Abstract
We report the case of a 75‐year‐old lady who presented with a L 2‐3 non‐union 18 months following a L 2‐3 and L 3‐4 posterior decompression and transforaminal lumbar interbody fusion. Halo of the L 2 pedicle screws on imaging was consistent with a non‐union at the L 2‐3 level. An anterior lumbar interbody fusion (ALIF) approach was originally considered. However, due to the high lumbar approach and patient habitus [body mass index (BMI) > 35], a decision was made to approach the L 2‐3 level using an oblique technique. This involved dissection anterior to the psoas muscle to access the L 2‐3 disc space. The psoas, kidney and retroperitoneum were retracted using a Synframe for the oblique trajectory. Removal of the prior trans‐foraminal lumbar interbody fusion cage was performed via the oblique approach and insertion of a revised implant. The operation was completed successfully with no perioperative complications noted. Length of stay was 3 days, with the patient achieving rapid pain relief. In the present report, we report the first case using an oblique lumbar interbody fusion (OLIF) approach for revision of a prior posterior fusion non‐union at the L 2,3 level. The OLIF technique is feasible for revision of a non‐union of upper lumbar levels, with satisfactory fusion achieved with acceptable feasibility.
Keywords: Oblique lumbar interbody fusion, Non‐union, Pseudoarthrosis
Introduction
Lumbar interbody fusion is an efficacious and safe surgical approach in patients with degenerative disc disease, spinal disc herniation, spinal deformity and instability, and discogenic back pain1. Over the past several decades, the surgical techniques for fusion have evolved, with increasingly minimally invasive approaches2, 3. Traditionally, fusion procedures were performed using onlay techniques, posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF). However, with the aim of minimizing spinal and paraspinal muscle dissection, alternative approaches have been developed and used, including anterior lumbar interbody fusion (ALIF) and extreme lateral lumbar interbody fusion (XLIF)4, 5, 6.
Most recently, the oblique trajectory has been adopted in a technique known as oblique lumbar interbody fusion (OLIF)7. While XLIF is not amenable at the L5S1 level due to obstruction by the iliac crests, the OLIF approach uses a retroperitoneal plane to access the disc via a corridor anterior to the iliac crests, and anterior to the psoas muscle (Fig. 1). In contrast to XLIF, no dissection and splitting of the psoas muscle is required, and therefore this theoretically reduces postoperative pain. While the main indication for OLIF as reported in the literature to date is at the L5S1, there have been few reports of using the oblique trajectory for other indications at higher lumbar levels. To the best of our knowledge, this is the first case report of OLIF performed at L2‐3 for non‐union following prior posterior fusion.
Figure 1.
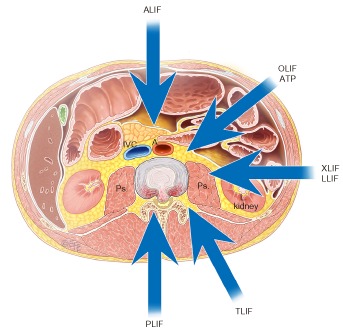
Direction of the oblique lumbar interbody fusion approach (OLIF). ALIF, anterior lumbar interbody fusion; ATP, anterior‐to‐psoas approach; XLIF, extreme lateral interbody fusion; LLIF, lateral lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; PLIF, posterior lumbar interbody fusion.
Case Report
We report a 75‐year‐old woman who presented with a L2‐3 non‐union 18 months following a L2‐3 and L3‐4 posterior decompression and TLIF. The initial surgery was performed for L2‐3 and L3‐4 canal stenosis with spondylolisthesis. Following an initial excellent result with relief of her neurogenic claudication, she developed recurrent back and leg pain 12 months following her initial procedure. Follow‐up imaging demonstrated a solid fusion at L3‐4, but a non‐union at L2‐3 with translation of the TLIF cage posteriorly into the spinal canal (Figs 2,3) . The halo of the L2 pedicle screws on imaging was consistent with a non‐union at the L2‐3 level. An ALIF approach was originally considered. However, due to the high lumbar approach and patient habitus (body mass index > 35), which makes it physically difficult to access the disc space anteriorly, a decision was made to approach the L2‐3 level using an oblique technique. It was considered too difficult to remove the TLIF cage using an extreme lateral approach (XLIF).
Figure 2.
