Abstract
This article describes the arch plate technique for treating lumbosacral tuberculosis. Lumbosacral tuberculosis often leads to the destruction of anterior vertebral columns and presacral or iliopsoas abscess, which requires an anterior approach to achieve thorough debridement. Due to the complexity of the anatomical structure of lumbosacral spine and the high requirement of fixation stability, a combined posterior approach to perform internal fixation is necessary, which is rather traumatic. On the other hand, most of the current anterior lumbosacral internal fixation systems cannot be applied to spinal tuberculosis patients who have irregular bony endplate destruction. The arch plate was designed as a cephalic narrow and caudal wide trapezoid or triangle outline according to the preliminary anatomic research. In terms of the endplate bony destruction, a multidirectional technique was introduced in the arch screws, which enables surgeons to arbitrarily change the direction of the screw in the range of 5°–20°, which increases the length and the inclination angles in the sagittal plane of the implant screw and makes sure that the autologous iliac bone graft fits the irregular bone destruction for maximum stability. This study demonstrated the effectiveness of one‐stage anterior debridement, bone grafting, and arch plate fixation to treat lumbosacral tuberculosis. The risk of intraoperative and postoperative complications, such as injury to major vessels, could be minimized. This surgical procedure had many advantages, including a shorter operation time, less blood loss, and better functional recovery over the conventional combined anterior and posterior approach.
Keywords: Anterior approach, Interbody fusion, Internal fixation, Lumbosacral, Spinal tuberculosis
Introduction
Lumbosacral tuberculosis often leads to the destruction of anterior vertebral columns and presacral or iliopsoas abscess, which requires anterior approach to achieve thorough debridement. Due to the complexity of the anatomical structure of lumbosacral spine and the high requirement of fixation stability, combined posterior approach to perform internal fixation is necessary, which is rather traumatic. Most of the current anterior lumbosacral internal fixation systems are designed for degenerative diseases with intact endplate. Therefore, these systems cannot be applied to the spinal tuberculosis patients who have irregular bony endplate destruction. This special anterior internal fixation system is designed according to the course of iliac vessels, the anatomic characteristics of lumbosacral spine and the shape of the damaged endplate. In addition, the multidirectional locking plate (arch plate) not only has many advantages including threaded locking angle stability and preventing the screw from backing out, but also has all kinds of screws driving in appropriate directions to avert irregular bone destruction and acquire maximum stability (Fig. 1).
Figure 1.
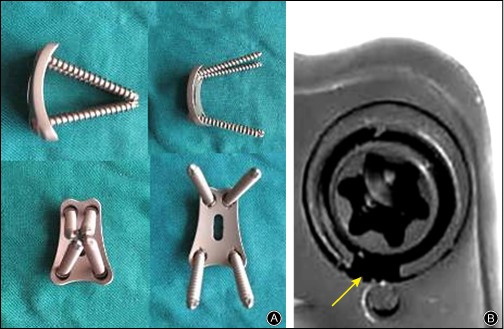
The arch plate can provide better stability for irregular bone defects of spinal tuberculosis with its multidirectional self‐locking technique. (A) The screw angles could can changed arbitrarily within 20° in any direction to guarantee maximum screw length within the residual bone. (B) Self‐locking threads ensure the maintaining of screw angles.
Technique
This patient was a 42‐year‐old man with lumbosacral tuberculosis. In addition to routine tests for the surgery, a computed tomography (CT) angiography (CTA) was done to confirm whether the vascular structure and safe zones in the lumbar sacral region were available for the surgery (Fig. 2).
Figure 2.
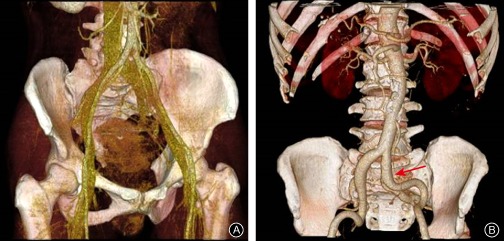
The anatomical relationship between the iliac vessels and lumbosacral region may be demonstrated by pre‐operation computed tomography angiography. (A) Available for anterior plate, (B) unavailable for anterior implant due to iliac arterial variation.
