Abstract
Importance
Although endovascular thrombectomy (EVT) in acute ischemic stroke is recommended by guidelines to improve functional recovery, thus far there are insufficient data on its association with mortality.
Objective
To identify guideline-relevant trials of EVT vs medical therapy reporting 90-day mortality and perform a meta-analysis.
Data Sources
All randomized clinical trials cited for recommendations on EVT vs medical therapy in the latest 2018 American Stroke Association/American Heart Association guidelines.
Study Selection
Ten American Stroke Association/American Heart Association guideline–relevant randomized clinical trials of EVT vs medical therapy were selected for inclusion. Two EVT trials were excluded owing to infrequent use of EVT.
Data Extraction and Synthesis
Data were abstracted by 2 independent investigators and double-checked by 4 others. Singular study data were integrated using the Cochran-Mantel-Haenszel method and a random-effects model to compute summary statistics of risk ratios (RR) with 95% CIs.
Main Outcomes and Measures
Risk of 90-day mortality and 90-day intracranial hemorrhage was analyzed; sensitivity analyses were performed in early-window EVT trials (which included patients from the onset of symptoms onward) vs late-window EVT trials (which included patients from 6 hours after onset of symptoms onward).
Results
In 10 trials with 2313 patients, EVT significantly reduced the risk for 90-day mortality by 3.7% compared with medical therapy (15.0% vs 18.7%; RR, 0.81; 95% CI, 0.68-0.98; P = .03). Trends were similar in early-window (RR, 0.83; 95% CI, 0.67-1.01; P = .06) and late-window trials only (RR, 0.76; 95% CI, 0.41-1.40; P = .38). There was no difference in the risk for intracranial hemorrhage in EVT vs medical therapy (4.2% vs 4.0%; RR, 1.11; 95% CI, 0.71-1.72; P = .65). Limitations of the studies include trial protocol heterogeneity and bias originating from prematurely terminated trials.
Conclusions and Relevance
This meta-analysis of all evidence on EVT cited in the 2018 American Stroke Association/American Heart Association guidelines shows significant benefits for survival during the first 90 days after acute ischemic stroke compared with medical therapy alone.
This meta-analysis examines 90-day mortality and 90-day intracranial hemorrhage reported in trials of endovascular thrombectomy vs medical therapy cited in the 2018 American Stroke Association/American Heart Association guidelines for acute ischemic stroke.
Key Points
Question
Is there a benefit for short-term survival with endovascular thrombectomy vs medical therapy in acute ischemic stroke?
Findings
In this meta-analysis of all randomized clinical trials of endovascular thrombectomy vs medical therapy cited in the 2018 American Stroke Association/American Heart Association guidelines for acute ischemic stroke, endovascular thrombectomy significantly reduced the risk for 90-day mortality compared with medical therapy, without a difference in risk of intracranial hemorrhage.
Meaning
There is considerable evidence of the benefits of endovascular thrombectomy for survival during the first 90 days after acute ischemic stroke.
Introduction
Twenty years after intravenous thrombolysis (IT) was established as the first-line therapy for acute ischemic stroke (AIS), several randomized clinical trials (RCTs)1,2,3,4,5,6 have proven benefits on functional recovery of endovascular thrombectomy (EVT) compared with medical therapy. The 2018 American Stroke Association/American Heart Association AIS guidelines7 thus adopted class IA to IIb recommendations for EVT in different clinical scenarios.
Parallels of this development with the history of the management of myocardial infarction are striking: in myocardial infarction as in AIS, IT was first established to improve clinical outcomes and then was found to be inferior to interventional strategies of primary percutaneous coronary intervention.8 However, unlike with the use of IT for myocardial infarction, mortality benefits of IT for AIS were not seen in short-term or long-term follow-up. In logic succession, all EVT trials focused on measures of functional recovery from AIS (Table)1,2,3,4,5,6,9,10,11,12 and were underpowered to detect differences in mortality, just like subsequent meta-analyses.13,14 Thus, it still remains unknown whether EVT also improves survival in AIS.