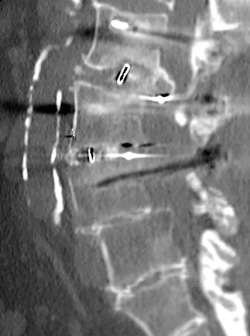
Preoperative computed tomography demonstrating non‐union of L 2‐3 with translation of transforaminal lumbar interbody fusion (TLIF) cage into spinal canal.
Figure 3.
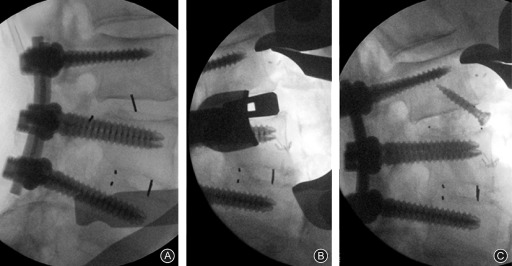
(A) Preoperative X‐ray demonstrating non‐union L 2‐3 with translation of transforaminal lumbar interbody fusion cage into spinal canal. (B) Intraoperative X‐ray with oblique lumbar interbody fusion approach and trial cage. (C) oblique lumbar interbody fusion cage with screw fixation.
The surgical procedure was performed according to the following steps:
Step 1: Following general anesthesia and endotracheal intubation, the patient was positioned lateral, with left side up. Using X‐ray imaging intensification, the level of the OLIF was confirmed prior to incision. The skin was prepared and draped.
Step 2 (approach and exposure): A linear incision and exposure of the lateral aspect of the spine, psoas and vertebral body of L2 and L3 was performed. A standard OLIF technique was used with dissection anterior to the psoas muscle to access the L2‐3 disc space. The psoas was retracted posteriorly with the kidney and retroperitoneum retracted anteriorly using a Synframe retractor system (Synthes, Paoli, PA, USA, Fig. 4).
Figure 4.
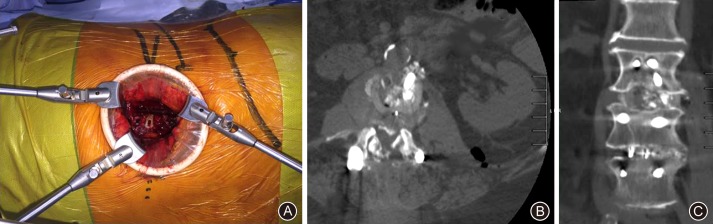
(A) Intraoperative view of the oblique corridor, with the psoas and retroperitoneum retracted using a Synframe. (B) Follow‐up computed tomography (CT) (transverse) of interbody cage. Arrow demonstrates oblique corridor used for revision of non‐union after previous fusion surgery. (C) Follow‐up CT (coronal) demonstrating appropriately positioned new revision cage inserted using an oblique trajectory.
Step 3: The anterior aspect of the psoas muscle and zone between the psoas and vessels was revealed and the level was rechecked to confirm the L2‐3 disc. No intraoperative neuromonitoring was required since the procedure was not trans‐psoas.
Step 4: A discectomy was performed to reach the interbody TLIF cage with obvious non‐union. The cage was removed with a combination of distraction (insert and rotate device) and dissection between the TLIF cage and endplate. A standard endplate preparation was performed prior to the placement of the OLIF cage. The cage was difficult to remove given that it had recessed into the inferior L2 endplate.
Step 5: Following endplate preparation, an 8°, 12 mm height cage was inserted using an oblique trajectory (Signature Spine, Sydney, Australia). The cage was packed with bone morphogenic protein (Infuse, Medtronic, Memphis, TN, USA) and allograft. A single screw was inserted into the L2 vertebral body for the fixation of the cage.
The operation was completed successfully with no perioperative complications noted and a minimal blood loss of 30 mL. At the latest 6‐month follow up the OLIF technique demonstrated satisfactory fusion for revision of a non‐union of upper lumbar levels.
Discussion
Surgical techniques, approaches and indications for lumbar interbody fusion are continually evolving. Recent developments have included the introduction of the true lateral transpsoas approach (LLIF/XLIF) and the oblique trajectory anterior to psoas (OLIF/ATP). XLIF is particularly useful at the upper lumbar levels as an alternative to traditional PLIF and TLIF surgery, which avoids dissection of longitudinal ligaments and paraspinal muscles, while avoiding direct trauma to the abdominal viscera8, 9, 10. However at L5S1, the XLIF technique has limited feasibility given that a direct lateral trajectory would be obstructed by the iliac crests and prevent adequate intervertebral disc exposure7. Furthermore, the lateral approach is made more complicated by the venous system of the iliolumbar vein and tethered common iliac vein, the inadvertent injury of which may cause fatal bleeding10. Dissection or minimally invasive splitting of the psoas muscle may also be associated with postoperative thigh pain, which has been discussed in several XLIF case reports and series.
