Abstract
Background:
Staff nurse and infection preventionist (IP) workload increases in response to exposures and outbreaks. Understanding the time burden associated with responding to specific pathogens may improve resource allocation. The purpose of this study was to evaluate workload increases reported by nurses and IPs in response to common exposures and outbreaks.
Methods:
Surveys were distributed to nurses in a New York hospital network and to IPs who attended the 2018 Association for Professionals in Infection Control and Epidemiology annual conference or to IPs who were members of local Association for Professionals in Infection Control and Epidemiology chapters. Respondents were asked to rate their daily workload increase and to rank their most time-consuming activities in response to exposure and outbreak scenarios.
Results:
A total of 150 nurses and 228 IPs responded. Among the nurses, >60-minute workload increases were reported for Clostridium difficile (76%), lice or scabies (46%), and influenza (45%). Among the IPs, >60-minute increases were reported for mumps or measles (66%), tuberculosis (64%), and C difficile (50%). Among the nurses, isolation precautions, patient and family education, and staffing changes were the most frequently reported time-consuming activities. Among the IPs, chart review, exposure list compiling, and preventive measures for exposures were the most frequently reported time-consuming activities.
Conclusions:
Organisms that are easier to treat and more difficult to spread, such as scabies or lice, can contribute substantially to nursing workload. Notably, three-quarters of the nurses and one-half of the IPs reported that C difficile adds >1 hour to their daily workload.
Keywords: Infection control, Health care-associated infections, Nursing personnel, Inpatients, Isolation, Burnout
Nurses are on the frontline of preventing and controlling health care–associated infections (HAIs). Preventing such infections relies in part on adherence to the guidelines and protocols developed by organizations such as the Centers for Disease Control and Prevention and are supported by infection prevention and control personnel. Exposures to endemic and epidemic infectious agents may have a negative impact on staff as well as patients because the exposures often require additional time and resources from the health care team that may compromise their routine workflow and distract from other pressing needs.1–3
Although nursing staff are on the frontline of preventing and controlling HAIs, studies of the relationship between hospital systems of nursing care and risk of HAIs have been limited primarily to assessment of single factors such as staffing or adherence to specific evidence-based guidelines.4–6 However, there are numerous unit- and institutional-level factors that impinge on nursing practice, including the intensity of daily patient care demands and distractions associated with staffing, patient mix and acuity, and the need for isolation precautions and multiple patient admissions and discharges. System-level factors include the occurrence of emergencies and outbreaks associated with such organisms as norovirus, tuberculosis (TB), measles, or influenza as well as rare events, such as the previous Ebola “scare,” which divert staff time to emergent planning and response.2,7 Quantifying the added workload burden on nurses of these system-level factors is key to buttress the basics of infection prevention behaviors and to identify tipping points for preparedness.
Infection preventionists (IPs) are charged with the surveillance, detection, identification, prevention, and control of HAIs. Their expertise extends across numerous domains and competencies, including leadership and program management, performance improvement and implementation science, technical aspects, and infection prevention and control.8,9 IPs must balance the routine demands of their work with crisis management and untoward events such as exposures and outbreaks.10 Although IPs spend approximately 25% of their time in routine surveillance and investigation efforts, it is likely that this time would increase in the face of an outbreak or investigation of an exposure to an infectious disease.11 Quantifying the relative added workload burden of response to exposures and outbreaks is key to delegating resources to other important activities, such as prevention of surgical site and device-associated infections.
Assessing the potential impact on both the nurse and IP workload required to care for patients in an outbreak or exposure situation is important to help determine adequate staffing needs and resource allocation at the time of an exposure or outbreak. Unfortunately, the added workload associated with such events is unknown. Therefore, the purpose of this study was to assess the impact of exposure to infectious agents frequently encountered in the acute care setting on the workload of clinical nursing staff and infection prevention and control staff (ie, IPs). To our knowledge, this will be the first study to assess the perceptions of both IPs and nurses on workload required during an exposure or outbreak and to compare the responses between the 2 groups.
METHODS
Design
This was a descriptive cross-sectional survey approved by the Columbia University Irving Medical Center Human Institutional Review Board (AAAR5255).
