Abstract
Objectives
Metacarpal (MC) fractures are very common, accounting for 18% of all fractures distal to the elbow. Many MC fractures can be treated non‐operatively; however, some are treated most effectively with surgical stabilization, for which there are multiple methods. It was postulated that plates would have a significantly higher (P < 0.05) load to failure than crossed K(XK)‐wires and that intramedullary metacarpal nails (IMNs) and XK‐wires would have equivalent load to failure.
Methods
Mid‐diaphyseal transverse fractures were created in 36 synthetic metacarpals and stabilized using nails, XK‐wires or non‐locking plates. Three‐point bending was performed with continuous recording of load and displacement. Statistical analysis was performed using single factor ANOVA and Scheffe's test. Statistical significance was defined as P < 0.05.
Results
Biomechanical testing revealed significant differences between groups in load‐to‐failure. Average load to failure was significantly greater in the plate (1669 ± 322 N) than the XK‐wire (146 ± 56 N) or IMN (110 ± 43 N) groups. The loads to failure of the K‐wires and nails were equivalent. Plates were 11 and 15 times stronger in three‐point bending than the K‐wires and nails, respectively. There was no statistically significant difference between strengths of the K‐wires and nails.
Conclusions
Although plates are the most stable means of fixation of midshaft metacarpal fractures, if minimally‐invasive techniques are indicated, intramedullary nails may provide equivalent stability as commonly‐used XK‐wires. Although some studies have shown favorable clinical outcomes with IMNs, additional clinical correlation of these biomechanical results to fracture healing and outcomes is needed.
Keywords: Biomechanical, Intramedullary nail, Metacarpal fracture, Stabilization
Introduction
Metacarpal (MC) fractures are very common, accounting for 18% of all fractures distal to the elbow1. Many MC fractures can be treated non‐operatively; however, some are treated most effectively by surgical stabilization2, 3, for which there are multiple methods that have been compared by many published studies2, 3, 4, 5, 6, 7. They include various plate‐and‐screw constructs (plate)8, 9, 10, 11, 12, 13, 14, screws alone15, percutaneous, intermetacarpal wires5, crossed K‐wires (XK‐wires)7, 16, intramedullary K‐wires7, 16, 17, the “bouquet” technique4, 18, 19, and proximally‐locked intramedullary metacarpal nails (IMNs)20, 21, 22. Relatively few studies have evaluated intramedullary nails, which have been designed to provide a minimally‐invasive, proximally‐locked option for stabilization of MC fractures.
The history of surgical stabilization of metacarpals began with intramedullary fixation by vom Saal16 and Lord17 in the 1950s. Both Lord and vom Saal emphasized the advantages of intramedullary metacarpal fixation over casting in preventing stiffness and expediting return to work. The first publications on IMN fixation in the 1950s reported successful outcomes without specific outcomes measures; for example, Lord wrote “Fixation has been good, union has been prompt, and no infection has been encountered”17. These devices provided no locking of the nail. Later, various wiring techniques were employed, ranging from XK‐wires, to cerclage wires, to wire loops6, 7. Small plates were introduced and used widely, studies showing that plates provided superior stabilization to cerclage wires and K‐wires6, 7. However, plates required larger surgical exposure and were associated with complications such as stiffness, nonunion, plate prominence, infection and tendon rupture. In 1987 and 1998, Stern and colleagues23, 24 reported complications associated with plate fixation of MC and phalangeal fractures. In the first study, complications occurred in 42% and in the second in 36% of MC fractures (24/66). In the follow‐up study, these authors concluded that, despite improvements in plate design and profile, use of titanium and operating room instrumentation, complications continued to occur because plates are often utilized in patients with open fractures and severely traumatized hands and digits.
