This cohort study uses a polygenic score approach to assess individual vulnerabilities and traits associated with exposure to bullying in childhood and adolescence.
Key Points
Question
What are key individual factors associated with exposure to bullying?
Findings
Using 35 polygenic scores as genetic proxies to study individual vulnerabilities and traits, this cohort study of 5028 genotyped individuals found that the largest associations were present between exposure to bullying and genetic vulnerabilities for mental health problems (eg, diagnosis of depression, attention-deficit/hyperactivity disorder).
Meaning
The findings implicate mental health vulnerabilities and other individual traits as risk factors for exposure to bullying, and prevention programs may improve long-term outcomes in children and adolescents at risk for experiencing bullying by addressing preexisting vulnerabilities to help break a cycle of repeated exposure to bullying.
Abstract
Importance
Exposure to bullying is a prevalent experience with adverse consequences throughout the life span. Individual vulnerabilities and traits, such as preexisting mental health problems, may be associated with increased likelihood of experiencing bullying. Identifying such individual vulnerabilities and traits is essential for a better understanding of the etiology of exposure to bullying and for tailoring effective prevention.
Objective
To identify individual vulnerabilities and traits associated with exposure to bullying in childhood and adolescence.
Design, Setting, and Participants
For this study, data were drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC), a population-based birth cohort study. The initial ALSPAC sample consisted of 14 062 children born to women residing in Avon, United Kingdom, with an expected date of delivery between April 1, 1991, and December 31, 1992. Collection of the ALSPAC data began in September 6, 1990, and the last follow-up assessment of exposure to bullying was conducted when participants were 13 years of age. Data analysis was conducted from November 1, 2017, to January 1, 2019.
Exposures
The polygenic score approach was used to derive genetic proxies that indexed vulnerabilities and traits. A total of 35 polygenic scores were computed for a range of mental health vulnerabilities (eg, depression) and traits related to cognition (eg, intelligence), personality (eg, neuroticism), and physical measures (eg, body mass index), as well as negative controls (eg, osteoporosis).
Main Outcomes and Measures
Single and multi–polygenic score regression models were fitted to test the association between indexed traits and exposure to bullying. Children completed the Bullying and Friendship Interview Schedule at the ages of 8, 10, and 13 years. A mean score of exposure to bullying across ages was used as the main outcome.
Results
A total of 5028 genotyped individuals (2481 boys and 2547 girls) with data on exposure to bullying were included. Among the 35 initially included polygenic scores, 11 were independently associated with exposure to bullying; no significant association was detected for the 24 remaining scores. In multivariable analyses, 5 polygenic scores were associated with exposure to bullying; the largest associations were present for genetic risk relating to mental health vulnerabilities, including diagnosis of depression (standardized b = 0.065; 95% CI, 0.035-0.095) and attention-deficit/hyperactivity disorder (standardized b = 0.063; 95% CI, 0.035-0.091), followed by risk taking (standardized b = 0.041; 95% CI, 0.013-0.069), body mass index (standardized b = 0.036; 95% CI, 0.008-0.064), and intelligence (standardized b = −0.031; 95% CI, −0.059 to 0.003).
Conclusion and Relevance
Using the multi–polygenic score approach, the findings implicate preexisting mental health vulnerabilities as risk factors for exposure to bullying. A mechanistic understanding of how these vulnerabilities link to exposure of bullying is important to inform prevention strategies.
Introduction
Bullying, defined as repeated, intentional aggression by a more powerful bully against a less powerful individual,1 is a widespread phenomenon among school-aged children and adolescents. Up to 1 in 5 adolescents encounter some form of bullying, such as physical, verbal, or social abuse by peers.2,3 Multiple lines of evidence have demonstrated its adverse consequences on mental health and well-being.4,5,6,7,8,9,10,11 To tailor preventive strategies, it is pivotal to understand the origins of exposure to bullying. Epidemiologic research at the phenotypic level has suggested a range of individual vulnerabilities and traits that may evoke bullying by peers, including preexisting mental health vulnerabilities (eg, hyperactivity, depression)12,13 and traits relating to cognition (eg, intelligence),14 personality,15 and physical characteristics (eg, obesity).16,17 Although such evidence implicates many putative individual vulnerabilities and traits associated with exposure to bullying, previous evidence comes solely from observational phenotypic studies.12,13,14,15,16,17 Integration of findings from multiple approaches with differing key sources of potential biases enables the triangulation of findings, strengthening causal inference.18 Thus, a systematic investigation of independent risk factors that reflect a range of potentially overlapping vulnerabilities and traits is needed.
One approach that can be used to provide insights into the etiology of exposure to bullying is the use of polygenic scores (PGSs), which exploit genetic data to study complex traits.19 The PGS approach allows us to derive genetic proxies for individual vulnerabilities and traits to test whether those vulnerabilities and traits are involved in the etiology of exposure to bullying. On the basis of summary statistics from a discovery genome-wide association study (GWAS) for a given trait, a PGS is computed in the target sample by aggregating the effects of many common genetic variants associated with that particular trait in a single individual-level score. Thus, PGSs represent genetic proxies for individual vulnerabilities, such as depression, which can then be tested for associations with exposure to bullying.20 If depression is causally involved in the etiology of exposure to bullying, the PGS for depression as a genetic proxy of depression symptoms should predict exposure to bullying. This approach can be conceived as a first step in a series of genetically informed designs,19,21,22 including mendelian randomization, which allows a deeper delving into the etiology of exposure to bullying (eMethods in the Supplement). The PGS approach has already helped to clarify the etiology of conditions such as substance use,23,24 depression,25 schizophrenia,26 and behavioral problems.27,28 A recent extension is the multi-PGS approach, a multivariate approach that assesses the unique effect per PGS.29,30 However, to our knowledge, no study to date has applied the PGS approach to systematically study the etiology of environmental exposures, such as exposure to bullying.
In this study, we used the PGS approach to triangulate evidence on factors involved in risk for exposure to bullying and to dissect its genetic architecture. Given the large number of PGSs available to date, this approach offers a unique opportunity to study simultaneously a wide range of genetic proxies for individual vulnerabilities and traits in a single comprehensive investigation.
Methods
Sample
We used phenotype and genotype data from the Avon Longitudinal Study of Parents and Children (ALSPAC). The initial ALSPAC sample consisted of 14 062 children born to women residing in Avon, United Kingdom, with an expected date of delivery between April 1, 1991, and December 31, 1992.31,32 Data analysis was conducted from November 1, 2017, to January 1, 2019. The study website contains details of all the data that are available through a fully searchable data dictionary and variable search tool.33 After quality control, genotype data were available for 7288 unrelated children of European ancestry (eMethods in the Supplement). A final sample of 5028 children with exposure to bullying and genotype data were included in the analyses. Children included in the analysis differed from nonincluded children in some demographic variables, but differences were small (eTable 1 in the Supplement). Ethical approval was obtained from the ALSPAC Law and Ethics Committee and SouthWest–Central Bristol National Health Service Research Ethics Committee, and participants gave written informed consent. The study uses fully anonymized ALSPAC data and no clinical or administrative records.