The patient was put in a Trendelenburg supine position under general anesthesia, and the patient's waist was elevated with a pad for a better exposure. The bridge of the operation table was right below the surgical region so that intraoperative correction of lumbar sacral angle could be performed. In addition, the hip and knee joints were put in a 20° flexion position to relax the iliac vessels.
A peritoneal approach or the transperitoneal approach could be used for this surgery. In this case, the transperitoneal approach was applied. A left side paramedian incision of 10 cm was made on the lower abdominal part after a C‐arm fluoroscopy confirmation of spinal levels. The rectus abdominis was directed to the right after the incision of anterior rectus sheath. Then, the transverse fascia and the peritoneal fat were opened and a blunt dissection was done until the anterior column of targeted spinal body was visible. The course of the left and right common iliac veins and artery were carefully identified to decide the safe zone between the vessels.
A blunt dissection was then performed within the safe zone to expose the anterior structures between L5 and S1 levels and the presacral abscess. Pus, caseous necrosis tissue, granulation tissue, bone sequestrum, psoas abscess, and the necrotic disc were thoroughly debrided and spinal canal decompression was also performed. In addition, the matter removed was sent for drug sensitivity tests with a gene chip.
The L5S1 intervertebral space was then distracted to correct the kyphosis deformity and to restore the lumbosacral angle and the height of the intervertebral space. The intervertebral distraction value was then measured.
Afterwards the surgical site was repeatedly rinsed with saline and hydrogen peroxide until the liquids turned clear.
One or two appropriate sized three cortical autogenous autologous iliac bones were taken from the rear part of the ipsilateral anterior superior iliac spine, according to the extent of defect area in the vertebral body and the thickness of the iliac crest, in order to buttress the L5S1 intervertebral space. The arch plate was placed in the anterior part of the L5 and S1 vertebral bodies. The entry point of the screw was prepared by a craniotomy cone, with a suggested convergence of the screw trajectory on the axial plane of between 5° to 10°. On the sagittal plane, the cranial screw trajectories should be towards the superior‐posterior of the L5 vertebra and the caudal trajectories should be towards the inferior posterior of sacral vertebra, so that the maximum screw length can be acquired. Under certain circumstances, the location of the plate and the direction of the screws were selected based on the condition of the residual bone defect. On finishing the implantation, all locking screws were tightened. Drainage tubes were properly placed and the wound was conventionally closed.
Follow Up
Post‐operatively, cefazolin sodium was used for 24 h followed by anti‐tuberculosis treatment. Three days postoperatively, the patient was encouraged to perform ambulatory exercise with the protection of a waist brace. The sutures were removed 8 days after surgery and the patient was discharged and prescribed with the waist brace for the next 3 months. The anti‐tuberculosis agents neede to be adjusted according to the drug sensitivity tests based on the intraoperative removals (Fig. 3) .
Figure 3.

Case demonstration: 42‐year‐old man with lumbosacral tuberculosis (A, B) preoperative anteroposterior and lateral X‐ray films; (C) preoperative computed tomography (CT); (D, E) preoperative MRI; (F,G) preoperative CT angiography (H, I) X‐ray 3 months after operation; (J, K) CT 3 months after operation; (L, M) X‐ray 12 months after operation; (O, P) CT 12 months after operation.
Discussion
Are Combined Anterior and Posterior Approaches for Treating Lumbosacral Tuberculosis Really Necessary?
Although the single‐stage or second‐stage combined anterior and posterior approaches meet the requirements of stability reconstruction and achieve good results in the treatment of lumbosacral spinal tuberculosis, surgical damage, operative time, and health‐care costs are significantly increased in these combined approaches1.
There are three main reasons for performing a combined anterior and posterior approach:
The lumbosacral anatomical structure is complex, especially when the surrounding tissue undergoes adhesions caused by the lesion, or the relatively limited range of exposure and space of internal fixation caused by iliac vessels' courses. An internal fixation system that is too close to the iliac vessels could cause a pseudoaneurysm, which is generally the consequence of a vascular injury.
The safety and efficacy concerns of implantation in the site of tuberculosis.
The effectiveness of current lumbosacral anterior internal fixation system. It is difficult to achieve biomechanical stability in implementing internal fixation devices because tuberculosis often leads to massive bone destruction in the anterior and middle spinal columns.
