Abstract
This study was designed to itemize and analyze the classification of fracture types and their corresponding outcomes in an attempt to provide a better understanding of the current treatment methods. Two PubMed searches were performed using the words “periprosthetic distal femur fracture” and “periprosthetic supracondylar femur fracture” in studies that were published in the previous 10 years (2004–2014). Data from 41 articlesthat met the general inclusion criteria, were collected and categorized into fracture type and treatment method groupings. Healing outcome and complications were the two parameters used to analyze the data. Treatment techniques were grouped in the following categories: locking plate, non‐locking plate, intramedullary nail/rod, screw, blade plate, cerclage wires, allograft, external fixation, revision arthroplasty, non‐operative, and other. Classification systems by Lewis and Rorabeck, the Association for Osteosynthesis/Orthopedic Trauma Association (AO/OTA), Su et al., Neer et al., Kim et al., Backstein et al., and the Société Française de Chirurgie Orthopédique et Traumatologique were reported. In total 448 fractures were identified, of which Rorabeck type II was the most common fracture studied. The two most successful treatment options for periprosthetic distal femur fractures were locking plate (87%) and intramedullary nail/rod (84%). The most frequent complications associated with periprosthetic distal femur fractures included non/mal/delayed union and the need for revision. Locking plates used to treat Rorabeck type II fractures had a complication rate of 35% and those treated with intramedullary nailing had a higher complication rate of 53%. In conclusion, the most frequent type of periprosthetic distal femur fracture after total knee arthroplasty was Rorabeck type II. The most common treatments for these types of fractures are locked plating and intramedullary nailing, with similar healing rates of 87% and 84%, respectively. However, the complication rate for locked plating was lower than for intramedullary nailing.
Keywords: Distal femur, Periprosthetic fracture, Systematic review, Total knee arthroplasty
Introduction
Total knee arthroplasty (TKA) is a common procedure performed in the elderly population. However, now that elderly patients with knee replacements are living longer and remaining active, fractures around knee replacements are becoming more prevalent. The rate of periprosthetic fractures after TKA is 0.3%–2.5%1. The most common periprosthetic fracture is that of the distal femur, although the fracture pattern can vary.
The most recent systematic review to explore periprosthetic distal femur fractures after TKA was conducted by Herrera et al. in 20082. Their review evaluated previous studies to form a conclusion on the best method fortreatment for periprosthetic distal femur fractures after TKA. They reported that locking plates and retrograde intramedullary nailing produced the most successful results, with retrograde intramedullary nailing slightly outperforming locking plates. Since the rate of periprosthetic fractures will presumably continue to rise, continuing research is needed to better understand and treat these types of fractures. Additionally, because each patient and fracture is unique, a more exhaustive approach may be advantageous.
Evaluating specific treatment methods and specific fracture types may lead to a quicker and more reliable approach in treating periprosthetic distal femur fractures. To date, no literature attempting to link treatment methods with classification types of distal femur fracture has been published. Prompted by the absence of this kind of itemized information, this systematic review examines the literature on the treatment of periprosthetic distal femur fractures after TKA from the past 10 years (i) to organize the reported fracture data by classification type and treatment method; (ii) to determine the most common type of fracture; (iii) to determine the most common treatment method; and (iv) to find any relationships between fracture type and treatment method with regard to outcome.
Methods
Two PubMed searches were performed using the words “periprosthetic distal femur fracture” and “periprosthetic supracondylar femur fracture.” The searches ended on July 8, 2014. Only articles in the English language that were published in the previous 10 years (2004–2014) were included. To be included, each article needed to meet the following general criteria: a study of distal femur fractures after a TKA using any treatment method(s) in which radiological and functional outcomes were analyzed. In order to maintain consistency, articles that examined secondary TKA or secondary distal femur fractures were not used. Additionally, studies that met our criteria but also involved patients with tibia fractures, patella fractures, total hip arthroplasties or other circumstances were included, as long as the individual results for each patient with a distal femur fracture could be identified. Patients without a distal femur fracture after TKA were excluded, as were patients with “floating” total knee prostheses. Review articles were not included.
Data were collected and organized using Microsoft Excel spreadsheets. Each article was thoroughly read and reviewed multiple times throughout the data collection process. The total number of patients and fractures excluded the patients who had died or were lost to follow up, but only if the patient's fracture(s) could be pinpointed to a specific classification. Healing outcome and complications were the two parameters used to analyze the data. Healing outcome referred to the state of the fracture's bony union, such as a malunion, nonunion, or successful union. A successful healing outcome excluded a malunion, nonunion, or hardware failure, unless stated otherwise by the authors. Complications were further divided into the following categories: infection, hardware/implant failure, nonunion/malunion/delayed union, revision, bone grafting, and other.
