Key Points
Question
Does revision amputation or replantation provide better outcomes for patients with traumatic digit amputation?
Findings
In this cohort study of 338 participants, disability and patient-reported outcome scores were significantly better after replantation of distal single-finger amputation and 3 or more finger amputations. Replantation after amputation of 3 or more fingers also resulted in better sensory function scores and 9-hole peg test times.
Meaning
Replantation was associated with better overall patient-reported outcomes, with some functional benefit compared with revision amputation in distal single-finger (excluding thumb) amputation and 3 or more finger amputation injury patterns.
This cohort study compares long-term patient-reported and functional outcomes between patients treated with revision amputation or replantation for digit amputations.
Abstract
Importance
Optimal treatment for traumatic digit amputation is unknown.
Objective
To compare long-term patient-reported and functional outcomes between patients treated with revision amputation or replantation for digit amputations.
Design, Setting, and Participants
Retrospective cohort study at 19 centers in the United States and Asia. Participants were 338 individuals 18 years or older with traumatic digit amputations with at least 1 year of follow-up after treatment. Participants were enrolled from August 1, 2016, to April 12, 2018.
Exposures
Revision amputation or replantation of traumatic digit amputations.
Main Outcomes and Measures
The primary outcome was the Michigan Hand Outcomes Questionnaire (MHQ) score. Secondary outcomes were the 36-Item Short Form Health Survey (SF-36), Disabilities of the Arm, Shoulder, and Hand (DASH), and Patient-Reported Outcomes Measurement Information System (PROMIS) upper-extremity module scores and functional outcomes.
Results
Among 338 patients who met all inclusion criteria, the mean (SD) age was 48.3 (16.4) years, and 85.0% were male. Adjusted aggregate comparison of patient-reported outcomes (PROs) between patients with revision amputation and replantation revealed significantly better outcomes in the replantation cohort measured by the MHQ (5.93; 95% CI, 1.03-10.82; P = .02), DASH (−4.29; 95% CI, −8.45 to −0.12; P = .04), and PROMIS (3.44; 95% CI, 0.60 to 6.28; P = .02) scores. In subgroup analyses, DASH scores were significantly lower (6 vs 9, P = .05), indicating less disability and pain, and PROMIS scores higher (78 vs 75, P = .04) after replantation. Patients with 3 or more digits amputated (including thumb) had significantly better PROs after replantation than those managed with revision amputation (22 vs 42, P = .03 for DASH and 61 vs 36, P = .01 for PROMIS). Patients who underwent replantation after 3 or more digits amputated (excluding thumb) had higher MHQ scores, which did not reach statistical significance (69 vs 65, P = .06). Revision amputation in the subgroup with single-finger amputation distal to the proximal interphalangeal joint resulted in better 2-point discrimination (6 vs 8 mm, P = .05). Compared with revision amputation, replantation resulted in better 9-hole peg test times in the subgroup with 3 or more digits amputated (including thumb) (46 vs 81 seconds, P = .001), better Semmes-Weinstein monofilament test in the subgroup with 3 or more digits amputated (excluding thumb) (3 vs 21 g, P = .008), and better 3-point pinch test in the subgroup with 2 digits amputated (excluding thumb) (6.7 vs 5.6 kg, P = .03).
Conclusions and Relevance
When technically feasible, replantation is recommended in 3 or more digits amputated and in single-finger amputation (excluding thumb) distal to the proximal interphalangeal joint because it achieved better PROs, with long-term functional benefit. Thumb replantation is still recommended for its integral role in opposition.
Introduction
Almost 45 000 traumatic digit amputations occur every year in the United States, which comprise 90% of all US amputations.1,2,3 Digit amputation primarily affects younger, working-age men, resulting in lost income and hindrance to future earnings.4,5 Traumatic digit amputations are detrimental to activities of daily living (ADLs) and work.6,7,8,9,10 Furthermore, because the hands are so visible, digit amputation can lead to social withdrawal and reduced quality of life.11 Although the psychological sequelae differ according to patients’ baseline mental health, social support, and financial resources, finger amputation injuries are associated with depression, anxiety, impaired self-confidence, and negative future outlook, especially in the event of multiple-digit amputations.8,12,13,14
Finger amputations are treated with revision amputation or replantation. Revision amputation is a quick procedure, requiring little postoperative rehabilitation, but digit shortening can hinder hand appearance, strength, and dexterity. Owing to microsurgical advancements, replantation restores hand appearance and most hand function, with success rates over 70%.15,16,17 However, it is a complex surgery, requiring prolonged rehabilitation and time off from work. Replantation is performed with increasing frequency in Asia.9,18 This may be attributed to the social stigma of finger amputation in Asian countries, such as Japan, where it is associated with organized crime. Conversely, in the United States, replantation rates have been declining since 2000, despite steady finger amputation rates.19 As of 2007, only 56% of members of the American Society for Surgery of the Hand performed replantations.20 Of those, 62% performed fewer than 5 cases a year.20 This is especially troubling because procedure volume leads to expertise and enhances replantation success.21,22
Studies comparing revision amputation and replantation have conflicting results. One study23 found that replantation results in better outcomes, but 2 other studies24,25 found no difference between the 2 interventions. After reporting null results, Tessler et al23 suggested that outcomes hinge more on injury type than treatment type. In addition to being limited to single-digit injuries, these studies were hampered by follow-up periods of less than 1 year and single-center enrollment. To overcome these shortcomings, we created the Finger Replantation and Amputation Challenges in Assessing Impairment, Satisfaction, and Effectiveness (FRANCHISE) collaboration, the largest such group to date, including 19 national and international centers in the United States and Asia assembled to retrospectively study digit amputation. Our study aimed to compare long-term patient-reported and functional outcomes in patients with digit amputation treated with revision amputation or replantation.