Exposure to Bullying Between the Ages of 8 and 13 Years
Exposure to bullying was assessed based on child reports at 8, 10, and 13 years of age using a modified version of the Bullying and Friendship Interview Schedule (BFIS).2 The BFIS items (eTable 2 in the Supplement) assess 9 bullying experiences in the past 6 months that involved overt (eg, had personal belongings taken) or relational (eg, exclusion by peers) bullying. Each item ranges from 0 to 3 (with 0 indicating no; 1, sometimes [<4 times]; 2, repeatedly [≥4 times]; and 3, very frequently [≥1 per week]). An overall exposure to bullying score was computed at each age as the mean across all items. A mean score across the ages of 8, 10, and 13 years was computed if data were available for at least 2 of the 3 time points.
PGS Analyses
The individual PGSs for ALSPAC participants were generated using PRSice software34 based on the ALSPAC genotype data and 35 publicly available summary statistics from GWASs. We selected GWASs that indexed individual vulnerabilities and traits that can plausibly evoke exposure to bullying, as well as negative controls (eTable 3 in the Supplement). The PGSs were computed for ALSPAC participants as the sum of alleles associated with the phenotype of interest (eg, depression), weighted by their effect sizes reported in the corresponding GWASs. Clumping was conducted to remove single-nucleotide polymorphisms in linkage disequilibrium (r2 > 0.10 within a 250–base pair window). The PGSs were computed for all P value thresholds of .01 to 1 at .01 increments (ie, at 99 thresholds) to obtain the P value of the best-fit PGS per GWAS data set. In PRSice, the best fit is defined as the P value threshold at which the PGS is associated with the phenotype (in our study, exposure to bullying) with the highest R2 obtained from linear regression analysis. Permutation (10 000 times) was used to generate an empirical P value for the best-fit threshold to reduce overfitting and to address the issue of multiple testing within each PGS (99 thresholds tested per PGS). To account for multiple testing across the individual PGSs tested in separate linear regression models (single-PGS models), false discovery rate–corrected P values are also provided.35 To assess the independent effects of the PGSs when modeled together, the best-fit PGSs that were associated with exposure to bullying were selected and included in a multi-PGS linear regression model using R, version 3.4.4.36 All linear regression models, including the single-PGS models tested in PRSice and the multi-PGS model tested in R, were controlled for sex and population stratification by including 15 principal components as covariates in the models. To facilitate interpretability, all PGSs were standardized.36
Results
Associations Between PGSs and Exposure to Bullying
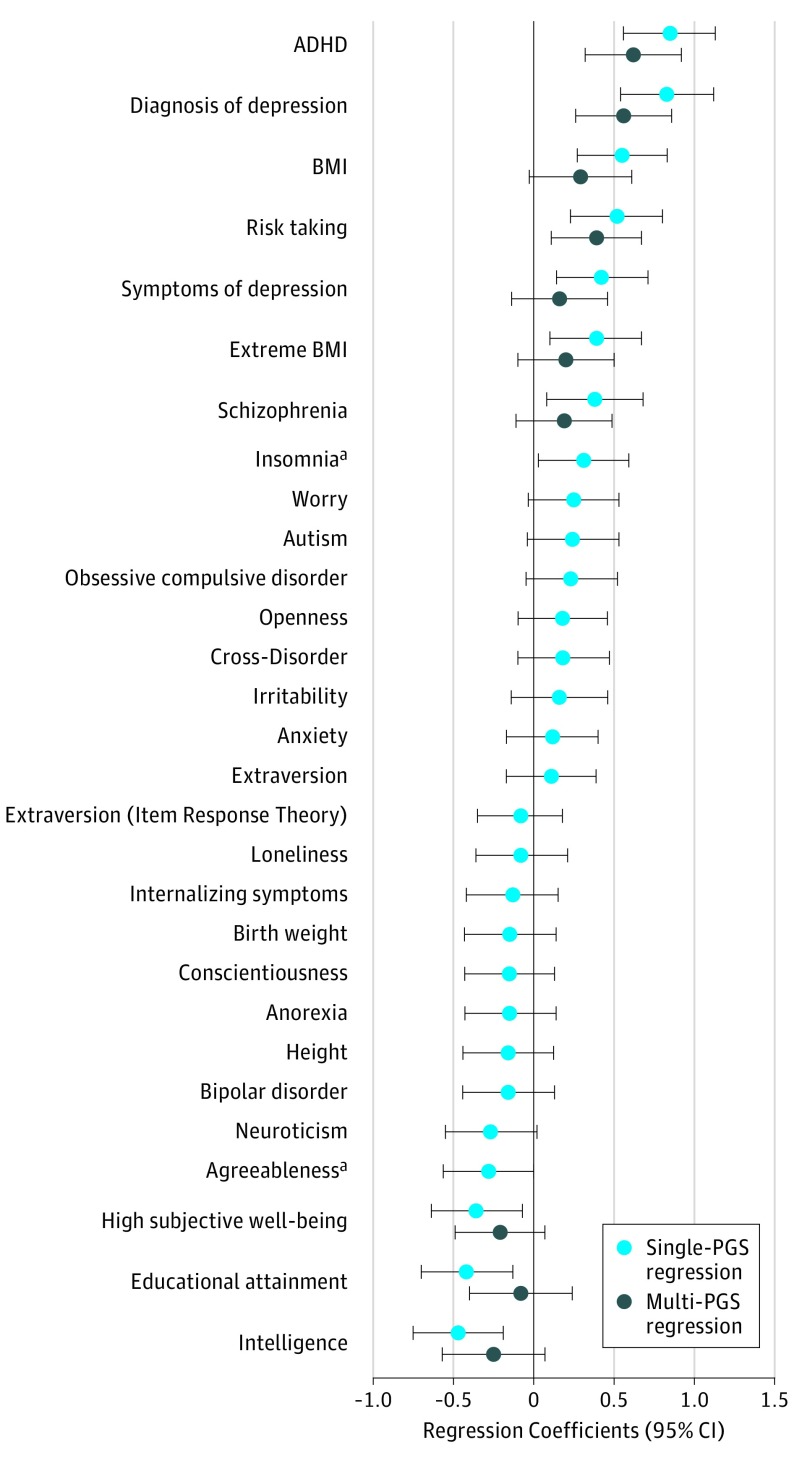
A total of 5028 genotyped individuals (2481 boys and 2547 girls) with data on exposure to bullying were included. A total of 4391 children (87.3%) in the sample reported some form of exposure to bullying at least once (mean BFIS score, >0) at the ages of 8, 10, and 13 years. The mean (SD) of the sum scores of the 9 BFIS items per time point was 2.23 (2.27) (range, 0.0-20.6). Correlations among all 35 included PGSs are displayed in Figure 1 (eTable 4 in the Supplement). The strongest correlations were present between cognitive measures (eg, intelligence and educational attainment: r for PGSs, 0.41) and measures related to mood (symptoms of depression and neuroticism: r for PGSs, 0.41). Table 1 and Figure 2 give the standardized estimates from the single-PGS and multi-PGS linear regression models. As shown in the single-PGS models, 10 PGSs remained significantly associated after permutations with exposure to bullying: diagnosis of depression (standardized b, 0.083; 95% CI, 0.054-0.112), symptoms of depression (standardized b, 0.042; 95% CI, 0.014-0.071), high subjective well-being (standardized b, −0.036; 95% CI, −0.064 to −0.007), attention-deficit/hyperactivity disorder (ADHD) (standardized b, 0.085; 95% CI, 0.056-0.113), schizophrenia (standardized b, 0.038, 95% CI, 0.008-0.068), intelligence (ie, IQ) (standardized b, −0.047; 95% CI, −0.075 to −0.019), educational attainment (standardized b, −0.042; 95% CI, −0.07 to −0.013), risk taking (standardized b, 0.052; 95% CI, 0.023-0.08), body mass index (BMI) (standardized b, 0.055; 95% CI, 0.027-0.083), and extreme BMI (standardized b, 0.039; 95% CI, 0.010-0.067).