Data collection
Convenience, nonrandomized sampling was used to distribute a 2-page survey to staff nurses and IPs. Staff nurses were recruited from 6 adult intensive care units in a large acute care hospital and from 2 pediatric medical surgical units in New York City. Research assistants distributed paper surveys to nurses during shift change. The single inclusion criterion was current employment as a registered nurse. Participants placed their completed surveys in a folder for privacy, and no identifying information was collected. The IPs were identified by the following 2 means: (1) membership in 2 regional chapters (New York and New Jersey) of the Association for Professionals in Infection Control and Epidemiology (APIC) and (2) attendance at the 2018 APIC national conference. For the chapter members, an electronic survey was sent via e-mail to all names in the membership database. The surveys were not linked to specific e-mails. Additionally, pen and paper surveys were distributed to attendees at a regularly scheduled meeting at each chapter. For the APIC conference, attendees were provided with a paper copy of the survey and invited to drop off the survey anonymously during the conference at a collection site. No identifying information was collected. For both methods of data collection, the single inclusion criterion was current employment in an IP capacity.
Measures
To develop the data collection instrument, key informants who are knowledgeable about infections most commonly encountered in the acute care setting (eg, hospital epidemiologists, nursing administrators and staff, and IPs) identified 5 prevalent categories of exposures that included lice or scabies, mumps or measles, pertussis, TB, and influenza and 5 categories of outbreaks that included methicillin-resistant Staphylococcus aureus (MRSA), other multidrug-resistant organisms (MDROs) (eg, vancomycin-resistant enterococci and multi-drug-resistant gram-negative bacteria), other respiratory viruses (eg, rhinovirus and adenovirus), Clostridium difficile, and gastrointestinal viruses (eg, norovirus and rotavirus).
To capture the relative increase in workload for each exposure, we asked the nurses and the IPs 2 questions. The first question asked the respondents to rank the overall increase in their daily workload for each of these exposures on a scale of 0–3, in which 0 = not applicable (no experience with the organism), 1 = increases workload minimally (<30 minutes of added work), 2 = increases workload moderately (approximately 30–60 minutes of added work), and 3 = increases workload dramatically (>60 minutes of added work).
In the second question, nurse respondents were asked to select the 3 most time-consuming activities for all outbreak and exposure incidents from the following 8 activities: (1) additional isolation precautions, which slow down patient care; (2) additional documentation in the electronic health record; (3) educating patients and families on outbreak or exposure precautions; (4) staffing changes because of either absent staff or cohorting patients; (5) requirement to take prophylactic medication (eg, azithromycin for pertussis); (6) visits to the workforce health and safety or occupational health department; (7) meeting or training with IPs; and (8) taking mandatory time off.
Similarly, IPs were asked to select the 3 most time-consuming activities for each outbreak or exposure from the following 10 activities: (1) case detection, (2) chart review, (3) ward rounding, (4) exposure list compilation, (5) staff and visitor notification, (6) family and patient education, (7) preventive measures for exposures, (8) documentation in the electronic health record, (9) reporting to regulatory authorities, and (10) reports to hospital supervisors.
Analyses
Survey data were analyzed using descriptive statistics (eg, frequencies, percentages, mean, and median) for characteristics of participating IPs and nurses and to identify the top 3 most time-consuming activities. The X2 test analyses were used to compare nurse and IP rankings. All statistical analyses were 2-sided, and P <.05 was considered statistically significant.
RESULTS
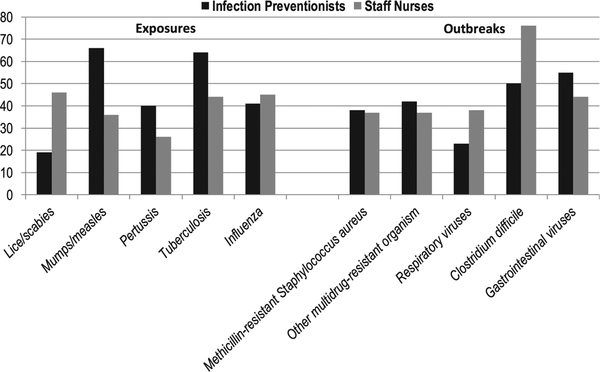
A total of 378 participants (150 staff nurses, 228 IPs) completed the survey (Table 1). Most of the IPs were also trained as nurses (80%). Most of the participants had >5 years of work experience (60% nurses, 68% IPs). Reported experience with each specific exposure or outbreak ranged from 43%−99% of the staff nurses and 71%−96% of the IPs. Of those with experience, there was a significant difference between nurses and IPs in the reported increase in workload for 8 of the 10 exposures or outbreaks (Fig 1 and Table 2).