Methods
Participants were enrolled from August 1, 2016, to April 12, 2018. Study centers were selected based on procedure volume, case diversity, clinical research experience, and prior successful collaboration with the principal investigator (K.C.C.). Patients treated with revision amputation or replantation were identified in each center’s electronic medical record using International Classification of Diseases, Ninth Revision codes (codes 886.0, 886.1, 885.0, and 885.1) and Current Procedural Terminology codes (codes 20816, 20822, 20824, 20827, 26951, and 26952). Patients with failed replantation who underwent revision amputation were included in the revision amputation cohort because the outcomes completely hinged on procedure type. Participants were 18 years or older at the time of assessment and underwent the most recent hand procedure at least 1 year before enrollment to ensure that their outcomes had been stable. All amputations included some bone loss. Patients who could not provide informed consent, underwent nontraumatic amputations, sustained bilateral amputations, or had amputations at or proximal to the metacarpophalangeal (MCP) joint were excluded.
Research personnel at each center contacted potential participants via phone, email, or postal mail to introduce the study. Interested individuals met with study coordinators for an assessment visit. Participating centers obtained local institutional review board approval for this study. All participants provided written informed consent and were paid $50 on completion of their assessment. Study data were collected in a database set up by The Plastic Surgery Foundation using research electronic data capture.26
Demographic Data
On enrollment, participants self-reported demographics, including age, sex, race/ethnicity, health insurance status, education level, annual household income, and employment status. They also self-reported injury information (work-relatedness, mechanism of injury, and associated injuries) at enrollment.
Patient-Reported Outcomes
Patient-reported outcomes (PROs) were assessed via the Michigan Hand Outcomes Questionnaire (MHQ),27,28,29,30,31 the Disabilities of the Arm, Shoulder, and Hand (DASH),10,32,33 and the Patient-Reported Outcomes Measurement Information System (PROMIS) upper-extremity module.34 These measures provide insight into upper extremity function and pain. We also administered the 36-Item Short Form Health Survey (SF-36), a common measure of quality of life.35 The MHQ, SF-36, and PROMIS are scored from 0 to 100, in which higher scores indicate better outcomes. DASH is also scored from 0 to 100, in which lower scores indicate better outcomes. Participants completed PROs in the most common language at each center (English, Japanese, Korean, or Mandarin Chinese). All translations have been validated via the translation–back translation method.36
Functional Assessments
Grip strength, lateral pinch strength, 2-point pinch strength, 3-point pinch strength, 9-hole peg test, and joint arc of motion were used to measure motor function. Range of motion at the MCP and proximal interphalangeal (PIP) joints was calculated as extension subtracted from flexion. Static 2-point discrimination (2PD) and Semmes-Weinstein (SW) monofilament test were used to assess sensory function. The 2PD was measured with a discriminator tool that ranged from 1 to 25 mm, with reference values categorized as normal sensation (<6 mm), fair sensation (6-10 mm), poor sensation (11-15 mm), and protective sensation only (>15 mm), with lower values indicating improved digit sensation.37 The 2PD and SW monofilament tests were assessed at the end of the amputated stump in patients with revision amputation. Participants were divided into the following subgroups based on the specific digit, number of digits, and level of amputation: (1) single-finger amputation (excluding thumb) distal to the PIP joint, (2) single-finger amputation (excluding thumb) proximal to the PIP joint, (3) thumb-only amputation distal to the interphalangeal (IP) joint, (4) thumb-only amputation proximal to the IP joint, (5) multiple fingers amputated (excluding thumb) (2 digits amputated), (6) multiple fingers amputated (including thumb) (2 digits amputated), (7) multiple fingers amputated (excluding thumb) (≥3 digits amputated), and (8) multiple fingers amputated (including thumb) (≥3 digits amputated).
Statistical Analysis
Sample size was determined based on a literature search and preliminary data by reviewing medical records and case logs 5 years before the study start at the coordinating centers (University of Michigan and The Plastic Surgery Foundation). Owing to similar case profiles at participating centers, we estimated the necessary sample size for the entire cohort to be approximately 238 undergoing revision amputation and 69 undergoing replantation. This projected sample size was expected to provide 90% power to detect a 6.6-point difference in our primary outcome measure (summary MHQ score) between the 2 treatments, assuming an SD of 15 and based on a 2-sided .05-level test. Descriptive statistics were calculated to summarize the participants’ demographic factors, PROs, and functional outcomes stratified by centers and treatment groups. Wilcoxon-Mann-Whitney test was used for continuous variables, and χ2 test or 2-tailed Fisher exact test was used for categorical variables. Potential confounders associated with treatment type were evaluated through a multivariable logistic regression using treatment type as the dependent variable and patient characteristics as covariates. The significant variables associated with treatment type were then applied to calculate propensity scores for replantation for each patient in the study cohort. To compare PROs and functional outcomes between the 2 treatment groups, we performed a mixed-effects linear regression model for each study outcome. In each model, we used the PRO or functional outcome as the dependent variable and the type of treatment (revision amputation vs replantation) as an explanatory variable, controlled for propensity scores calculated from the above logistic regression models of treatment type using the corresponding significant outcome variables to adjust for the associations of potential confounders. We introduced a random intercept for each center in our final model to account for the correlation of study outcomes within each center. Adjusted mean differences and 95% CIs from each model are reported. In addition, we performed the same analytical approach for each injury group by conducting stratified analysis. No significant confounder between study outcomes and treatment type was found in any injury pattern; therefore, mixed-effects linear regression models of each study outcome were constructed using each injury group as subcohorts and a random intercept representing each center. Statistical significance was set at 2-sided P < .05. All analyses were performed with statistical software (R, version 3.2.2; R Foundation).
