Abstract
Objective
Unilateral hemilaminectomy (UHIL), an alternative surgical approach to intradural lesions, involves a unilateral approach to meningeal opening that provides an adequate window for tumor extraction while leaving most of the vertebral structures intact. The techniques and results of a modified hemilaminectomy technique with spinal endoscopy is discussed and limited unilateral hemilaminectomy for intradural tumors (UHIT) evaluated prospectively.
Methods
Relevant clinical variables, operative reports, histological findings, pre‐ and post‐operative imaging, and follow‐up data for 11 consecutive patients (five males, six females; mean age 63.36 ± 20.69 years) who underwent modified hemilaminectomy over a 3 year time period were analyzed. Contrast‐enhanced MRI was used to demonstrate the side, size and location of the suspected tumor or intradural lesion and CT to evaluate the bone anatomy. Post‐operative MRI and CT allowed evaluation of anatomy following resection.
Results
Lesions included meningiomas (n = 2), neuromas (n = 3), and metastases, cysts or gliomas (n = 6). Pre‐operative indications in order of incidence included cord compression, claudication, lower back pain, radiculopathy, paraplegia, weakness, incontinence, and generalized neuro‐deterioration. There were no major complications, and no spinal deformity or instability at final follow up (mean, 13 months; range, 3–36 months).
Conclusion
Our data suggest that there is a place for the UHIT approach. This minimally invasive approach is useful for resecting all intradural tumors. UHIL is a useful minimally invasive technique for resecting intradural spinal tumors with maximal preservation of musculoligamentous attachments and posterior bony elements and should be considered an improvement on currently employed techniques.
Keywords: Arachnoid cyst, Hemilaminectomy, Intradural tumor, Technique
Introduction
Spinal tumors occur rarely, the global incidence reportedly being in the range of 1–2.5 per 100,000 people1, 2, 3, 4. Laminectomy, which facilitates access and visualization, has traditionally been the most common approach for access to intradural spinal cord lesions and tumors. However other approaches, including laminotomy, hemilaminectomy and inter‐laminar fenestration, have also been reported. While complete resection is desirable, the strongest predictors of surgical outcomes are pre‐morbid, pre‐operative and post‐operative general clinical status, tumor grading and location5. Previous reports also suggest that the best overall neurological improvements occur in the patients with the most precise surgical plans, suggesting a key role for investigative imaging such as CT and MRI in preoperative planning in such cases6.
Currently, the major goals of surgical procedures for intradural lesions include: (i) complete, pathologically confirmed resection/removal of the intraspinal lesion/tumor; (ii) minimizing invasiveness and risk management; and (iii) limiting iatrogenic trauma and post‐operative complications. Unilateral hemilaminectomy (UHIL) is an alternative surgical approach to intradural lesions that was first described by Yasargil in 1991; it involves a unilateral approach to meningeal opening, thus providing an adequate window for tumor resection while leaving most of the vertebral structures intact7. Because few published articles have described advances of hemilaminectomy in the last decade and there have been no large‐scale prospective studies, there is a need to re‐evaluate and standardize operating methodology8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18. Biomechanical data from multiple studies have demonstrated that UHIL is superior to laminectomy in preservation of joint integrity and reducing postoperative complications19, 20. Furthermore, many studies have demonstrated a strong association between standard laminectomy and post‐operative complications; namely, spinal deformity and damage to dissected structures during the approach. This relationship is particularly strong in pediatric subjects12, 17, 18. In this clinical article, we present the operative techniques for UHIL and an evaluation of the effectiveness of this approach through analysis of a consecutive case series.
Patients and Methods
The study protocol was approved by the Northern Hospital Network Human Research Ethics Committee. From January 2007 to November 2012, microsurgical unilateral hemilaminectomies were performed by the senior author (RJM) on 11 consecutive patients with intradural tumors (UHITs). Clinical variables, operative reports, histological findings, pre‐ and post‐operative images, and follow‐up information were reviewed21.
Contrast‐enhanced MRIs were performed to demonstrate the side, size and location of the suspected tumor or intradural lesion and pre‐operative CTs to evaluate the bone anatomy and thus assess the surgical corridor. Post‐operative imaging included an MRI and CT to show the extent of the bone window, thus allowing evaluation of post‐resection anatomy.
