Abstract
Thoracic spinal stenosis is a relatively common disorder causing paraplegia in the population of China. Until nowadays, the clinical management of thoracic spinal stenosis is still demanding and challenging with lots of questions remaining to be answered. A clinical guideline for the treatment of symptomatic thoracic spinal stenosis has been created by reaching the consensus of Chinese specialists using the best available evidence as a tool to aid practitioners involved with the care of this disease. In this guideline, many fundamental questions about thoracic spinal stenosis which were controversial have been explained clearly, including the definition of thoracic spinal stenosis, the standard procedure for diagnosing symptomatic thoracic spinal stenosis, indications for surgery, and so on. According to the consensus on the definition of thoracic spinal stenosis, the soft herniation of thoracic discs has been excluded from the pathological factors causing thoracic spinal stenosis. The procedure for diagnosing thoracic spinal stenosis has been quite mature, while the principles for selecting operative procedures remain to be improved. This guideline will be updated on a timely schedule and adhering to its recommendations should not be mandatory because it does not have the force of law.
Keywords: Thoracic spinal stenosis, Diagnosis, Treatment
Introduction
This clinical guideline for symptomatic thoracic spinal stenosis has been developed by ninety‐seven spinal surgery specialists from mainland China and is for spinal surgeons to consult with the aim of standardizing their diagnostic and therapeutic procedures and improving the clinical outcomes of patients with symptomatic thoracic spinal stenosis. A project team from Peking University Third Hospital was responsible for the drafting this guideline, this team being financially supported by a grant from the Science and Technology Commission of Beijing. This guideline will be updated in future to incorporate progress in fundamental research and clinical practices. Because this guideline does not have the force of law, adhering to its recommendations is not mandatory. Should litigation occur, this guideline cannot be used as a legal justification of treatment choices.
Definition and Characteristics of Thoracic Spinal Stenosis
Definition
Symptomatic thoracic spinal stenosis (TSS) is here defined as a reduction in the capacity of the thoracic spinal canal with associated compression of the spinal cord and (or) nerve roots giving rise to a variety of clinical symptoms, the reduction in capacity being caused by one or more pathological factors, including ossification of ligaments in the spinal canal, hard disc herniation, posterior vertebral osteophytes and developmental spinal stenosis1, 2.
Pathological Factors Causing Thoracic Spinal Stenosis
Many pathological factors may result in reduction in the capacity of the thoracic spinal canal and consequent compressing of the spinal cord or nerve roots, including ossification of the thoracic ligamentum flavum (OLF) and thoracic longitudinal ligament (OPLL), thoracic disc herniation with ossification of the annulus fibrosus, osteophytes of the posterior edges of vertebral bodies and hyperplasia of the facet joints.
The definition of TSS does not include myelopathy secondary to calcification of thoracic discs, thoracic soft disc herniation, thoracic carcinoma (primary or metastatic), thoracic active tuberculosis, thoracic fracture or dislocation or thoracic scoliosis or kyphosis.
Segments Involved in Thoracic Spinal Stenosis
The segment range is from the T1 vertebral body to the T12–L1 intervertebral disc.
Standard Name for Thoracic Spinal Stenosis
Because many pathological factors may lead to TSS and two or more of those factors commonly coexist, we suggest using the term “Symptomatic TSS” to name the main diagnosis and listing the responsible pathological factors as subsidiary diagnoses. For example: Thoracic Spinal Stenosis (T8–11 OLF, T9–10 OPLL).
Standardized Diagnosis of Thoracic Spinal Stenosis
Symptomatic TSS can only be diagnosed when the patient has at least one of the symptoms or signs listed below under the heading of “Symptoms” and radiological images show that the thoracic spinal canal is stenotic and the spinal cord compressed. Additionally, the clinical and radiological findings must match. A patient with only abnormal radiological findings and no symptoms or signs cannot be diagnosed as having symptomatic TSS3, 4, 5, 6.
Symptoms
One or both legs may be heavy, weak, and stiff, impairing balance when walking.
Extensive numbness and (or) pain in one or both legs.
Spinal cord‐related claudication.
Difficulty in urination and defecation or sexual dysfunction.
Zonesthesia on the chest or abdomen.
Radiculopathy in the chest or abdomen.
Signs
Signs indicating upper motor neuron disorder such as hypermyotonia in the legs and positive Babinski or Chaddock signs.