Table 1.
Characteristics of participating IPs and staff nurses
| IPs | N (%) | Staff nurses | N (%) |
|---|---|---|---|
| Total respondents | 228 | Total respondents | 150 |
| Discipline* | Population | ||
| Nursing | 182(80) | Adult | 103(69) |
| Public health | 19(8) | Pediatric | 47(31) |
| Infection prevention | 19(8) | Inpatient unit | |
| Others | 24(11) | Intensive care | 110(73) |
| Current practice environment | Progressive care/medical surgical | 17(11) | |
| Acute care | 171(81) | Other | 21 (14) |
| Long-term care | 17(8) | Experience as registered nurse (y) | |
| Other | 24(11) | <1 | 5(3) |
| Worked as IP (y) | 1−3 | 31 (21) | |
| <1 | 8 (4) | >3−5 | 22 (15) |
| 1−3 | 30(13) | >5−10 | 42 (28) |
| >3−5 | 32(14) | >10 | 48 (32) |
| >5−10 | 40(18) | — | — |
| >10 | 113(50) | — | — |
NOTE. Percentages are calculated based on number of responses to each question. IP, infection preventionist.
Multiple responses permitted.
Fig 1.
Percent of infection preventionists and staff nurses reporting that exposure or outbreak adds >60 minutes to their daily workload.
Table 2.
Increased workload associated with exposures and outbreaks of organisms in health care settings reported by IPs and staff nurses
| IPs | Staff nurses | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N (%) reporting experience with pathogen | <30 min | 30–60 min | >60 min | N (%) reporting experience with pathogen | <30 min | 30–60 min | >60 min | P value* | |
| Exposures | |||||||||
| Lice or scabies | 202 (89) | 93 (46) | 71 (35) | 38 (19) | 87 (58) | 21 (24) | 26 (30) | 40 (46) | <.001 |
| Mumps or measles | 163(71) | 24(15) | 31 (19) | 108 (66) | 64(43) | 27 (42) | 14(22) | 23 (36) | <.001 |
| Pertussis | 179(79) | 36 (20) | 71 (40) | 72 (40) | 68 (45) | 30 (44) | 20 (29) | 18(26) | <.001 |
| TB | 209 (92) | 21 (10) | 54 (26) | 134(64) | 117(78) | 19(16) | 47 (40) | 51 (44) | .002 |
| Influenza | 219(96) | 55 (25) | 74 (34) | 90(41) | 143(95) | 25(17) | 54 (38) | 64 (45) | .23 |
| Outbreaks | |||||||||
| MRSA | 189 (83) | 56 (30) | 62 (33) | 71 (38) | 149(99) | 27(18) | 67 (45) | 55 (37) | .02 |
| Other MDRO | 189 (83) | 55 (29) | 54 (29) | 80 (42) | 147(98) | 26(18) | 67 (46) | 54(37) | .003 |
| Respiratory viruses | 181 (79) | 72 (40) | 68 (38) | 41 (23) | 144(96) | 25(17) | 65 (45) | 54 (38) | <.001 |
| Clostridium difficile | 201 (88) | 34(17) | 67 (33) | 100(50) | 124(83) | 4(3) | 26 (21) | 94 (76) | <.001 |
| Gastrointestinal viruses | 202 (89) | 32 (16) | 59 (29) | 111(55) | 133(89) | 20 (15) | 55 (41) | 58 (44) | .06 |
IPs, infection preventionists; MDRO, multidrug-resistant organism; MRSA, methicillin-resistant Staphylococcus aureus; TB, tuberculosis.
Results of the X2 test comparing infection preventionist and staff nurse responses.