Figure 1. Heat Map of Genetic Correlations Among All Included 35 Polygenic Scores (PGSs).
The strongest correlations were present between cognitive measures (eg, intelligence and educational attainment: r for PGSs, 0.41) and measures related to mood (symptoms of depression and neuroticism: r for PGSs, 0.41). ADHD indicates attention-deficit/hyperactivity disorder; BMI, body mass index; and OCD, obsessive compulsive disorder.
Table 1. Single-PGS and Multi-PGS Linear Regression Models.
| Vulnerabilities and Traits | Discovery Sample, No. | SNPs, No. | P Valuea | Single-PGS Modelsb | Multi-PGS Modelb,e | Restricted Multi-PGS modelb,f | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Standardized Coefficient, b (95% CI) | Permutation P valuec | Permutation/FDR P Valued | Standardized Coefficient, b (95% CI) | P Value | Standardized Coefficient, b (95% CI) | P Value | ||||
| Mental Health Vulnerabilities | ||||||||||
| Depression diagnosis | 173 005 | 24 085 | .03 | 0.083 (0.054 to 0.112) | <.001 | <.001 | 0.056 (0.026 to 0.086) | <.001 | 0.065 (0.035 to 0.095) | <.001 |
| Depression symptoms | 16 460 | 99 457 | .45 | 0.042 (0.014 to 0.071) | .01 | .05 | 0.016 (−0.014 to 0.046) | .26 | NA | NA |
| Loneliness | 10 760 | 125 870 | .41 | −0.008 (−0.036 to 0.021) | .98 | .98 | NA | NA | NA | NA |
| Insomnia | 113 006 | 20 288 | .03 | 0.031 (0.003 to 0.059) | .10 | .25 | NA | NA | NA | NA |
| Worry | 348 219 | 42 062 | .06 | 0.025 (−0.003 to 0.053) | .11 | .41 | NA | NA | NA | NA |
| High subjective well-being | 298 420 | 94 303 | .86 | −0.036 (−0.064 to −0.007) | .048 | .14 | −0.021 (−0.049 to 0.007) | .15 | NA | NA |
| Anxiety | 18 186 | 17 194 | .04 | 0.012 (−0.017 to 0.04) | .87 | .93 | NA | NA | NA | NA |
| Internalizing symptoms | 4596 | 95 391 | .63 | −0.013 (−0.042 to 0.015) | .83 | .93 | NA | NA | NA | NA |
| ADHD | 55 374 | 35 130 | .07 | 0.085 (0.056 to 0.113) | <.001 | <.001 | 0.062 (0.032 to 0.092) | <.001 | 0.063 (0.035 to 0.091) | <.001 |
| Autism | 15 954 | 8376 | .02 | 0.024 (−0.004 to 0.053) | .25 | .49 | NA | NA | NA | NA |
| OCD | 9725 | 178 011 | .60 | 0.023 (−0.005 to 0.052) | .29 | .52 | NA | NA | NA | NA |
| Anorexia | 14 477 | 7910 | .01 | −0.015 (−0.043 to 0.014) | .72 | .87 | NA | NA | NA | NA |
| Bipolar disorder | 16 731 | 16 216 | .05 | −0.016 (−0.044 to 0.013) | .64 | .87 | NA | NA | NA | NA |
| Schizophrenia | 105 318 | 24 577 | .02 | 0.038 (0.008 to 0.068) | .03 | .10 | 0.019 (−0.011 to 0.049) | .22 | NA | NA |
| Cross disorder | 61 220 | 67 223 | .44 | 0.018 (−0.010 to 0.047) | .49 | .76 | NA | NA | NA | NA |
| Cognitive Measures | ||||||||||
| Intelligence | 269 867 | 17 342 | .01 | −0.047 (−0.075 to −0.019) | .004 | .02 | −0.025 (−0.057 to 0.007) | .11 | −0.031 (−0.059 to −0.003) | .03 |
| Educational attainment | 766 345 | 113 854 | .24 | −0.042 (−0.07 to −0.013) | .01 | .048 | −0.008 (−0.040 to 0.024) | .64 | NA | NA |
| Personality Traits | ||||||||||
| Risk taking | 436 236 | 80 415 | .16 | 0.052 (0.023 to 0.08) | .002 | .01 | 0.039 (0.011 to 0.067) | .007 | 0.041 (0.013 to 0.069) | .004 |
| Neuroticism | 168 105 | 175 479 | .57 | −0.027 (−0.055 to 0.002) | .17 | .38 | NA | NA | NA | NA |
| Irritability | 345 231 | 11 888 | .01 | 0.016 (−0.014 to 0.046) | .60 | .84 | NA | NA | NA | NA |
| Openness | 17 375 | 90 205 | .77 | 0.018 (−0.01 to 0.046) | .52 | .76 | NA | NA | NA | NA |
| Extraversion | 17 375 | 11 612 | .04 | 0.011 (−0.017 to 0.039) | .89 | .93 | NA | NA | NA | NA |
| Item response theory | 63 030 | 21 054 | .04 | −0.008 (−0.035 to 0.018) | .88 | .93 | NA | NA | NA | NA |
| Conscientiousness | 17 375 | 3715 | .01 | −0.015 (−0.043 to 0.013) | .71 | .87 | NA | NA | NA | NA |
| Agreeableness | 17 375 | 13 959 | .05 | −0.028 (−0.056 to 0) | .16 | .38 | NA | NA | NA | NA |
| Physical Traits | ||||||||||
| BMI | 681 275 | 44 601 | .10 | 0.055 (0.027 to 0.083) | .001 | .01 | 0.029 (−0.003 to 0.061) | .06 | 0.036 (0.008 to 0.064) | .01 |
| Extreme BMI | 16 068 | 26 154 | .15 | 0.039 (0.01 to 0.067) | .03 | .10 | 0.02 (−0.010 to 0.050) | .17 | NA | NA |
| Birth weight | 205 475 | 18 921 | .02 | −0.015 (−0.043 to 0.014) | .62 | .84 | NA | NA | NA | NA |
| Height | 693 529 | 32 725 | .02 | −0.016 (−0.044 to 0.012) | .51 | .76 | NA | NA | NA | NA |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; BMI, body mass index; FDR, false discovery rate; NA, not applicable; OCD, obsessive compulsive disorder; PGS, polygenic score; SNP, single-nucleotide polymorphism.