Signs indicating mixed upper and lower motor neuron disorder such as patellar tendon hyperreflexia combined with Achilles tendon hyporeflexia. This type of sign is usually found in spinal stenosis of the thoracolumbar region.
Signs indicating extensive lower motor neuron disorder that cannot completely be explained by lumbar spinal disease.
Radiological Imaging
Plain X‐Ray Films
Plain X‐ray films can show the characteristic features of diffuse idiopathic skeletal hyperostosis, OPLL, posterior vertebral osteophytes, OLF, skeletal fluorosis and typical or atypical Scheuermann disease. However, they may show no abnormalities. Plain films can also help to decide whether there are anatomical variants such as transitional vertebrae that make it essential to confirm the level precisely intraoperatively.
MRI
Magnetic resonance imaging can show OLF, OPLL, posterior vertebral osteophytes and posterior marginal cartilaginous nodes as well as deformation of the spinal cord caused by compression and signal changes within the spinal cord.
CT
Computed tomography can show OLF, OPLL, posterior vertebral osteophytes, thoracic disc herniation combined with ossification of the annulus fibrosus, posterior marginal cartilaginous node, and so on.
Procedure for Diagnosing Symptomatic Thoracic Spinal Stenosis
Confirmation of Suspected Cases
When patient exhibits one or more of the following phenomena, TSS should be suspected and checked for further.
One or both legs heavy, weak, and stiff impairing balance when walking.
Bilateral or unilateral legs perform spinal cord related claudication.
Extensive numbness and (or) pain in one or both legs.
Physical examination shows signs indicating upper motor neuron disorder in the legs with no abnormalities in the arms.
Physical examination shows signs indicating mixed upper and lower motor neuron disorder or extensive lower motor neuron disorder.
A diagnosis of cervical spondylotic myelopathy (CSM) has been confirmed in the presence of severe lower extremity and mild upper extremity symptoms.
A diagnosis of diffuse idiopathic skeletal hyperostosis, skeletal fluorosis, ankylosing spondylitis or continuous type of OPLL has been confirmed.
Previous cervical surgery for CSM after which upper limb symptoms improved dramatically whereas lower limb symptoms did not improve or even became worse.
Zonesthesia or radiculopathy on the chest or abdomen.
Further Assessment of Suspected Cases
Patients suspected of having TSS should be checked as follows (Fig. 1).
Figure 1.
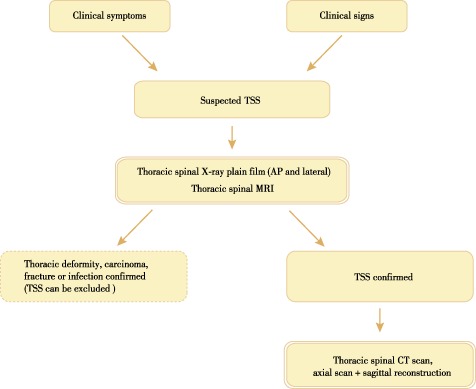
Diagnostic algorithm for suspected TSS.
Step One: Thoracic Spinal X‐Ray Plain Film (AP and Lateral), MRI (Sagittal and Axial, T1WI and T2WI)
If there are no abnormalities in plain films and MR images, TSS can be excluded. TSS can also be excluded if thoracic deformity, carcinoma, fracture, tuberculosis or pyogenic infection is confirmed and OLF or OPLL excluded. TSS is confirmed if MR images show OLF, OPLL, thoracic disc herniation with ossification of the annulus fibrosus, osteophytes of the posterior edges of vertebral bodies or hyperplasia of the facet joints. MR imaging is helpful for determining the radiological type of OLF or OPLL (solitary, continuous or saltatory type), the encroaching ratio in each segment, the degree of compression of the spinal cord and signals within the spinal cord.
Step Two: Thoracic Spinal CT Scan
In patients with solitary thoracic OLF or OPLL or disc herniation, a CT scan of the involved segment is recommended, whereas in those with the continuous or saltatory type of OLF or OPLL, a CT scan of the whole thoracic spine, including an axial scan and sagittal reconstruction, is recommended.
A CT scan's bony window can clarify whether there is ossification of the annulus fibrosus or posterior marginal cartilaginous node and also show the form, size and inner characteristics of areas of ossification and degree of compression of the dural sac and spinal cord.