Prompted by the wide variety of MC fracture patterns and associated soft tissue injuries, surgeons continued to develop and study new stabilization techniques. Several authors have described “bouquet osteosynthesis” of intramedullary nailing in which multiple small K‐wires are inserted and buried to stabilize the fracture4, 18, 19, 25, 26. These studies have reported generally high patient satisfaction and a low rate of infection and other complications. However, this approach provides minimal rotational stability, is technically challenging, costly and requires a secondary intervention to remove the wires.
Few clinical studies of IMNs have been published, the largest having been performed by one of the implant's designers21. Orbay and Touhami reported excellent clinical outcomes for IMNs with few complications but did not perform biomechanical testing or compare IMN fixation with other stabilization options. Their study included 150 metacarpal and proximal phalanx fractures in 125 patients. Ninety‐five fractures in 83 patients were treated with proximally‐locked IMNs, whereas 55 fractures in 42 patients were treated with non‐locking nails. Of the 95 locking nails, 76 were in MCs and 19 in phalanges. In the locking nail patients, the total active motion was 244° (94% of normal contralateral side) and strength was 92% of the contralateral side. All fractures had healed by an average of 5.7 weeks. Complications were seen in seven patients, two in each group developing extensor tendon irritation that necessitated early nail removal and in three patients (one in the non‐locking and two in the IMN group) the nail penetrated through the MC head, also necessitating early nail removal.
Ozer et al. compared non‐locked IMNs and plate fixation for MC fractures in a series of 52 consecutive closed, displaced, extra‐articular metacarpal fractures22. Thirty‐eight patients underwent IMN fixation and 14 plate‐screw fixation. These researchers used the same IMNs as Orbay but did not utilize proximal locking sleeves. They found no statistically significant differences in post‐healing range of motion, time to union or Disabilities of the Arm, Shoulder, and Hand scores. Surgical time was significantly less in the IMN group. However, 5/38 patients in the IMN group lost fixation and had issues with nail penetration into the metacarpophalangeal joint, necessitating hardware removal in the operating room and revision with plate‐screw fixation. In addition, 15 patients in the IMN group (five ring fingers and ten small fingers) had extensor tendon irritation and required removal of hardware without tenolysis.
We have identified no published studies on the biomechanical stability provided by MC IMNs. This study investigated the biomechanical stability of MC fractures stabilized by three different methods: plates, XK‐wires and IMN. We postulated that plates would have a significantly higher (P < 0.05) load to failure than XK‐wires or IMNs and that XK‐wires would have equivalent load to failure as IMNs.
Materials and Methods
Thirty‐six fourth‐generation synthetic MCs (Sawbones; Pacific Research Laboratories, Vashon, WA, USA) were obtained. Mid‐diaphyseal transverse fractures were created with an oscillating autopsy saw, one millimeter thick. The specimens were randomly assigned to one of three fixation groups: IMN, XK‐wires, or plates and screws and the fractures reduced by the allocated method. There were 12 specimens in each group.
In the IMN group, 0.062 blunt‐end nails (Small Bone Fixation System; Hand Innovations, Biomet, Warsaw, IN, USA) were implanted by making a corticotomy with the opening awl just distal to the proximal articular surface. The nails were then contoured with a gentle apex‐palmar bend to allow for easier advancement in the medullary canal and to achieve three‐point fixation. The distal ends were impacted into the distal metaphyses and the proximal ends locked into the volar cortexes with locking sleeves as described by Orbay20 (Fig. 1).
Figure 1.
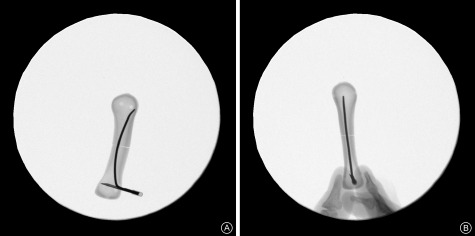
Anteroposterior (A) and lateral (B) fluoroscopic views of an intramedullary nail in a composite metacarpal.
In the XK‐wire group, two 0.062 diameter K‐wires were implanted in a crossed fashion. Positioning of hardware was confirmed with mini‐C fluoroscopy and visualization.
