This analysis of all US military casualties in Afghanistan and Iraq from October 2001 through December 2017 assesses the association of trends in survival with advances in initial battlefield interventions.
Key Points
Question
What were the main factors associated with reductions in mortality during the current conflicts in Afghanistan and Iraq?
Findings
This analysis of all US military casualties from October 2001 through December 2017 found that survival among the most critically injured casualties increased 3-fold during the course of the conflicts and that 3 key interventions (tourniquets, blood transfusions, and prehospital transport within 60 minutes) were associated with 44% of mortality reduction.
Meaning
Across 16 years of conflict, military trauma system advancements, namely, improvements in methods to control bleeding, replace blood, and reduce time to treatment, may be associated with increased survival of battle casualties.
Abstract
Importance
Although the Afghanistan and Iraq conflicts have the lowest US case-fatality rates in history, no comprehensive assessment of combat casualty care statistics, major interventions, or risk factors has been reported to date after 16 years of conflict.
Objectives
To analyze trends in overall combat casualty statistics, to assess aggregate measures of injury and interventions, and to simulate how mortality rates would have changed had the interventions not occurred.
Design, Setting, and Participants
Retrospective analysis of all available aggregate and weighted individual administrative data compiled from Department of Defense databases on all 56 763 US military casualties injured in battle in Afghanistan and Iraq from October 1, 2001, through December 31, 2017. Casualty outcomes were compared with period-specific ratios of the use of tourniquets, blood transfusions, and transport to a surgical facility within 60 minutes.
Main Outcomes and Measures
Main outcomes were casualty status (alive, killed in action [KIA], or died of wounds [DOW]) and the case-fatality rate (CFR). Regression, simulation, and decomposition analyses were used to assess associations between covariates, interventions, and individual casualty status; estimate casualty transitions (KIA to DOW, KIA to alive, and DOW to alive); and estimate the contribution of interventions to changes in CFR.
Results
In aggregate data for 56 763 casualties, CFR decreased in Afghanistan (20.0% to 8.6%) and Iraq (20.4% to 10.1%) from early stages to later stages of the conflicts. Survival for critically injured casualties (Injury Severity Score, 25-75 [critical]) increased from 2.2% to 39.9% in Afghanistan and from 8.9% to 32.9% in Iraq. Simulations using data from 23 699 individual casualties showed that without interventions assessed, CFR would likely have been higher in Afghanistan (15.6% estimated vs 8.6% observed) and Iraq (16.3% estimated vs 10.1% observed), equating to 3672 additional deaths (95% CI, 3209-4244 deaths), of which 1623 (44.2%) were associated with the interventions studied: 474 deaths (12.9%) (95% CI, 439-510) associated with the use of tourniquets, 873 (23.8%) (95% CI, 840-910) with blood transfusion, and 275 (7.5%) (95% CI, 259-292) with prehospital transport times.
Conclusions and Relevance
Our analysis suggests that increased use of tourniquets, blood transfusions, and more rapid prehospital transport were associated with 44.2% of total mortality reduction. More critically injured casualties reached surgical care, with increased survival, implying improvements in prehospital and hospital care.
Introduction
“The only winner in war is medicine.”1 Indeed, many medical advances have originated or been propagated during warfare. Tourniquets to control bleeding were used on the battlefield2,3,4 as far back as 326 bce during Alexander the Great’s invasion of Persia.5 Rapid and efficient evacuation of wounded soldiers was pioneered by Larrey6 in 1793 and further refined by Letterman during the American Civil War.6,7 Refinements of casualty triage and evacuation, as well as blood replacement, continued in World War I, when it was also observed that decreasing time to treatment increased survival.6,8 Improvements in reducing time to treatment continued during World War II6 and the Korea and Vietnam conflicts with helicopter transport of casualties and mobile army surgical hospitals.6 For recent conflicts in Afghanistan and Iraq, evolving tactical combat casualty care (TCCC)9 guidelines again reduced time to treatment by promoting the deployment of resources and trained first responder personnel10,11 close to the point of injury12,13 on the battlefield, particularly for bleeding control14,15,16 and blood replacement.15,17,18,19,20
The case-fatality rate (CFR) for Afghanistan and Iraq was first reported to be the lowest in US military history in 2004.21 However, there has been no assessment of combat casualty care statistics or major interventions encompassing the entirety of the conflicts to date. Thus, for military operations in Afghanistan and Iraq from 2001 through 2017, our goals were to analyze trends in overall combat casualty statistics; assess associations between individual and aggregate measures of injury, medical and nonmedical interventions, and mortality; and estimate what the CFR would have been if changes in interventions had not occurred.
Methods
Design and Study Setting
Retrospective analysis was conducted of all US combat casualties in Afghanistan and Iraq from October 1, 2001, through December 31, 2017. This project was determined by the US Department of Defense Joint Trauma System human subjects research determination officer to be research not involving human subjects as defined in Protection of Human Subjects (32 CFR §219.101[b][4]).
Data Sources
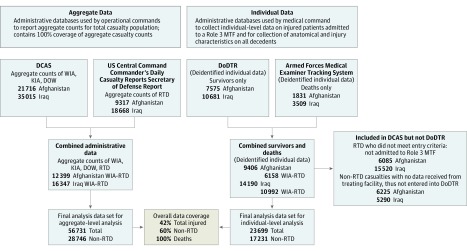
Data for US combat casualties were compiled from 4 Department of Defense databases: the Defense Manpower Data Center Defense Casualty Analysis System, the Joint Trauma System Department of Defense Trauma Registry (DoDTR), the Armed Forces Medical Examiner Tracking System (AFMETS), and the US Central Command Commander’s Daily Secretary of Defense Casualty Reports. A data flow diagram is presented in Figure 1.