Results
The searches for periprosthetic distal femur fracture and periprosthetic supracondylar femur fracture for articles published within the previous 10 years yielded 301 results (Fig. 1). Of these, 41 articles met the remaining criteria, generating 1054 patients with 1068 fractures. Nine studies did not report all or some of the fractures, leaving 142 fractures unclassified. An overview of the 41 articles, showing the overall union rate of each study, is presented in Table 1.
Figure 1.
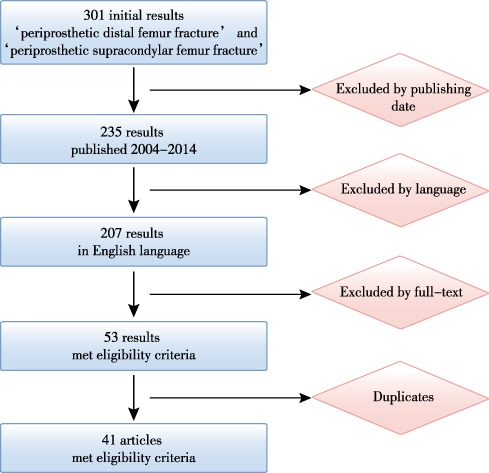
Flow chart illustrating the process of including and excluding studies.
Table 1.
Overview of selected articles
| Authors | Patients (n) | Fractures (n) | Classification system | Treatment method(s) | Successful union (%) |
|---|---|---|---|---|---|
| Ha et al.3 | 14 | 14 | Rorabeck | Locking plate | 100 |
| Jassim et al.4 | 10 | 10 | Rorabeck | Other | 100 |
| Agarwal et al.1 | 15 | 15 | Rorabeck | Locking plate | 100 |
| Revision arthroplasty | |||||
| Non‐operative | |||||
| Gondalia et al.5 | 42 | 42 | AO/OTA | Locking plate | 71 |
| Intramedullary nail/rod | |||||
| Saidi et al.6 | 23 | 23 | Backstein | Allograft | 96 |
| Other | |||||
| Meneghini et al.7 | 85 | 85 | Rorabeck | Locking plate | 84 |
| Intramedullary nail/rod | |||||
| Lee et al.8 | 25 | 25 | Rorabeck | Intramedullary nail/rod | 100 |
| Chen et al.9 | 35 | 36 | Not reported | Other | ‐ |
| Singh and Bhalodiya10 | 23 | 23 | Rorabeck | Locking plate | 78 |
| Non‐locking plate | |||||
| Non‐operative | |||||
| Ries and Marsh11 | 2 | 2 | AO/OTA | Locking plate | 100 |
| Lizaur‐Utrilla et al.12 | 28 | 28 | Rorabeck | Locking plate | 89 |
| Intramedullary nail/rod | |||||
| Screw | |||||
| Revision arthroplasty | |||||
| Kilicoglu et al.13 | 16 | 16 | Neer | Locking plate | 100 |
| Intramedullary nail/rod | |||||
| Ozcan et al.14 | 1 | 2 | Rorabeck | Locking plate | 100 |
| Ries et al.15 | 20 | 20 | AO/OTA | Locking plate | 89 |
| Aldrian et al.16 | 86 | 86 | Su | Locking plate | 88 |
| Intramedullary nail/rod | |||||
| Bae et al.17 | 32 | 33 | Rorabeck | Locking plate | 73 |
| Non‐locking plate | |||||
| Gavaskar et al.18 | 20 | 20 | Rorabeck | Locking plate | 95 |
| Horneff et al.19 | 63 | 63 | Rorabeck | Locking plate | 81 |
| Intramedullary nail/rod | |||||
| Hou et al.20 | 52 | 52 | AO/OTA | Locking plate | 75 |
| Intramedullary nail/rod | |||||
| Jeavons et al.21 | 1 | 1 | Rorabeck | Other | 100 |
| Hoffmann et al.22 | 35 | 36 | AO/OTA | Locking plate | 92 |
| Ebraheim et al.23 | 27 | 27 | not reported | Locking plate | 89 |
| Pot et al.24 | 1 | 1 | not reported | Other | 100 |
| Vallier and Immler25 | 70 | 71 | AO/OTA | Locking plate | 72 |
| Blade plate | |||||
| Ehlinger et al.26 | 15 | 16 | SOFCOT | Locking plate | 94 |
| Streubel et al.27 | 61 | 61 | AO/OTA | Locking plate | 85 |
| Mortazavi et al.28 | 16 | 18 | Kim | Other | 100 |
| Beris et al.29 | 3 | 3 | Rorabeck | External fixation | 100 |
| Platzer et al.30 | 37 | 37 | Su | Locking plate | 89 |
| Intramedullary nail/rod | |||||
| Revision arthroplasty | |||||
| Non‐operative | |||||
| Han et al.31 | 7 | 8 | Rorabeck | Intramedullary nail/rod | 100 |
| Kolb et al.32 | 21 | 21 | AO/OTA | Blade plate | 95 |
| Norrish et al.33 | 15 | 16 | not reported | Locking plate | 92 |