In the plate group, standard, straight, 2.5 mm F3 plates (Hand Innovations) were cut to six holes and positioned dorsally. On both sides of the fractures, three 2.5 mm non‐locking cortical screws were inserted with bi‐cortical fixation following the standard AO technique27.
Three‐point bending was performed on a servohydraulic materials test frame (Bionix 858; MTS, Eden Prairie, MN, USA). Specimens were positioned on parallel steel bars and secured rotationally with custom‐formed polyester resin molds. Three‐point bending force was applied under displacement control at the fracture sites in an apex‐dorsal direction at a velocity of 10 mm/min with continuous recording of load and displacement. The bending force was positioned directly over the fracture (Fig. 2). This setup was chosen because it is the most common pattern of clinical fracture displacement. The protocol was based on previously published studies10, 12.
Figure 2.

Servohydraulic test frame showing testing of IMN. The artificial bones are positioned palmar side up.
In the plate group, failure was defined as a sharp change in the force‐displacement curve (Fig. 3). In the XK‐wire and IMN groups, failure was more difficult to define because it occurred over a continuum during which the wires and nails backed out and bent. This has also been noted in previous studies of K‐wire fixation7. In the IMN group, the nails tended to dislodge from the distal metaphyseal bone while the proximal locking mechanism remained stable. The amount of displacement that occurred at the fracture site was visualized and the point at which clinical failure was believed to have occurred noted. It was determined that this point of failure occurred when the MTS actuator had traveled 5.5 mm toward the table. The force required to achieve 5.5 mm of vertical displacement in the XK‐wires and IMN was measured.
Figure 3.
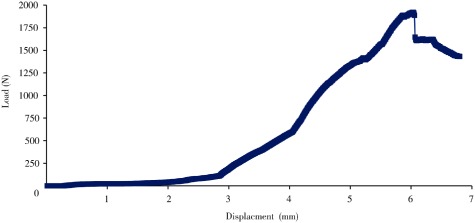
Load‐displacement curve for specimens stabilized with plates and screws.
Statistical Analysis
An a priori power analysis using an effect size determined from a prior study 12 showed that approximately six sawbone metacarpals were needed in each group (sample size, 18) to achieve a power of 80. A post hoc power analysis was performed after all samples had been tested. All sample data were used in the final calculations. Statistical analysis was performed using single factor anova to detect differences between groups. Post hoc analysis using Scheffe's test was then performed to test for differences among individual groups. Statistical significance was defined as P < 0.05.
Results
Biomechanical testing revealed significant differences between groups in load‐to‐failure. In the plate group, failure occurred as the plate bent slightly, cracks propagated in the bone and screws began to back out. In only one specimen was there a fracture with significant bony displacement. Average load to failure was significantly greater in the plate group (1669 ± 322 N) than the XK‐wire (146 ± 56 N) or IMN (110 ± 43 N) groups (P < 0.05). The XK‐wire group load to failure showed a trend toward greater stability than the IMN group; however, this difference was not statistically significant (P = 0.09, Fig. 4).
Figure 4.
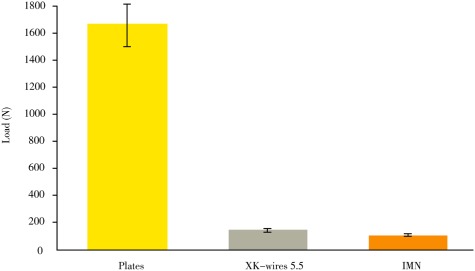
Average load to failure (in Newtons).
Discussion
Metacarpal fractures are common and can be stabilized in multiple ways. Unlike other MC fracture fixation methods, the biomechanical stability of proximally‐locked IMNs for MC fractures has not previously been compared to other commonly utilized techniques. Our data support both of our hypotheses and suggest that plate‐screw constructs are 11 and 15 times more stable than XK‐wires and IMNs, respectively. Although XK‐wire constructs showed a trend toward greater stability than proximally‐locked IMNs, these two techniques did not differ significantly instability (P = 0.09).