P value threshold for the best-fit PGS.
Included covariates were sex and the 15 principal components.
P value estimate after permutation (10 000 times).
P value estimate after permutation (10 000 times) and FDR adjustment.
Linear regression model, including all PGSs with a permutated (10 000 permutations) P > .05 estimated in single-PGS regression models.
Linear regression model, including all PGSs from the multi-PGS regression models except PGSs that were not significant after FDR correction in single-PGS models and variables that are in collinearity (eMethods in the Supplement).
Figure 2. Single–Polygenic Score (PGS) and Multi-PGS Linear Regression Results.
Standardized coefficients and 95% CIs (error bars) obtained from single-PGS regression models (light blue dots) and a multi-PGS regression model (dark blue dots). For the single-PGS regression estimates, separate models per individual PGS were tested (controlled for sex and 15 principal components). For the multi-PGS regression estimates, a multivariable model was tested, including 10 PGS, sex, and 15 principal components. ADHD indicates attention-deficit/ hyperactivity disorder; BMI, body mass index.
aNot significant after permutation (10 000 times) and not included in the multi-PGS model.
When the 10 PGSs were simultaneously included in the first multi-PGS regression model (Table 1), 3 PGSs were independently associated with exposure to bullying: diagnosis of depression (standardized b, 0.056; 95% CI, 0.026-0.086), ADHD (standardized b, 0.062; 95% CI, 0.032-0.092), and risk taking (standardized b, 0.039; 95% CI, 0.011-0.067). In a second multi-PGS model, we tested a restricted version of the previous model (Table 1) to reduce collinearity. In the restricted multi-PGS model, we included only PGSs that remained significant after false discovery rate correction of the permutated P values and selected only the most significant PGSs from a set of PGSs associated with the same underlying construct (eg, cognition as the latent construct, reflected in intelligence and educational attainment) (eMethods in the Supplement). Compared with the first multi-PGS model, 2 additional PGSs were associated with exposure to bullying in the restricted version: BMI and intelligence.
In the restricted multi-PGS model, 5 PGSs were independently associated with exposure to bullying; the largest associations were present for genetic risk related to mental health vulnerabilities, including diagnosis of depression (standardized b = 0.065; 95% CI, 0.035-0.095) and ADHD (standardized b = 0.063; 95% CI, 0.035-0.091), followed by risk taking (standardized b = 0.041; 95% CI, 0.013-0.069), BMI (standardized b = 0.036; 95% CI, 0.008-0.064), and intelligence (standardized b = −0.031; 95% CI, −0.059 to 0.003). Of the 6 negative controls, only poor self-rated health was significant (standardized b, 0.057; 95% CI, 0.028-0.086) (Table 2).
Table 2. Linear Regression for Negative Control Polygenic Scores.
| Negative Control Phenotype | Discovery Sample, No. | SNPs, No. | P Valuea | Standardized Coefficient, b (95% CI) | Permutation P Valueb |
|---|---|---|---|---|---|
| Alcoholic liver disease | 361 194 | 126 650 | .35 | −0.027 (−0.056 to 0.001) | .18 |
| Family history of Alzheimer disease | 314 278 | 8591 | .01 | −0.032 (−0.060 to −0.004) | .09 |
| Poor self-rated health | 111 749 | 96 877 | .22 | 0.057 (0.028 to 0.086) | <.001 |
| Inflammatory bowel disease | 34 652 | 103 729 | .24 | 0.017 (−0.011 to 0.045) | .52 |
| Osteoporosis | 142 487 | 60 289 | .09 | 0.006 (−0.024 to 0.035) | .99 |
| Parkinson disease | 5691 | 3744 | .01 | −0.019 (−0.047 to 0.009) | .52 |
Abbreviation: SNP, single-nucleotide polymorphism.
P value threshold for the best-fit polygenic genic.
P value estimate after permutation (10 000 times).
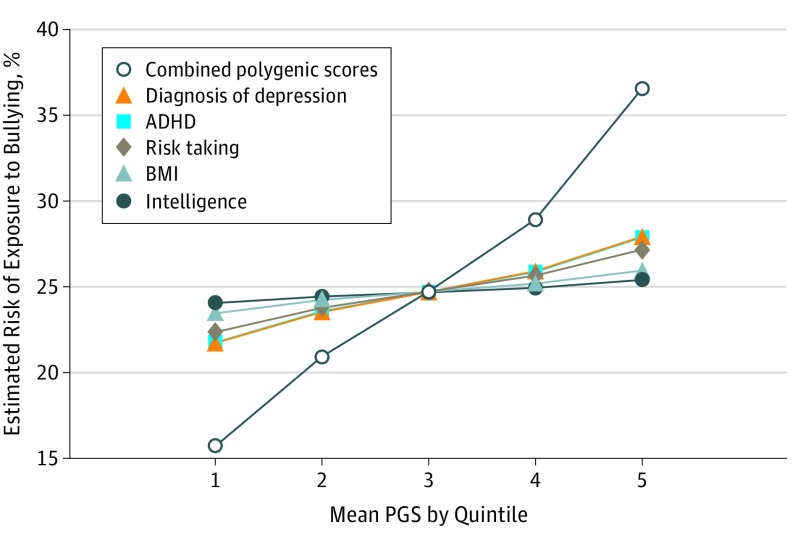
Figure 3 shows the combined additive effects of the 5 PGSs (diagnosis of depression, ADHD, risk taking, BMI, and intelligence) and their independent effects. Estimates are reported as predicted prevalence rates of exposure to bullying per mean PGS per quintile (eTables 5-8 in the Supplement for logistic regression estimates and the predicted probabilities). Children in the lowest quintile for all 5 PGSs had a predicted prevalence of 15.7% compared with 36.6% among children in the highest quintile.