Figure 1. Data Flow Diagram.
Wounded in action (WIA), killed in action (KIA), died of wounds (DOW), and returned to duty (RTD) are administratively determined categories, not medically determined designations. Killed in action and DOW are designations meant to distinguish administratively between deaths occurring before a casualty reaches a treatment facility (KIA) and after reaching a treatment facility (DOW). CFR indicates case-fatality rate; DCAS, Defense Casualty Analysis System; DoDTR, Department of Defense Trauma Registry; and MTF, military treatment facility.
Aggregate Combat Casualty Care Statistics
Casualties in the Defense Manpower Data Center Defense Casualty Analysis System were administratively defined as either (1) killed in action (KIA) (ie, died before reaching a medical treatment facility) or (2) wounded in action (ie, reached a military treatment facility alive). Wounded in action casualties were further categorized as either died of wounds (DOW), died after reaching a medical treatment facility, or alive. Three standard combat casualty care statistics22 were calculated from these groups: CFR, percentage KIA, and percentage DOW by using the following equations:
| CFR = [(KIA + DOW)/(KIA + WIA)] × 100, |
| %KIA = {KIA/[KIA + (WIA − RTD)]} × 100, and |
| %DOW = [DOW/(WIA − RTD)] × 100. |
Survival rates for critically injured individuals with an Injury Severity Score (ISS) (rated as mild, 1-9; moderate, 10-15; severe, 16-24; and critical, 25-75) of 25 to 75 were calculated as follows:
| %Survival for ISS of 25-75 = [AliveISS, 25-75/(WIAISS, 25-75 + KIAISS, 25-75)] × 100. |
Measures of Injury Characteristics, Severity, and Interventions
Deidentified, individual-level data for 23 699 casualties were obtained from DoDTR and AFMETS for casualties who either survived and met criteria for entry into DoDTR or died (KIA or DOW) and were entered into AFMETS (Figure 1). The outcome for individual-level analyses was defined as KIA, DOW, or alive based on DoDTR and AFMETS casualty status designations. Demographic variables included age in years, sex, and branch of service (Air Force, Army, Coast Guard, Marines, or Navy). Measures of injury characteristics included body regions (head, neck, chest, abdomen, extremity, or external) coded as 6 non–mutually exclusive indicators,18 3 categories of mechanism of injury (MOI) (explosion, gunshot, or other), and 4 categories of ISS (mild, 1-9; moderate, 10-15; severe, 16-24; and critical, 25-75).18,23 Interval-level ISS was calculated using the civilian Abbreviated Injury Scale (AIS), 2005 revision.24
Intervention measures were not available at the individual level for deceased casualties; therefore, period-specific aggregate percentages of casualties who received tourniquets, blood transfusion, and prehospital transport within 60 minutes were used. These measures reflect changes in trauma system practice rather than individual patient intervention. Tourniquet use was measured as the percentage of casualties with extremity injuries with a tourniquet placed. Blood product transfusion was measured as the percentage of casualties who received at least 1 U of blood product during prehospital transport or at an in-theater surgical facility. Prehospital transport times were measured as the percentage of casualties transported to initial surgical capability within 60 minutes.
Statistical Analysis
Aggregate combat casualty care statistics, including CFR, %DOW, and %KIA as well as percentage of survival with ISS of 25 to 75 (critical) are reported graphically as quarterly trends smoothed by cubic splines. Individual data were proportionally weighted25 to total population counts based on Defense Casualty Analysis System data to account for selection bias17 (details are in the eAppendix in the Supplement).
Multivariable multinomial logistic regression models were used to analyze associations between all patient-level covariates and the outcome (KIA, DOW, or alive). Models were fit as generalized linear mixed models to account for individual-level and aggregate-level data. Simulation analysis was performed for Afghanistan and Iraq to estimate casualty transitions from KIA to DOW, from KIA to alive, and from DOW to alive and the corresponding CFR, %DOW, and %KIA under the counterfactual scenario26,27 that tourniquets, blood transfusions, and prehospital transport times remained unchanged from the early stages of each conflict. Case-fatality rates peaked in Afghanistan between October 2001 and June 2006 and in Iraq between March and December 2003; these periods reflect early stages of the conflicts (“early period”), when the use of tourniquets and other interventions were at their lowest. The periods from July 2006 through June 2009, in Afghanistan, and from January 2004 through December 2007, reflect initial trauma system responses and ongoing efforts to adapt to the evolving medical needs of each conflict (“middle period”). The periods from July 2009 through December 2017 in Afghanistan and from January 2008 through December 2017 reflect later stages of each conflict generally defined by broader implementation of trauma system standards of care, as well as operational and policy decisions, which ultimately led to de-escalation and troop withdrawals in Iraq and implementation of changes to policy and operational tactics in Afghanistan, including Secretary of Defense mandated reduction of prehospital transport times to 60 minutes or less18 (“late period”). Consequently, these period cutoffs were used to create a pre-post analysis design for simulation. Rate-difference decomposition methods were used to estimate the relative contribution of each factor to the difference between expected and actual casualty status28 (details are in the eAppendix in the Supplement). Descriptive analysis, regression, simulations, and decompositions were performed in SAS, version 9.4 (SAS Institute Inc). Statistical significance was set at .05 based on 2-sided P values.