Table. Study Characteristics of Included Trials.
| Study | Journal | No. of Centers in Trial | No. of Patients (EVT/MT) | Randomization | Inclusion Criteria | Device Used | IT Use (% per Group) | Primary End Point(s) |
|---|---|---|---|---|---|---|---|---|
| DAWN,9 2018 | New England Journal of Medicine | 26 | 107/99 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA and M1) within 6-24 h, with NIHSS/imaging mismatch | 100% Trevo | 5/13 | Utility-weighted mRS at 90 d; mRS score 0-2 at 90 d |
| DEFUSE 3,10 2018 | New England Journal of Medicine | 38 | 92/90 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA and M1) within 6-16 h, with penumbra/infarct mismatch (CT perfusion/MRI) | 74% Stent retriever, 25% aspiration | 11/9 | mRS at 90 d |
| ESCAPE,11 2015 | New England Journal of Medicine | 22 | 165/150 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA and M1) within 12 h | 77% Solitaire, 9% other | 73/79 | mRS at 90 d |
| EXTEND-IA,2 2015 | New England Journal of Medicine | 14 | 35/35 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA, M1, and M2) within 4.5 h | 100% Solitaire | 100/100 | Perfusion at 24 h; early improvement (NIHSS) at 24 h |
| MR CLEAN,6 2015 | New England Journal of Medicine | 16 | 233/267 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA, M1, M2, A1, and A2) within 4.5 h | 81.5% Stent retriever | 87/91 | mRS at 90 d |
| MR RESCUE,12 2013 | New England Journal of Medicine | 22 | 64/54 | Endovascular therapy + MT vs MT alone | Anterior stroke within 8 h | 58% Merci, 22% Penumbra, 17% both | 44/30 | Correlation of penumbral imaging (CT/MRI) with mRS at 90 d |
| REVASCAT,4 2015 | New England Journal of Medicine | 4 | 103/103 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA and M1) within 8 h | 95% Solitaire | 68/78 | mRS at 90 d |
| SWIFT PRIME,3 2015 | New England Journal of Medicine | 39 | 98/97 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA and M1) within 6 h | 100% Solitaire | 100/100 | mRS at 90 d |
| THERAPY,5 2016 | Stroke | 36 | 55/53 | Endovascular therapy + MT vs MT alone | Anterior stroke (ICA and MCA) and thrombus length ≥8 mm | 100% Penumbra | 100/100 | mRS 0-2 at 90 d |
| THRACE,1 2016 | Lancet Neurology | 26 | 204/208 | Endovascular therapy + MT vs MT alone | Stroke (ICA, M1, and BA) within 4 h | 77% Solitaire, 15% Penumbra, 7% other | 100/100 | mRS 0-2 at 90 d |
Abbreviations: A1, A1 segment of the anterior cerebral artery; A2, A2 segment of the anterior cerebral artery; BA, basilar artery; CT, computed tomography; DAWN, DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention With Trevo; DEFUSE 3, Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke; ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing CT to Recanalization Times; EVT, endovascular thrombectomy; EXTEND-IA, Extending the Time for Thrombolysis in Emergency Neurological Deficits—Intra-Arterial; ICA, internal carotid artery; IT, intravenous thrombolysis; M1, M1 segment of middle cerebral artery; M2, M2 segment of middle cerebral artery; MCA, middle cerebral artery; MR CLEAN, Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands; MR RESCUE, Mechanical Retrieval and Recanalization of Stroke Clots Using Embolectomy; MRI, magnetic resonance imaging; mRS, modified ranking scale; MT, medical therapy; NIHSS, National Institutes of Health Stroke Scale; REVASCAT, Randomized Trial of Revascularization With Solitaire FR Device vs Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting Within Eight Hours of Symptom Onset; SWIFT PRIME, Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment; THERAPY, The Randomized, Concurrent Controlled Trial to Assess the Penumbra System’s Safety and Effectiveness in the Treatment of Acute Stroke; THRACE, Mechanical Thrombectomy After Intravenous Alteplase vs Alteplase Alone After Stroke.