Figure 3. Individual and Combined Associations of Polygenic Scores (PGSs) With Risk of Exposure to Bullying.
Plot of the predicted percentages obtained from multivariable logistic regression of 5 PGSs (diagnosis of depression, attention-deficit/hyperactivity disorder [ADHD], risk taking, body mass index [BMI], and intelligence) and risk of exposure to bullying (eTables 5-8 and eMethods in the Supplement). The difference in magnitude between the individual effects of the 5 PGSs and the additive effects of the 5 PGSs combined in estimating risk of exposure to bullying is shown.
A range of complementary analyses using the restricted multi-PGS model were conducted, in which we (1) tested the association with an outcome that captured chronicity of exposure to bullying (eTable 2 in the Supplement), (2) controlled for the effects of bullying perpetration, and (3) tested for PGS-by-sex interactions. As reported in eTables 9 and 10 in the Supplement, (1) the patterns of associations were similar for chronicity of exposure to bullying; (2) depression, BMI, and intelligence remained significantly associated with exposure to bullying when bullying perpetration was included as a covariate but not the effects of ADHD and risk taking; and (3) there was no evidence of an interaction effect with sex.
Discussion
This was the first study, to our knowledge, to use PGSs as genetic proxies to systematically examine the role of a wide range of individual vulnerabilities and traits as risk factors for exposure to bullying. Our approach implicated several vulnerabilities associated with exposure to bullying, with mental health difficulties contributing the most, including depression and ADHD. In addition, PGSs for risk taking, BMI, and intelligence were independently associated with exposure to bullying. No other genetic proxy was associated with exposure to bullying, including proxies related to other mental health disorders (eg, bipolar disorder, autism, and obsessive-compulsive disorder), traits related to personality (eg, neuroticism), and physical measures other than BMI (eg, height). In the following subsections, we discuss the (1) novel insights into factors involved in risk for exposure to bullying, (2) interpretation of genetic factors associated with exposure to bullying, and (3) insights into prevention.
Insights Into the Etiology of Exposure to Bullying
To our knowledge, for the first time based on genomic evidence, this study suggests that having a genetic predisposition for a number of individual vulnerabilities and traits is associated with exposure to bullying. This finding is in line with a body of research that focused on the consequences of exposure to bullying,37 suggesting that the association between exposure to bullying and mental health outcomes can partially be accounted for by preexisting heritable vulnerabilities and traits.4 In particular, our findings implicate a genetic vulnerability to mental health problems, namely, externalizing symptoms and traits (ie, ADHD and risk taking) and internalizing symptoms (ie, depression). Our findings support a critical role of early mental health symptoms in the vulnerability to experience bullying.38 A genetic propensity for high intelligence was associated with a reduced risk of experiencing bullying, adding to previous evidence of an association between cognitive skills and exposure to bullying.14,39 As the only physical trait, a genetic risk for high BMI was associated with an increase in exposure to bullying, in line with previous research.16,17
Contrary to previous observational evidence,15,40 no other individual vulnerabilities (eg, bipolar disorder, anxiety disorder) or traits (eg, neuroticism) were associated with exposure to bullying in our multivariable analysis, which could be attributable to different reasons. First, mental health conditions, such as bipolar disorder, usually fully manifest later in life, which may explain why their genetic proxies were not associated with exposure to bullying in the sample of children in our study. Second, such disorders are rare in population cohorts of children like this study sample (ie, a lack of power may have hampered the detection of existing associations). Power issues may therefore explain why schizophrenia was only associated with exposure to bullying under less stringent conditions (eg, schizophrenia PGS was no longer significant after correction for multiple testing). Regarding the lack of association between exposure to bullying and previously associated personality traits,15,41 the PGSs used in this study were based on large studies (eg, based on GWAS samples >450 000 for irritability and >160 000 for neuroticism). Considering that such PGSs have been reported to contribute to child outcomes,42 the lack of association unlikely reflects insufficient power. Instead, our findings suggest that some of the previously observed associations might be driven by co-occurring internalizing or externalizing symptoms.
The PGS approach enabled the systematic investigation of a wide range of potential independent pathways involved in exposure to bullying. Of importance, we did not interpret associations between PGSs and bullying as direct genetic contributions (ie, genetic variants cannot code directly for exposure to bullying). Instead, they represent indirect contributions (eg, the genetic risk for ADHD increases the risk of ADHD symptoms, which, in turn, is associated with an increase in exposure to bullying). Such interpretation is consistent with the use of genetic instruments to assess the nature of associations between a risk factor and an outcome, as in mendelian randomization studies.
Our results provide an avenue for future etiologic studies, which are essential to gaining a deeper understanding of how these vulnerabilities link to exposure to bullying. After sufficiently large genotyped samples with data on bullying become available, future studies could use genetic variants to refine pathways within a structural equation modeling framework43 and explore possible gene × environment interactions. Such research could help improve the mechanistic understanding and identify protective contributing factors (eg, social support, mental health intervention, and school type) that may mitigate some of the effects of preexisting vulnerabilities.
Interpreting Genetic Factors Associated With Exposure to Bullying
Behavioral genetic studies44,45 have demonstrated that exposure to bullying is heritable. Heritability of environmental exposures, such as bullying, reflects what is commonly described as gene-environment correlations (rGEs) (ie, that environmental exposures do not happen at random but partly depend on genetic factors). An evocative rGE is one type of rGE, whereby genetically influenced characteristics (eg, depressive symptoms) evoke an environmental response.46 To our knowledge, for the first time based on genomic data, we supported previous findings of genetic contributions to exposure to bullying and further examined the nature of these genetic factors by identifying genetically influenced characteristics that can make individuals more vulnerable to experiencing bullying. Of importance, other types of rGEs, such as passive rGE, may partly explain the findings (eDiscussion in the Supplement). On the basis of our results, we are unable to distinguish the genetic effects in the child from those in the parent that affect the child indirectly. However, passive rGE is unlikely to fully account for the associations found in our study,47 and further studies could explore the nature of nurture of exposure to bullying by embedding the PGS approach within family designs.21
Of importance, rGE is not independent of the context in which it occurs. For example, body image perceptions vary substantially across countries: being overweight is positively perceived (eg, as a sign of strength and health) in some countries but negatively perceived in others.48 In that example, we hypothesize that a genetic predisposition for high BMI would unlikely be associated with exposure to bullying in cultures with positive attitudes toward being overweight. In other words, BMI-related genetic influences on exposure to bullying can be silenced in different contexts (ie, may not be present in all cultural contexts) (eDiscussion in the Supplement). Such socially dependent effects can be tested by repeating analyses across contexts.
