Abstract
This cohort study examines the incidence of mortality 1 year after the start of hemodialysis in patients 65 years and older.
Shared decision making about dialysis, a potentially burdensome or harmful treatment for older adults, requires accurate estimates of prognosis.1 More than 120 000 people in the United States initiated chronic dialysis in 2015, half of whom were older than 65 years.2 The 1-year mortality rate after dialysis initiation for these older adults, based on the United States Renal Data System (USRDS) registry, is currently approximately 30%.2 However, the USRDS does not include all patients who start dialysis—most notably omitting those who die before an outpatient dialysis provider enters them into the registry. Therefore, USRDS-based mortality estimates are not generalizable to all patients who initiate dialysis. Registry data also lack detailed information on functional and cognitive status, which can significantly affect treatment decisions and outcomes. Thus, existing data2,3 may not provide optimal support for real-time decision making about dialysis initiation in older adults. To address these knowledge gaps, we used data from the Health and Retirement Study, a nationally representative, longitudinal survey of older adults, to describe mortality within the first year after dialysis initiation.
Methods
Using Health and Retirement Study data from April 3, 1998, to December 21, 2014, linked to Medicare claims and the National Death Index, we identified all patients 65.5 years and older with fee-for-service Medicare and an initial claim for dialysis. Data analysis was performed from January 5, 2017, to December 19, 2018. The institutional review board at Icahn School of Medicine at Mount Sinai approved this study and granted a waiver of informed consent.
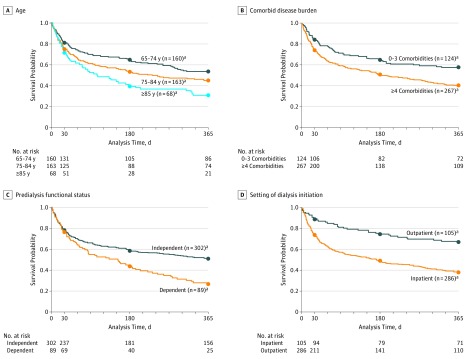
We calculated mortality at 30, 180, and 365 days after dialysis initiation and estimated 1-year Kaplan-Meier survival curves by age, comorbidity, predialysis functional status, and dialysis initiation setting. To identify characteristics independently associated with mortality at each time, we built parsimonious multivariate, complementary log-log regression models. A P value less than .05 determined with unpaired, 2-tailed testing was considered significant. Analyses were conducted in SAS, version 9.4 (SAS Institute Inc) and Stata, version 15 (Stata Corp).
Results
Among 391 Medicare beneficiaries initiating dialysis, 68 patients (17.4%) were 85 years or older, 89 patients (22.8%) required assistance with 1 or more activities of daily living, 267 patients (68.3%) had 4 or more comorbidities, and 286 patients (73.1%) started dialysis in the hospital (Table). Death occurred in 88 patients (22.5%) within 30 days after starting dialysis, 173 (44.2%) within 180 days, and 213 (54.5%) within 365 days. At 1 year, 65 of 89 patients (73.0%) with activity of daily living dependence, 48 of 68 patients (70.6%) 85 years or older, and 178 of 286 patients (62.2%) initiating dialysis as inpatients had died (Figure). After multivariate adjustment, factors significantly associated with higher 1-year mortality included activity of daily living dependence (hazard ratio [HR], 1.88; 95% CI, 1.36-2.61; P ≤ .001), age 85 years or older (HR, 1.85; 95% CI, 1.23-2.80; P = .003), inpatient dialysis initiation (HR, 2.17; 95% CI, 1.49-3.15; P ≤ .001), and having 4 or more comorbidities (HR, 1.50; 95% CI, 1.07-2.09; P = .02).
Table. Mortality Rates Stratified by Patient Characteristics (N = 391).