Methods
To approach this question, RCTs comparing EVT vs medical therapy for treatment of AIS were selected from all guideline-referenced RCTs on endovascular therapy in the 2018 American Stroke Association/American Heart Association guideline.7 Methods were applied according to Cochrane Collaboration and PRISMA recommendations: 2 independent investigators (Y.L. and G.W.) performed intention-to-treat data abstractions on study characteristics, risk of bias, and 90-day mortality and 90-day intracranial hemorrhage outcomes from published reports, which were double-checked accordingly by 4 of us (V.S., M.B., C.P., and A.K.). Risk ratios (RRs) and 95% CIs were used as summary statistics, and singular studies were integrated with the Cochran-Mantel-Haenszel method and a random-effects model. Statistical heterogeneity was quantified with the I2 statistic. A 2-tailed P < .05 was considered statistically significant.
Results
Included trial characteristics are shown in the Table1,2,3,4,5,6,9,10,11,12: 10 RCTs of EVT vs medical therapy referenced in the 2018 American Stroke Association/American Heart Association guideline7 with a total of 2313 patients and a consistent follow-up of 90 days were included. Excluded trial characteristics are shown in eTable 1 in the Supplement: 5 trials were excluded for the wrong comparators, and trials were excluded for using EVT devices in only a minority of patients (mainly those with intra-arterial thrombolysis). Risk of bias of included trials was generally low (eTable 2 in the Supplement).
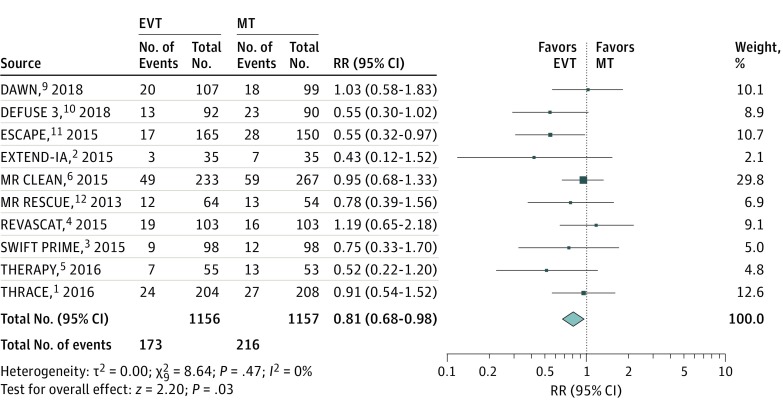
In the cumulative meta-analysis, EVT significantly reduced the risk for 90-day mortality by 3.7% compared with medical therapy (15.0% vs 18.7%; RR, 0.81; 95% CI, 0.68-0.98; P = .03; Figure 1), with a number needed to treat of 27 to prevent 1 death from all causes. Trends were similar when analyzing early-window EVT vs IT (all trials except DAWN [DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention With Trevo]9 and DEFUSE 3 [Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke]10: RR, 0.83; 95% CI, 0.67-1.01; P = .06) or late-window trials separately (DAWN9 and DEFUSE 310: RR, 0.76; 95% CI, 0.41-1.40; P = .38).
Figure 1. All-Cause Mortality in Randomized Clinical Trials of Endovascular Thrombectomy (EVT) vs Medical Therapy (MT) at 90 Days.