Results
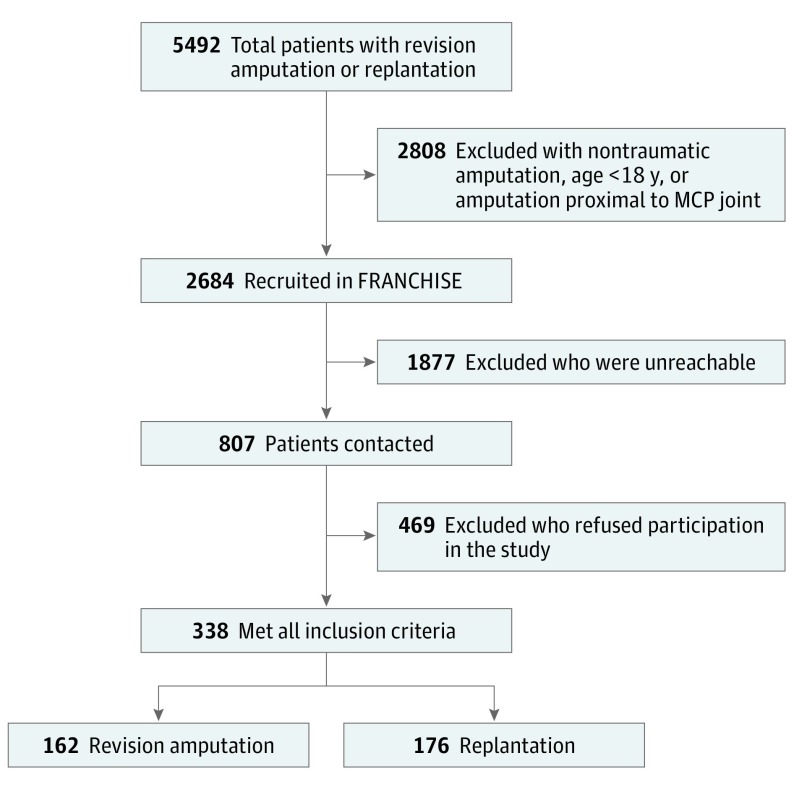
Over 2 years, FRANCHISE centers collectively screened 5492 patients treated with revision amputation or replantation. Among those, 2808 patients (51.1%) were ineligible, most commonly because of nontraumatic amputation, age younger than 18 years, or amputation proximal to the MCP joint. Of the 2684 eligible patients, 1877 could not be reached, and 469 refused to participate in the study. As we started to recruit patients, we found it affordable to enroll patients in the 2 treatment arms with a 1:1 ratio. This balanced recruitment was more efficient for the statistical analysis, and we only required 110 participants from each treatment group to achieve the same statistical power as before. We were able to successfully enroll 338 participants, among whom 162 were treated with revision amputation and 176 were treated with replantation (Figure).
Figure. Study Screening and Enrollment.
FRANCHISE indicates Finger Replantation and Amputation Challenges in Assessing Impairment, Satisfaction, and Effectiveness; MCP, metacarpophalangeal.
Among the 338 patients who met all inclusion criteria in this retrospective cohort study, the mean (SD) age was 48.3 (16.4) years, and 85.0% were male. At both US and foreign centers, there were no significant differences in treatment received based on age, sex, health insurance status, education level, annual household income, or work-relatedness of injury (Table 1). Foreign centers, mostly located in Asia, did not have ethnic/racial diversity in their enrolled patients, but there was no difference in treatment based on race/ethnicity in the United States. At foreign centers, injury pattern was independent of treatment. Conversely, at the US centers, treatment varied significantly based on injury pattern, with patients sustaining single-finger amputations least likely to receive replantation, whereas those with multiple-digit amputations were most likely to receive replantation.
Table 1. Demographic Characteristics of Study Participants by Center and Treatment.
| Variable | US Centersa | Non-US Centersb | ||||
|---|---|---|---|---|---|---|
| Revision Amputation | Replantation | P Value | Revision Amputation | Replantation | P Value | |
| No. of participants | 112 | 25 | NA | 50 | 151 | NA |
| Age, mean (SD), y | 52.1 (17.4) | 48.1 (16.2) | .14 | 48.0 (17.0) | 45.2 (15.0) | .21 |
| Time since injury, mean (SD), mo | 79.6 (53.1) | 68.1 (35.0) | .06 | 41.4 (21.3) | 46.2 (26.6) | .39 |
| Sex, No. (%) | ||||||
| Male | 91 (81.3) | 22 (88.0) | .56 | 44 (88.0) | 130 (86.1) | .73 |
| Female | 21 (18.8) | 3 (12.0) | 6 (12.0) | 21 (13.9) | ||
| Race/ethnicity, No. (%) | ||||||
| White | 96 (85.7) | 19 (76.0) | .23 | 0 | 0 | NA |
| All other races/ethnicities | 16 (14.3) | 6 (24.0) | 50 (100) | 151 (100) | ||
| Insurance status, No. (%) | ||||||
| No | 12 (10.7) | 1 (4.0) | .53 | 12 (24.0) | 32 (21.2) | .68 |
| Yes | 94 (83.9) | 21 (84.0) | 38 (76.0) | 119 (78.8) | ||
| Missing | 6 (5.4) | 3 (12.0) | 0 | 0 | ||
| Education level, No. (%) | ||||||
| Less than college graduate | 78 (69.6) | 14 (56.0) | .28 | 42 (84.0) | 123 (81.5) | .58 |
| College graduate or higher | 33 (29.5) | 8 (32.0) | 6 (12.0) | 23 (15.2) | ||
| Missing | 1 (0.9) | 3 (12.0) | 2 (4.0) | 5 (3.3) | ||
| Annual household income, No. (%) | ||||||
| <$60 000 | 59 (52.7) | 9 (36.0) | .34 | 46 (92.0) | 132 (87.4) | .36 |
| ≥$60 000 | 50 (44.6) | 12 (48.0) | 2 (4.0) | 13 (8.6) | ||
| Missing | 3 (2.7) | 4 (16.0) | 2 (4.0) | 6 (4.0) | ||
| Work-related injury, No. (%) | ||||||
| No | 82 (73.2) | 14 (56.0) | .09 | 6 (12.0) | 20 (13.2) | .82 |
| Yes | 30 (26.8) | 11 (44.0) | 44 (88.0) | 131 (86.8) | ||
| Amputation group, No. (%) | ||||||
| Single-finger amputation (excluding thumb) | 60 (53.6) | 2 (8.0) | <.001 | 31 (62.0) | 65 (43.0) | .15 |
| Thumb-only amputation | 18 (16.1) | 10 (40.0) | 5 (10.0) | 26 (17.2) | ||
| Multiple fingers amputated (excluding thumb) | 29 (25.9) | 8 (32.0) | 12 (24.0) | 49 (32.5) | ||
| Multiple fingers amputated (including thumb) | 5 (4.5) | 5 (20.0) | 2 (4.0) | 11 (7.3) | ||
Abbreviation: NA, not applicable.