The treatment of choice for resection of intradural tumors is considered UHIL7; however, the standard procedure was modified in the present study (Fig. 1). Following assessment of relevant investigative imaging modalities, including CT and MRI, general anesthesia induced and the patient placed in a prone position on the operating table. A decision was then made on the approach side for performing the hemilaminectomy that would provide the best access, this decision being based on a number of factors, including the side of the canal predominantly occupied by the lesion or tumor and the angulation of the spinous processes. In some cases, the patient was rolled slightly to the contralateral side to facilitate ease of access to the canal. Hemilaminectomy was performed using a combination of a high speed drill with 2 mm and 3 mm round burrs, followed by Kerrison rongeur removal of additional bone to create an adequate surgical corridor. Subsequently, the dura was opened to maximize access to the lesion or tumor. Micro‐neurosurgical techniques were used to remove the lesion or tumor (Fig. 2). For visualization superior or inferior to the surgical space, an endoscope was sometimes introduced into the canal (Fig. 3). Following lesion or tumor resection, closure was performed in the standard fashion (Video S1). It is important to note that if the window achieved after lamina removal is inadequate for extraction, various structures, including the base of the spinous process and articulating processes of the nearby pedicle may have to be removed. In contrast, only partial removal is required in patients with thick laminae.
Figure 1.
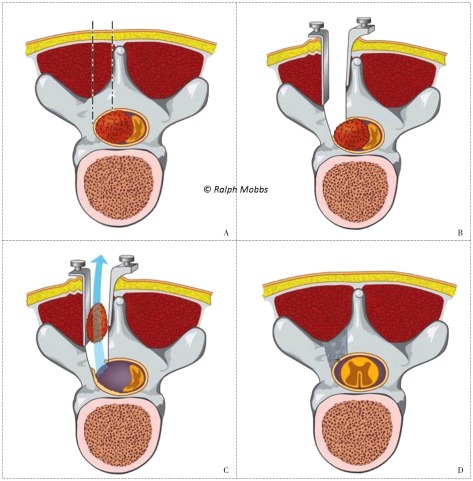
Surgical workflow for UHIL. (A) Surgical planning and confirmation of correct level. (B) Hemilaminectomy and dural opening to reveal pathology. (C) Surgical resection through the unilateral exposure. (D) Closure with dural suture, return of unilateral muscle retraction to the midline and standard wound closure.
Figure 2.
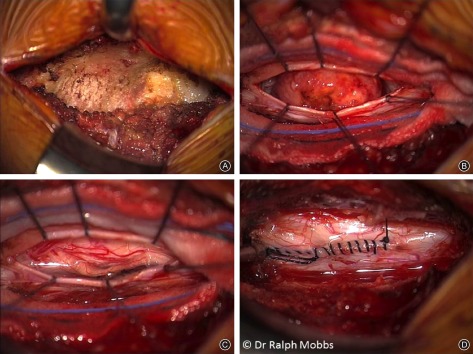
Intraoperative surgical workflow for UHIL. (A) Incision and unilateral lamina/spinous process exposure. (B) Dural incision and exposure of pathology. (C) Resection of lesion with identification of spinal cord/nerve roots. (D) Dural closure.
Figure 3.
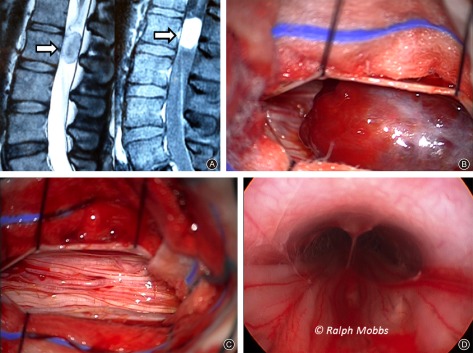
Intradural endoscopy. (A) CT image showing large intradural lesion. (B) Dural exposure and identification of pathology. (C) Removal of lesion. (D) Endoscopy to confirm intradural clearance proximal and distal to dural exposure.
Results
Patient Variables
Of the 11 study patients, five were male and six female. Their mean age was 63.36 ± 20.69 years. Nine tumors were removed and two arachnoid cysts fenestrated. Two of the tumors were metastases, one from an osteosarcoma and the other a melanoma. Pre‐operative indications in order of incidence included: cord compression, claudication, lower back pain, radiculopathy, paraplegia, weakness, incontinence and generalized neurological deterioration. No patients had contraindications to surgical intervention. The locations and histopathology of the lesions are shown in Table 1. The mean follow‐up time was 13 months (range, 3–36 months).