Due to the complexity of the anatomy of lumbosacral spine, the incidence of vascular injury in anterior internal fixation and stability reconstruction surgery ranges from 1.2% to 15.6%2, 3. With respect to the complex anatomy of anterior lumbosacral and related surrounding tissue, Inamasu et al. defined the concept of a clear space zone in front of the lumbosacral spine, a triangle consisting of these surrounding structures, including the iliac vessels on both sides and the superior border of the sacropromontory4. This triangular area contained no major blood vessels or nerve trunks. Barrey et al. reported an in vivo anatomic evaluation using a preoperative 3D‐CT to develop the concept of a vascular window in 146 patients5. A vascular window at L5S1 was defined as the free vascular area for the anterior part of the L5S1 disc. In our previous anatomic cadaveric study, 41 human lumbosacral spines, including those of 26 men and 15 women, were analyzed. The study demonstrated that when an L5S1 interbody fusion and an internal fixation were performed via an anterior approach, the surgery space mainly depended on three factors, including: (i) the location of the left common iliac vein and the right common iliac artery; (ii) the confluence angle of the left and the right common iliac veins and their corresponding relationship with adjacent lumbosacral vertebrae; and (iii) the width of the override point of the left common iliac vein and the right common iliac artery at different levels of the lumbosacral spine. The area appropriate for internal fixation could be defined by several structures, including the midline of the sacrum as a medial border and the external iliac vein as a lateral border, average width of 24.5 mm (22–27 mm), and an average length of about 30 mm (the vertical distance between the upper edge of the anterior hole of S1 and the sacral promontory). The area did not contain any important structures, such as major blood vessels and nerves. The arch plate was well designed, from the shape to the overall integrity, based on these anatomic parameters. The trapezoidal or triangular shapes were suitable for all body types.
Choice of Anterior Lumbosacral Internal Fixation Systems
Since there is a tendency of slipping forward when the L5 vertebra bears the weight of the trunk due to an S1 vertebral body anteversion, the main structures resisting against an L5 slipping forward are the L5S1 facet joint and the intervertebral space. When the tuberculosis focus is located at the L5S1 level, the intervertebral disc could collapse and the vertebral body bone destruction could cause a decrease in the lumbosacral angle. Meanwhile, given the tendency of L5S1 facet joint detachment, the L5S1 facet joint would be the only structure resisting the L5S1 shear stress, which could accelerate facet joint degeneration, causing lumbosacral pain. The principle for a lumbosacral tuberculosis treatment is to restore the height of the vertebral body in order to place the bone graft against the local shear and axial stress, and to reconstruct the early stability of the spine through internal fixation6, 7.
However, all existing anterior lumbosacral internal fixation systems, such as SynFix‐LR (Synthes, Solothurn, Switzerland)8, the Trinica anterior lumbar plate system (Zimmor, Minneapolis, MN, USA)9, and the Pyramid anterior lumbar plate (Sofamor, Menphis, TN, USA)10, cannot be applied to spinal tuberculosis patients who have irregular bony endplate destruction. He and Xu performed a single‐stage anterior debridement and autograft fusion combined with two self‐locking titanium anterior lumbosacral vertebrae plates (SCIENT X, Parc Ariane, FRANCE) in order to treat 13 cases of lumbosacral tuberculosis1. The average operative time, blood loss, hospital stay, and lumbosacral correction angle were 190 min, 410 mL, 15 days, and 5.1°, respectively, which proved the safety and efficacy of the one‐stage anterior surgical procedure. However, Pach, designed with two split titanium plates, had several limitations; for instance; a complicated placement procedure, unstable parallelogram construction, and a vulnerable locking sheet preventing screw loosening.
In this case, the arch plate was designed as a cephalic narrow and caudal wide trapezoid or triangle outline according to preliminary anatomic research. The cephalic narrow and caudal wide trapezoid shape resolved the deficiencies of the Pach titanium plate, such as its cumbersome placement procedures and unstable parallelogram construction. In terms of endplate bony destruction, a multidirectional technique was introduced in the arch screws, which enabled surgeons to arbitrarily change the direction of the screw in the range of 5–20° and increase the length and the inclination angles in the sagittal plane of the implant screw. When tightening a locking head screw, the screw and the plate would come together to possess threaded locking angle stability and prevent the screw loosening. The arch plate, using a multidirectional self‐locking technology has many advantages, including threaded locking angle stability and preventing the screw from backing off. Furthermore, it has various directions for screw driving to make sure the autologous iliac bone graft fits the irregular bone destruction in order to acquire maximum stability. At the 6‐month follow up, bone healing and trabecular bone formation were observed through the interface between the endplate and the bone graft.