| Chettiar et al.34 | 13 | 14 | not reported | Intramedullary nail/rod | 100 |
| Large et al.35 | 50 | 50 | Rorabeck | Locking plate | 64 |
| Non‐locking plate | |||||
| Intramedullary nail/rod | |||||
| Screw | |||||
| Blade plate | |||||
| Fulkerson et al.36 | 18 | 18 | not reported | Locking plate | 94 |
| Ricci et al.37 | 20 | 22 | AO/OTA | Locking plate | 86 |
| Hurson et al.38 | 1 | 1 | not reported | External fixation | 100 |
| Srinivasan et al.39 | 6 | 6 | AO/OTA | Revision arthroplasty | 100 |
| Gliatis et al.40 | 9 | 10 | Rorabeck | Intramedullary nail/rod | 100 |
| Bezwada et al.41 | 30 | 30 | not reported | Locking plate | 93 |
| Intramedullary nail/rod | |||||
| Kassab et al.42 | 10 | 10 | Rorabeck | Allograft | 90 |
AO/OTA, Association for Osteosynthesis/Orthopedic Trauma Association; SOFCOT, Société Française de Chirurgie Orthopédique et Traumatologique.
Treatment techniques were grouped in the following categories: locking plate, non‐locking plate, intramedullary nail/rod, screw, blade plate, cerclage wires, allograft, external fixation, revision arthroplasty, non‐operative, and other. Classification systems by Lewis and Rorabeck, the Association for Osteosynthesis/Orthopedic Trauma Association (AO/OTA), Su et al., Kim et al., Neer et al., Backstein et al., and the Société Française de Chirurgie Orthopédique et Traumatologique (SOFCOT) were reported43, 44, 45, 46, 47, 48, 49 (Figs 2, 3, 4).
Figure 2.
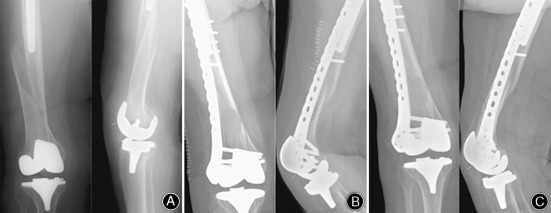
Periprosthetic distal femur fractures (Su type I, Rorabeck type I) was treated with a distal femoral locking plate that spanned the entire interprosthetic zone. (A) preoperative, (B) postoperative day one, (C) union and full‐weight bearing at 17 weeks.
Figure 3.

Periprosthetic distal femur fractures (Su Type II, Rorabeck type II) were treated with a distal femoral locking plate showing; (A) preoperative anteroposterior radiograph; (B) preoperative lateral radiograph; (C) postoperative anteroposterior radiographs demonstrating acceptable reduction of the periprosthetic distal femur fracture treated with reverse locking plate fixation; (D) postoperative lateral radiograph; (E) postoperative anteroposterior radiographs at 3 months demonstrating minimal callus formation and sustained fracture reduction in weight bearing patient; (F) postoperative lateral radiograph at 3 months.
Figure 4.

Periprosthetic distal femur fracture (Su type III, Rorabeck type III) was treated with a distal femoral locking plate showing: (A) preoperative anteroposterior radiograph; (B) preoperative lateral radiograph; (C) postoperative anteroposterior radiographs; (D) postoperative lateral radiograph; (E) postoperative anteroposterior radiographs at 3 months; (F) postoperative lateral radiograph at 3 months.
Many articles contained ambiguous data, so not all fractures could be indentified with their corresponding specific healing outcome and/or complication(s). Of the 1068 total fractures, 488 could be matched with their corresponding healing outcome and 448 could be matched with their corresponding complications (Table 2). The most common documented fracture type was Rorabeck type II (n = 363). There was not enough information to determine either healing outcome or complication(s) of AO/OTA 32A, 32B, 33A, and 33C1; Su type I and II; SOFCOT B1 and C.
Table 2.