Results
Aggregate-Level Analyses
Combat Casualty Care Statistics
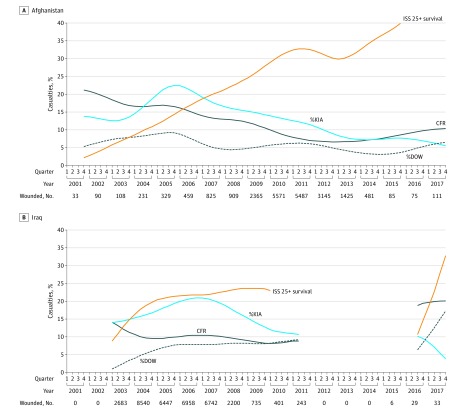
Aggregate mortality statistics for 56 763 total casualties are reported as cubic spline-smoothed quarterly trends (Figure 2) (more details can be found in the eAppendix and eTable 1 in the Supplement). Case-fatality rate was high during early periods of both conflicts and improved over time. As of December 31, 2017, the overall CFR in Afghanistan was 8.6%, down from its peak of 20.0% at the onset in October 2001; in Iraq, it was 10.1%, down from its peak of 20.4% in March 2003 (Figure 2). Concurrently, the percentage of survival with an ISS of 25 to 75 (critical) increased from 8.9% to 32.9% by the end of 2017 in Iraq, and from 2.2% in 2001 to 39.9% by the end of 2017 in Afghanistan (Figure 2). Critically injured casualties accounted for 16.2% of casualties and 90.1% of combat deaths overall in Afghanistan, and 16.4% of casualties and 90.5% of combat deaths overall in Iraq (eFigure 1 in the Supplement).
Figure 2. Trends in Combat Casualty Care Statistics.
Percentage survival for critically injured casualties (ISS [Injury Severity Score], 25-75 [ISS 25+]) for Afghanistan (A) and Iraq (B) by using cubic spline estimations smoothed over time from October 2001 through December 2017. The y-axis indicates percentage of casualties. The plot for ISS 25+ survival is truncated for Afghanistan after 2015 and for Iraq after 2009 owing to small sample sizes, which generated unstable spline estimates. The gap in data for Iraq between 2011 and 2016 reflects the absence of combat operations during this period. CFR indicates case-fatality rate; %KIA, percentage who were killed in action; and %DOW, percentage who died of wounds.
Injury Characteristics and Major Intervention Trends
Injury patterns, including body region, MOI, and ISS, changed over the course of both conflicts (Table 1). The percentage of casualties with head injuries doubled in Afghanistan from 30.3% during the early period (October 2001 to June 2006) to 59.0% during the late period (July 2009 to December 2017) and increased by a factor of 2.5, from 20.9% during the early period (March 2003 to December 2003) to 53.0% during the late period (January 2008 to December 2017), in Iraq. Traumatic amputation increased in Afghanistan by 28%, from 9.2% (early period) to 11.8% (late period), but decreased slightly in Iraq, from 8.1% (early period) to 7.7% (late period). Explosive MOI increased from 61.4% (early period) to 80.5% during the middle period (July 2006 to June 2009) in Afghanistan and then decreased slightly to 77.4% (late period). In Iraq, explosive MOI increased from 70.1% (early period) to 79.8% (late period). Injury Severity Scores increased over time in Iraq (Table 1) but increased and decreased cyclically in Afghanistan (eAppendix and eFigure 2C in the Supplement). Use of tourniquets for individuals with extremity injuries increased from 13.8% (early period) to 34.1% (late period) in Afghanistan and from 2.3% (early period) to 18.5% (late period) in Iraq (Table 1 and eFigure 3 in the Supplement). Blood transfusion increased from 6.5% (early period) to 19.4% (late period) in Afghanistan and from 4.4% (early period) to 10.8% (late period) in Iraq. Transport to surgical capability within 60 minutes increased substantially in Afghanistan, from 17.5% (early period) to 76.3% (late period), and was consistently high in Iraq, from 66.0% (early period) to 75.9% (late period) (Table 1 and eFigure 3 in the Supplement).
Table 1. Population-Weighted Injury Descriptionsa.
| Injury Characteristics | Afghanistan | Iraq | ||||
|---|---|---|---|---|---|---|
| Early | Middle | Late | Early | Middle | Late | |
| Oct 2001 to Jun 2006 |
Jul 2006 to Jun 2009 |
Jul 2009 to Dec 2017 |
Mar 2003 to Dec 2003 |
Jan 2004 to Dec 2007 |
Jan 2008 to Dec 2017 |
|
| Unweighted, No. | 699 | 2109 | 6621 | 1462 | 11 204 | 1604 |
| Weighted, No. | 1105 | 2593 | 18 199 | 2683 | 28 686 | 3646 |
| Body region (individual), % | ||||||
| Head | 30.3 | 58.8 | 59.0 | 20.9 | 34.8 | 53.0 |
| Face | 25.1 | 26.0 | 26.1 | 25.2 | 26.3 | 22.8 |
| Chest | 19.2 | 22.1 | 19.4 | 13.0 | 17.2 | 19.6 |
| Abdomen | 20.3 | 23.9 | 24.6 | 18.2 | 20.2 | 16.7 |
| Extremity | 51.1 | 47.4 | 50.0 | 47.0 | 50.9 | 45.0 |
| Traumatic amputation | 9.2 | 8.4 | 11.8 | 8.1 | 7.8 | 7.7 |
| Severe (AIS score, 3-6)b | 30.8 | 25.4 | 28.7 | 20.0 | 27.0 | 23.6 |
| External | 72.2 | 68.9 | 74.8 | 76.3 | 76.3 | 72.4 |
| Severe multiple-trauma (ISS 16-75) | 24.8 | 25.7 | 25.6 | 17.7 | 24.3 | 24.0 |
| Mechanism of injury (individual), % | ||||||
| Explosive | 61.4 | 80.5 | 77.4 | 70.1 | 78.7 | 79.8 |
| Gunshot | 29.1 | 17.9 | 21.2 | 18.4 | 18.1 | 16.6 |
| Otherc | 9.5 | 1.6 | 1.4 | 11.5 | 3.2 | 3.5 |
| Injury Severity Score (individual), % | ||||||
| 1-9 (Mild) | 56.3 | 59.0 | 58.2 | 66.3 | 55.8 | 59.6 |
| 10-15 (Moderate) | 15.8 | 12.6 | 14.7 | 12.8 | 16.9 | 13.9 |
| 16-24 (Severe) | 10.3 | 10.4 | 11.3 | 7.3 | 10.5 | 11.3 |
| 25-75 (Critical) | 17.7 | 18.0 | 15.8 | 13.6 | 16.8 | 15.2 |
| Mean (SD) | 14.5 (25.2) | 14.2 (25.0) | 12.9 (25.2) | 11.4 (22.8) | 13.8 (27.4) | 12.9 (25.2) |
| Interventions (aggregate), % | ||||||
| Tourniquet | 13.8 | 18.3 | 34.1 | 2.3 | 16.7 | 18.5 |
| Blood transfusion | 6.5 | 15.3 | 19.4 | 4.4 | 13.3 | 10.8 |
| Transport to surgical capability ≤60 min | 17.5 | 42.7 | 76.3 | 66.0 | 64.5 | 75.9 |
| Patient status (individual), % | ||||||
| Killed in action | 12.5 | 9.7 | 5.1 | 9.5 | 7.7 | 6.6 |
| Died of wounds | 3.3 | 2.3 | 2.1 | 2.0 | 2.3 | 3.1 |
| Survived | 84.3 | 88.0 | 92.8 | 88.5 | 90.0 | 90.1 |
Abbreviations: AIS, Abbreviated Injury Scale; ISS, Injury Severity Score.