Step Three: Comprehensive Analysis of Clinical Symptoms, Signs and Radiological Findings
Comprehensive analysis is required to confirm the diagnosis, including the qualitative diagnosis and responsible segment.
Step Four: Performing Other Related Tests
In about 30%–40% of cases, TSS is combined with CSM. Hence, the upper limbs should be examined and cervical spinal X‐ray and MRI performed if necessary6, 7, 8. Similarly, in about 10%–15% of cases TSS is combined with lumbar spinal stenosis; lumbar spinal X‐ray and MRI should be performed when there is radiculopathy in the legs and lumbar spinal stenosis is suspected4, 7, 8, 9.
Cervical or lumbar spinal plain films, including AP and lateral views, should be performed in patients with upper or lower TSS to assist in identifying any transitional vertebrae and confirming the precise level intraoperatively.
In patients whose clinical features do not conform with the radiological findings or those suspected of having motor neuron diseases, an electromyogram should be performed.
Treatment of Symptomatic Thoracic Spinal Stenosis
Non‐Surgical Treatment
The overwhelming majority of clinical studies show that non‐surgical treatment is not effective in patients with TSS and that decompressing surgery is the only effective treatment approach8, 9, 10, 11, 12, 13, 14, 15, 16, 17. In patients with chest or abdominal wall radiculopathy or mild myelopathy, short‐term conservative treatment is acceptable provided close follow‐up is provided. Appropriate forms of conservative treatment include medication (non‐steroidal anti‐inflammatory drugs, neurotrophic medicines) and physical therapy.
Indications for Surgery in Patients with Thoracic Spinal Stenosis
Patients with serious symptoms of thoracic myelopathy should be treated surgically as soon as the diagnosis has been established.
Patients with mild symptoms of thoracic myelopathy can be treated conservatively with close follow‐up. If progressive deterioration in symptoms occurs, surgery should promptly be undertaken.
The target surgical region or segment in which compression is occurring should be identified by comprehensive analysis of the clinical symptoms, signs and radiological features.
Intra‐operative Monitoring of Electrophysiology
Continuous intra‐operative monitoring of both motor and sensory evoked potentials is recommended to facilitate timely recognition of intra‐operative spinal cord injury.
Principles for Selecting Operative Procedures
TSS secondary to OLF: posterior en bloc or segmental laminectomy or floating decompression is recommended. A high speed drill should be used. Internal fixation and fusion can be performed in patients with thoracolumbar regional stenosis and those who have undergone multiple segmental laminectomy7, 8, 9, 10, 12, 13, 14, 18, 19.
TSS secondary to disc related factors (hard disc herniation, posterior vertebral hyperplasia, posterior marginal cartilaginous node): both anterolateral approach and posterior transforaminal approach discectomy and fusion can be appropriate20, 21, 22, 23, 24.
TSS secondary to OPLL: the procedure should be chosen according to the location and form of the area of ossification and the degree of compression of the spinal cord25, 26, 27, 28, 29, 30, 31, 32. For solitary OPLL in the middle or lower thoracic spine, both anterolateral and posterior transforaminal resection of the OPLL with fixation and fusion is appropriate. For short regional OPLL (two to three segments), a posterior approach circumferential decompression and fusion is appropriate; sometimes posterior laminectomy alone can achieve sufficient decompression of the spinal cord. The optimal operative procedure for long regional OPLL (more than three segments) depends on the form of OPLL. When the area of ossification is flat, posterior laminectomy with decompression of one more segment cranially and caudally is recommended, whereas when it is raised, posterior laminectomy and selective circumferential decompression is recommended. Primary posterior laminectomy and secondary anterolateral resection of the OPLL and fusion is also appropriate.
TSS secondary to OLF combined with OPLL or hard disc herniation: the surgical procedure should be selected according to the specific characteristics of the condition21, 25, 28, 33, 34: If anterior compression is mild, posterior laminectomy is recommended, whereas if posterior compression is mild, both anterolateral decompression with fusion and posterior transforaminal circumferential decompression with fusion are appropriate. If both anterior and the posterior compression are severe, posterior circumferential decompression on combined posterior and anterior approaches can be performed.