Fractures (n)
| Fractures with sufficient data | ||||
|---|---|---|---|---|
| Classification system | Subclassification |
Fractures n = 1068 |
Healing outcome n = 488 |
Complications n = 448 |
| Rorabeck | Type I | 12 | 10 | 7 |
| Type II | 363 | 345 | 310 | |
| Type III | 15 | 15 | 13 | |
| AO/OTA | 32A | 10 | 0 | 0 |
| 32B | 3 | 0 | 0 | |
| 33A | 39 | 0 | 0 | |
| 33A1 | 70 | 5 | 5 | |
| 33A2 | 67 | 16 | 16 | |
| 33A3 | 108 | 27 | 27 | |
| 33B2 | 2 | 2 | 2 | |
| 33C1 | 11 | 0 | 0 | |
| 33C2 | 20 | 1 | 1 | |
| Su | Type I | 43 | 0 | 0 |
| Type II | 76 | 0 | 0 | |
| Type III | 14 | 10 | 10 | |
| Backstein | F2 | 23 | 23 | 23 |
| Kim | Type III | 18 | 18 | 18 |
| Neer | Type II | 13 | 13 | 13 |
| Type III | 1 | 1 | 1 | |
| Type IIII | 2 | 2 | 2 | |
| SOFCOT | B1 | 6 | 0 | 0 |
| C | 10 | 0 | 0 | |
| Unclassified | — | 142 | 0 | 0 |
AO/OTA, Association for Osteosynthesis/Orthopedic Trauma Association; SOFCOT, Société Française de Chirurgie Orthopédique et Traumatologique.
Each fracture with adequate reported data was grouped based on its classification and method of treatment. The success rate of the 488 fractures is reported in Table 3. The largest sample sizes were of Rorabeck type II fractures treated with a locking plate and Rorabeck type II fractures treated with an intramedullary nail/rod. In all, 87% of fractures treated with a locking plate and 84% of fractures treated with an intramedullary nail/rod healed successfully.
Table 3.
Healing outcome (n)
| Classification | Subclassification | Method | Successful healing outcome (%) |
|---|---|---|---|
| Rorabeck | Type I | Locking plate | 2/2 (100) |
| Intramedullary nail/rod | 1/1 (100) | ||
| Screw | 1/1 (100) | ||
| External fixation | 1/1 (100) | ||
| Non‐operative | 3/5 (60) | ||
| Type II | Locking plate | 157/180 (87) | |
| Non‐locking plate | 15/26 (58) | ||
| Intramedullary nail/rod | 102/122 (84) | ||
| Screw | 7/10 (70) | ||
| Blade plate | 3/4 (75) | ||
| External fixation | 2/2 (100) | ||
| Other | 1/1 (100) | ||
| Type III | Allograft | 9/10 (90) | |
| Revision arthroplasty | 4/5 (80) | ||
| AO/OTA | 33A1 | Locking plate | 3/3 (100) |
| Blade plate | 1/1 (100) | ||
| Revision arthroplasty | 1/1 (100) | ||
| 33A2 | Locking plate | 8/8 (100) | |
| Blade plate | 7/7 (100) | ||
| Revision arthroplasty | 1/1 (100) | ||
| 33A3 | Locking plate | 10/13 (77) | |
| Blade plate | 12/13 (92) | ||
| Revision arthroplasty | 1/1 (100) | ||
| 33B2 | Revision arthroplasty | 2/2 (100) | |
| 33C2 | Revision arthroplasty | 1/1 (100) | |
| Su | Type III | Other | 10/10 (100) |
| Backstein | F2 | Allograft | 6/7 (86) |
| Other | 16/16 (100) | ||
| Neer | Type II | Locking plate | 7/7 (100) |
| Intramedullary nail/rod | 5/6 (83) | ||
| Type III | Intramedullary nail/rod | 1/1 (100) | |
| Type IIII | Locking plate | 2/2 (100) | |
| Kim | Type III | Other | 18/18 (100) |
AO/OTA, Association for Osteosynthesis/Orthopedic Trauma Association.
The complications of the 448 fractures are reported in Table 4. The most frequent complications were non/mal/delayed union and revision, with 61 and 63 instances of each, respectively. The largest sample sizes were of Rorabeck type II fractures with a locking plate and Rorabeck type II fractures treated with an intramedullary nail/rod. Fractures treated with a locking plate had a complication rate of 35% and fractures treated with an intramedullary nail/rod had a complication rate of 53%.
Table 4.