Percentage of patients with injuries by body region, mechanism of injury, ISS, and patient status for Afghanistan and Iraq by major time periods from October 2001 through December 2017. Interventions are aggregate and all other variables are individual level.
The AIS is an anatomically based traumatic injury severity scoring system that classifies injuries by body region according to its relative severity on a 6-point scale (1 indicates minor; 6, maximal).24
Other injuries include blunt trauma injuries, such as falls, motor vehicle crashes, and aircraft crashes.
Individual-Level Analyses
Multivariable, multinomial logistic regression models (eAppendix and eTable 2 in the Supplement) were used to conduct simulations in which tourniquet use, blood transfusion, and transport times within 60 minutes were held to mean levels observed during early periods in Afghanistan and Iraq. The models suggest that each 10% increase in casualties transported to surgical capability within 60 minutes was associated with lower odds of KIA mortality in Afghanistan (odds ratio [OR], 0.89; 95% CI, 0.84-0.94; P < .001) but with a slight increase in odds of KIA mortality in Iraq (OR, 1.05; 95% CI, 1.02-1.08; P < .001). Each 10% increase in casualties who received a blood transfusion was associated with lower odds of DOW mortality in Afghanistan (OR, 0.75; 95% CI, 0.60-0.94; P = .01). However, the results for Iraq (OR, 0.84; 95% CI, 0.68-1.05; P = .11), were not statistically significant. Each 10% increase in casualties with extremity injuries who had tourniquets placed was associated with lower odds of KIA (OR, 0.85; 95% CI, 0.74-0.97; P = .02) and DOW (OR, 0.87; 95% CI, 0.74-1.01; P = .06) mortality in Iraq, although the findings for DOW were not statistically significant. Results of a sensitivity analysis indicated that collinearity between intervention variables (eTable 3 in the Supplement) was associated with P values of estimates closer to the null but had no association with the magnitude of OR estimates themselves (eAppendix and eTable 4 in the Supplement). Explosive MOI was associated with higher odds of KIA mortality in Afghanistan (OR, 1.34; 95% CI, 1.02-1.77; P = .04) and Iraq (OR, 2.14; 95% CI, 1.76-2.60; P < .001) and higher odds of DOW mortality in Iraq (OR, 1.72; 95% CI, 1.40-2.13; P < .001). Higher ISS was associated with greater odds of KIA and DOW mortality in Afghanistan and Iraq.
Furthermore, simulation results suggest transitions in casualty status distributions from KIA to DOW and alive and from DOW to alive (Table 2) were associated with changes in the interventions studied. Of simulated KIA in Afghanistan, 278 of 1692 patients (16.4%) survived and 300 (17.7%) were DOW. Similarly, of simulated KIA in Iraq, 450 of 3140 (14.3%) survived and 536 (17.1%) were DOW. Most casualties who were classified as DOW (300 of 431 [69.6%] in Afghanistan and 536 of 769 [69.7%] in Iraq) would have been classified as KIA under simulated conditions.
Table 2. Expected Casualty Status and Case-Fatality Rates in Afghanistan and Iraq With Early-Period Interventions Distributions Throughout vs Actual Casualty Status and Case-Fatality Rates.
| Intervention or Casualty Status by Conflict | Early Perioda | Late Periodb | |
|---|---|---|---|
| Observed | Expected | Observed | |
| Afghanistan | |||
| Intervention, No. | 1105 | NA | 20 792 |
| Tourniquet, % | 13.8 | NA | 32.1 |
| Blood transfusion, % | 6.5 | NA | 18.9 |
| Transport ≤60 min, % | 17.5 | NA | 72.1 |
| Casualty status | |||
| Killed in action | 12.5 | 8.1 | 5.9 |
| Died of wounds | 3.3 | 7.1 | 2.1 |
| Alive | 84.3 | 84.6 | 91.8 |
| Case-fatality rate | 15.7 | 15.4 | 8.2 |
| Iraq | |||
| Intervention, No. | 2683 | NA | 32 332 |
| Tourniquet, % | 2.3 | NA | 16.9 |
| Blood transfusion, % | 4.4 | NA | 10.8 |
| Transport ≤60 min, % | 66.0 | NA | 65.8 |
| Casualty status | |||
| Killed in action | 9.5 | 9.7 | 7.6 |
| Died of wounds | 2.0 | 6.9 | 2.4 |
| Alive | 88.5 | 83.4 | 90.1 |
| Case-fatality rate | 11.5 | 16.6 | 9.9 |
Abbreviation: NA, not applicable.