Curtis National Hand Center at MedStar Union Memorial Hospital, University of Michigan, The Ohio State University, Regions Hospital Minnesota, Southern Illinois University Medicine, University of Pittsburgh Medical Center, University of Washington Medical Center, University of Wisconsin Health, Vanderbilt University Medical Center, and Washington University Medical Centers.
Anjo Kosei Hospital (Japan), Chang Gung Memorial Hospital (Taiwan), China-Japan Union Hospital of Jilin University, Ganga Hospital (India), Japanese Red Cross Otsu Hospital, Nagoya University Hospital (Japan), Nara City Hospital (Japan), National University Hospital Singapore, and W Hospital (Daegu, Korea).
Adjusted aggregate comparison of PROs between patients with revision amputation and replantation revealed significantly better outcomes in the replantation cohort measured by the MHQ (5.93; 95% CI, 1.03-10.82; P = .02), DASH (−4.29; 95% CI, −8.45 to −0.12; P = .04), and PROMIS (3.44; 95% CI, 0.60-6.28; P = .02). These results are summarized in Table 2.
Table 2. Multivariable Analysis Comparison Between Revision Amputation and Replantation Groups.
| Variable | Mean (SD) | Adjusted Mean Difference (95% CI)a | P Value | |
|---|---|---|---|---|
| Revision Amputation | Replantation | |||
| MHQ | 76.81 (18.93) | 76.78 (17.64) | 5.93 (1.03 to 10.82) | .02b |
| DASH | 13.84 (16.12) | 11.29 (14.86) | −4.29 (−8.45 to −0.12) | .04b |
| PCS | 51.76 (8.03) | 53.22 (7.30) | 0.50 (−1.56 to 2.57) | .63 |
| MCS | 53.41 (9.56) | 52.08 (10.93) | 0.48 (−2.20 to 3.16) | .73 |
| PROMIS | 70.63 (12.32) | 73.50 (9.37) | 3.44 (0.60 to 6.28) | .02b |
| 2PD | 6.80 (3.30) | 8.44 (4.26) | 0.76 (−0.31 to 1.83) | .17 |
| Grip strength | 31.54 (13.79) | 32.36 (14.18) | 2.34 (−1.37 to 6.05) | .22 |
| Lateral pinch strength | 8.93 (3.68) | 8.56 (4.10) | 0.56 (−0.31 to 1.43) | .21 |
| 2-Point pinch strength | 6.10 (2.96) | 5.70 (3.70) | −0.31 (−1.07 to 0.45) | .42 |
| 3-Point pinch strength | 6.92 (3.25) | 6.66 (4.45) | −0.14 (−1.06 to 0.78) | .76 |
| 9-Hole peg test | 28.39 (17.87) | 26.32 (10.55) | −1.56 (−5.44 to 2.32) | .43 |
| SW monofilament test | 13.50 (42.56) | 9.77 (36.51) | 2.17 (−8.73 to 13.06) | .70 |
| Thumb MCP joint ROM | 45.50 (25.35) | 57.83 (18.46) | 9.06 (−4.72 to 22.84) | .21 |
| Thumb IP joint ROM | 63.00 (39.07) | 60.03 (35.06) | −8.18 (−32.74 to 16.38) | .52 |
| Finger MCP joint ROM | 76.28 (13.35) | 75.77 (16.18) | 2.29 (−3.10 to 7.68) | .41 |
| Finger PIP joint ROM | 70.14 (30.51) | 74.93 (38.79) | 4.21 (−11.87 to 20.30) | .61 |
Abbreviations: DASH, Disabilities of the Arm, Shoulder, and Hand; IP, interphalangeal; MCP, metacarpophalangeal; MCS, SF-36 mental component subscale; MHQ, Michigan Hand Outcomes Questionnaire; PCS, SF-36 physical component subscale; 2PD, 2-point discrimination; PIP, proximal interphalangeal; PROMIS, Patient-Reported Outcomes Measurement Information System upper-extremity module; ROM, range of motion; SF-36, 36-Item Short Form Health Survey; SW, Semmes-Weinstein.
Standardized β coefficients and standard errors calculated from multivariable linear regression controlling for propensity scores, with a random intercept for each center.
Statistically significant at P < .05.
A multivariable logistic regression of treatment type with patient characteristics confirmed that center and injury pattern were 2 potential confounding factors associated with treatment type. Patients at the US centers were significantly less likely to undergo replantation (odds ratio [OR], 0.10; 95% CI, 0.01-0.22) than those at international centers. Injury patterns associated with undergoing replantation included thumb-only amputation distal or proximal to the IP joint (OR, 3.92 [95% CI, 1.32-11.71] and 5.77 [95% CI, 1.84-18.10], respectively), 3 or more digits amputated with or without thumb involvement (OR, 4.77 [95% CI, 0.98-23.14] and 7.72 [95% CI, 2.86-20.88], respectively), and 2-digit amputation (including thumb) (OR, 18.87; 95% CI, 2.72-131.09) (eTable in the Supplement).
Mixed-effects multivariable linear regression stratified by injury pattern demonstrated that the replantation cohort overall had better MHQ, DASH, and PROMIS scores compared with the revision amputation cohort within each injury pattern (Table 3). Patients with replantation who sustained single-digit amputations distal to the PIP joint scored significantly better on DASH (6 vs 9, P = .05) and PROMIS (78 vs 75, P = .04). Comparing functional outcomes in this subgroup, the replantation cohort had worse 2PD (8 vs 6 mm, P = .05) but had better PIP joint motion, which did not reach statistical significance (83° vs 71°, P = .06) (Table 4). In the subgroup with single-digit amputations proximal to the PIP joint, no differences were observed in PROs or functional outcomes between the 2 treatment groups. There were no significant differences in PROs based on treatment received for patients who sustained thumb amputations either proximal or distal to the IP joint, and there were also no significant differences in functional outcomes among patients with thumb-only amputations proximal to the IP joint. Patients who underwent replantation of the thumb after injury distal to the IP joint appeared to have better MCP joint motion, although this did not reach statistical significance (60° vs 35°, P = .06).