Surgical Strategy for TSS Combined with CSM or Lumbar Spinal Stenosis
TSS combined with CSM: the clinical symptoms, signs and radiological findings must be comprehensively assessed, the symptoms being the major guide. And it is recommended to decide and treat the primary responsible lesion7, 8, 9, 35. If the symptoms are mild in the upper limbs and severe in the lower limbs, prior thoracic decompression is recommended, especially when the signals within the cervical spinal cord are normal on MRI. If the symptoms are severe in all four limbs, or the cervical spinal cord is markedly compressed with abnormal inner signals on MRI, prior cervical decompression surgery is recommended. Thoracic decompression may be needed if the symptoms in the lower limbs have not improved significantly by 3 months follow‐up. In patients with upper thoracic OLF combined with cervical multi‐segmental OPLL, one‐ or two‐stage posterior cervical laminoplasty and posterior thoracic laminectomy is recommended.
TSS combined with lumbar spinal stenosis or lumbar disc herniation: the clinical symptoms should be considered the major guide to identifying the primary responsible lesion and selecting a treatment approach. When both pathologies are relatively severe, the principle is to decompress the thoracic spinal cord first7, 8, 9, 36.
Criteria for Evaluating the Surgical Outcome of TSS
Clinical Evaluation
Changes in spinal cord function should be assessed by calculating Japanese Orthopaedic Association thoracic spinal cord (full score = 11)13 or Chinese Orthopaedic Association thoracic spinal cord scores (full score = 22)37.
Changes in pain should be assessed with VAS scores (0–10).
Changes in social and psychological state should be assessed with the SF‐36)38.
Changes in coexisting cervical or lumbar disorders should be assessed by calculating the Japanese Orthopaedic Association cervical spinal cord scores (full score = 17) and the Oswestry disability index.
Radiological Evaluation
Decompression of the spinal cord: assessment of completeness of resection of the compressive lesion and the appearance of the spinal cord and dural sac.
Changes in curvature of the thoracic and whole spine: identification and assessment of postoperative deterioration in thoracic kyphotic angle (iatrogenic kyphosis), improvement in preoperative kyphotic deformity and the sagittal and coronary balance of the trunk.
Location of the implants: assessment as to whether the locations of the screws and cages meet the requirements for mechanical stability.
Results of fusion: assessment as to whether bony fusion has been achieved by the 6 month follow‐up.
List of Names of Consultant Specialists
Bo‐hua Chen, Qi‐xin Chen, Zhong‐qiang Chen, Yong‐long Chi, Geng‐ting Dang, Shu‐cai Deng, Hui‐qiang Ding, Jian Dong, Shi‐qing Feng, Zhao‐qing Guo, Yong Hai, Ding‐jun Hao, Yi Hong, Tie‐sheng Hou, Xiao‐kui Hou, Shu‐xun Hou, Jian‐zhong Hu, You‐gu Hu, Dong‐sheng Huang, Huang‐yuan Huang, Hong‐jun Huo, Quan Ji, Jian‐yuan Jiang, Da‐di Jin, Wei Lei, Chun‐de Li, Fang Li, Feng Li, Fo‐bao Li, Ming Li, Wei‐shi Li, Zhong‐shi Li, Jian‐hua Lin, Bin Liu, Bo Liu, Hai‐ying Liu, Shang‐li Liu, Shao‐yu Liu, Xiao‐guang Liu, Yi Liu, Zhong‐jun Liu, Zhuo‐jing Luo, Guo‐hua Lv, Hua‐song Ma, Xue‐xiao Ma, Xun Ma, Yuan‐zheng Ma, Qiang Qi, Gui‐xing Qiu, Yong Qiu, Di‐ke Ruan, Wen‐dong Ruan, Hui‐yong Shen, Jian‐xiong Shen, Wei‐bin Sheng, Jian‐gang Shi, Jun Shu, Jie‐fu Song, Jin‐hui Song, Yue‐ming Song, Chang‐tai Sun, Chui‐guo Sun, Tian‐sheng Sun, Huan Wang, Pei Wang, Yan Wang, Yi‐peng Wang, Yi‐sheng Wang, Zhe Wang, Zi‐li Wang, Ji Wu, Feng‐liang Wu, Wen‐wen Wu, Qun Xia, Song‐hua Xiao, Zeng‐ming Xiao, Jian‐zhong Xu, Lin Xu, Yuan Xue, Ming Yan, Hui‐lin Yang, Qun Yang, You‐geng Yang, Qing‐shui Yin, Hai‐feng Yuan, Wen Yuan, Lei Zang, Yan Zeng, Yong‐gang Zhang, Zhi‐cheng Zhang, Jie Zhao, Yu Zhao, Yan‐ping Zheng, Yue Zhou, Yue Zhu, Qing‐san Zhu, De‐wei Zou.