The early period is defined as October 2001 to June 2006 in Afghanistan and March 2003 to December 2003 in Iraq.
The late period is defined as July 2006 to December 2017 in Afghanistan and January 2004 to December 2017 in Iraq.
Under simulated conditions, the CFR would have been 15.6% (95% CI, 14.2%-16.5%) vs the actual CFR of 8.6% in Afghanistan (Table 3) and 16.3% (95% CI, 15.2%-17.3%) vs the actual CFR of 10.1% in Iraq (Table 3). This equates to an estimated 3672 (95% CI, 3209-4244) additional deaths, 1506 (95% CI, 1212-1711) in Afghanistan and 2166 (95% CI, 1997-2533) in Iraq, that would have occurred if the interventions studied had remained unchanged from the early periods of the conflicts. The interventions studied were associated with prevention of 1622 (95% CI, 1538-1712) estimated additional deaths, of which 474 (95% CI, 439-510) were associated with tourniquets, 873 (95% CI, 840-910) with blood transfusion, and 275 (95% CI, 259-292) with prehospital transport times, whereas 1450 (95% CI, 1416-1485) estimated additional deaths were associated with other factors, including MOI, body region of injury, and ISS, and 600 (95% CI, 571-630) were unexplained by these variables (Table 3). Overall, 1622 of 3672 (44.2%) estimated prevented deaths were associated with observed changes in the 3 interventions studied, 949 (63.0%) in Afghanistan and 673 (31.1%) in Iraq.
Table 3. Estimated Contribution of Interventions and Other Factors to the Difference in Deaths in Simulated Circumstances and Actual Deaths (Estimated Additional Deaths) From Rate-Difference Decomposition Procedure.
| Variable | Contribution, % (95% CI) | Estimated Additional Deaths, No. (95% CI) |
|---|---|---|
| Afghanistan | ||
| Extremity injuries with tourniquet | 15.9 (14.6 to 17.2) | 239 (220 to 259) |
| Received blood product transfusion | 28.6 (27.4 to 29.8) | 431 (413 to 455) |
| Transported within 60 min | 18.5 (17.5 to 19.5) | 279 (264 to 294) |
| Other factorsa | 34.8 (33.9 to 35.7) | 524 (511 to 538) |
| Unexplained | 2.2 (1.1 to 3.3) | 33 (17 to 50) |
| Subtotal | 100 | 1506 (1212 to 1711) |
| Iraq | ||
| Extremity injuries with tourniquet | 10.9 (10.1 to 11.6) | 235 (219 to 251) |
| Received blood product transfusion | 20.4 (19.7 to 21.0) | 442 (427 to 455) |
| Transported within 60 min | −0.2 (−0.2 to −0.1) | −4 (−5 to −2) |
| Other factors | 42.7 (41.8 to 43.7) | 926 (905 to 947) |
| Unexplained | 26.2 (25.6 to 26.8) | 567 (554 to 580) |
| Subtotal | 100 | 2166 (1997 to 2533) |
| Total | ||
| Extremity injuries with tourniquet | 12.9 (12.0 to 13.9) | 474 (439 to 510) |
| Received blood product transfusion | 23.8 (22.9 to 24.8) | 873 (840 to 910) |
| Transported within 60 min | 7.5 (7.1 to 8.0) | 275 (259 to 292) |
| Other factors | 39.5 (38.6 to 40.4) | 1450 (1416 to 1485) |
| Unexplained | 16.4 (15.6 to 17.2) | 600 (571 to 630) |
| Total | 100 | 3672 (3209 to 4244) |
Other factors includes age, sex, military service, branch, body region of injury, mechanism of injury, and Injury Severity Score.
Discussion
To our knowledge, this is the most complete compilation of combat casualty data and the first to report trends in combat casualty care statistics, major interventions, and mortality outcomes across 16 years of combat in Afghanistan and Iraq. The first of several key findings was that there was a greater than 3-fold increase in survival for the most critically injured casualties with ISSs of 25 or greater. Considering that greater than 90% of all combat deaths were among critically injured casualties, that a notable reduction in these casualty deaths occurred during a period when complex explosive injuries increased, and that there were steady increases in the proportion of critically injured casualties in Iraq and intermittent increases in Afghanistan, this is a substantial achievement.
Changes in Wounding Causes, Patterns, and Interventions
One hallmark of the current conflicts has been the increase in explosive devices as primary MOIs. Explosive injuries were associated with a 34.1% increase in odds of KIA death in Afghanistan and a 114% increase in odds of KIA death and 72% increase in odds of DOW death in Iraq (eAppendix and eTable 2 in the Supplement). The shift to a predominantly explosive injury mechanism was accompanied by a commensurate shift in wounding pattern and toward complex multiple-trauma injuries involving more than 1 body region.29
The military trauma system responded to changes in MOI and injury patterns by introducing new or improved devices to control bleeding. Simulation results suggest that increased use of tourniquets was associated with increased survival from traumatic extremity amputation or vascular injury. Early in the Afghanistan and Iraq conflicts, traumatic amputation was more life threatening because tourniquets were rarely used and bleeding control was not rapid enough. Although the tourniquet concept is centuries old, improvements in tourniquet effectiveness, ease of use, and increased availability at the point of injury developed during current conflicts helped to propagate their use and improve casualty survival.5,30
Consistent with other studies,17,18,19,20,31 our results indicate that increased use of blood transfusion was another important correlate of mortality reduction, more so in Afghanistan than Iraq. The reason for this difference is multifactorial and may include conflict duration, refinements in clinical practice guidelines over time, and a global trend toward reducing time to blood transfusion, particularly through prehospital use. Research conducted from 2003 to 2008 led to advances in component therapy32,33 and safer use of fresh whole blood.34,35,36 In turn, this advance benefited more casualties in Afghanistan as fighting continued and intensified there, whereas it diminished in Iraq.