Because, to our knowledge, no other studies, have published biomechanical data on the Small Bone Fixation system (IMN; Hand Innovations) for MC fractures, we were unable to compare our findings directly with those previously reported. This investigation is the first biomechanical study comparing the MC IMN to other commonly used fixation techniques. Understanding the properties of the available implants is important for surgeons because it helps them to choose the most appropriate one for the specific clinical situation. One of the strengths of this study is the use of composite bones. Many previous studies of MC fractures have utilized either cadaveric bones or pig metacarpals6, 7, 9, 11, 28, 29, 30, 31, 32, 33. Composite metacarpal bones have a consistent size and mechanical behavior that allows a comparison of the various fixation devices with fewer confounding variables. Cadaveric MCs could potentially confound biomechanical testing data because of inter‐specimen variations in bone quality, mineral content, cortical thickness and bone size. Pig MCs, although utilized in previous studies because of their consistent size and bone quality, have a medullary canal that is much larger than that in human bones and are therefore not stabilized effectively by the IMN. Many recent studies have begun to use synthetic bones to eliminate inter‐specimen variability8, 10, 12, 13, 34.
Limitations of our study include lack of in vivo testing or testing of specimens in torsion or with apex‐volar or with axial loads. Because MC fractures generally displace into apex‐dorsal angulation, we applied a bending force that created that type of displacement. Also, we did not investigate the effects of repeated submaximal forces. Additionally, no soft‐tissues were present to provide additional stability. Because the XK‐wires and IMNs did not fail because of hardware failure or a dramatic shift in the load‐displacement curve, testing in torsion or with repeated sub‐maximal forces would not likely yield valid data. Also, we believed it unnecessary to test with an apex‐volar load because this is unlikely to be a mode of failure in vivo. Finally, it should be noted that the principles of fracture fixation for metacarpals differ from those of long bones or the upper or lower extremities, because only minimal stability is required for early rehabilitation.
In conclusion, the data confirm that plates are the most stable means of fixation of midshaft metacarpal fractures. Given the complications associated with plate fixation, our data suggest that, although much less stable than plates, IMNs may be an additional option for MC fracture stabilization. An ideal clinical application might include treatment of multiple transverse or short‐oblique MC fractures in which there is significant soft tissue trauma and swelling. In this situation IMNs, like K‐wires, would allow for minimally‐invasive stabilization that is simple to perform. Also, the speed of IMN implantation could be advantageous in unstable trauma patients. Although some studies have shown favorable clinical outcomes with IMNs20, 21, 22, additional clinical correlation of these biomechanical results with fracture healing and other outcomes is needed.
Our data indicate that plate fixation provides a very stable construct, one that is 11 and 15 times as stable as XK‐wires or IMN, respectively. However, plate fixation is not without complications and requires more soft‐tissue dissection than the other methods. If minimally‐invasive techniques are indicated, the current study's data suggest that IMNs may provide equivalent stability to commonly‐used XK‐wires and may be a viable option for metacarpal shaft fracture stabilization.
Acknowledgments
Thanks to Biomet for providing hardware and to Matthew Allen DVM and Gregory P. Kolovich MD (both of Ohio State University, Columbus, OH, USA) for consultation.
Disclosure: This research received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors. Biomet (Warsaw, IN, USA) provided the hardware used in this study. The authors report no other potential conflicts of interest. The authors have no agreement that forbids them from publishing the results of this research.