In terms of hours spent, in descending order, the percent of nurses reporting an additional workload burden of >60 minutes per exposure or outbreak was C difficile (76%), lice or scabies (46%), influenza (45%), TB (44%), gastrointestinal viruses (44%), respiratory viruses (38%), MRSA and MDROs (each 37%), mumps or measles (36%), and pertussis (26%). In terms of hours spent, in descending order, the percent of the IPs reporting an additional workload burden of >60 minutes per exposure or outbreak was mumps or measles (66%), TB (64%), gastrointestinal viruses (55%), C difficile (50%), MDROs (42%), influenza (41%), pertussis (40%), MRSA (38%), respiratory viruses (23%), and lice or scabies (19%).
Differences in the time that nurses and IPs dedicated or reallocated to prevent and control outbreaks and exposures by organism were also evident. For example, with a TB case in a hospital setting, 54% of the nurses reported a daily increase of <60 minutes, whereas 64% of the IPs reported an increase of >60 minutes. Similarly, response to lice outbreaks/exposures was perceived differently; 46% of the nurses reported an increased workload of >60 minutes per day as compared with 46% of the IPs who reported an increase of <30 minutes. There were also significant differences in the ranking of the most time-consuming tasks. For nurses, the most time-consuming tasks were related to direct patient care, with 92% indicating that additional isolation slowed down patient care, followed by 63% for patient and family education. The most time-consuming task for IPs was related to documentation (Table 3), with 65% selecting chart review and 61% compiling lists of exposures.
Table 3.
Top 3 most time-consuming activities associated with exposures and outbreaks reported by IPs and staff nurses
| No.(%) ofIPs reporting each activity as being in the top 3 | No. (%) ofstaffnurses reporting each activity as being in the top 3 | ||
|---|---|---|---|
| Chart review | 148(65) | Additional isolation precautions that slow down patient care | 138 (92) |
| Exposure list compiling | 139(61) | Educating patients and families on outbreak and exposure precautions | 94 (63) |
| Preventive measures for exposures | 99 (43) | Staffing changes owing to absent staff or patient cohorting | 84 (56) |
| Staff and visitor notifications | 79 (35) | Additional documentation in the electronic health record | 44 (29) |
| Case detection | 67 (29) | Visits to workforce health and safety | 30 (20) |
| Ward rounding | 44(19) | Possibility ofhaving to take time off | 30 (20) |
| Reporting to regulatory authorities | 35 (15) | Requirement to take prophylactic medication (eg, azithromycin for pertussis) | 19 (13) |
| Patient and family education | 23 (10) | Meeting or training with infection prevention and control | 16(11) |
| Reporting to hospital supervisors | 19(8) | ||
| Documentation in the electronic health record | 7(3) |
IPs, infection preventionists.
DISCUSSION
In response to an outbreak or exposure to infectious agents, nurses are likely to spend a large proportion of their time on additional isolation precautions and family and patient education, whereas IPs spend most of their time on chart review and compiling exposure lists. Both nurses and IPs, however, report spending the least amount of time on ward rounding and meeting or training on infection control. This is concerning as exposure and outbreak conditions also have potential to further strain nurses’ adherence to standard precautions, and interaction and feedback between nurses and IPs can facilitate that adherence. In addition, adherence to standard precautions has been shown to be suboptimal in routine conditions and not effectively integrated into the existing patient care workload.12,13
A cumulative effect of additional time and requirements on increased infection prevention activities has been associated with nurses cutting corners, making trade-offs in care, and decreased quality and continuity of care.4 Recent work by Scheithauer et al5 also suggests that even with highly trained, expert clinicians and a well-staffed setting, workload can negatively impact the most basic HAI prevention behaviors such as hand hygiene. Therefore, outbreak and exposure conditions may foster a negative cycle of increased workload, exposures, and HAIs. This speaks to the importance of continued and ongoing training on the basic standards as well as preparedness for the unexpected, so that nurses have the capacity and competency to respond when emergent situations arise.