Table 1.
Location and histopathology of lesions (cases)
| Level of lesion | Type of lesion | Total | ||
|---|---|---|---|---|
| Meningioma | Neuroma | Other* | ||
| Cervical | — | — | 1 | 1 |
| Thoracic | 2 | — | 2 | 4 |
| Lumbosacral | — | 3 | 3 | 6 |
| Total | 2 | 3 | 6 | 11 |
*Metastases, cysts, and glioma.
Peri‐Operative and Follow‐Up Findings
Using our modified UHIL technique, no major complications occurred in any of the study patients observed. Specifically, there were no instances of damage to the spinal cord or vertebral artery. In one case, two nerves entering the lesion had to be slowly dissected. No patients had radiological evidence of instability or spinal deformity. All 11 patients demonstrated physical improvement at latest follow‐up.
Discussion
While the increasing implementation of minimally invasive surgical techniques globally over the past decades has reflected the importance of reducing surgical trauma, there is no clinically robust clinical evidence for minimally invasive surgery for spinal lesions or tumors22, 23, 24. No randomized controlled trials comparing procedures have been published; the nature of these lesions would make such a study difficult to coordinate regardless of whether it was in a single center or multi‐institutional setting. To our knowledge, this is the first published Australian series reporting the use of UHIT as a minimally invasive endoscopic option for intradural lesions and tumors.
Given the minimally invasive nature of UHIT, which preserves the mechanically relevant bone structures and facet joints17, there may be a smaller incidence of spinal instability following this procedure than after complete laminectomy and laminotomy. According to Iacoangeli et al., a posterior approach is the safest of all methods when indicated; these authors advise posterior UHIL in all elderly patients with intradural lesions, regardless of how ventral the pathology lies25. Sun et al. describe a potential use for UHIL in all lateral intradural lesions regardless of how ventral or lateral they sit; our dataset, although small, supports their proposal18.
In addition, multiple studies have demonstrated that the minimal invasiveness of UHIL yields reductions in both operating time and blood loss15, 16. In accordance with this, patients who have undergone UHIL may have rapid recoveries and rehabilitation with little to no complications18. All of these considerations, in addition to its superior stability, support use of the modified technique described here. Importantly, although our study did not directly compare the outcomes of different techniques, our outcomes were directly comparable with those of previous studies in terms of tumor recurrence, complication rate and physical recovery.
Biomechanical data further justifies the minimally invasive hemilaminectomy approach because it achieves superior structural integrity across all lumbar levels compared with traditional laminectomy. Finite element model experiments have demonstrated a greater degree of flexion and less annular stress associated with minimally invasive surgical techniques, likely leading to reduction in post‐operative disc degeneration19. In addition, as demonstrated by Ogden et al., there is a strong correlation between the overall extent of removal of posterior elements and vertebral mobility during axial loading20.
Technical Requirements of the Limited Approach
Effective imaging evaluation and localization are imperative prerequisites for obtaining ideal outcomes. In our 11 cases, level and lesion localization was determined pre‐operatively by CT and MRI imaging. Additionally, the surgical planes were verified intra‐operatively by X‐raying the levels surrounding the lesions.
In accordance with the principles of minimally invasive approaches, the windows of approach were restricted where possible as defined in the Patients and Methods section. When a wider corridor of approach was required, adjacent structures, including the base of the spinous process, articulating portions of the pedicles and surrounding spinous ligaments (interspinous, supraspinous and the ligamentum flavum), were removed Careful removal of these structures is essential to prevent associated complications and damage to surrounding adjacent spinal roots, meningeal damage and leakage of cerebrospinal fluid12, 14. These complications must also be avoided during the repositioning and closure of the site. Though it requires some flexibility on the surgeon's part, similar modified hemilaminectomies have been employed in other studies17, 18. With suitable experience in microscopic and endoscopic surgical techniques, we believe that the UHIL approach can be successfully applied with minimal complications, as demonstrated in the present study; however, larger prospective studies are required to validate our findings. Similarly positive results have also been reported for a Japanese study that found no statistically significant deterioration across a 10‐year period26. However, UHIL is inappropriate for some lesions, including bilateral extradural lesions, large lesions with vertebral scalloping and lesions with unclear borders25. There may also be concerns in young patients with intramedullary tumors in the cervical and lumbar spine, in whom surgical intervention may lead to postoperative deformity and spinal instability.