Insights for Prevention of Exposure to Bullying
Most current prevention programs focus on antibullying strategies that aim to reduce the occurrence of bullying (eg, KiVa,49 Olweus Bullying Prevention Program50). Our findings of genetic contributions to exposure to bullying do not undermine the importance of antibullying strategies because, as stated above, genetic factors are not deterministic and can be context dependent; thus, modifying the context may be beneficial. Our genetically informed approach strengthens evidence regarding the role of preexisting vulnerabilities involved in exposure to bullying. We suggest that awareness of such preexisting vulnerabilities can help to further tailor antibullying strategies in vulnerable children. Such strategies could, for example, include school-based interventions aimed at reducing stigma regarding mental health and other vulnerabilities (eg, obesity51 or cognitive impairments). In addition, more accessible early mental health care within schools could help reduce symptoms, potentially reducing risk of future bullying and long-term psychopathologic symptoms. Finally, a better understanding of how preexisting vulnerabilities and traits express themselves in different contexts may provide insights into how the association between preexisting vulnerabilities and exposure to bullying can be silenced, (eg, by changing the specific environment in which this association is expressed).
A limitation of antibullying strategies is that they currently fail to stop all bullying and have a limited influence on mental health outcomes in children.52 Genetically influenced vulnerabilities are likely to be fairly stable over time,53 which potentially put children at risk for repeated exposure to bullying and the associated adverse consequences on children’s mental health.4,5 Children’s preexisting mental health difficulties may also evoke less social support,54 aggravating the consequences of exposure to bullying.55 Targeted prevention programs should address those vulnerabilities to interrupt the cycle of repeated bullying and, therefore, prevent persistent mental health difficulties.
Limitations
This study has some limitations. Although the PGS approach used in this study constitutes a tool that retains key advantages over simple association analyses at the phenotype level by using genetic proxies that are more robust to confounding,56 the approach relies on assumptions that cannot be tested using currently available data (eDiscussion in the Supplement). A large GWAS of exposure to bullying, which is not currently available, would allow replication of our findings and implementation of a set of more robust methods (eg, 2-sample mendelian randomization, multivariable mendelian randomization, and methods to assess reverse and bidirectional relationships21) to support stronger causal inference. In addition, the independent contributions of the individual PGSs to exposure to bullying were small. However, this was expected given that (1) exposure to bullying is multifactorial, (2) current PGSs only partially capture the heritability of their traits, and (3) PGSs likely affect risk of exposure to bullying indirectly. Finally, attrition in the ALSPAC cohort could mean that we did not capture the most genetically vulnerable children, thus obscuring associations with exposure to bullying. However, included and nonincluded children had similar family histories of mental disorder and early developmental characteristics, suggesting that this was not the case.
Conclusions
These results implicate preexisting mental health vulnerabilities as risk factors for exposure to bullying. A mechanistic understanding of how these vulnerabilities link to exposure to bullying is important to inform prevention strategies.
eMethods. Genotyping and Quality Control Procedures, Polygenic Scores, and Analysis
eDiscussion. Insights and Interpretations
eTable 1. Early Participant Characteristics for Nonincluded vs Included Individuals
eTable 2. Bullying and Friendship Interview Schedule
eTable 3. Overview GWAS Summary Statistics
eTable 4. Pearson Correlation Estimates Between Polygenic Scores
eTable 5. Multivariable Logistic Regression Analysis (Sex Excluded)
eTable 6. Multivariable Logistic Regression Analysis (Sex Included)
eTable 7. Single-PRS Prediction of Exposure to Bullying
eTable 8. Multi-PRS Prediction of Exposure to Bullying
eTable 9. Sensitivity Analyses on the Restricted Multi-PGS Regression Model
eTable 10. Linear Regression Models Testing for Interaction Effects With Sex
eReferences
References
- 1.Olweus D. Bullying at School: What We Know and What Can We Do. Malden, MA: Blackwell Publishing Inc; 1993. [Google Scholar]
- 2.Wolke D, Woods S, Stanford K, Schulz H. Bullying and victimization of primary school children in England and Germany: prevalence and school factors. Br J Psychol. 2001;92(pt 4):673-696. doi: 10.1348/000712601162419 [DOI] [PubMed] [Google Scholar]
- 3.Modecki KL, Minchin J, Harbaugh AG, Guerra NG, Runions KC. Bullying prevalence across contexts: a meta-analysis measuring cyber and traditional bullying. J Adolesc Health. 2014;55(5):602-611. doi: 10.1016/j.jadohealth.2014.06.007 [DOI] [PubMed] [Google Scholar]
- 4.Singham T, Viding E, Schoeler T, et al. . Concurrent and longitudinal contribution of exposure to bullying in childhood to mental health: the role of vulnerability and resilience. JAMA Psychiatry. 2017;74(11):1112-1119. doi: 10.1001/jamapsychiatry.2017.2678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schoeler T, Duncan L, Cecil CM, Ploubidis GB, Pingault J-B. Quasi-experimental evidence on short- and long-term consequences of bullying victimization: a meta-analysis. Psychol Bull. 2018;144(12):1229-1246. doi: 10.1037/bul0000171 [DOI] [PubMed] [Google Scholar]
- 6.Brendgen M, Poulin F. Continued bullying victimization from childhood to young adulthood: a longitudinal study of mediating and protective factors. J Abnorm Child Psychol. 2018;46(1):27-39. doi: 10.1007/s10802-017-0314-5 [DOI] [PubMed] [Google Scholar]
- 7.Nguyen AJ, Bradshaw CP, Townsend L, Gross A, Bass J. It gets better: attenuated associations between latent classes of peer victimization and longitudinal psychosocial outcomes in four low-resource countries [published online October 8, 2018]. J Youth Adolesc. [DOI] [PubMed] [Google Scholar]