Disclosure: This work was supported by the Science and Technology Commission Project Fund of Beijing (D101100049910007).
Contributor Information
the Spine Surgery Group of Chinese Orthopedic Association:
Bo‐hua Chen, Qi‐xin Chen, Zhong‐qiang Chen, Yong‐long Chi, Geng‐ting Dang, Shu‐cai Deng, Hui‐qiang Ding, Jian Dong, Shi‐qing Feng, Zhao‐qing Guo, Yong Hai, Ding‐jun Hao, Yi Hong, Tie‐sheng Hou, Xiao‐kui Hou, Shu‐xun Hou, Jian‐zhong Hu, You‐gu Hu, Dong‐sheng Huang, Huang‐yuan Huang, Hong‐jun Huo, Quan Ji, Jian‐yuan Jiang, Da‐di Jin, Wei Lei, Chun‐de Li, Fang Li, Feng Li, Fo‐bao Li, Ming Li, Wei‐shi Li, Zhong‐shi Li, Jian‐hua Lin, Bin Liu, Bo Liu, Hai‐ying Liu, Shang‐li Liu, Shao‐yu Liu, Xiao‐guang Liu, Yi Liu, Zhong‐jun Liu, Zhuo‐jing Luo, Guo‐hua Lv, Hua‐song Ma, Xue‐xiao Ma, Xun Ma, Yuan‐zheng Ma, Qiang Qi, Gui‐xing Qiu, Yong Qiu, Di‐ke Ruan, Wen‐dong Ruan, Hui‐yong Shen, Jian‐xiong Shen, Wei‐bin Sheng, Jian‐gang Shi, Jun Shu, Jie‐fu Song, Jin‐hui Song, Yue‐ming Song, Chang‐tai Sun, Chui‐guo Sun, Tian‐sheng Sun, Huan Wang, Pei Wang, Yan Wang, Yi‐peng Wang, Yi‐sheng Wang, Zhe Wang, Zi‐li Wang, Ji Wu, Feng‐liang Wu, Wen‐wen Wu, Qun Xia, Song‐hua Xiao, Zeng‐ming Xiao, Jian‐zhong Xu, Lin Xu, Yuan Xue, Ming Yan, Hui‐lin Yang, Qun Yang, You‐geng Yang, Qing‐shui Yin, Hai‐feng Yuan, Wen Yuan, Lei Zang, Yan Zeng, Yong‐gang Zhang, Zhi‐cheng Zhang, Jie Zhao, Yu Zhao, Yan‐ping Zheng, Yue Zhou, Yue Zhu, Qing‐san Zhu, and De‐wei Zou
References
- 1. Chen ZQ. Summary of the Chinese symposium on thoracic spinal stenosis in 2006. Zhonghua Gu Ke Za Zhi, 2007, 27: 39–42 (in Chinese). [Google Scholar]
- 2. Chen ZQ, Dang GT, Hu YC, Sun CG. Summary of the second Chinese symposium on thoracic spinal stenosis. Zhonghua Gu Ke Za Zhi, 2010, 30: 1021–1024 (in Chinese). [Google Scholar]
- 3. Zhou F, Dang GT. Diagnosis of cervical ossification of the posterior longitudinal ligament combined with thoracic ossification of the ligamentum flavum. Zhonghua Gu Ke Za Zhi, 1995, 15: 575–577 (in Chinese). [Google Scholar]
- 4. Liu XG, Cai QL, Dang GT, et al An analysis of misdiagnosis and reoperation for thoracic spinal stenosis. Zhongguo Ji Zhu Ji Sui Za Zhi, 2000, 10: 336–338 (in Chinese). [Google Scholar]
- 5. Liu N, Chen ZQ, Qi Q, Guo ZQ. Correlation between spinal canal encroachment and neurologic deficits in thoracic ossification of the ligamentum flavum. Zhonghua Gu Ke Za Zhi, 2007, 27: 481–484 (in Chinese). [Google Scholar]
- 6. Sun CG, Chen ZQ. The clinical diagnosis of thoracic ossification of the ligamentum flavum combined with cervical spondylotic myelopathy. Jizhu Wai Ke Za Zhi, 2007, 5: 18–21 (in Chinese). [Google Scholar]
- 7. Chen ZQ, Dang GT, Liu XG, et al The surgical procedure for thoracic ossification of the ligamentum flavum. Zhonghua Gu Ke Za Zhi, 1999, 19: 197–200 (in Chinese). [Google Scholar]
- 8. Chen ZQ, Sun CG, Dang GT, et al The surgical outcome of thoracic myelopathy caused by ossification of the ligamentum flavum. Zhongguo Ji Zhu Ji Sui Za Zhi, 2006, 16: 485–488 (in Chinese). [Google Scholar]
- 9. Sun CG, Chen ZQ, Liu ZJ, et al Long term outcome after decompressive surgery for thoracic myelopathy caused by ossification of the ligamentum flavum. Zhonghua Wai Ke Za Zhi, 2012, 50: 426–429 (in Chinese). [PubMed] [Google Scholar]