The impact on nurses’ time suggests that administrators will need to carefully plan, allocate resources, and use tailored approaches in the setting of outbreaks and exposures to ensure that patient safety needs are met. In this study, we were able to quantify the most time-consuming tasks reported by nurses, 92% were related to isolation precautions, with about three-fourths of the nurses reporting an increase of >60 minutes in their workload related to C difficile. Prior qualitative work has established that the burden of C difficile management and prevention is extreme for both frontline nurses and the organization.14 Our findings, roughly extrapolated to the most recent 2016 US data of nearly 96,000 hospital-onset, and an additional 120,000 community-onset, inpatient C difficile cases in 3,605 US hospitals,15 each of whom requires 3 shifts of nursing care per day, and given an average length of stay of 5.8 days per patient,16 would equate to nearly 3 million extra hours of nursing care needed annually (216,000 patients × 3 shifts of nurses per day × 5.8 days × 0.76% who report >60 minutes increase workload per patient = 2,856,384 hours). Because nurses must incorporate these additional tasks into their routine workflow, one might ask from which patients and tasks these hours are reallocated and if these hours are budgeted by hospital administrators, what is the economic impact? Staffing the equivalent of 13 extra registered nurse hours (or a 0.36 full-time equivalent nurse) per patient with C difficile is not feasible, particularly in medically underserved areas. Therefore, in addition to the actions needed to respond when these events occur, these findings offer compelling reasons to proactively support both nurses and IPs to conduct the routine measures and behaviors that are needed to prevent exposures and outbreaks.
Workload burden varied by professional discipline because the roles and responsibilities of the nurse and the IP differ in important ways. Understanding the roles and demands on other members of the interdisciplinary care team is essential for the provision of seamless and safe patient care. For example, regarding the differences found in TB response, IP workload may include the following: (1) identifying and screening potential health care workers and patients exposed to a suspected TB patient who was diagnosed after movement throughout the facility without airborne protections in place; (2) working with plant operations and nursing staff to ensure negative isolation is maintained in a patient room; (3) ensuring workers are donning and doffing protective respirators appropriately; and (4) follow-up with occupational health on screening tests and treatment of employees and with providers on potentially exposed patients over a period of months. Each delayed TB diagnosis has been found to increase IP workload by 38 person-hours.17 In contrast, the staff nurse exposed may be unaware all of these IP activities are occurring for this duration of time and perceive no additional workload burden once the patient is discharged.
Similarly, divergence in perception of workload burden may occur following a scabies or lice exposure, which typically is limited to a 24-hour period of treatment for the suspected carrier, and cleaning of the contaminated items with no further treatment or follow-up of the employees is warranted. The IP may not perceive this to be a substantial increase in burden compared to the workload associated with response to a TB case. However, the communication demands on the IPs are extensive as many “worried well” demand treatment, furlough, or reassignment. Staff, managers, and other stakeholders often place a premium on the “emotional labor” of the IP’s work in terms of availability and acceptability of guidance and feedback.9 And in contrast to the IPs, the perceptions of burden for the staff nurses and the managers may be high, given the diversion of time to staff reassignments and resources dedicated to communication. This divergence in interprofessional perceptions of workload can impact the overall functioning of hospital teams and outcomes for patients.
Limitations
This is a descriptive cross-sectional study, and, therefore, we are unable to evaluate the consequences of the increased burden on IPs, nurses, or patients. The nurses surveyed were from 1 large academic medical center, and the perceptions of workload may not be generalizable to other settings. The IPs were members of a voluntary professional organization and may differ from IPs who are not members and or who have different or multiple roles within their organization. Perceptions of both groups may be subject to recall bias, as we do not know the elapsed time from the experience with an exposure or outbreak in the categories assessed, or the frequency of experience with these occurrences.
CONCLUSIONS
In the already challenging context of insufficient integration of infection prevention behaviors with existing workload, outbreaks and exposures occur, therefore straining effective prevention and control measures by both frontline nurses and IPs. This study addressed a gap in our understanding of the relative impact on nurse and IP workload when caring for patients in an outbreak or exposure situation. Assessing the time burden associated with outbreaks and exposures is an important step to develop and implement prevention and response protocols to minimize added resource requirements.
Relevance to clinical practice
Quantifying the impact and burden associated with common outbreaks and exposures informs the direct practice nurse and IP to better anticipate, plan, and act as an immediate response, and administrators and policy makers to develop comprehensive, flexible, systems solutions to support the safe provision of care as a longer-term response.
Funding/support:
This study was funded by the Agency for Healthcare Research and Quality (R01HS024915) Nursing Intensity of Patient Care Needs and Rates of Healthcare-Associated Infections. A.J.H. was supported by a grant (1K01OH011186) funded by the Centers for Disease Control and Prevention.