- 8.Moore SE, Norman RE, Suetani S, Thomas HJ, Sly PD, Scott JG. Consequences of bullying victimization in childhood and adolescence: a systematic review and meta-analysis. World J Psychiatry. 2017;7(1):60-76. doi: 10.5498/wjp.v7.i1.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ttofi MM, Farrington DP, Lösel F, Loeber R. Do the victims of school bullies tend to become depressed later in life? a systematic review and meta-analysis of longitudinal studies. J Aggress Conflict Peace Res. 2011;3(2):63-73. doi: 10.1108/17596591111132873 [DOI] [Google Scholar]
- 10.Arseneault L. Annual research review: the persistent and pervasive impact of being bullied in childhood and adolescence: implications for policy and practice. J Child Psychol Psychiatry. 2018;59(4):405-421. doi: 10.1111/jcpp.12841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arseneault L. The long-term impact of bullying victimization on mental health. World Psychiatry. 2017;16(1):27-28. doi: 10.1002/wps.20399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barker ED, Boivin M, Brendgen M, et al. . Predictive validity and early predictors of peer-victimization trajectories in preschool. Arch Gen Psychiatry. 2008;65(10):1185-1192. doi: 10.1001/archpsyc.65.10.1185 [DOI] [PubMed] [Google Scholar]
- 13.Cook CR, Williams KR, Guerra NG, Kim TE, Sadek S. Predictors of bullying and victimization in childhood and adolescence: a meta-analytic investigation. Sch Psychol Q. 2010;25(2):65-83. doi: 10.1037/a0020149 [DOI] [Google Scholar]
- 14.Verlinden M, Veenstra R, Ghassabian A, et al. . Executive functioning and non-verbal intelligence as predictors of bullying in early elementary school. J Abnorm Child Psychol. 2014;42(6):953-966. doi: 10.1007/s10802-013-9832-y [DOI] [PubMed] [Google Scholar]
- 15.Mulder S, van Aken M. Socially anxious children at risk for victimization: the role of personality. Soc Dev. 2013;23(4):719-733. doi: 10.1111/sode.12068 [DOI] [Google Scholar]
- 16.Janssen I, Craig WM, Boyce WF, Pickett W. Associations between overweight and obesity with bullying behaviors in school-aged children. Pediatrics. 2004;113(5):1187-1194. doi: 10.1542/peds.113.5.1187 [DOI] [PubMed] [Google Scholar]
- 17.Lumeng JC, Forrest P, Appugliese DP, Kaciroti N, Corwyn RF, Bradley RH. Weight status as a predictor of being bullied in third through sixth grades. Pediatrics. 2010;125(6):e1301-e1307. doi: 10.1542/peds.2009-0774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lawlor DA, Tilling K, Davey Smith G. Triangulation in aetiological epidemiology. Int J Epidemiol. 2016;45(6):1866-1886. doi: 10.1093/ije/dyw314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gage SH, Davey Smith G, Ware JJ, Flint J, Munafò MR.G = E: what GWAS can tell us about the environment. PLoS Genet. 2016;12(2):e1005765. doi: 10.1371/journal.pgen.1005765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dudbridge F. Power and predictive accuracy of polygenic risk scores. PLoS Genet. 2013;9(3):e1003348. doi: 10.1371/journal.pgen.1003348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pingault J-B, O’Reilly PF, Schoeler T, Ploubidis GB, Rijsdijk F, Dudbridge F. Using genetic data to strengthen causal inference in observational research. Nat Rev Genet. 2018;19(9):566-580. doi: 10.1038/s41576-018-0020-3 [DOI] [PubMed] [Google Scholar]
- 22.Pingault J-B, Murray J, Munafo M, Viding E. Causal inference in psychopathology: using mendelian randomisation to identify environmental risk factors for psychopathology. Psychopathol Rev. 2017;4(1):4-25. doi: 10.5127/pr.038115 [DOI] [Google Scholar]
- 23.Du Rietz E, Coleman J, Glanville K, Choi SW, O’Reilly PF, Kuntsi J. Association of polygenic risk for attention-deficit/hyperactivity disorder with co-occurring traits and disorders. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(7):635-643. doi: 10.1016/j.bpsc.2017.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Power RA, Verweij KJH, Zuhair M, et al. . Genetic predisposition to schizophrenia associated with increased use of cannabis. Mol Psychiatry. 2014;19(11):1201-1204. doi: 10.1038/mp.2014.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jokela M, Elovainio M, Keltikangas-Järvinen L, et al. . Body mass index and depressive symptoms: instrumental-variables regression with genetic risk score. Genes Brain Behav. 2012;11(8):942-948. doi: 10.1111/j.1601-183X.2012.00846.x [DOI] [PubMed] [Google Scholar]
- 26.Derks EM, Vorstman JAS, Ripke S, Kahn RS, Ophoff RA; Schizophrenia Psychiatric Genomic Consortium . Investigation of the genetic association between quantitative measures of psychosis and schizophrenia: a polygenic risk score analysis. PLoS One. 2012;7(6):e37852. doi: 10.1371/journal.pone.0037852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jansen PR, Polderman TJC, Bolhuis K, et al. . Polygenic scores for schizophrenia and educational attainment are associated with behavioural problems in early childhood in the general population. J Child Psychol Psychiatry. 2018;59(1):39-47. doi: 10.1111/jcpp.12759 [DOI] [PubMed] [Google Scholar]
- 28.Riglin L, Eyre O, Cooper M, et al. . Investigating the genetic underpinnings of early-life irritability. Transl Psychiatry. 2017;7(9):e1241. doi: 10.1038/tp.2017.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krapohl E, Patel H, Newhouse S, et al. . Multi-polygenic score approach to trait prediction. Mol Psychiatry. 2018;23(5):1368-1374. doi: 10.1038/mp.2017.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdellaoui A, Nivard MG, Hottenga J-J, et al. . Predicting loneliness with polygenic scores of social, psychological and psychiatric traits. Genes Brain Behav. 2018;17(6):e12472. doi: 10.1111/gbb.12472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boyd A, Golding J, Macleod J, et al. . Cohort profile: the “children of the 90s”—the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42(1):111-127. doi: 10.1093/ije/dys064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fraser A, Macdonald-Wallis C, Tilling K, et al. . Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol. 2013;42(1):97-110. doi: 10.1093/ije/dys066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bristol University Avon Longitudinal Study of Parents and Children: Data and Samples. http://www.bristol.ac.uk/alspac/researchers/our-data/. Accessed January 3, 2019.