Complications (n)
| Classification | Subclassification | Method | Fractures | Complications | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Infection | Hardware/implant failure | Non/mal/delayed union | Revision | Bone grafting | Other | Total (%) | ||||
| Rorabeck | Type I | Locking plate | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) |
| Screw | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | ||
| External fixation | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 (100) | ||
| Non‐operative | 3 | 0 | 0 | 2 | 0 | 0 | 0 | 2 (67) | ||
| Type II | Locking plate | 169 | 7 | 2 | 23 | 12 | 7 | 8 | 59 (35) | |
| Non‐locking plate | 26 | 1 | 1 | 10 | 8 | 4 | 6 | 30 (115) | ||
| Intramedullary nail/rod | 98 | 1 | 6 | 19 | 21 | 1 | 4 | 52 (53) | ||
| Screw | 10 | 0 | 0 | 3 | 3 | 1 | 0 | 7 (70) | ||
| Blade plate | 4 | 1 | 0 | 0 | 0 | 0 | 1 | 2 (50) | ||
| External fixation | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 1 (50) | ||
| Other | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | ||
| Type III | Allograft | 10 | 1 | 0 | 1 | 3 | 1 | 1 | 7 (70) | |
| Revision arthroplasty | 3 | 0 | 0 | 1 | 0 | 0 | 0 | 1 (33) | ||
| AO/OTA | 33A1 | Locking plate | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) |
| Blade plate | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | ||
| Revision arthroplasty | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | ||
| 33A2 | Locking plate | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | |
| Blade plate | 7 | 0 | 0 | 0 | 1 | 0 | 0 | 1 (14) | ||
| Revision arthroplasty | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | ||
| 33A3 | Locking plate | 13 | 2 | 4 | 1 | 0 | 0 | 4 | 11 (85) | |
| Blade plate | 13 | 1 | 1 | 0 | 2 | 5 | 2 | 11 (85) | ||
| Revision arthroplasty | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | ||
| 33B2 | Revision arthroplasty | 2 | 0 | 0 | 0 | 0 | 0 | 1 | 1 (50) | |
| 33C2 | Revision arthroplasty | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | |
| Su | Type III | Other | 10 | 2 | 0 | 0 | 0 | 0 | 4 | 6 (60) |
| Backstein | F2 | Allograft | 7 | 1 | 0 | 1 | 1 | 0 | 0 | 3 (43) |
| Other | 16 | 2 | 0 | 0 | 2 | 0 | 1 | 5 (31) | ||
| Neer | Type II | Locking plate | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) |
| Intramedullary nail/rod | 6 | 0 | 0 | 0 | 0 | 0 | 1 | 1 (17) | ||
| Type III | Intramedullary nail/rod | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | |
| Type IIII | Locking plate | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 (0) | |
| Kim | Type III | Other | 18 | 0 | 0 | 0 | 10 | 0 | 0 | 10 (56) |
| Total | 448 | 21 | 14 | 61 | 63 | 19 | 33 | 211 (47) | ||
AO/OTA, Association for Osteosynthesis/Orthopedic Trauma Association.
Discussion
Several treatment methods, both conservative and surgical, are currently used to treat periprosthetic distal femur fractures after TKA. However, due to variations in individual patient health and distal femur fracture patterns, the optimal method of treatment remains controversial and no gold standard of treatment has been established. The current selection of treatment methods may not provide a one size fits all solution. Instead, treatment methods may show successful outcomes when coupled with a specific fracture pattern. Therefore, the major goal of this study was to identify the most successful treatment methods for specific fracture types by examining the past literature.
Distal femur fractures can be categorized by different systems that focus on different characteristics. In this study, the classification systems developed by Rorabeck and AO/OTA were used most frequently, with 390 fractures classified under the Rorabeck system and 330 classified under the AO/OTA system. The Rorabeck classification system emphasizes the stability of the knee prosthesis and the displacement of the fracture43. The AO/OTA classification system focuses on the location of the fracture on the distal femur and the complexity of the fracture pattern44. The most common subclassification was Rorabeck type II, with 363 fractures. A Rorabeck type II fracture is labeled as a displaced fracture with a stable prosthesis43.
The popularity of the Rorabeck and AO/OTA systems may lie in their concision and simplicity, although the Rorabeck system may predominate because it includes prosthesis stability. The other classification systems used in the selected literature focused on features such as bone amount, bone quality, and reducibility. While these are important factors to consider when treating fractures, these systems do not emphasize the fracture's displacement or pattern, which may limit their widespread use. A classification system that encompasses all these features may be beneficial. Creating a system to include key features, such as fracture displacement and pattern, as well as other supporting features, may provide detailed classifications that can match each patient's unique condition. Therefore, instead of a universal treatment method, different methods that treat different clasees of fracture may be more effective.