Although prehospital transport times were consistently more rapid in Iraq, where more than two-thirds of all casualties and three-fourths of critical casualties19 were transported from the point of injury to surgical capability within 60 minutes, this was not so in Afghanistan. Before June 2009, when Secretary of Defense Robert Gates mandated prehospital transport times be reduced to 60 minutes or less, percentages of casualties transported within 60 minutes ranged from 17.5% to 42.7% (Table 1). After the mandate, the percentage of casualties meeting the 60-minute target increased rapidly to levels comparable to Iraq. Our findings suggest that, similar to previous reports,17,18 more rapid transport was associated with reduced odds of KIA death in Afghanistan (eAppendix and eTable 2 in the Supplement). The data also suggest that more rapid transport may have been associated with a small increase in odds of DOW death in Afghanistan but was offset by reductions in KIA and reduction in odds of DOW from tourniquet and blood transfusion practices. This finding supports the explanation that casualty distributions in Afghanistan shifted from KIA to DOW owing to the reduction of transport time and helps explain the slight increase in %DOW from 2008 through 2010,37 when %KIA decreased. Given that most casualties in Iraq were transported within 60 minutes, which did not change substantively over time, and that more critically injured patients who would have died at or near the point of injury were being evacuated faster in Iraq, the observed association with KIA death in Iraq may be confounded.19
Casualty Status Transitions and Reduced Mortality
The combination of intervention changes likely contributed to a shift in casualty distributions from KIA to DOW, from KIA to alive, and from DOW to alive status (Table 2). To our knowledge, this is the first report to estimate transitions of casualties who survived, but who in previous periods would have died as either KIA or DOW. This finding provides insight into how reductions in CFR and increased survival among the most critically injured patients were achieved. Approximately 90% of casualties who were estimated to be KIA under simulated conditions but who actually survived had ISSs of 25 or greater, and more than 90% of these individuals had severe multiple-trauma injuries, most of which included head, chest, and extremity injuries caused by an explosive mechanism (eAppendix and eTable 5 in the Supplement).
Results of simulations of casualty status distributions in Afghanistan suggest that 300 patients were DOW who would have been KIA previously, 278 survived who previously would have been KIA, 1312 survived who would have previously been DOW, and 84 died who would have previously survived. Similarly, in Iraq, 536 casualties were DOW who previously would have been KIA, 450 survived who previously would have been KIA, 1867 survived who would have previously been DOW, and 151 died who would have previously survived. These estimated casualty transitions equate to the prevention of 1506 additional fatalities in Afghanistan and 2166 additional fatalities in Iraq, a total of 3672 additional deaths that were prevented, of which 474 (12.9%) were associated with tourniquet use (239 in Afghanistan and 235 in Iraq), 873 (23.8%) with blood transfusion (431 in Afghanistan and 442 in Iraq), and 275 (7.5%) with prehospital transport times within 60 minutes (279 in Afghanistan and –4 in Iraq). In all, 44.2% of the reduction in mortality observed in Afghanistan (63.0%) and Iraq (31.1%) across the course of the conflicts to date was associated with improvements in these 3 interventions, whereas most of the remainder was associated with other covariates.
Simulations of the counterfactual scenario in which improvements in interventions did not occur suggest that there would have been a higher total CFR in both Afghanistan (15.4 simulation vs 8.2 actual) and Iraq (16.6 simulation vs 9.9 actual) during the middle and late periods. These results illustrate how changes in individual patient characteristics and outcomes both underlie and are masked by aggregate measures of CFR, %KIA, and %DOW. This underscores both the limitations of aggregate measures and why it is a mistake to make inferences about trauma system performance based on a single metric in isolation.21,37 The findings also demonstrate that comparisons with historical conflicts based on single metrics without accounting for differences in wounding causes and patterns, injury severity, and other factors is problematic.21,37
Strengths and Limitations
The great strength of this study is that it has achieved the highest level of individual-level data coverage, 60% of all non–returned to duty casualties, including all deaths recorded by AFMETS that are rarely included in military medical analyses, throughout more than 16 years of conflict in both Afghanistan and Iraq.
This analysis has several limitations. First, data describing individuals who died are limited to demographic characteristics, body region of injury, MOI, and severity. Data regarding interventions, including those analyzed herein, are not captured within AFMETS. Therefore, interventions had to be assessed using a multilevel mixed design, which limits individual variability in these factors. In addition, clinical need for tourniquets and blood transfusion could not be precisely ascertained. It is likely that other medical (eg, in-hospital care, coordinated trauma system, and hypothermia prevention) and nonmedical (eg, personal protective equipment, warfighter technology) factors played a role in reducing mortality, but adequate measurement does not currently exist for these. Second, DoDTR excludes many minor casualties classified as returned to duty. Therefore, the DoDTR data are biased toward more severely injured casualties. To adjust for this, we used inverse probability population weights; however, it is possible that our weighting strategy did not account for all potential biases between missing returned to duty casualties and those captured by DoDTR. Finally, we relied on administrative definitions of KIA and DOW, which may contain some casualties who are misclassified. Because the published literature lacks similar analyses from historical conflicts or the civilian sector, comparisons with other conflicts could not be made.
