenerative process affects the mobility of the functional spinal unit, which moves from a normal disc to a more unstable phase with increased mobility and further degeneration. However, as the degeneration enters the later phases and becomes more severe, the range of motion stabilizes because ankylosis develops13.
Evaluation of Lumbar Degeneration by kMRI
Lumbar degeneration is closely associated with abnormal segmental motion. Kong et al. performed kMRI on 1575 functional spine units in 315 patients14. They found that abnormal segmental motion noted on kinetic MR images is closely associated with disc degeneration, facet joint osteoarthritis, and the pathological characteristics of the interspinous ligaments, ligamentum flavum and paraspinal muscles. By measuring abnormal segmental motion and grading radiographic parameters simultaneously, kMRI of patients with mechanical back pain may provide valuable information about the stability of the functional spine unit14.
Two studies that comprehensively evaluated lumbar stability by kMRI were identified15, 16. Their findings supported the contentions that facet joint degeneration is followed by disc degeneration with increasing age and that segmental mobility is influenced by disc degeneration, facet joint osteoarthritis and ligament pathology. Therefore, the status of the intervertebral discs, facet joints and ligamentum flavum should be taken into consideration when evaluating stability within the lumbar spine15, 16.
The detection of lumbar disc herniation is improved by kMRI. Zou et al. reported kMRI findings in 553 patients with symptomatic back pain, both with and without radiculopathy, who had been referred for lumbar spine examination by MRI17. Significantly more severe lumbar disc herniation was found by examining flexion and extension views than by examining neutral views alone. kMRI views provide valuable added information, especially in patients with symptomatic radiculopathy in whom no abnormalities are evident on conventional MRI17.
Do et al. used kMRI to assess the relationship between degree of facet tropism and amount of dynamic disc bulge in the lumbar spine in 410 consecutive patients with low back pain18. Their findings suggested that severe facet tropism is only associated with increased disc bulge at L4–L5 in a subset of older patients (Table 1).
Table 1.
List of published articles concerning kMRI analysis of the spinal degeneration and relevant data from those articles
| Author | Year | Journal | Number of patients | Body part | With/without symptoms | Research priority | Conclusions |
|---|---|---|---|---|---|---|---|
| Morishita10 | 2008 | J Orthop Surg | 1046 | Cervical Lumbar | Symptomatic | Diagnosis of disc herniation | kMRI effective for evaluating degeneration |
| Morishita9 | 2008 | Spine (Phila Pa 1976) | 289 | Cervical | Symptomatic | Effect of degeneration | Cervical cord compression exacerbates cervical function |
| Daffner11 | 2009 | Spine (Phila Pa 1976) | 407 | Cervical | Symptomatic | Adjacent vertebral motion | Herniated discs have no effect on adjacent vertebral motion |
| Miyazaki12 | 2008 | Spine (Phila Pa 1976) | 267 | Cervical | Symptomatic | Sagittal alignment | Sagittal alignment changes affect cervical kinematics |
| Miyazaki13 | 2008 | Spine (Phila Pa 1976) | 164 | Cervical | Symptomatic | Degeneration and motion | Degeneration affects the mobility of spinal unit |
| Kong14 | 2009 | J Neurosurg Spine | 315 | Lumbar | Symptomatic | Abnormal segmental motion | Abnormal segmental motion related to disc degeneration |
| Kong16 | 2009 | Spine (Phila Pa 1976) | 316 | Lumbar | Symptomatic | Facet joint degeneration | Facet joint degeneration affects lumbar mobility |
| Zou17 | 2008 | Spine (Phila Pa 1976) | 553 | Lumbar | Symptomatic | Detection of disc herniation | kMRI helps detection of disc herniation |
| Do18 | 2011 | Eur Spine J | 410 | Lumbar | Symptomatic | Facet tropism | Facet tropism associated with increased disc bulge |
| Morishita19 | 2009 | Spine (Phila Pa 1976) | 295 | Cervical | Symptomatic | Upper cervical spine | Atlantoaxial joint related to spinal cord protection |
| Tan20 | 2012 | Eur Spine J | 100 | Lumbar | Symptomatic | Lumbar mobility | Translational motion is greatest in proximal levels |
Discussion
Traditional MR imaging can be a powerful tool for assessing disc degeneration and herniation21. However, standard MR imaging studies are limited by the fact that they can only assess patients in a horizontal non‐weight‐bearing position. Thus, they provide only static images and the causes of some problems are not visible in a non‐weight‐bearing position. kMRI technology has recently been developed to allow investigators to examine and analyze mechanical instability in neutral, flexion and extension weight‐bearing positions. kMRI is useful for quantifying reduction in cervical and lumbar spine range of motion and changes in disc height and is thus a valuable adjunct in patients suspected of having lumbar segmental instability, especially when symptoms are triggered by particular postures22.