Locked plating and intramedullary nailing are currently the most common methods of treatment, as reflected in this study, due to their minimally invasive surgical technique. Rorabeck type II fractures treated with a locking plate or intramedullary nail/rod had similarly successfully healing rates of 87% and 84%, respectively. Nine articles, totaling 461 fractures, in our study directly compared locked plating and intramedullary nailing. Five articles found no overall advantage to either method, while three articles supported locked plating and one article favored nailing5, 7, 13, 16, 19, 20, 30, 35, 41.
Although the healing rate for Rorabeck type II fractures between locked plating and the intramedullary nail/rod was similar, the complication rates differed. The complication rate for the intramedullary nail/rod was 18% higher than for locked plating. The two most frequent complications were non/mal/delayed union and revision, which seems reasonable as revision usually follows a malunion or nonunion.
There were several limitations to this study. Since data from 41 articles were compiled there was a lack of consistent standards from study to study. This included different brands of equipment being used, fracture classifications judged by different people, and different definitions of medical terms. In addition, each article was retrospective in nature and most lacked a control group. This study's detailed breakdown of each fracture resulted in small sample sizes for most of the groups in the classification and subclassification types. Additionally, the lack of comprehensive data for each fracture limited our sample sizes.
Conclusion
The most frequent type of periprosthetic distal femur fracture after TKA is Rorabeck type II. The most common treatments for these types of fractures are locked plating and intramedullary nailing, with similar healing rates of 87 and 84%, respectively. However, the complication rate for locked plating was lower than for intramedullary nailing.
Disclosure: The authors declare no conflicts of interest. No benefits in any form have been, or will be, received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1. Agarwal S, Sharma RK, Jain JK. Periprosthetic fractures after total knee arthroplasty. J Orthop Surg, 2014, 22: 24–29. [DOI] [PubMed] [Google Scholar]
- 2. Herrera DA, Kregor PJ, Cole PA, Levy BA, Jonsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981–2006). Acta Orthop, 2008, 79: 22–27. [DOI] [PubMed] [Google Scholar]
- 3. Ha CW, Shon OJ, Lim SW, Park KH. Minimally invasive plate osteosynthesis for periprosthetic distal femoral fractures after total knee arthroplasty. Knee Surg Relat Res, 2014, 26: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jassim SS, McNamara I, Hopgood P. Distal femoral replacement in periprosthetic fracture around total knee arthroplasty. Injury, 2014, 45: 550–553. [DOI] [PubMed] [Google Scholar]
- 5. Gondalia V, Choi DH, Lee SC, et al Periprosthetic supracondylar femoral fractures following total knee arthroplasty: clinical comparison and related complications of the femur plate system and retrograde‐inserted supracondylar nail. J Orthop Traumatol, 2014, 15: 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saidi K, Ben‐Lulu O, Tsuji M, Safir O, Gross AE, Backstein D. A comparison of treatment using allograft‐implant composites, standard revision components, distal femoral replacements prosthesis. J Arthroplasty, 2014, 29: 110–114. [DOI] [PubMed] [Google Scholar]
- 7. Meneghini RM, Keyes BJ, Reddy KK, Maar DC. Modern retrograde intramedullary nails versus periarticular locked plates for supracondylar femur fractures after total knee arthroplasty. J Arthroplasty, 2014, 29: 1478–1481. [DOI] [PubMed] [Google Scholar]
- 8. Lee SS, Lim SJ, Moon YW, Seo JG. Outcomes of long retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty. Arch Orthop Trauma Surg, 2014, 134: 47–52. [DOI] [PubMed] [Google Scholar]
- 9. Chen AF, Choi LE, Colman MW, et al Primary versus secondary distal femoral arthroplasty for treatment of total knee arthroplasty periprosthetic femur fractures. J Arthroplasty, 2013, 28: 1580–1584. [DOI] [PubMed] [Google Scholar]