Surgery Tips
Before the surgery, a complete radiology examination should be acquired, especially a CTA, to fully appraise the surgeon of the anatomical structures of the iliac vessels and lumbosacral region.
The patient is put in a Trendelenburg supine position to reduce intestinal accumulation within the surgical site, and the patient's waist is elevated with a pad for better exposure. In addition, the hip and knee joints are put in a flexion position of 20° to relax the iliac vessels.
The abscess may be confirmed by a syringe puncture before blunt dissection and traction of prevertebral fascia and the abscess wall. Make sure to debride the lesion within the abscess wall to avoid any iatrogenic injury.
The caseous necrosis and granulation tissue should be sent for pathology, tuberculosis culture, drug sensitivity tests and drug‐resistant gene detection with a gene chip.
If the bone quality is good enough, the cranial screw trajectories should be towards the superior‐posterior of L5 vertebra and the caudal trajectories should be towards the inferior posterior of sacral vertebra on the sagittal plane, so that the maximum screw length may be acquired. If the bone defect is irregular, the location of the plate and the direction of the screws should be decided based on the condition of the residual bone structures.
Highlights
Lumbosacral tuberculosis may be treated by one stage anterior only approach.
The arch plate system, using multidirectional self‐locking technology has many advantages, including threaded locking angle stability and preventing the screw backing off, and the various directions for the screw to fit the irregular bone destruction in order to acquire maximum stability.
Supporting information
Video Image
Disclosure: The authors have no conflict of interest to declare.
References
- 1. He Q, Xu J. Comparison between the antero‐posterior and anterior approaches for treating L5‐S1 vertebral tuberculosis. Int Orthop, 2012, 36: 345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Samuel S. Comment on Oguz et al.: a new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop, 2010, 34: 613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wood KB, Devine J, Fischer D, Dettori JR, Janssen M. Vascular injury in elective anterior lumbosacral surgery. Spine (Phila Pa 1976), 2010, 35 (9 Suppl.): S66–S75. [DOI] [PubMed] [Google Scholar]
- 4. Inamasu J, Kim DH, Logan L. Three‐dimensional computed tomographic anatomy of the abdominal great vessels pertinent to L4‐L5 anterior lumbar interbody fusion. Minim Invasive Neurosurg, 2005, 48: 127–131. [DOI] [PubMed] [Google Scholar]
- 5. Barrey C, Ene B, Louis‐Tisserand G, Montagna P, Perrin G, Simon E. Vascular anatomy in the lumbar spine investigated by three‐dimensional computed tomography angiography: the concept of vascular window. World Neurosurg, 2013, 79: 784–791. [DOI] [PubMed] [Google Scholar]
- 6. Choi KC, Ryu KS, Lee SH, Kim YH, Lee SJ, Park CK. Biomechanical comparison of anterior lumbar interbody fusion: stand‐alone interbody cage versus interbody cage with pedicle screw fixation—a finite element analysis. BMC Musculoskelet Disord, 2013, 14: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim DJ, Yun YH, Moon SH, Riew KD. Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine (Phila Pa 1976), 2004, 29: E275–E279. [DOI] [PubMed] [Google Scholar]
- 8. Schimmel JJ, Poeschmann MS, Horsting PP, Schönfeld DH, van Limbeek J, Pavlov PW. PEEK cages in lumbar fusion: mid‐term clinical outcome and radiological fusion. J Spinal Disord Tech, 2012. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 9. Lee CH, Hsu CC, Huy DC. An optimization study of the screw orientation on the interfacial strength of the anterior lumbar plate system using neurogenetic algorithms and experimental validation. J Biomech Eng, 2014, 136: doi: 10.1115/1.4028412. [DOI] [PubMed] [Google Scholar]
- 10. Gerber M, Crawford NR, Chamberlain RH, Fifield MS, LeHuec JC, Dickman CA. Biomechanical assessment of anterior lumbar interbody fusion with an anterior lumbosacral fixation screw‐plate: comparison to stand‐alone anterior lumbar interbody fusion and anterior lumbar interbody fusion with pedicle screws in an unstable human cadaver model. Spine (Phila Pa 1976), 2006, 31: 762–768. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video Image