The spine is subjected to great compressive forces during activities of daily living2. Mechanical loading of the spine (caused by axial compression and dynamic motion) puts mechanical stress on the intervertebral discs; this is an important factor in the development of intervertebral disc degeneration. Therefore, it is helpful to evaluate patients with spinal disorders under mechanical loading. For this reason, kMRI is useful for diagnosing, evaluating and managing degenerative disease or injury within the spine. Some researchers have reported that some patients require pain control prior to kMRI because they experience severe discogenic or radicular pain in upright, weight‐bearing positions9, 10. It is difficult for such patients to maintain their position for more than 30 min. Because patients with severe myelopathy should avoid dynamic motion or superfluous loading, neurological evaluation and observation prior to and during kMRI may be necessary.
So far, the effects of degenerative discs on adjacent segmental motion have not been fully elucidated. Dvir et al. used kMRI to determine segmental motion, angular variation and disc height at levels adjacent to disc herniations using different dynamic, weight‐bearing positions23. These authors had previously demonstrated the advantages of using kMRI for evaluating intervertebral motion. Because its can image patients in various weight‐bearing positions, kMRI provides additional diagnostic capabilities compared with other radiographic techniques. In addition, kMRI provides a thorough assessment of motion and can identify discontinuities in intervertebral motion that would be missed using only supine MRI images or dynamic radiographs.
In the future, it would be useful to compare long‐term clinical and kMRI findings as they pertain to cervical disc herniation, disc degeneration and adjacent segment disease. This would allow for a greater understanding of the nature of the relationship between these two disorders. Despite its limitations, it is believed that use of kMRI technology to evaluate changes in cervical range of motion at levels adjacent to disc herniation has provided unique insights into adjacent segment kinematics. kMRI has also been used to evaluate upper cervical mobility. Morishita et al. performed cervical kMRI on 295 consecutive patients with neck pain but without neurologic symptoms19. Their findings suggested that only the kinematics of atlantoaxial movement, particularly posterior movement, is greatly affected by narrowing of the space available for the cord. The central atlantoaxial joint may be closely involved in the mechanisms for protecting the spinal cord by restricting atlantoaxial movement19.
The potential benefits of kMRI f spinal imaging over that of recumbent MRI (rMRI) include the identification of occult spinal disease that is dependent on true axial loading, the unmasking of kinetic‐dependent spinal disease and the ability to scan the patient in the position(s) that are associated with clinically relevant signs and symptoms. The imaging unit that is under study has low claustrophobic potential and yields comparatively high resolution images with little motion or shift artifact. Overall, studies have shown that rMRI underestimates the presence and maximum degree of gravity‐dependent spinal pathology and misses pathology of a dynamic nature or factors that are more apparent with kMRI. Furthermore, by identifying the abnormality responsible for their clinical presentation, kMRI enables optimal linkage of the patient's clinical syndrome with the responsible abnormality, thereby providing improvements over currently available imaging technologies in both imaging sensitivity and specificity24.
In their study, Zou et al. graded cervical disc degeneration using MRI and measured the motion with kMRI17. They found changes in translational motion and angular variation in each cervical unit following degeneration. Translational motion changed as the disc degenerated from its normal state to an unstable phase and finally to an ankylosed stage with increased stability. Angular variation decreases significantly in severe degeneration. It is believed that kinetic MRI can be used in clinical practice to examine spinal intervertebral mobility and determine the most appropriate treatment by studying the progression of disc degeneration (i.e., whether the disc eventually stabilizes or continues to degenerate).
Conventional MRI scanners can only obtain images of patients in prone and supine positions. In addition, conventional MRI cannot portray dynamic segmental motion. It also cannot image patients in weight‐bearing positions, which are optimal for accurately determining motion. However, the recent development of kMRI technology allows patients to be imaged in various weight‐bearing positions. kMRI is an outstanding tool for dynamic detection of segmental instability. It is capable of imaging patients in upright neutral, flexion, and extension weight‐bearing positions. Therefore it is a promising means of investigating conditions that can lead to spinal instability. Karadimas et al. studied lumbar segmental motion in healthy and degenerative discs using positional MR images and found that changes in segmental motion were related to the degree of disc degeneration21. In another study, Tan et al. evaluated lumbar segmental mobility in patients without significant degenerative disc disease and found that translational motion was greatest in the proximal lumbar levels, whereas angular motion was similar in the mid‐lumbar levels but decreased at L1–L2 and L5–S1 20.