- 10. Singh SP, Bhalodiya HP. Outcome and incidence of periprosthetic supracondylar femoral fracture in TKA. Indian J Orthop, 2013, 47: 591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ries ZG, Marsh JL. Far cortical locking technology for fixation of periprosthetic distal femur fractures: a surgical technique. J Knee Surg, 2013, 26: 15–18. [DOI] [PubMed] [Google Scholar]
- 12. Lizaur‐Utrilla A, Miralles‐Munoz FA, Sanz‐Reig JS. Functional outcome of total knee arthroplasty after periprosthetic distal femoral fracture. J Arthroplasty, 2013, 28: 1585–1588. [DOI] [PubMed] [Google Scholar]
- 13. Kilicoglu OI, Akgul T, Saglam Y, Yazicioglu O. Comparison of locked plating and intramedullary nailing for periprosthetic supracondylar femur fractures after knee arthroplasty. Acta Orthop Belg, 2013, 79: 417–421. [PubMed] [Google Scholar]
- 14. Ozcan O, Boya H, Ates A, Dogruoz F. Bilateral periprosthetic distal femoral fractures following total knee arthroplasty. Eklem Hastalik Cerrahisi, 2013, 24: 178–181. [DOI] [PubMed] [Google Scholar]
- 15. Ries Z, Hansen K, Bottlang M, Madey S, Fitzpatrick D, Marsh JL. Healing results of periprosthetic distal femur fractures treated with far cortical locking technology: a preliminary retrospective study. Iowa Orthop J, 2013, 33: 7–11. [PMC free article] [PubMed] [Google Scholar]
- 16. Aldrian S, Schuster R, Haas N, et al Fixation of supracondylar femoral fractures following total knee arthroplasty: is there any difference comparing angular stable plate fixation versus rigid interlocking nail fixation? Arch Orthop Trauma Surg, 2013, 133: 921–927. [DOI] [PubMed] [Google Scholar]
- 17. Bae DK, Song SJ, Yoon KH, Kim TY. Periprosthetic supracondylar femoral fractures above total knee arthroplasty: comparison of the locking and non‐locking plating methods. Knee Surg Sports Traumatol Arthrosc, 2014, 22: 2690–2697. [DOI] [PubMed] [Google Scholar]
- 18. Gavaskar AS, Tummala NC, Subramanian M. The outcome and complications of the locked plating management for the periprosthetic distal femur fractures after a total knee arthroplasty. Clin Orthop Surg, 2013, 5: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Horneff JG III, Scolaro JA, Jafari SM, Mirza A, Parvizi J, Mehta S. Intramedullary nailing versus locked plate for treating supracondylar periprosthetic femur fractures. Orthopedics, 2013, 36: e561–e566. [DOI] [PubMed] [Google Scholar]
- 20. Hou Z, Bown TR, Irgit K, et al Locked plating of periprosthetic femur fractures above total knee arthroplasty. J Orthop Trauma, 2012, 26: 427–432. [DOI] [PubMed] [Google Scholar]
- 21. Jeavons RP, Dowen D, O'Brien S. The use of a revision femoral stem to manage a distal femoral periprosthetic fracture in a well‐fixed total knee arthroplasty. J Arthroplasty, 2012, 27: 156–159. [DOI] [PubMed] [Google Scholar]
- 22. Hoffmann MF, Jones CB, Sietsema DL, Koenig SJ, Tornetta P III. Outcome of periprosthetic distal femoral fractures following knee arthroplasty. Injury, 2012, 43: 1084–1089. [DOI] [PubMed] [Google Scholar]
- 23. Ebraheim NA, Liu J, Hashmi SZ, Sochacki KR, Moral MZ, Hirschfeld AG. High complication rate in locking plate fixation of lower periprosthetic distal femur fractures in patients with total knee arthroplasties. J Arthroplasty, 2012, 27: 809–813. [DOI] [PubMed] [Google Scholar]
- 24. Pot JH, van Heerwaarden RJ, Patt TW. An unusual way of intramedullar fixation after a periprosthetic supracondylar femur fracture. J Arthroplasty, 2012, 27: 494.e5–494.e8. [DOI] [PubMed] [Google Scholar]
- 25. Vallier HA, Immler W. Comparison of the 95‐degree angled blade plate and the locking condylar plate for the treatment of distal femoral fractures. J Orthop Trauma, 2012, 26: 327–333. [DOI] [PubMed] [Google Scholar]
- 26. Ehlinger M, Adam P, Abane L, et al Treatment of periprosthetic femoral fractures of the knee. Knee Surg Sports Traumatol Arthrosc, 2011, 19: 1473–1478. [DOI] [PubMed] [Google Scholar]
- 27. Streubel PN, Gardner MJ, Morshed S, Collinge CA, Gallagher B, Ricci WM. Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? J Bone Joint Surg Br, 2010, 92: 527–534. [DOI] [PubMed] [Google Scholar]
- 28. Mortazavi SMJ, Kurd MF, Bender B, Post Z, Parvizi J, Purtill JJ. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty, 2010, 25: 775–780. [DOI] [PubMed] [Google Scholar]