Table 3. Stratified Analysis of Patient-Reported Outcomes by Treatment Type in the Revision Amputation and Replantation Groups.
| Variable | Revision Amputation | Replantation | Adjusted Mean Difference (95% CI)a | P Valuea | ||
|---|---|---|---|---|---|---|
| No. | Mean (95% CI) | No. | Mean (95% CI) | |||
| Single-Finger Amputation (Excluding Thumb) Distal to the PIP Joint | ||||||
| MHQ | 76 | 84 (80 to 87) | 49 | 84 (81 to 88) | 2.16 (−3.60 to 7.92) | .47 |
| DASH | 77 | 9 (7 to 12) | 50 | 6 (4 to 7) | −3.47 (−6.90 to −0.04) | .05b |
| PCS | 77 | 53 (51 to 54) | 52 | 55 (54 to 57) | 1.82 (−0.99 to 4.63) | .21 |
| MCS | 77 | 54 (52 to 56) | 52 | 52 (48 to 55) | −1.50 (−5.94 to 2.93) | .51 |
| PROMIS | 39 | 75 (73 to 78) | 52 | 78 (77 to 79) | 2.72 (0.11 to 5.33) | .04b |
| Single-Finger Amputation (Excluding Thumb) Proximal to the PIP Joint | ||||||
| MHQ | 12 | 66 (53 to 80) | 15 | 76 (69 to 84) | 11.11 (−1.79 to 24.00) | .11 |
| DASH | 11 | 18 (4 to 33) | 15 | 10 (5 to 14) | −9.47 (−20.85 to 1.91) | .12 |
| PCS | 11 | 52 (47 to 57) | 15 | 53 (48 to 57) | 1.09 (−4.68 to 6.85) | .72 |
| MCS | 11 | 49 (42 to 57) | 15 | 55 (51 to 59) | 6.86 (−1.02 to 14.75) | .11 |
| PROMIS | 8 | 70 (61 to 79) | 15 | 75 (69 to 80) | 2.05 (−6.45 to 10.56) | .64 |
| Thumb-Only Amputation Distal to the IP Joint | ||||||
| MHQ | 15 | 81 (75 to 88) | 14 | 84 (74 to 94) | 2.72 (−9.30 to 14.73) | .66 |
| DASH | 15 | 9 (2 to 15) | 14 | 4 (0 to 8) | −4.86 (−11.85 to 2.13) | .19 |
| PCS | 15 | 53 (50 to 57) | 15 | 54 (49 to 60) | −2.66 (−9.74 to 4.42) | .47 |
| MCS | 15 | 56 (52 to 59) | 15 | 52 (46 to 57) | 5.43 (−1.94 to 12.79) | .17 |
| PROMIS | 5 | 73 (66 to 80) | 15 | 75 (72 to 79) | 2.51 (−3.65 to 8.67) | .45 |
| Thumb-Only Amputation Proximal to the IP Joint | ||||||
| MHQ | 8 | 74 (62 to 85) | 20 | 79 (70 to 87) | 2.30 (−12.17 to 16.78) | .76 |
| DASH | 8 | 13 (1 to 25) | 20 | 16 (7 to 26) | 3.69 (−9.82 to 17.2) | .60 |
| PCS | 8 | 53 (44 to 62) | 20 | 51 (47 to 54) | −3.87 (−11.13 to 3.40) | .31 |
| MCS | 8 | 54 (50 to 58) | 20 | 54 (50 to 59) | −1.05 (−8.52 to 6.42) | .79 |
| PROMIS | 7 | 71 (62 to 79) | 20 | 70 (66 to 74) | −0.92 (−8.63 to 6.79) | .82 |
| Multiple Fingers Amputated (Excluding Thumb) (2 Digits Amputated) | ||||||
| MHQ | 28 | 70 (61 to 79) | 23 | 72 (64 to 79) | 9.72 (−4.07 to 23.52) | .18 |
| DASH | 28 | 15 (10 to 21) | 23 | 14 (7 to 21) | −3.57 (−13.10 to 5.96) | .47 |
| PCS | 28 | 51 (48 to 55) | 23 | 53 (50 to 55) | 2.80 (−2.11 to 7.72) | .27 |
| MCS | 28 | 52 (48 to 56) | 23 | 51 (47 to 56) | −0.07 (−6.57 to 6.43) | .98 |
| PROMIS | 10 | 66 (56 to 76) | 23 | 73 (70 to 77) | 7.03 (−0.38 to 14.43) | .08 |
| Multiple Fingers Amputated (Including Thumb) (2 Digits Amputated) | ||||||
| MHQ | 2 | 65 | 7 | 70 (47 to 92) | −0.20 (−49.18 to 48.78) | .99 |
| DASH | 2 | 14 | 8 | 9 (0 to 19) | −4.97 (−22.57 to 12.63) | .61 |
| PCS | 2 | 43 | 8 | 53 (46 to 60) | 5.12 (−9.18 to 19.42) | .52 |
| MCS | 2 | 63 | 8 | 51 (42 to 61) | −6.19 (−24.68 to 12.29) | .55 |
| PROMIS | 0 | NA | 8 | 73 (65 to 81) | NA | NA |
| Multiple Fingers Amputated (Excluding Thumb) (≥3 Digits Amputated) | ||||||
| MHQ | 12 | 65 (52 to 77) | 34 | 69 (62 to 76) | 12.64 (0.12 to 25.16) | .06 |
| DASH | 13 | 28 (15 to 42) | 36 | 17 (10 to 24) | −6.14 (−20.33 to 8.05) | .40 |
| PCS | 13 | 47 (42 to 52) | 36 | 52 (50 to 55) | 2.66 (−2.52 to 7.84) | .32 |
| MCS | 13 | 52 (45 to 59) | 36 | 51 (47 to 55) | 4.81 (−3.06 to 12.67) | .24 |
| PROMIS | 7 | 64 (55 to 73) | 36 | 70 (66 to 74) | 2.09 (−6.75 to 10.94) | .65 |
| Multiple Fingers Amputated (Including Thumb) (≥3 Digits Amputated) | ||||||
| MHQ | 6 | 61 (44 to 79) | 7 | 63 (39 to 87) | 23.57 (0.60 to 46.54) | .09 |
| DASH | 6 | 42 (18 to 67) | 8 | 22 (7 to 37) | −31.10 (−52.89 to −9.31) | .03 |
| PCS | 6 | 50 (43 to 58) | 8 | 51 (43 to 60) | 4.06 (−7.20 to 15.33) | .51 |
| MCS | 6 | 56 (47 to 65) | 8 | 49 (35 to 62) | 2.57 (−10.35 to 15.49) | .71 |
| PROMIS | 3 | 36 (14 to 58) | 8 | 61 (51 to 72) | 30.45 (17.47 to 43.43) | .01 |
Abbreviations: DASH, Disabilities of the Arm, Shoulder, and Hand (0-100, with 0 indicating no disability); IP, interphalangeal; MCS, SF-36 mental component subscale (0-100, with 100 indicating perfect health); MHQ, Michigan Hand Outcomes Questionnaire (0-100, with 100 indicating no disability); NA, not applicable; PCS, SF-36 physical component subscale (0-100, with 100 indicating perfect health); PIP, proximal interphalangeal; PROMIS, Patient-Reported Outcomes Measurement Information System upper-extremity module (0-100, with 100 indicating no disability); SF-36, 36-Item Short Form Health Survey.