Today, kMRI can deliver the ability to scan patients in a weight‐bearing position. This allows imaging of patients in the exact position that elicits symptoms, thus providing a detailed evaluation of musculoskeletal pathology. The potential benefits of kMRI spinal imaging over conventional MRI include the unmasking of positionally related pathologies and the ability to scan the patient in the position in which clinically relevant signs and symptoms occur. It may prove useful to incorporate kMRI when making a diagnosis and selecting treatment in patients with spinal, radicular and referred pain syndromes originating from spinal pathology. Furthermore, kMRI may more specifically and sensitively relate patients' clinical symptoms with the responsible pathology than conventional MRI studies.
Though kMRI is still being developed, it does still have some limitations. First, the hardware is costly for the hospital and the procedure expensive and time‐consuming for the patients. Second, some patients with severe neurologic symptoms would not be able to tolerate a positional MRI scan. Third, this is a review and not a meta‐analysis. Therefore, we cannot truly compare its effectiveness with that of other modalities. The studies we identified are so inherently different that it is difficult to draw specific conclusions or combine data for meta‐analysis. Because most of the reviewed studies are from single institutions, study bias was unavoidable. No detailed clinical data on the reported patients is available, only their objective imaging findings. All patients were “symptomatic” (back, neck, leg or arm pain); there are no control data for asymptomatic patients. However, despite these limitations, we believe that the results of the reviewed studies are likely to reflect clinical use of kMRI for spinal degenerative diseases.
In conclusion, kMRI is effective for diagnosing, evaluating and managing degenerative disease within the spine, but still has some limitations. In particular, kMRI improves detection of missed spinal disc herniation and provides a new modality for studying the biomechanical mechanisms in degenerative spine units. kMRI may more specifically and sensitively relate the patient's clinical symptoms to objective evidence of the responsible pathology than conventional MRI.
Disclosure: No funds were received in support of this work.
References
- 1. Zigler JE, Strausser DW. The aging spine In: Fardon DF, Garfin SR, Abitbol et al. eds. Orthopaedic knowledge update: spine 2. Rosemont: American Academy of Orthopaedic Surgeons, 2002, 123–133. [Google Scholar]
- 2. Avinash GP, Ioannis NG, Leonard IV. Biomechanics of the spine In: Spivak JM, Connolly PJ, eds. Orthopaedic knowledge update: spine 3. Rosemont: American Academy of Orthopaedic Surgeons, 2006, 25–32. [Google Scholar]
- 3. Yu WD, Williams SL. Spinal imaging: radiographs, computed tomography, and magnetic resonance imaging In: Spivak JM, Connolly PJ, eds. Orthopaedic knowledge update: spine 3. Rosemont: American Academy of Orthopaedic Surgeons, 2006, 57–67. [Google Scholar]
- 4. Ruangchainikom M, Daubs MD, Suzuki A, et al Effect of cervical kyphotic deformity type on the motion characteristics and dynamic spinal cord compression. Spine (Phila Pa 1976), 2014, 39: 932–938. [DOI] [PubMed] [Google Scholar]
- 5. Lord EL, Alobaidan R, Takahashi S, et al Kinetic magnetic resonance imaging of the cervical spine: a review of the literature. Global Spine J, 2014, 4: 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hayashi T, Daubs MD, Suzuki A, Phan K, Shiba K, Wang JC. Effect of Modic changes on spinal canal stenosis and segmental motion in cervical spine. Eur Spine J, 2014, 23: 1737–1742. [DOI] [PubMed] [Google Scholar]
- 7. Li YW, Lord E, Cohen Y, et al Effects of sagittal endplate shape on lumbar segmental mobility as evaluated by kinetic magnetic resonance imaging. Spine (Phila Pa 1976), 2014, 39: E1035–1041. [DOI] [PubMed] [Google Scholar]