Individual and summary risk ratios (RRs) with 95% CIs for all-cause mortality in randomized clinical trials of EVT vs MT at 90 days of follow-up. The size of the data markers indicates the study weight within the pooled meta-analysis. Detailed study weights are given in the respective column and correspond to the size of the data markers. Study weights were calculated according to the random-effects Cochran-Mantel-Haenszel model used. DAWN indicates DWI or CTP Assessment With Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention With Trevo; DEFUSE 3, Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke; ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing CT to Recanalization Times; EXTEND-IA, Extending the Time for Thrombolysis in Emergency Neurological Deficits—Intra-Arterial; MR CLEAN, Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands; MR RESCUE, Mechanical Retrieval and Recanalization of Stroke Clots Using Embolectomy; REVASCAT, Randomized Trial of Revascularization With Solitaire FR Device vs Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting Within Eight Hours of Symptom Onset; SWIFT PRIME, Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment; THERAPY, The Randomized, Concurrent Controlled Trial to Assess the Penumbra System’s Safety and Effectiveness in the Treatment of Acute Stroke; and THRACE, Mechanical Thrombectomy After Intravenous Alteplase vs Alteplase Alone After Stroke.
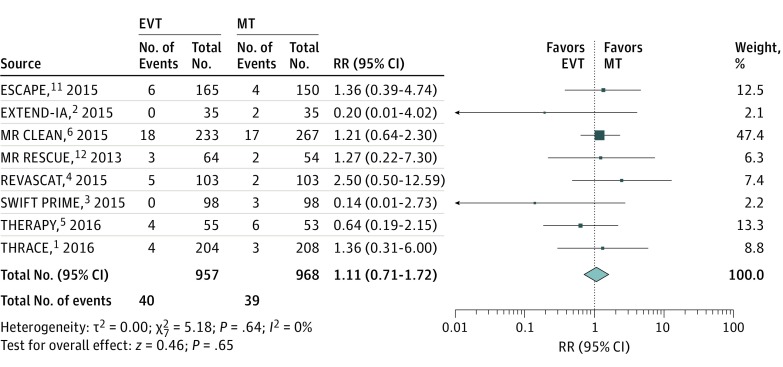
In early-window EVT trials, nearly all patients received EVT in addition to IT (Table),1,2,3,4,5,6,9,10,11,12 with a potential risk for symptomatic intracranial hemorrhage to confound mortality. The meta-analysis of intracranial hemorrhage events, however, showed no differences between EVT and medical therapy (4.2% vs 4.0%; RR, 1.11; 95% CI, 0.71-1.72; P = .65) (Figure 2). Thus, the observed risk reduction for mortality probably does not originate from differences in adverse effects but from the functional benefits of EVT also translating to improved 90-day survival.
Figure 2. Symptomatic Intracranial Hemorrhage in Randomized Clinical Trials of Early-Window Endovascular Thrombectomy (EVT) vs Medical Therapy (MT) at 90 Days.
Individual and summary risk ratios (RRs) with 95% CIs for symptomatic intracranial hemorrhage in randomized clinical trials of early-window EVT vs MT. The size of the data markers indicates the study weight within the pooled meta-analysis. Detailed study weights are given in the respective column and correspond to the size of the data markers. Study weights were calculated according to the random-effects Cochran-Mantel-Haenszel model used. ESCAPE, Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion With Emphasis on Minimizing CT to Recanalization Times; EXTEND-IA, Extending the Time for Thrombolysis in Emergency Neurological Deficits—Intra-Arterial; MR CLEAN, Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands; MR RESCUE, Mechanical Retrieval and Recanalization of Stroke Clots Using Embolectomy; REVASCAT, Randomized Trial of Revascularization With Solitaire FR Device vs Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting Within Eight Hours of Symptom Onset; SWIFT PRIME, Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment; THERAPY, The Randomized, Concurrent Controlled Trial to Assess the Penumbra System’s Safety and Effectiveness in the Treatment of Acute Stroke; and THRACE, Mechanical Thrombectomy After Intravenous Alteplase vs Alteplase Alone After Stroke.
Discussion
Previous works also observed mortality benefits between groups in favor of EVT; however, the differences were statistically insignificant (eg, 3.6%13 and 2.6%,14 with P values of approximately .15), similar to the present sensitivity analysis in early-window trials only. However, by including all trials of EVT methods, this meta-analysis features the largest number of analyzed patients and events, to our knowledge, and achieves sufficient power to reach statistical significance.