Mean difference and P value calculated from mixed linear regression, with a random intercept for each center.
Statistically significant at P < .05.
Table 4. Functional Results Comparison by Treatment Type in the Revision Amputation and Replantation Groups.
| Variablea | Revision Amputation | Replantation | Adjusted Mean Difference (95% CI)b | P Valueb | ||
|---|---|---|---|---|---|---|
| No. | Mean (95% CI) | No. | Mean (95% CI) | |||
| Single-Finger Amputation (Excluding Thumb) Distal to the PIP Joint | ||||||
| 2PD, mm | 78 | 6 (5 to 7) | 50 | 8 (6 to 9) | 1.45 (0.01 to 2.88) | .05c |
| SW monofilament test, g | 76 | 12 (2 to 21) | 51 | 3 (3 to 4) | −6.88 (−18.46 to 4.71) | .25 |
| Grip strength, kg | 78 | 34 (31 to 37) | 52 | 35 (31 to 38) | 2.33 (−3.09 to 7.74) | .40 |
| Lateral pinch strength, kg | 78 | 9.1 (8.2 to 10.0) | 52 | 8.6 (7.8 to 9.4) | 0.23 (−0.98 to 1.45) | .71 |
| 2-Point pinch strength, kg | 78 | 6.3 (5.6 to 7.0) | 52 | 5.8 (4.9 to 6.8) | −0.48 (−1.45 to 0.49) | .33 |
| 3-Point pinch strength, kg | 78 | 7.3 (6.6 to 8.1) | 52 | 7.3 (6.3 to 8.3) | −0.11 (−1.18 to 0.96) | .84 |
| 9-Hole peg test, s | 38 | 26 (19 to 32) | 50 | 23 (21 to 25) | −3.53 (−9.38 to 2.32) | .24 |
| MCP ROM, ° | 78 | 76 (72 to 81) | 52 | 77 (72 to 82) | 4.64 (−1.16 to 10.44) | .12 |
| PIP ROM, ° | 78 | 71 (62 to 81) | 52 | 83 (73 to 92) | 14.04 (−0.23 to 28.32) | .06 |
| Single-Finger Amputation (Excluding Thumb) Proximal to the PIP Joint | ||||||
| 2PD, mm | 9 | 9 (6 to 12) | 13 | 9 (6 to 12) | −1.21 (−5.78 to 3.37) | .61 |
| SW monofilament test, g | 10 | 42 (27 to 111) | 15 | 3 (3 to 4) | −4.10 (−37.36 to 29.15) | .81 |
| Grip strength, kg | 12 | 32 (25 to 39) | 15 | 32 (26 to 38) | 0.10 (−8.10 to 8.29) | .98 |
| Lateral pinch strength, kg | 12 | 9.9 (6.5 to 13.4) | 15 | 7.8 (6.4 to 9.3) | −1.07 (−4.58 to 2.44) | .56 |
| 2-Point pinch strength, kg | 12 | 5.6 (3.3 to 7.8) | 15 | 5.5 (4.4 to 6.6) | −0.40 (−2.57 to 1.78) | .72 |
| 3-Point pinch strength, kg | 12 | 7.8 (4.8 to 10.8) | 15 | 7.1 (5.7 to 8.6) | 0.13 (−2.95 to 3.20) | .94 |
| 9-Hole peg test, s | 8 | 31 (16 to 46) | 15 | 24 (18 to 30) | −5.01 (−17.47 to 7.46) | .44 |
| MCP ROM, ° | 5 | 76 (62 to 91) | 15 | 72 (63 to 80.2) | −7.18 (−22.07 to 7.71) | .36 |
| PIP ROM, ° | 2 | 48 (84 to 179) | 15 | 61 (36 to 86) | 13.50 (−55.02 to 82.02) | .71 |
| Thumb-Only Amputation Distal to the IP Joint | ||||||
| 2PD, mm | 15 | 8 (7 to 9) | 14 | 9 (6 to 12) | −0.36 (−3.25 to 2.54) | .81 |
| SW monofilament test, g | 15 | 22 (0 to 52) | 15 | 9 (0 to 21) | −12.94 (−43.07 to 17.19) | .41 |
| Grip strength, kg | 15 | 40 (35 to 45) | 15 | 37 (28 to 47) | −5.71 (−17.72 to 6.29) | .36 |
| Lateral pinch strength, kg | 15 | 10.1 (8.3 to 11.9) | 15 | 9.7 (7.4 to 11.9) | −0.50 (−3.91 to 2.91) | .78 |
| 2-Point pinch strength, kg | 15 | 7.1 (5.9 to 8.4) | 15 | 7.2 (4.3 to 10.0) | −0.11 (−3.00 to 2.78) | .94 |
| 3-Point pinch strength, kg | 15 | 8.3 (7.1 to 9.6) | 15 | 8.5 (4.9 to 12.1) | 0.23 (−2.82 to 3.28) | .88 |
| 9-Hole peg test, s | 5 | 25 (20 to 31) | 14 | 25 (22 to 28) | 0.32 (−4.61 to 5.25) | .90 |
| MCP ROM, ° | 5 | 35 (8 to 79) | 15 | 60 (53 to 68) | 22.70 (2.21 to 43.19) | .06 |
| IP ROM, ° | 5 | 47 (9 to 103) | 15 | 66 (48 to 83) | 17.39 (−17.89 to 52.68) | .36 |
| Thumb-Only Amputation Proximal to the IP Joint | ||||||
| 2PD, mm | 8 | 7 (4 to 11) | 20 | 12 (10 to 14) | 3.76 (−0.11 to 7.64) | .08 |
| SW monofilament test, g | 8 | 3 (2 to 4) | 20 | 40 (0 to 81) | 37.19 (−23.64 to 98.01) | .25 |
| Grip strength, kg | 8 | 34 (24 to 44) | 20 | 38 (30 to 46) | 3.65 (−9.38 to 16.68) | .59 |
| Lateral pinch strength, kg | 8 | 8.9 (6.4 to 11.3) | 20 | 9.1 (6.0 to 12.2) | 0.30 (−2.43 to 3.03) | .83 |
| 2-Point pinch strength, kg | 8 | 6.7 (4.5 to 8.9) | 20 | 6.0 (3.7 to 8.3) | 0.10 (−2.70 to 2.90) | .95 |
| 3-Point pinch strength, kg | 8 | 7.4 (5.2 to 9.6) | 20 | 8.1 (4.5 to 11.6) | 0.63 (−2.87 to 4.13) | .73 |
| 9-Hole peg test, s | 7 | 29 (23 to 34) | 19 | 27 (23 to 30) | −2.05 (−7.88 to 3.79) | .50 |
| MCP ROM, ° | 7 | 53 (39 to 66) | 20 | 56 (46 to 66) | 3.14 (−14.21 to 20.48) | .73 |
| IP ROM, ° | 7 | 61 (12 to 133) | 19 | 56 (37 to 74) | −18.65 (−50.62 to 13.31) | .27 |