Footnotes
The contents are the sole responsibility of the authors and do not represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services.
Conflicts of interest: None to report.
References
- 1.Colindres CV, Bryce E, Coral–Rosero P, Ramos–Soto RM, Bonilla F, Yassi A. Effect of effort–reward imbalance and burnout on infection control among Ecuadorian nurses. Int Nurs Rev 2018;65:190–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lam SK, Kwong EW, Hung MS, Pang SM, Chiang VC. Nurses’ preparedness for infectious disease outbreaks: a literature review and narrative synthesis of qualitative evidence. J Clin Nurs 2018;27:e1244–55. [DOI] [PubMed] [Google Scholar]
- 3.Musau J, Baumann A, Kolotylo C, O’shea T, Bialachowski A. Infectious disease outbreaks and increased complexity of care. Int Nurs Rev 2015;62:404–11. [DOI] [PubMed] [Google Scholar]
- 4.Kaba A, Baumann A, Kolotylo C, Akhtar-Danesh N. A descriptive case study of the changing nature of nurses’ work: the impact of managing infectious diseases requiring isolation. Am J Infect Control 2017;45:200–2. [DOI] [PubMed] [Google Scholar]
- 5.Scheithauer S, Batzer B, Dangel M, Passweg J, Widmer A. Workload even affects hand hygiene in a highly trained and well-staffed setting: a prospective 365/7/24 observational study. J Hosp Infect 2017;97:11–6. [DOI] [PubMed] [Google Scholar]
- 6.Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis 2015;15: 212–24. [DOI] [PubMed] [Google Scholar]
- 7.Yanke E, Moriarty H, Carayon P, Safdar N. A qualitative, interprofessional analysis of barriers to and facilitators of implementation of the Department of Veterans Affairs’ Clostridium difficile prevention bundle using a human factors engineering approach. Am J Infect Control 2018;46:276–84. [DOI] [PubMed] [Google Scholar]
- 8.Bubb TN, Billings C, Berriel-Cass D, Bridges W, Caffery L, Cox J, et al. APIC professional and practice standards. Am J Infect Control 2016;44:745–9. [DOI] [PubMed] [Google Scholar]
- 9.Murphy DM, Hanchett M, Olmsted RN, Farber MR, Lee TB, Haas HP, et al. Competency in infection prevention: a conceptual approach to guide current and future practice. Am J Infect Control 2012;40:296–303. [DOI] [PubMed] [Google Scholar]
- 10.Hale R, Powell T, Drey NS, Gould DJ. Working practices and success of infection prevention and control teams: a scoping study. J Hosp Infect 2015;89:77–81. [DOI] [PubMed] [Google Scholar]
- 11.Landers T, Davis J, Crist K, Malik C. APIC MegaSurvey: methodology and overview. Am J Infect Control 2017;45:584–8. [DOI] [PubMed] [Google Scholar]
- 12.Hessels AJ, Genovese-Schek V, Agarwal M, Wurmser T, Larson EL. Relationship between patient safety climate and adherence to standard precautions. Am J Infect Control 2016;44:1128–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sadule-Rios N, Aguilera G. Nurses’ perceptions of reasons for persistent low rates in hand hygiene compliance. Intensive Crit Care Nurs 2017;42:17–21. [DOI] [PubMed] [Google Scholar]
- 14.Guillemin I, Marrel A, Beriot–Mathiot A, Doucet C, Kazoglou O, Luxemburger C, et al. How do Clostridium difficile infections affect nurses’ everyday hospital work: a qualitative study. Int J Nurs Pract 2015;21:38–45. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. 2016. national and state healthcare-associated infections progress report. Available from: https://www.cdc.gov/hai/data/portal/progress-report.html. Accessed November 11, 2018.
- 16.Shrestha MP, Bime C, Taleban S. Decreasing Clostridium difficile–associated fatality rates among hospitalized patients in the United States: 2004–2014. Am J Med 2018;131:90–6. [DOI] [PubMed] [Google Scholar]
- 17.Kelly AM, D’Agostino JF, Andrada LV, Liu J, Larson E. Delayed tuberculosis diagnosis and costs of contact investigations for hospital exposure: New York City 2010–2014. Am J Infect Control 2017;45:483–6. [DOI] [PMC free article] [PubMed] [Google Scholar]