- 8. Lao LF, Daubs MD, Scott TP, Phan KH, Wang JC. Missed cervical disc bulges diagnosed with kinematic magnetic resonance imaging. Eur Spine J, 2014, 23: 1725–1729. [DOI] [PubMed] [Google Scholar]
- 9. Morishita Y, Hida S, Miyazaki M, et al The effects of the degenerative changes in the functional spinal unit on the kinematics of the cervical spine. Spine (Phila Pa 1976), 2008, 33: E178–E182. [DOI] [PubMed] [Google Scholar]
- 10. Morishita Y, Hymanson H, Miyazaki M, et al Kinematic evaluation of the spine: a kinetic magnetic resonance imaging study. J Orthop Surg (Hong Kong), 2008, 16: 348–350. [DOI] [PubMed] [Google Scholar]
- 11. Daffner SD, Xin J, Taghavi CE, et al Cervical segmental motion at levels adjacent to disc herniation as determined with kinetic magnetic resonance imaging. Spine (Phila Pa 1976), 2009, 34: 2389–2394. [DOI] [PubMed] [Google Scholar]
- 12. Miyazaki M, Hymanson HJ, Morishita Y, et al Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. Spine (Phila Pa 1976), 2008, 33: E870–E876. [DOI] [PubMed] [Google Scholar]
- 13. Miyazaki M, Hong SW, Yoon SH, et al Kinematic analysis of the relationship between the grade of disc degeneration and motion unit of the cervical spine. Spine (Phila Pa 1976), 2008, 33: 187–193. [DOI] [PubMed] [Google Scholar]
- 14. Kong MH, Hymanson HJ, Song KY, et al Kinetic magnetic resonance imaging analysis of abnormal segmental motion of the functional spine unit. J Neurosurg Spine, 2009, 10: 357–365. [DOI] [PubMed] [Google Scholar]
- 15. Jang SY, Kong MH, Hymanson HJ, Jin TK, Song KY, Wang JC. Radiographic parameters of segmental instability in lumbar spine using kinetic MRI. J Korean Neurosurg Soc, 2009, 45: 24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kong MH, Morishita Y, He W, et al Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology by using kinetic magnetic resonance imaging. Spine (Phila Pa 1976), 2009, 34: 2537–2544. [DOI] [PubMed] [Google Scholar]
- 17. Zou J, Yang H, Miyazaki M, et al Missed lumbar disc herniations diagnosed with kinetic magnetic resonance imaging. Spine (Phila Pa 1976), 2008, 33: E140–E144. [DOI] [PubMed] [Google Scholar]
- 18. Do DH, Taghavi CE, Fong W, Kong MH, Morishita Y, Wang JC. The relationship between degree of facet tropism and amount of dynamic disc bulge in lumbar spine of patients symptomatic for low back pain. Eur Spine J, 2011, 20: 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Morishita Y, Falakassa J, Naito M, Hymanson HJ, Taghavi C, Wang JC. The kinematic relationships of the upper cervical spine. Spine (Phila Pa 1976), 2009, 34: 2642–2645. [DOI] [PubMed] [Google Scholar]
- 20. Tan Y, Aghdasi BG, Montgomery SR, Inoue H, Lu C, Wang JC. Kinetic magnetic resonance imaging analysis of lumbar segmental mobility in patients without significant spondylosis. Eur Spine J, 2012, 21: 2673–2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Karadimas EJ, Siddiqui M, Smith FW, Wardlaw D. Positional MRI changes in supine versus sitting postures in patients with degenerative lumbar spine. J Spinal Disord Tech, 2006, 19: 495–500. [DOI] [PubMed] [Google Scholar]
- 22. Waris E, Eskelin M, Hermunen H, Kiviluoto O, Paajanen H. Disc degeneration in low back pain. A 17‐year follow‐up study using magnetic resonance imaging. Spine (Phila Pa 1976), 2007, 32: 681–684. [DOI] [PubMed] [Google Scholar]
- 23. Dvir Z, Gal‐Eshel N, Shamir B, Prushansky T, Pevzner E, Peretz C. Cervical Motion in patients with chronic disorders of the cervical spine: a reproducibility study. Spine (Phila Pa 1976), 2006, 31: E394–E399. [DOI] [PubMed] [Google Scholar]
- 24. Jinkins JR, Dworkin JS, Damadian RV. Upright, weight‐bearing, dynamic‐ kinetic MRI of the spine: initial results. Eur Radiol, 2005, 15: 1815–1825. [DOI] [PubMed] [Google Scholar]