Conclusions
Case-fatality rates in Afghanistan and Iraq represent the lowest mortality in US military history. However, mortality was much higher at the outset of each conflict. Increased use of tourniquets, increased use of blood transfusion, and rapid prehospital transport times were associated with 44% of reductions in mortality. Given that the primary cause of death in combat trauma is hemorrhage,38 these findings are not surprising. The key lesson from 16 years of conflict is that military trauma system advancements may be associated with increased survival, echoing historical themes of continued improvements to hemorrhage control and blood replacement and reducing time to treatment.39
eAppendix. Supplemental Methods and Results
eTable 1. Overall Combat Casualty Care Statistics
eTable 2. Results of Multivariable, Multinomial Logistic Regression Analysis
eTable 3. Correlation Matrix for Intervention Variables
eTable 4. Results of Sensitivity Analysis of Multivariable, Multinomial Logistic Regression Analysis
eTable 5. Injury Characteristics of Patients Who Transitioned From KIA to DOW and From KIA and DOW to Alive
eFigure 1. Mortality for Critically Injured Patients With Injury Severity Score (ISS) of 25 or Higher
eFigure 2. Key Injury Descriptions
eFigure 3. Major Interventions and Policy Directives
References
- 1.Rosenfeld L. Four Centuries of Clinical Chemistry. New York, NY: Taylor & Francis; 1999. [Google Scholar]
- 2.Mabry RL. Tourniquet use on the battlefield. Mil Med. 2006;171(5):352-356. doi: 10.7205/MILMED.171.5.352 [DOI] [PubMed] [Google Scholar]
- 3.Schwartz AM. The historical development of methods of hemostasis. Surgery. 1958;44(3):604-610. [PubMed] [Google Scholar]
- 4.Welling DR, McKay PL, Rasmussen TE, Rich NM. A brief history of the tourniquet. J Vasc Surg. 2012;55(1):286-290. doi: 10.1016/j.jvs.2011.10.085 [DOI] [PubMed] [Google Scholar]
- 5.Kragh JF Jr, Swan KG, Smith DC, Mabry RL, Blackbourne LH. Historical review of emergency tourniquet use to stop bleeding. Am J Surg. 2012;203(2):242-252. doi: 10.1016/j.amjsurg.2011.01.028 [DOI] [PubMed] [Google Scholar]
- 6.Goniewicz M. Effect of military conflicts on the formation of emergency medical services systems worldwide. Acad Emerg Med. 2013;20(5):507-513. doi: 10.1111/acem.12129 [DOI] [PubMed] [Google Scholar]
- 7.Place RJ. The strategic genius of Jonathan Letterman: the relevancy of the American Civil War to current health care policy makers. Mil Med. 2015;180(3):259-262. doi: 10.7205/MILMED-D-14-00419 [DOI] [PubMed] [Google Scholar]
- 8.Stansbury LG, Hess JR. Blood transfusion in World War I: the roles of Lawrence Bruce Robertson and Oswald Hope Robertson in the “most important medical advance of the war”. Transfus Med Rev. 2009;23(3):232-236. doi: 10.1016/j.tmrv.2009.03.007 [DOI] [PubMed] [Google Scholar]
- 9.Butler FK Jr, Hagmann J, Butler EG. Tactical combat casualty care in special operations. Mil Med. 1996;161(suppl):3-16. doi: 10.1093/milmed/161.suppl_1.3 [DOI] [PubMed] [Google Scholar]
- 10.Kotwal RS, Montgomery HR, Kotwal BM, et al. . Eliminating preventable death on the battlefield. Arch Surg. 2011;146(12):1350-1358. doi: 10.1001/archsurg.2011.213 [DOI] [PubMed] [Google Scholar]
- 11.Kotwal RS, Montgomery HR, Miles EA, Conklin CC, Hall MT, McChrystal SA. Leadership and a casualty response system for eliminating preventable death. J Trauma Acute Care Surg. 2017;82(6S)(suppl 1):S9-S15. doi: 10.1097/TA.0000000000001428 [DOI] [PubMed] [Google Scholar]
- 12.Butler FK, Holcomb JB, Schreiber MA, et al. . Fluid resuscitation for hemorrhagic shock in tactical combat casualty care: TCCC guidelines change 14-01—2 June 2014. J Spec Oper Med. 2014;14(3):13-38. [DOI] [PubMed] [Google Scholar]
- 13.Kellerman A, Elster E, eds. Out of the Crucible: How the US Military Transformed Combat Casualty Care in Iraq and Afghanistan. Fort Sam Houston, TX: Borden Institute; 2017. [Google Scholar]
- 14.Kragh JF Jr, Walters TJ, Baer DG, et al. . Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1-7. doi: 10.1097/SLA.0b013e31818842ba [DOI] [PubMed] [Google Scholar]
- 15.Cannon JW. Hemorrhagic shock. N Engl J Med. 2018;378(19):1852-1853. [DOI] [PubMed] [Google Scholar]
- 16.Schroll R, Smith A, McSwain NE Jr, et al. . A multi-institutional analysis of prehospital tourniquet use. J Trauma Acute Care Surg. 2015;79(1):10-14. doi: 10.1097/TA.0000000000000689 [DOI] [PubMed] [Google Scholar]
- 17.Howard JT, Kotwal RS, Santos-Lazada AR, Martin MJ, Stockinger ZT. Reexamination of a battlefield trauma golden hour policy. J Trauma Acute Care Surg. 2018;84(1):11-18. doi: 10.1097/TA.0000000000001727 [DOI] [PubMed] [Google Scholar]
- 18.Kotwal RS, Howard JT, Orman JA, et al. . The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surg. 2016;151(1):15-24. doi: 10.1001/jamasurg.2015.3104 [DOI] [PubMed] [Google Scholar]
- 19.Kotwal RS, Scott LLF, Janak JC, et al. . The effect of prehospital transport time, injury severity, and blood transfusion on survival of US military casualties in Iraq. J Trauma Acute Care Surg. 2018;85(1S)(suppl 2):S112-S121. [DOI] [PubMed] [Google Scholar]