References
- 1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am, 2001, 26: 908–915. [DOI] [PubMed] [Google Scholar]
- 2. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg, 2008, 16: 586–595. [DOI] [PubMed] [Google Scholar]
- 3. Freeland AE, Geissler WB, Weiss AP. Surgical treatment of common displaced and unstable fractures of the hand. Instr Course Lect, 2002, 51: 185–201. [PubMed] [Google Scholar]
- 4. Strub B, Schindele S, Sonderegger J, Sproedt J, von Campe A, Gruenert JG. Intramedullary splinting or conservative treatment for displaced fractures of the little finger metacarpal neck? A prospective study. J Hand Surg Eur Vol, 2010, 35: 725–729. [DOI] [PubMed] [Google Scholar]
- 5. Wong TC, Ip FK, Yeung SH. Comparison between percutaneous transverse fixation and intramedullary K‐wires in treating closed fractures of the metacarpal neck of the little finger. J Hand Surg Br, 2006, 31: 61–65. [DOI] [PubMed] [Google Scholar]
- 6. Firoozbakhsh KK, Moneim MS, Howey T, Castaneda E, Pirela‐Cruz MA. Comparative fatigue strengths and stabilities of metacarpal internal fixation techniques. J Hand Surg Am, 1993, 18: 1059–1068. [DOI] [PubMed] [Google Scholar]
- 7. Vanik RK, Weber RC, Matloub HS, Sanger JR, Gingrass RP. The comparative strengths of internal fixation techniques. J Hand Surg Am, 1984, 9: 216–221. [DOI] [PubMed] [Google Scholar]
- 8. Sakai A, Oshige T, Zenke Y, Menuki K, Murai T, Nakamura T. Mechanical comparison of novel bioabsorbable plates with titanium plates and small‐series clinical comparisons for metacarpal fractures. J Bone Joint Surg Am, 2012, 94: 1597–1604. [DOI] [PubMed] [Google Scholar]
- 9. Doht S, Jansen H, Meffert R, Frey S. Higher stability with locking plates in hand surgery? Biomechanical investigation of the TriLock system in a fracture model. Int Orthop, 2012, 36: 1641–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gajendran VK, Szabo RM, Myo GK, Curtiss SB. Biomechanical comparison of double‐row locking plates versus single‐ and double‐row non‐locking plates in a comminuted metacarpal fracture model. J Hand Surg Am, 2009, 34: 1851–1858. [DOI] [PubMed] [Google Scholar]
- 11. Ochman S, Doht S, Paletta J, Langer M, Raschke MJ, Meffert RH. Comparison between locking and non‐locking plates for fixation of metacarpal fractures in an animal model. J Hand Surg Am, 2010, 35: 597–603. [DOI] [PubMed] [Google Scholar]
- 12. Sohn RC, Jahng KH, Curtiss SB, Szabo RM. Comparison of metacarpal plating methods. J Hand Surg Am, 2008, 33: 316–321. [DOI] [PubMed] [Google Scholar]
- 13. Fischer KJ, Bastidas JA, Provenzano DA, Tomaino MM. Low‐profile versus conventional metacarpal plating systems: a comparison of construct stiffness and strength. J Hand Surg Am, 1999, 24: 928–934. [DOI] [PubMed] [Google Scholar]
- 14. Dabezies EJ, Schutte JP. Fixation of metacarpal and phalangeal fractures with miniature plates and screws. J Hand Surg Am, 1986, 11: 283–288. [DOI] [PubMed] [Google Scholar]
- 15. Crawford GP. Screw fixation for certain fractures of the phalanges and metacarpals. J Bone Joint Surg Am, 1976, 58: 487–492. [PubMed] [Google Scholar]
- 16. Vom Saal FH. Intramedullary fixation in fractures of the hand and fingers. J Bone Joint Surg Am, 1953, 35: 5–16. [PubMed] [Google Scholar]