Importantly, the inclusion of a further sub‐specialized technique in the form of multilevel inter‐laminar fenestration methodology should be considered when the required expertise is available. Such methods have demonstrated positive outcomes. However, apart from a large cohort study by Koch et al. and some single case reports, little data is available on the efficacy of this procedure and how it compares with other modes of lesion resection23, 24.
Limitations of the present study include the lack of postoperative neurological outcomes. Given that internal fixation is not necessary with hemilaminectomy, whereas it is with laminectomy, it is difficult to make definitive conclusions comparing the flexion achieved by either technique based on the present results. The present case series is also limited by its small size27, 28, comprising only five pathological types with short follow‐up, these factors prevent making more definitive conclusions. However, we have demonstrated that the minimally invasive approach can be useful for resecting different types of intradural lesions, regardless of subtype.
Conclusions
In this study, we evaluated the place of UHIL in resecting spinal intradural lesions. Despite the small numbers necessitated by the relatively low incidence of such lesions, our surgical experiences and results suggest that there is a place for such an approach. The diversity in our sample indicates that a minimally invasive approach is useful for resecting all intradural lesions, regardless of histological subtype. Through superior preservation of spinal structures compared with conventional approaches, we have been able to achieve acceptable results and would recommend such a procedure by qualified and experienced surgeons in appropriately selected patients.
Supporting information
Video S1 Unilateral hemilaminectomy.
Disclosure: No funds were received in support of this work.
References
- 1. Elia‐Pasquet S, Provost D, Jaffré A, et al Incidence of central nervous system tumors in Gironde, France. Neuroepidemiology, 2004, 23: 110–117. [DOI] [PubMed] [Google Scholar]
- 2. Liigant A, Asser T, Kulla A, Kaasik AE. Epidemiology of primary central nervous system tumors in Estonia. Neuroepidemiology, 2000, 19: 300–311. [DOI] [PubMed] [Google Scholar]
- 3. Schellinger KA, Propp JM, Villano JL, McCarthy BJ. Descriptive epidemiology of primary spinal cord tumors. J Neurooncol, 2008, 87: 173–179. [DOI] [PubMed] [Google Scholar]
- 4. Duong LM, McCarthy BJ, McLendon RE, et al . Descriptive epidemiology of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors, United States, 2004–2007. Cancer, 2012, 118: 4220–4227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nambiar M, Kavar B. Clinical presentation and outcome of patients with intradural spinal cord tumours. J Clin Neurosci, 2012, 19: 262–266. [DOI] [PubMed] [Google Scholar]
- 6. Garcés‐Ambrossi GL, McGirt MJ, Mehta VA, et al Factors associated with progression‐free survival and long‐term neurological outcome after resection of intramedullary spinal cord tumors: analysis of 101 consecutive cases. J Neurosurg Spine, 2009, 11: 591–599. [DOI] [PubMed] [Google Scholar]
- 7. Yasargil MG, Tranmer BI, Adamson TE, Roth P. Unilateral partial hemilaminectomy for the removal of extra‐ and intramedullary tumors and AVMs. Adv Tech Stand Neurosurg. 1991; 113–132. [DOI] [PubMed] [Google Scholar]
- 8. Liu K, Shi J, Jia L, Yuan W. Surgical technique: hemilaminectomy and unilateral lateral mass fixation for cervical ossification of the posterior longitudinal ligament. Clin Orthop Relat Res, 2013, 471: 2219–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Canbay S, Hasturk AE, Basmaci M, Erten F, Harman F. Management of thoracal and lumbar Schwannomas using a unilateral approach without instability: an analysis of 15 cases. Asian Spine J, 2012, 6: 43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. González‐Martínez EL, García‐Cosamalón PJ, Fernández‐Fernández JJ, Ibáñez‐Plágaro FJ, Alvarez B. Minimally invasive approach of extramedullary intradural spinal tumours. Review of 30 cases. Neurocirugia (Astur), 2012, 23: 175–181. [DOI] [PubMed] [Google Scholar]