- 29. Beris AE, Lykissas MG, Sioros V, Mavrodontidis AN, Korompilias AV. Femoral periprosthetic fracture in osteoporotic bone after a total knee replacement: treatment with Ilizarov external fixation. J Arthroplasty, 2010, 25: 1168.e9–1168.e12. [DOI] [PubMed] [Google Scholar]
- 30. Platzer P, Schuster R, Aldrian S, et al Management and outcome of periprosthetic fracture after total knee arthroplasty. J Trauma, 2010, 68: 1464–1470. [DOI] [PubMed] [Google Scholar]
- 31. Han HS, Oh KW, Kang SB. Retrograde intramedullary nailing for periprosthetic supracondylar fractures of the femur after total knee arthroplasty. Clin Orthop Surg, 2009, 1: 201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kolb K, Koller H, Lorenz I, et al Operative treatment of distal femoral fractures above total knee arthroplasty with the indirect reduction technique: a long‐term follow‐up study. Injury, 2009, 40: 433–439. [DOI] [PubMed] [Google Scholar]
- 33. Norrish AR, Jibri ZA, Hopgood P. The LISS plate treatment of supracondylar fractures above a total knee replacement: a case‐control study. Acta Orthop Belg, 2009, 75: 642–648. [PubMed] [Google Scholar]
- 34. Chettiar K, Jackson MP, Brewin J, Dass D, Butler‐Manuel PA. Supracondylar periprosthetic femoral fractures following total knee arthroplasty: treatment with a retrograde intramedullary nail. Int Orthop, 2009, 33: 981–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Large TM, Kellam JF, Bosse MJ, Sims SH, Althausen P, Masonis JL. Locked plating of supracondylar periprosthetic femur fractures. J Arthroplasty, 2008, 23: 115–120. [DOI] [PubMed] [Google Scholar]
- 36. Fulkerson E, Tejwani N, Stuchin S, Egol K. Management of periprosthetic femur fractures with a first generation locking plate. Injury, 2007, 38: 965–972. [DOI] [PubMed] [Google Scholar]
- 37. Ricci WM, Loftus T, Cox C, Borrelli J. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma, 2006, 20: 190–196. [DOI] [PubMed] [Google Scholar]
- 38. Hurson C, Synnott K, McCormack D. Above‐knee Ilizarov external fixation for early periprosthetic supracondylar femoral fracture—a case report. Knee, 2005, 12: 145–147. [DOI] [PubMed] [Google Scholar]
- 39. Srinivasan K, Macdonald DA, Tzioupis CC, Giannoudis PV. Role of long stem revision knee prosthesis in periprosthetic and complex distal femoral fractures: a review of eight patients. Injury, 2005, 36: 1094–1102. [DOI] [PubMed] [Google Scholar]
- 40. Gliatis J, Megas P, Panagiotopoulos E, Lambiris E. Midterm results of treatment with a retrograde nail for supracondylar periprosthetic fractures of the femur following total knee arthroplasty. J Orthop Trauma, 2005, 19: 164–170. [DOI] [PubMed] [Google Scholar]
- 41. Bezwada HP, Neubauer P, Baker J, Israelite CL, Johanson NA. Periprosthetic supracondylar femur fractures following total knee arthroplasty. J Arthroplasty, 2004, 19: 453–458. [DOI] [PubMed] [Google Scholar]
- 42. Kassab M, Zalzal P, Azores GMS, Pressman A, Liberman B, Gross AE. Management of periprosthetic femoral fractures after total knee arthroplasty using a distal femoral allograft. J Arthroplasty, 2004, 19: 361–368. [DOI] [PubMed] [Google Scholar]
- 43. Rorabeck CH, Taylor JW. Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin North Am, 1999, 30: 265–277. [DOI] [PubMed] [Google Scholar]
- 44. Marsh JL, Slongo TF, Agel J, et al Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma, 2007, 21 (10 Suppl.): S1–S161. [DOI] [PubMed] [Google Scholar]
- 45. Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthrop Surg, 2004, 12: 12–20. [DOI] [PubMed] [Google Scholar]
- 46. Kim K, Egol KA, Hozack WJ, Parvizi J. Periprosthetic fractures after total knee arthroplasties. Clin Orthop Relat Res, 2006, 446: 167–175. [DOI] [PubMed] [Google Scholar]
- 47. Neer CS II, Grantham SA, Shelton ML. Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am, 1967, 49: 591–613. [PubMed] [Google Scholar]
- 48. Backstein D, Safir O, Gross A. Periprosthetic fractures of the knee. J Arthroplasty, 2007, 22: 45–49. [DOI] [PubMed] [Google Scholar]
- 49. Tricoire JL, Vogt F, Laffosse JM. Periprosthetic fractures around total hip and knee arthroplasty. Radiographic evaluation in periprosthetic fractures around the knee. Rev Chir Orthop, 2006, 92 (5 Suppl.): S57–S60. [PubMed] [Google Scholar]