- 34.Euesden J, Lewis CM, O’Reilly PF. PRSice: polygenic risk score software. Bioinformatics. 2015;31(9):1466-1468. doi: 10.1093/bioinformatics/btu848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benjamini Y, Drai D, Elmer G, Kafkafi N, Golani I. Controlling the false discovery rate in behavior genetics research. Behav Brain Res. 2001;125(1-2):279-284. doi: 10.1016/S0166-4328(01)00297-2 [DOI] [PubMed] [Google Scholar]
- 36.Team RCR. A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 37.Riglin L, Hammerton G, Heron J, et al. . Developmental contributions of schizophrenia risk alleles and childhood peer victimization to early-onset mental health trajectories. Am J Psychiatry. 2018;176(1):p201818010075. doi: 10.1176/appi.ajp.2018.18010075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: ‘much ado about nothing’? Psychol Med. 2010;40(5):717-729. doi: 10.1017/S0033291709991383 [DOI] [PubMed] [Google Scholar]
- 39.Vaillancourt T, Brittain HL, McDougall P, Duku E. Longitudinal links between childhood peer victimization, internalizing and externalizing problems, and academic functioning: developmental cascades. J Abnorm Child Psychol. 2013;41(8):1203-1215. doi: 10.1007/s10802-013-9781-5 [DOI] [PubMed] [Google Scholar]
- 40.Acquah EO, Topalli P-Z, Wilson ML, Junttila N, Niemi PM. Adolescent loneliness and social anxiety as predictors of bullying victimisation. Int J Adolesc Youth. 2016;21(3):320-331. doi: 10.1080/02673843.2015.1083449 [DOI] [Google Scholar]
- 41.Whelan YM, Kretschmer T, Barker ED. MAOA, early experiences of harsh parenting, irritable opposition, and bullying-victimization: a moderated indirect-effects analysis. Merrill-Palmer Q. 2014;60(2):217. doi: 10.13110/merrpalmquar1982.60.2.0217 [DOI] [Google Scholar]
- 42.Jones HJ, Heron J, Hammerton G, et al. ; 23 and Me Research Team . Investigating the genetic architecture of general and specific psychopathology in adolescence. Transl Psychiatry. 2018;8(1):145. doi: 10.1038/s41398-018-0204-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burgess S, Daniel RM, Butterworth AS, Thompson SG; EPIC-InterAct Consortium . Network mendelian randomization: using genetic variants as instrumental variables to investigate mediation in causal pathways. Int J Epidemiol. 2015;44(2):484-495. doi: 10.1093/ije/dyu176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Connolly EJ, Beaver KM. Considering the genetic and environmental overlap between bullying victimization, delinquency, and symptoms of depression/anxiety. J Interpers Violence. 2016;31(7):1230-1256. doi: 10.1177/0886260514564158 [DOI] [PubMed] [Google Scholar]
- 45.Ball HA, Arseneault L, Taylor A, Maughan B, Caspi A, Moffitt TE. Genetic and environmental influences on victims, bullies and bully-victims in childhood. J Child Psychol Psychiatry. 2008;49(1):104-112. doi: 10.1111/j.1469-7610.2007.01821.x [DOI] [PubMed] [Google Scholar]
- 46.Jaffee SR, Price TS. Gene-environment correlations: a review of the evidence and implications for prevention of mental illness. Mol Psychiatry. 2007;12(5):432-442. doi: 10.1038/sj.mp.4001950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bates TC, Maher BS, Medland SE, et al. . The nature of nurture: using a virtual-parent design to test parenting effects on children’s educational attainment in genotyped families. Twin Res Hum Genet. 2018;21(2):73-83. doi: 10.1017/thg.2018.11 [DOI] [PubMed] [Google Scholar]
- 48.Cogan JC, Bhalla SK, Sefa-Dedeh A, Rothblum ED. A comparison study of United States and African students on perceptions of obesity and thinness. J Cross Cult Psychol. 1996;27(1):98-113. doi: 10.1177/0022022196271007 [DOI] [Google Scholar]
- 49.Kärnä A, Voeten M, Little TD, Poskiparta E, Kaljonen A, Salmivalli C. A large-scale evaluation of the KiVa antibullying program: grades 4-6. Child Dev. 2011;82(1):311-330. doi: 10.1111/j.1467-8624.2010.01557.x [DOI] [PubMed] [Google Scholar]
- 50.Olweus D, Limber SP. Bullying in school: evaluation and dissemination of the Olweus Bullying Prevention Program. Am J Orthopsychiatry. 2010;80(1):124-134. doi: 10.1111/j.1939-0025.2010.01015.x [DOI] [PubMed] [Google Scholar]
- 51.Puhl RM, Neumark-Sztainer D, Austin SB, Luedicke J, King KM. Setting policy priorities to address eating disorders and weight stigma: views from the field of eating disorders and the US general public. BMC Public Health. 2014;14(1):524. doi: 10.1186/1471-2458-14-524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gaffney H, Ttofi MM, Farrington DP. Evaluating the effectiveness of school-bullying prevention programs: an updated meta-analytical review [published online July 20, 2018]. Aggress Violent Behav. [Google Scholar]
- 53.Knopik VS, Neiderhiser JM, DeFries JC, Plomin R. Behavioral Genetics. 7th ed New York, NY: Worth Publishers; 2016. [Google Scholar]
- 54.Colarossi LG, Eccles JS. A prospective study of adolescents’ peer support: gender differences and the influence of parental relationships. J Youth Adolesc. 2000;29(6):661-678. doi: 10.1023/A:1026403922442 [DOI] [Google Scholar]
- 55.Davidson LM, Demaray MK. Social support as a moderator between victimization and internalizing-externalizing distress from bullying. School Psych Rev. 2007;36(3):383. [Google Scholar]
- 56.Bulik-Sullivan B, Finucane HK, Anttila V, et al. ; ReproGen Consortium; Psychiatric Genomics Consortium; Genetic Consortium for Anorexia Nervosa of the Wellcome Trust Case Control Consortium 3 . An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47(11):1236-1241. doi: 10.1038/ng.3406 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Genotyping and Quality Control Procedures, Polygenic Scores, and Analysis
eDiscussion. Insights and Interpretations
eTable 1. Early Participant Characteristics for Nonincluded vs Included Individuals
eTable 2. Bullying and Friendship Interview Schedule
eTable 3. Overview GWAS Summary Statistics
eTable 4. Pearson Correlation Estimates Between Polygenic Scores
eTable 5. Multivariable Logistic Regression Analysis (Sex Excluded)
eTable 6. Multivariable Logistic Regression Analysis (Sex Included)
eTable 7. Single-PRS Prediction of Exposure to Bullying
eTable 8. Multi-PRS Prediction of Exposure to Bullying
eTable 9. Sensitivity Analyses on the Restricted Multi-PGS Regression Model
eTable 10. Linear Regression Models Testing for Interaction Effects With Sex
eReferences