| Multiple Fingers Amputated (Excluding Thumb) (2 Digits Amputated) | ||||||
| 2PD, mm | 26 | 6 (5 to 7) | 22 | 8 (6 to 10) | 1.51 (−0.46 to 3.48) | .14 |
| SW monofilament test, g | 27 | 7 (1 to 13) | 23 | 17 (0 to 38) | 0.53 (−11.11 to 12.18) | .93 |
| Grip strength, kg | 27 | 27 (21 to 32) | 23 | 32 (25 to 38) | 8.83 (−1.22 to 18.88) | .09 |
| Lateral pinch strength, kg | 27 | 9.0 (7.9 to 10.1) | 23 | 8.4 (6.6 to 10.2) | 0.39 (−1.90 to 2.68) | .74 |
| 2-Point pinch strength, kg | 27 | 5.6 (4.7 to 6.5) | 23 | 6.3 (4.4 to 8.2) | 1.38 (−0.61 to 3.37) | .18 |
| 3-Point pinch strength, kg | 27 | 5.6 (4.9 to 6.4) | 22 | 6.7 (5.3 to 8.1) | 1.86 (0.26 to 3.46) | .03c |
| 9-Hole peg test, s | 9 | 26 (18 to 33) | 21 | 25 (22 to 29) | −0.16 (−6.51 to 6.19) | .96 |
| Multiple Fingers Amputated (Including Thumb) (2 Digits Amputated) | ||||||
| 2PD, mm | 2 | 11 | 8 | 8 (5 to 11) | 0.48 (−7.36 to 8.33) | .91 |
| SW monofilament test, g | 2 | 0 | 7 | 3 (2 to 5) | 1.33 (−2.34 to 5.01) | .52 |
| Grip strength, kg | 2 | 14 | 8 | 39 (25 to 54) | 10.01 (−28.70 to 48.71) | .64 |
| Lateral pinch strength, kg | 2 | 4.5 | 8 | 7.2 (5.7 to 8.7) | −2.12 (−6.64 to 2.40) | .41 |
| 2-Point pinch strength, kg | 2 | 3.0 | 8 | 5.4 (4.1 to 6.7) | −0.93 (−4.46 to 2.60) | .63 |
| 3-Point pinch strength, kg | 2 | 3.8 | 8 | 6.0 (4.8 to 7.2) | −0.98 (−3.23 to 1.27) | .44 |
| 9-Hole peg test, s | 0 | NA | 7 | 28 (20 to 35) | 0.48 (−7.36 to 8.33) | .91 |
| Multiple Fingers Amputated (Excluding Thumb) (≥3 Digits Amputated) | ||||||
| 2PD, mm | 11 | 8 (5 to 10) | 31 | 8 (7 to 10) | −0.29 (−3.01 to 2.42) | .83 |
| SW monofilament test, g | 11 | 21 (1 to 42) | 31 | 3 (2 to 3) | −17.14 (−29.05 to −5.24) | .01c |
| Grip strength, kg | 11 | 23 (15 to 31) | 34 | 25 (22 to 28) | 1.80 (−4.74 to 8.34) | .59 |
| Lateral pinch strength, kg | 11 | 7.9 (5.6 to 10.3) | 33 | 8.4 (6.9 to 9.9) | 1.81 (−0.29 to 3.90) | .10 |
| 2-Point pinch strength, kg | 11 | 6.3 (3.7 to 8.9) | 33 | 4.8 (3.8 to 5.8) | −0.28 (−1.93 to 1.37) | .74 |
| 3-Point pinch strength, kg | 9 | 5.7 (4.7 to 6.6) | 32 | 4.4 (3.4 to 5.5) | −1.05 (−2.98 to 0.88) | .30 |
| 9-Hole peg test, s | 5 | 31 (21 to 41) | 32 | 30 (25 to 34) | −3.50 (−13.90 to 6.90) | .52 |
| Multiple Fingers Amputated (Including Thumb) (≥3 Digits Amputated) | ||||||
| 2PD, mm | 5 | 8 (2 to 14) | 8 | 8 (7 to 9) | −1.91 (−5.64 to 1.82) | .36 |
| SW monofilament test, g | 5 | 1 (0 to 2) | 7 | 3 (0 to 6) | −1.54 (−2.75 to −0.33) | .07 |
| Grip strength, kg | 5 | 23 (0 to 53) | 8 | 22 (11 to 32) | 6.83 (−13.69 to 27.34) | .54 |
| Lateral pinch strength, kg | 5 | 5.6 (0.0 to 12.0) | 8 | 9.7 (4.7 to 14.6) | 5.3 (−0.44 to 11.04) | .13 |
| 2-Point pinch strength, kg | 5 | 4.5 (0.0 to 9.4) | 7 | 4.5 (0.5 to 8.5) | 1.61 (−3.35 to 6.57) | .56 |
| 3-Point pinch strength, kg | 5 | 4.0 (0.0 to 44.6) | 6 | 5.1 (0 to 10.9) | 2.47 (−4.61 to 9.54) | .53 |
| 9-Hole peg test, s | 2 | 81 | 7 | 46 (28 to 65) | −50.29 (−56.94 to −43.65) | .001c |
Abbreviations: IP, interphalangeal; MCP, metacarpophalangeal; NA, not applicable; 2PD, 2-point discrimination (injured finger); PIP, proximal interphalangeal; ROM, range of motion (injured finger); SW, Semmes-Weinstein monofilament (injured finger, most distal point).
The following variables refer to the injured hand: Grip strength, Lateral pinch strength, 2-Point pinch strength, 3-Point pinch strength, and 9-Hold peg test.
Mean difference and P value calculated from mixed linear regression, with a random intercept for each center.
Statistically significant at P < .05.
Patients with 3 or more digits amputated (including thumb) had significantly better PROs after replantation than those managed with revision amputation (22 vs 42, P = .03 for DASH and 61 vs 36, P = .01 for PROMIS). Patients with replantation had a significantly better 9-hole peg test time than patients with revision amputation (46 vs 81 seconds, P = .001). Patients with replantation who sustained an amputation of 3 or more fingers (excluding thumb) had a higher MHQ score than patients with revision amputation (69 vs 65, P = .06). Revision amputation in the subgroup with single-finger amputation distal to PIP joint resulted in better 2PD (6 vs 8 mm, P = .05). Patients with replantation also had better sensory threshold in this subgroup with SW monofilament test (3 vs 21 g, P = .008). Patients with replantation with amputation of 2 fingers (excluding thumb) had significantly stronger 3-point pinch strength than patients with revision amputation (6.7 vs 5.6 kg, P = .03).