Limitations
Limitations include trial heterogeneity in study protocols (early-window and late-window) and EVT (eg, different modalities and generations of thrombectomy devices). Risk of bias additionally originates from analysis of secondary trial end points and incomplete recruitment in the prematurely terminated trials. Therefore, results must be interpreted with considerable caution. However, new EVT trials designed to show mortality differences in AIS might never be performed; thus, a meta-analysis of available data may be the only way to analyze short-term survival. Low statistical heterogeneity (I2 and τ2 in Figure 1 and Figure 2) additionally indicates robust effects. Long-term follow-ups of singular RCTs will be interesting with respect to mortality: the 2-year MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) study data have already shown a trend toward improved survival during the first 90 days after AIS with EVT.15
Conclusions
Taken together, there is considerable evidence in guideline-referenced RCTs that EVT significantly benefits survival during the first 90 days after AIS compared with medical therapy alone. We cannot help but see the parallels: endovascular strategies may well turn out to be as successful in AIS as in myocardial infarction.
eTable 1. Study Characteristics of Excluded Trials
eTable 2. Risk of Bias of Included Studies
References
- 1.Bracard S, Ducrocq X, Mas JL, et al. ; THRACE Investigators . Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016;15(11):1138-1147. doi: 10.1016/S1474-4422(16)30177-6 [DOI] [PubMed] [Google Scholar]
- 2.Campbell BC, Mitchell PJ, Kleinig TJ, et al. ; EXTEND-IA Investigators . Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009-1018. doi: 10.1056/NEJMoa1414792 [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, Bonafe A, et al. ; SWIFT PRIME Investigators . Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke. N Engl J Med. 2015;372(24):2285-2295. doi: 10.1056/NEJMoa1415061 [DOI] [PubMed] [Google Scholar]
- 4.Jovin TG, Chamorro A, Cobo E, et al. ; REVASCAT Trial Investigators . Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296-2306. doi: 10.1056/NEJMoa1503780 [DOI] [PubMed] [Google Scholar]
- 5.Mocco J, Zaidat OO, von Kummer R, et al. ; THERAPY Trial Investigators . Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke. 2016;47(9):2331-2338. doi: 10.1161/STROKEAHA.116.013372 [DOI] [PubMed] [Google Scholar]
- 6.Berkhemer OA, Fransen PS, Beumer D, et al. ; MR CLEAN Investigators . A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11-20. doi: 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 7.Powers WJ, Rabinstein AA, Ackerson T, et al. ; American Heart Association Stroke Council . 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110. doi: 10.1161/STR.0000000000000158 [DOI] [PubMed] [Google Scholar]
- 8.Ibanez B, James S, Agewall S, et al. ; ESC Scientific Document Group . 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the Management of Acute Myocardial Infarction in Patients Presenting With ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 9.Nogueira RG, Jadhav AP, Haussen DC, et al. ; DAWN Trial Investigators . Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11-21. doi: 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 10.Albers GW, Marks MP, Kemp S, et al. ; DEFUSE 3 Investigators . Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718. doi: 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goyal M, Demchuk AM, Menon BK, et al. ; ESCAPE Trial Investigators . Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030. doi: 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 12.Kidwell CS, Jahan R, Gornbein J, et al. ; MR RESCUE Investigators . A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914-923. doi: 10.1056/NEJMoa1212793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goyal M, Menon BK, van Zwam WH, et al. ; HERMES Collaborators . Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723-1731. doi: 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 14.Román LS, Menon BK, Blasco J, et al. ; HERMES Collaborators . Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol. 2018;17(10):895-904. doi: 10.1016/S1474-4422(18)30242-4 [DOI] [PubMed] [Google Scholar]
- 15.van den Berg LA, Dijkgraaf MG, Berkhemer OA, et al. ; MR CLEAN Investigators . Two-year outcome after endovascular treatment for acute ischemic stroke. N Engl J Med. 2017;376(14):1341-1349. doi: 10.1056/NEJMoa1612136 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Study Characteristics of Excluded Trials
eTable 2. Risk of Bias of Included Studies