- 20.Shackelford SA, Del Junco DJ, Powell-Dunford N, et al. . Association of prehospital blood product transfusion during medical evacuation of combat casualties in Afghanistan with acute and 30-day survival. JAMA. 2017;318(16):1581-1591. doi: 10.1001/jama.2017.15097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gawande A. Casualties of war—military care for the wounded from Iraq and Afghanistan. N Engl J Med. 2004;351(24):2471-2475. doi: 10.1056/NEJMp048317 [DOI] [PubMed] [Google Scholar]
- 22.Holcomb JB, Stansbury LG, Champion HR, Wade C, Bellamy RF. Understanding combat casualty care statistics. J Trauma. 2006;60(2):397-401. doi: 10.1097/01.ta.0000203581.75241.f1 [DOI] [PubMed] [Google Scholar]
- 23.Performance improvement and patient safety In: Rotondo M, Cribari C, Smith S, eds. Resources for Optimal Care of the Injured Patient. 6th ed Chicago, IL: American College of Surgeons; 2014:114-133. https://www.facs.org/quality-programs/trauma/tqp/center-programs/vrc/resources. Accessed April 4, 2018. [Google Scholar]
- 24.Gennarelli TA, Wodzin E. AIS 2005: a contemporary injury scale. Injury. 2006;37(12):1083-1091. doi: 10.1016/j.injury.2006.07.009 [DOI] [PubMed] [Google Scholar]
- 25.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278-295. doi: 10.1177/0962280210395740 [DOI] [PubMed] [Google Scholar]
- 26.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861-1867. doi: 10.1001/jama.293.15.1861 [DOI] [PubMed] [Google Scholar]
- 27.Höfler M. Causal inference based on counterfactuals. BMC Med Res Methodol. 2005;5(28):28. doi: 10.1186/1471-2288-5-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fairlie R. An extension of the Blinder-Oaxaca decomposition technique to logit and probit models. J Econ Soc Meas. 2005;30(4):305-316. [Google Scholar]
- 29.DePalma RG, Burris DG, Champion HR, Hodgson MJ. Blast injuries. N Engl J Med. 2005;352(13):1335-1342. doi: 10.1056/NEJMra042083 [DOI] [PubMed] [Google Scholar]
- 30.Butler FK. Military history of increasing survival: the U.S. military experience with tourniquets and hemostatic dressings in the Afghanistan and Iraq conflicts. J Spec Oper Med. 2015;15(4):149-152. [DOI] [PubMed] [Google Scholar]
- 31.Sperry JL, Guyette FX, Brown JB, et al. ; PAMPer Study Group . Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med. 2018;379(4):315-326. doi: 10.1056/NEJMoa1802345 [DOI] [PubMed] [Google Scholar]
- 32.Spinella PC, Perkins JG, Grathwohl KW, et al. . Effect of plasma and red blood cell transfusions on survival in patients with combat related traumatic injuries. J Trauma. 2008;64(2)(suppl):S69-S77. doi: 10.1097/TA.0b013e318160ba2f [DOI] [PubMed] [Google Scholar]
- 33.Borgman MA, Spinella PC, Perkins JG, et al. . The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805-813. doi: 10.1097/TA.0b013e3181271ba3 [DOI] [PubMed] [Google Scholar]
- 34.Repine TB, Perkins JG, Kauvar DS, Blackborne L. The use of fresh whole blood in massive transfusion. J Trauma. 2006;60(6)(suppl):S59-S69. doi: 10.1097/01.ta.0000219013.64168.b2 [DOI] [PubMed] [Google Scholar]
- 35.Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66(4)(suppl):S69-S76. doi: 10.1097/TA.0b013e31819d85fb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chandler MH, Roberts M, Sawyer M, Myers G. The US military experience with fresh whole blood during the conflicts in Iraq and Afghanistan. Semin Cardiothorac Vasc Anesth. 2012;16(3):153-159. doi: 10.1177/1089253212452344 [DOI] [PubMed] [Google Scholar]
- 37.Nessen SC, Gurney J, Rasmussen TE, et al. . Unrealized potential of the US military battlefield trauma system: DOW rate is higher in Iraq and Afghanistan than in Vietnam, but CFR and KIA rate are lower. J Trauma Acute Care Surg. 2018;85(1S)(suppl 2):S4-S12. . doi: 10.1097/TA.0000000000001969 [DOI] [PubMed] [Google Scholar]
- 38.Eastridge BJ, Mabry RL, Seguin P, et al. . Death on the battlefield (2001-2011): implications for the future of combat casualty care [published correction appears in J Trauma Acute Care Surg. 2013;74(2):706]. J Trauma Acute Care Surg. 2012;73(6)(suppl 5):S431-S437. doi: 10.1097/TA.0b013e3182755dcc [DOI] [PubMed] [Google Scholar]
- 39.Cannon JW. Prehospital damage-control resuscitation. N Engl J Med. 2018;379(4):387-388. doi: 10.1056/NEJMe1805705 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplemental Methods and Results
eTable 1. Overall Combat Casualty Care Statistics
eTable 2. Results of Multivariable, Multinomial Logistic Regression Analysis
eTable 3. Correlation Matrix for Intervention Variables
eTable 4. Results of Sensitivity Analysis of Multivariable, Multinomial Logistic Regression Analysis
eTable 5. Injury Characteristics of Patients Who Transitioned From KIA to DOW and From KIA and DOW to Alive
eFigure 1. Mortality for Critically Injured Patients With Injury Severity Score (ISS) of 25 or Higher
eFigure 2. Key Injury Descriptions
eFigure 3. Major Interventions and Policy Directives