| Characteristic | Total, No. (%)a | Died Within 30 Days (n = 88 [22.5%]) | Died Within 180 Days (n = 173 [44.2%]) | Died Within 365 Days (n = 213 [54.5%]) |
|---|---|---|---|---|
| Age at dialysis initiation, y | ||||
| 65-74 | 160 (40.9) | 30 (18.7) | 56 (35.0) | 75 (46.9)b |
| 75-84 | 163 (41.7) | 39 (23.9) | 76 (46.6)b | 90 (55.2)b |
| ≥85 | 68 (17.4) | 19 (27.9) | 41 (60.3)b | 48 (70.6)b |
| Sex | ||||
| Male | 185 (47.3) | 42 (22.7) | 85 (46.0) | 107 (57.8) |
| Female | 206 (52.7) | 46 (22.3) | 88 (42.7) | 106 (51.5) |
| Race/ethnicity | ||||
| Non-Hispanic white | 257 (65.7) | 62 (24.1) | 121 (47.1) | 151 (58.8)b |
| Not white | 134 (34.3) | 26 (19.4) | 52 (38.8) | 62 (46.3)b |
| High school graduate | ||||
| Yes | 222 (56.8) | 54 (24.3) | 97 (43.7) | 118 (53.2) |
| No | 169 (43.2) | 34 (20.1) | 76 (45.0) | 95 (56.2) |
| Body mass indexc,d | ||||
| >25 | 269 (69.9) | 53 (19.7)b | 115 (42.8) | 142 (52.8) |
| <25 | 116 (30.1) | 34 (29.3)b | 57 (49.1) | 70 (60.3) |
| No. of comorbiditiesc | ||||
| 0-3 | 124 (31.7) | 19 (15.3)b | 43 (34.7)b | 53 (42.7)b |
| ≥4 | 267 (68.3) | 69 (25.8)b | 130 (48.7)b | 160 (59.9)b |
| Nursing home residentc | ||||
| No | 361 (92.3) | NRe | 154 (42.7)b | 190 (52.6)b |
| Yes | 30 (7.7) | <11f | 19 (63.3)b | 23 (76.7)b |
| Incident dialysis location | ||||
| Outpatient | 105 (26.9) | 12 (11.4)b | 27 (25.7)b | 35 (33.3)b |
| Inpatient | 286 (73.1) | 76 (26.6)b | 146 (51.0)b | 178 (62.2)b |
| Self-reported healthc,g | ||||
| Good/very good/excellent | 141 (36.1) | 30 (21.3) | 58 (41.1) | 73 (51.8) |
| Poor/fair | 248 (63.8) | 58 (23.4) | 115 (46.4) | 139 (56.0) |
| Cognitive statusc | ||||
| Not dementia | 322 (82.4) | 67 (20.8) | 134 (41.6)b | 169 (52.5) |
| Dementia | 69 (17.7) | 21 (30.4) | 39 (56.5)b | 44 (63.8) |
| Predialysis functional statusc | ||||
| Independent for all ADLs | 302 (77.2) | 67 (22.2) | 123 (40.7)b | 148 (49.0)b |
| Any ADL dependence | 89 (22.8) | 21 (23.6) | 50 (56.2)b | 65 (73.0)b |
Abbreviation: ADL, activities of daily living.
Percentages have been rounded and, therefore, might not total 100.
P ≤ .05 from Fisher exact test of characteristic and within-time-frame mortality.
Ascertained at the interview prior to dialysis initiation.
Missing for 6 participants who were therefore dropped from the regression model.
Not reportable because it would result in complementary disclosure of exact sample size less than 11.
Health and Retirement Study guidelines do not permit reporting exact sample sizes when number is less than 11.
Missing for 2 participants.
Figure. One-Year, Unadjusted Survival Curves .
Mortality for age (A), comorbidity (B), predialysis functional status (C), and setting of dialysis initiation (D) across the study.
aSample size at time of dialysis initiation.
Discussion
Drawing on nationally representative data, we found that 22.5% of Medicare beneficiaries initiating dialysis died within 30 days, 44.2% died within 6 months, and 54.5% died within 1 year—almost double the 1-year mortality rate reported for older adults in the USRDS registry.2 The oldest patients, non-Hispanic white patients, those with predialysis activity of living dependence or a high burden of comorbidity, and those who started dialysis in the hospital fared the worst.
These results provide a complement to data from the USRDS registry. By more closely approximating real-world clinical situations in which it cannot be known whether patients will require chronic dialysis and whether they will survive long enough to enter the USRDS registry, these results may further support shared decision making regarding dialysis initiation. Our findings also may support the importance of age, race, comorbidity burden, functional status, and site of dialysis initiation in estimating subsequent mortality among older adults.1,3,4,5,6
Several limitations must be considered. First, although drawing on a nationally representative cohort of older adults, the study’s subset of Medicare beneficiaries who initiated dialysis was small, offered limited power, and may not fully represent the population starting dialysis. Second, these data cannot describe survival among the counterfactual group of older adults with advanced kidney disease who did not start dialysis.
The limited survival among older patients who initiated dialysis may help to frame prognostic expectations and support more informative discussions about dialysis initiation in older adults.
References
- 1.Moss AH. Renal Physicians Association Clinical Practice Guideline on Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis. 2nd ed Rockville, Maryland: Renal Physicians Association; 2010. [Google Scholar]
- 2.2017 USRDS Annual Data Report: Epidemiology Of Kidney Disease in the United States. Bethesda, MD: Renal Physicians Association 2017. [Google Scholar]
- 3.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361(16):1539-1547. doi: 10.1056/NEJMoa0904655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Couchoud CG, Beuscart J-BR, Aldigier J-C, Brunet PJ, Moranne OP; REIN registry . Development of a risk stratification algorithm to improve patient-centered care and decision making for incident elderly patients with end-stage renal disease. Kidney Int. 2015;88(5):1178-1186. doi: 10.1038/ki.2015.245 [DOI] [PubMed] [Google Scholar]
- 5.Yu MK, Wong SPY, Liu CF, Hebert PL, O’Hare AM. Clinical presentation at initiation of maintenance dialysis and subsequent survival: A retrospective cohort study. Hemodial Int. 2019;23(1):106-116. [DOI] [PubMed] [Google Scholar]
- 6.Kucirka LM, Grams ME, Lessler J, et al. . Association of race and age with survival among patients undergoing dialysis. JAMA. 2011;306(6):620-626. doi: 10.1001/jama.2011.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]