- 10. Zhou J, Chen N, Dong J, et al The surgical outcome and factors influencing it for thoracic ossification of the ligamentum flavum. Fudan Xue Bao Yi Xue Ban, 2010, 37: 379–383. [Google Scholar]
- 11. Kuh SU, Kim YS, Cho YE, et al Contributing factors affecting the prognosis surgical outcome for thoracic OLF. Eur Spine J, 2006, 15: 485–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Park BC, Min WK, Oh CW, et al Surgical outcome of thoracic myelopathy secondary to ossification of ligamentum flavum. Joint Bone Spine, 2007, 74: 600–605. [DOI] [PubMed] [Google Scholar]
- 13. Hirabayashi H, Ebara S, Takahashi J, et al Surgery for thoracic myelopathy caused by ossification of the ligamentum flavum. Surg Neurol, 2008, 69: 114–116, discussion 116. [DOI] [PubMed] [Google Scholar]
- 14. Chen XQ, Yang HL, Wang GL, et al Surgery for thoracic myelopathy caused by ossification of the ligamentum flavum. J Clin Neurosci, 2009, 16: 1316–1320. [DOI] [PubMed] [Google Scholar]
- 15. Hur H, Lee JK, Lee JH, Kim JH, Kim SH. Thoracic myelopathy caused by ossification of the ligamentum flavum. J Korean Neurosurg Soc, 2009, 46: 189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ando K, Imagama S, Ito Z, et al Predictive factors for a poor surgical outcome with thoracic ossification of the ligamentum flavum by multivariate analysis: A multicenter study. Spine (Phila Pa 1976), 2013, 38: E748–E754. [DOI] [PubMed] [Google Scholar]
- 17. Gao R, Yuan W, Yang L, Shi G, Jia L. Clinical features and surgical outcomes of patients with thoracic myelopathy caused by multilevel ossification of the ligamentum flavum. Spine J, 2013, 13: 1032–1038. [DOI] [PubMed] [Google Scholar]
- 18. Xue Y, Wang P, Ma XL, et al Laminar shelling decompression for treatment of thoraicic ossification of ligamentum flavum with spondylotic myelopathy. Zhonghua Gu Ke Za Zhi, 2006, 26: 161–164 (in Chinese). [Google Scholar]
- 19. Jia LS, Chen XS, Zhou SY, Shao J, Zhu W. En bloc resection of lamina and ossified ligamentum flavum in the treatment of thoracic ossification of the ligamentum flavum. Neurosurgery, 2010, 66: 1181–1186. [DOI] [PubMed] [Google Scholar]
- 20. Wu XD, Chen HJ, Yuan W, et al Giant calcified thoracic disc herniation in a child: A case report and review of the literature. J Bone Joint Surg Am, 2010, 92: 1992–1996. [DOI] [PubMed] [Google Scholar]
- 21. Qi Q, Chen ZQ, Liu N, et al Circumspinal decompression through a single posterior incision to treat thoracolumbar disc herniation. Chin Med J (Engl), 2011, 124: 3852–3857. [PubMed] [Google Scholar]
- 22. Liu N, Chen Z, Qi Q, Li W, Guo Z. Circumspinal decompression and fusion through a posterior midline incision to treat central calcified thoracolumbar disc herniation: A minimal 2‐year follow‐up study with reconstruction CT. Eur Spine J, 2014, 23: 373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ding WY, Li BJ, Shen Y, et al The treatment of thoracic disc herniation via posterolateral approach. Zhonghua Gu Ke Za Zhi, 2006, 26: 39–42 (in Chinese). [Google Scholar]
- 24. Qi Q, Chen ZQ, Du JZ, et al Surgical treatment of the thoracic and thoracolumbar disc herniation through a posterior far lateral approach. Zhonghua Gu Ke Za Zhi, 2010, 30: 1063–1067 (in Chinese). [Google Scholar]