With the relatively new OLIF approach, an oblique corridor at the plane between the anterior great vessels and more lateral psoas muscles is accessed using a mini‐open incision. The benefits of this approach include minimal peritoneal retraction and no neuromonitoring required for retractor placement since a transpsoas approach is not employed8. The oblique trajectory allows direct visualization of the disc space and allows the surgeon to avoid surgical trauma to the psoas muscle and lumbosacral plexus altogether. Furthermore, the angle of the oblique approach also allows for a unique view of the epidural space should the surgeon desire, facilitating removal of ventral osteophytes and disc herniation, combining both direct and indirect decompression advantages.
Typical indications for fusion procedures such as ALIF and OLIF in prior reports include degenerative disc disorders, discitis and pseudoarthrosis at L5S1, as well as isthmic spondylolisthesis11, 12. However, the advantages of the oblique trajectory may also be apparent at high lumbar levels. There have been few reports of the use of OLIF at L2‐3 and L3‐4 levels. Even though the issue of obstruction by iliac crests is not as evident at high lumbar spine levels, an oblique trajectory may facilitate access even in patients with very difficult adult degenerative scoliosis. Furthermore, while there are some studies on the use of other approaches such as ALIF for pseudoarthrosis following failed posterior surgery13, there is limited available evidence in the literature to support this as an indication for OLIF, particularly at the higher lumbar levels.
In the present description, we report the first case of using OLIF for revision of a prior posterior fusion non‐union at the L2‐3 level. The OLIF technique is feasible at this disc level, with satisfactory fusion achieved with acceptable oblique trajectory feasibility. We advocate expanding the indications of the OLIF approach to include failed posterior fusion cases from high lumbar intervertebral disc levels.
Disclosure: No funds were received in support of this work.
References
- 1. Assaker R. Minimal access spinal technologies: state‐of‐the‐art, indications, and techniques. Joint Bone Spine, 2004, 71: 459–469. [DOI] [PubMed] [Google Scholar]
- 2. Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion—systematic review and meta‐analysis. Br J Neurosurg, 2015:1–7. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Phan K, Rao PJ, Kam AC, Mobbs RJ. Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: systematic review and meta‐analysis. Eur Spine J, 2015, 24: 1017–1030. [DOI] [PubMed] [Google Scholar]
- 4. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J, 2006, 6: 435–443. [DOI] [PubMed] [Google Scholar]
- 5. Phan K, Rao PJ, Scherman DB, Dandie G, Mobbs RJ. Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci, 2015, 22: 1714–1721. [DOI] [PubMed] [Google Scholar]
- 6. Acosta FL, Liu J, Slimack N, Moller D, Fessler R, Koski T. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine, 2011, 15: 92–96. [DOI] [PubMed] [Google Scholar]
- 7. Silvestre C, Mac‐Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini‐open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J, 2012, 6: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand‐alone lateral interbody fusion. J Neurosurg Spine, 2013, 19: 110–118. [DOI] [PubMed] [Google Scholar]
- 9. Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976), 2010, 35 (26 Suppl.): S331–S337. [DOI] [PubMed] [Google Scholar]
- 10. Davis TT, Hynes RA, Fung DA, et al Retroperitoneal oblique corridor to the L2‐S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine, 2014, 21: 785–793. [DOI] [PubMed] [Google Scholar]
- 11. Mobbs RJ, Loganathan A, Yeung V, Rao PJ. Indications for anterior lumbar interbody fusion. Orthop Surg, 2013, 5: 153–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Phan K, Mobbs RJ. Sacrum fracture following L5‐S1 stand‐alone interbody fusion for isthmic spondylolisthesis. J Clin Neurosci, 2015, 22: 1837–1839. [DOI] [PubMed] [Google Scholar]
- 13. Mobbs RJ, Phan K, Thayaparan GK, Rao PJ. Anterior lumbar interbody fusion as a salvage technique for pseudarthrosis following posterior lumbar fusion surgery. Global Spine J, 2015, doi: 10.1055/s-0035-1555656. [DOI] [PMC free article] [PubMed] [Google Scholar]