- 17. Lord RE. Intramedullary fixation of metacarpal fractures. J Am Med Assoc, 1957, 164: 1746–1749. [DOI] [PubMed] [Google Scholar]
- 18. Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg Am, 1995, 20 (3 Pt 2): S86–S90. [DOI] [PubMed] [Google Scholar]
- 19. Gonzalez MH, Igram CM, Hall RF Jr. Flexible intramedullary nailing for metacarpal fractures. J Hand Surg Am, 1995, 20: 382–387. [DOI] [PubMed] [Google Scholar]
- 20. Orbay J. Intramedullary nailing of metacarpal shaft fractures. Tech Hand Up Extrem Surg, 2005, 9: 69–73. [DOI] [PubMed] [Google Scholar]
- 21. Orbay JL, Touhami A. The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Hand Clin, 2006, 22: 279–286. [DOI] [PubMed] [Google Scholar]
- 22. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. Comparison of intramedullary nailing versus plate‐screw fixation of extra‐articular metacarpal fractures. J Hand Surg Am, 2008, 33: 1724–1731. [DOI] [PubMed] [Google Scholar]
- 23. Stern PJ, Wieser MJ, Reilly DG. Complications of plate fixation in the hand skeleton. Clin Orthop Relat Res, 1987, 214: 59–65. [PubMed] [Google Scholar]
- 24. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am, 1998, 23: 827–832. [DOI] [PubMed] [Google Scholar]
- 25. Foucher G, Chemorin C, Sibilly A. A new technique of osteosynthesis in fractures of the distal 3rd of the 5th metacarpus. Nouv Presse Med, 1976, 5: 1139–1140. (in French) [PubMed] [Google Scholar]
- 26. Sletten IN, Nordsletten L, Husby T, Odegaard RA, Hellund JC, Kvernmo HD. Isolated, extra‐articular neck and shaft fractures of the 4th and 5th metacarpals: a comparison of transverse and bouquet (intra‐medullary) pinning in 67 patients. J Hand Surg Eur Vol, 2012, 37: 387–395. [DOI] [PubMed] [Google Scholar]
- 27. Ruedi TP, Buckley RE, Moran CG. AO Principles of Fracture Management, 2nd edn New York: Thieme, 2007. [Google Scholar]
- 28. Dona E, Gillies RM, Gianoutsos MP, Walsh WR. Plating of metacarpal fractures: unicortical or bicortical screws? J Hand Surg Br, 2004, 29: 218–221. [DOI] [PubMed] [Google Scholar]
- 29. Waris E, Ashammakhi N, Happonen H, et al Bioabsorbable miniplating versus metallic fixation for metacarpal fractures. Clin Orthop Relat Res, 2003, 410: 310–319. [DOI] [PubMed] [Google Scholar]
- 30. Waris E, Ashammakhi N, Raatikainen T, Tormala P, Santavirta S, Konttinen YT. Self‐reinforced bioabsorbable versus metallic fixation systems for metacarpal and phalangeal fractures: a biomechanical study. J Hand Surg Am, 2002, 27: 902–909. [DOI] [PubMed] [Google Scholar]
- 31. Prevel CD, Eppley BL, Jackson JR, et al Mini and micro plating of phalangeal and metacarpal fractures: a biomechanical study. J Hand Surg Am, 1995, 20: 44–49. [DOI] [PubMed] [Google Scholar]
- 32. Prevel CD, McCarty M, Katona T, et al Comparative biomechanical stability of titanium bone fixation systems in metacarpal fractures. Ann Plast Surg, 1995, 35: 6–14. [DOI] [PubMed] [Google Scholar]
- 33. Mann RJ, Black D, Constine R, Daniels AU. A quantitative comparison of metacarpal fracture stability with five different methods of internal fixation. J Hand Surg Am, 1985, 10 (6 Pt 2): 1024–1028. [DOI] [PubMed] [Google Scholar]
- 34. Bozic KJ, Perez LE, Wilson DR, Fitzgibbons PG, Jupiter JB. Mechanical testing of bioresorbable implants for use in metacarpal fracture fixation. J Hand Surg Am, 2001, 26: 755–761. [DOI] [PubMed] [Google Scholar]