- 11. Dahlberg D, Halvorsen CM, Lied B, Helseth E. Minimally invasive microsurgical resection of primary, intradural spinal tumours using a tubular retraction system. Br J Neurosurg, 2012, 26: 472–475. [DOI] [PubMed] [Google Scholar]
- 12. Balak N. Unilateral partial hemilaminectomy in the removal of a large spinal ependymoma. Spine J, 2008, 8: 1030–1036. [DOI] [PubMed] [Google Scholar]
- 13. Boström A, Bürgel U, Reinacher P, et al A less invasive surgical concept for the resection of spinal meningiomas. Acta Neurochir (Wien), 2008, 150: 551–556. [DOI] [PubMed] [Google Scholar]
- 14. Chiou SM, Eggert HR, Laborde G, Seeger W. Microsurgical unilateral approaches for spinal tumour surgery: eight years' experience in 256 primary operated patients. Acta Neurochir (Wien), 1989, 100: 127–133. [DOI] [PubMed] [Google Scholar]
- 15. Iacoangeli M, Gladi M, Di Rienzo A, et al Minimally invasive surgery for benign intradural extramedullary spinal meningiomas: experience of a single institution in a cohort of elderly patients and review of the literature. Clin Interv Aging, 2012, 7: 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tredway TL, Santiago P, Hrubes MR, Song JK, Christie SD, Fessler RG. Minimally invasive resection of intradural‐extramedullary spinal neoplasms. Neurosurgery, 2006, 58 (1 Suppl.): ONS52‐8. discussion ONS52‐8. [DOI] [PubMed] [Google Scholar]
- 17. Oktem IS, Akdemir H, Kurtsoy A, Koç RK, Menkü A, Tucer B. Hemilaminectomy for the removal of the spinal lesions. Spinal Cord, 2000, 38: 92–96. [DOI] [PubMed] [Google Scholar]
- 18. Sun CX, Meng XL, Xie SN, Yu Y, Yang HJ, Wu B. Unilateral hemilaminectomy for patients with intradural extramedullary tumors. J Zhejiang Univ Sci B, 2011, 12: 575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xie T, Qian J, Lu Y, Chen B, Jiang Y, Luo C. Biomechanical comparison of laminectomy, hemilaminectomy and a new minimally invasive approach in the surgical treatment of multilevel cervical intradural tumour: a finite element analysis. Eur Spine J, 2013, 22: 2719–2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ogden AT, Bresnahan L, Smith JS, Natarajan R, Fessler RG. Biomechanical comparison of traditional and minimally invasive intradural tumor exposures using finite element analysis. Clin Biomech (Bristol, Avon), 2009, 24: 143–147. [DOI] [PubMed] [Google Scholar]
- 21. Frankel HL, Hancock DO, Hyslop G, et al The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia, 1969, 7: 179–192. [DOI] [PubMed] [Google Scholar]
- 22. Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion—systematic review and meta‐analysis. Br J Neurosurg, 2015, 12: 1–7. [DOI] [PubMed] [Google Scholar]
- 23. Koch‐Wiewrodt D, Wagner W, Perneczky A. Unilateral multilevel interlaminar fenestration instead of laminectomy or hemilaminectomy: an alternative surgical approach to intraspinal space‐occupying lesions. Technical note. J Neurosurg Spine, 2007, 6: 485–492. [DOI] [PubMed] [Google Scholar]
- 24. Xie T, Qian J, Wu X, Lu Y, Hu G, Luo C. Unilateral, multilevel, interlaminar fenestration in the removal of a multisegment cervical intramedullary ependymoma. Spine J, 2013, 13: 747–753. [DOI] [PubMed] [Google Scholar]
- 25. Iacoangeli M, Gladi M, Di Rienzo A, et al Minimally invasive surgery for benign intradural extramedullary spinal meningiomas: experience of a single institution in a cohort of elderly patients and review of the literature. Clin Interv Aging, 2012, 7: 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Naganawa T, Miyamoto K, Hosoe H, Suzuki N, Shimizu K. Hemilaminectomy for removal of extramedullary or extradural spinal cord tumors: medium to long‐term clinical outcomes. Yonsei Med J, 2011, 52: 121–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Phan K, Tian DH, Cao C, Black D, Yan TD. Systematic review and meta‐analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg, 2015, 4: 112–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Phan K, Mobbs RJ. Systematic reviews and meta‐analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg, 2015, doi: 10.3978/jss.2015.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1 Unilateral hemilaminectomy.