- 25. Liu XG, Liu ZJ, Chen ZQ, et al Cave‐in technique 360 degree circumferential decompression for thoracic spinal stenosis with ossification of the posterior longitudinal ligament. Zhonghua Gu Ke Za Zhi, 2010, 30: 1059–1062 (in Chinese). [Google Scholar]
- 26. Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: An update on its biology, epidemiology, and natural history. Neurosurgery, 2006, 58: 1027–1039, discussion 1027–1039. [DOI] [PubMed] [Google Scholar]
- 27. Tokuhashi Y, Matsuzaki H, Oda H, Uei H. Effectiveness of posterior decompression for patients with ossification of the posterior longitudinal ligament in the thoracic spine. Spine (Phila Pa 1976), 2006, 31: E26–E30. [DOI] [PubMed] [Google Scholar]
- 28. Li WS, Chen ZQ, Zeng Y, et al The clinical features and therapeutic strategy for thoracic ossification of the posterior longitudinal ligament. Zhonghua Gu Ke Za Zhi, 2007, 27: 15–18 (in Chinese). [Google Scholar]
- 29. Hioki A, Miyamoto K, Hosoe H, Shimizu K. Two‐staged decompression for thoracic paraparesis due to the combined ossification of the posterior longitudinal ligament and the ligamentum flavum: A case report. Arch Orthop Trauma Surg, 2008, 128: 175–177. [DOI] [PubMed] [Google Scholar]
- 30. Kawahara N, Tomita K, Murakami H, et al Circumspinal decompression with dekyphosis stabilization for thoracic myelopathy due to ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976), 2008, 33: 39–46. [DOI] [PubMed] [Google Scholar]
- 31. Min JH, Jang JS, Lee SH. Clinical results of ossification of the posterior longitudinal ligament of the thoracic spine treated by anterior decompression. J Spinal Disord Tech, 2008, 21: 116–119. [DOI] [PubMed] [Google Scholar]
- 32. Yamazaki M, Okawa A, Fujiyoshi T, Furuya T, Koda M. Posterior decompression with instrumented fusion for thoracic myelopathy caused by ossification of the posterior longitudinal ligament. Eur Spine J, 2010, 19: 691–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Palumbo MA, Hilibrand AS, Hart RA, et al Surgical treatment of thoracic spinal stenosis. Spine (Phila Pa 1976), 2001, 26: 558–566. [DOI] [PubMed] [Google Scholar]
- 34. Aizawa T, Sato T, Sasaki H, et al Results of surgical treatment for thoracic myelopathy: Minimum 2‐year follow‐up study in 132 patients. J Neurosurg Spine, 2007, 7: 13–20. [DOI] [PubMed] [Google Scholar]
- 35. Sun CG, Chen ZQ, Liu XG. Selection of surgical procedures for thoracic ossification of the ligamentum flavum combined with cervical spondylotic myelopathy. Zhonghua Gu Ke Za Zhi, 2010, 30: 1087–1090 (in Chinese). [Google Scholar]
- 36. Matsumoto Y, Harimaya K, Doi T, et al Clinical characteristics and surgical outcome of the symptomatic ossification of ligamentum flavum at the thoracic level with combined lumbar spinal stenosis. Arch Orthop Trauma Surg, 2012, 132: 465–470. [DOI] [PubMed] [Google Scholar]
- 37. Wang LS, Dang GT, Liu ZJ, et al A discussion of the grading of cervical spinal cord injury. Zhongguo Ji Zhu Ji Sui Za Zhi, 1991, 1: 52–54 (in Chinese). [Google Scholar]
- 38. Jr Ware JE, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Med Care, 1992, 30: 473–483. [PubMed] [Google Scholar]