Discussion
Patients with replantation with single-digit amputation distal to the PIP joint had better DASH and PROMIS scores but worse 2PD than patients with revision amputation. Similarly, patients who underwent replantation with amputation of 3 or more digits (including thumb) scored better on DASH and PROMIS and had better 9-hole peg test results than patients with revision amputation. Only a single potential functional improvement (MCP joint motion), which did not reach statistical significance, was seen in the replantation cohort for patients with thumb-only amputation distal to the IP joint. Similarly, few functional improvements were seen in 2-finger amputations (excluding thumb) and 3 or more amputations (excluding thumb), including, 3-point pinch strength and SW monofilament test, respectively.
Owing to small sample size and being single-center studies, prior comparative studies had increased likelihood of selection bias, lack of scientific rigor, and decreased external validity. Jones et al38 suggested that thumbs should be replanted because of greater grip strength in the replanted thumb. Hattori et al39 concluded that successful single-fingertip replantations can result in better outcomes based on DASH and range of motion. Tessler et al23 demonstrated that for dominant-hand injuries replantation resulted in less anxiety in patients compared with revision amputation. They also found that patients who had digit replantation to the nondominant hand had better DASH scores than the cohort who had dominant-hand replantation.23
Large absolute mean differences in the MHQ (23 points), DASH (31 points), and PROMIS (31 points), as well as the 9-hole peg test (50 seconds), between patients with revision amputation and replantation who sustained 3 or more digits amputated (including thumb) may be attributable to difficulties in opposition (Tables 3 and 4). In contrast, the small absolute mean differences in DASH (3 points) and PROMIS (3 points) between the revision amputation and replantation cohorts in single-finger distal amputations are smaller than the minimal clinically important difference of both instruments. The minimal clinically important difference is approximately 10 for DASH40 and has been preliminarily stated as 9 for PROMIS upper extremity.41 However, given the statistical differences in PROs, our recommendation is to consider replantation in patients with single-finger amputation distal to the PIP joint until further studies are conducted.
When multiple fingers are amputated, even if the fingers have some remaining length after revision amputation, the ability to oppose and grasp may not be as agile as having full-length fingers. Based on the higher PROs and improved dexterity (thumb involved) after replantation in patients with 3 or more digits amputated compared with those who underwent revision amputation, we recommend replantation in this injury pattern when technically feasible. We recommend replantation as well in the subgroup with 3 or more digits amputated not involving the thumb based on the higher MHQ score (although the difference did not reach statistical significance) and the significantly different sensory threshold. Our conclusions for 2-digit amputation involving the thumb were limited by inadequate power in the revision amputation cohort; however, extrapolating from the results in the subgroup with 3 or more digits amputated, we likewise recommend replantation if the thumb is involved in a 2-digit amputation. Two-digit amputation not involving the thumb should be managed on a case-by-case basis according to the patient’s occupation, beliefs, and clinical scenario because some patients may adjust over time to compensate for the missing fingers by altering ways to perform ADLs. In addition, multiple significant results favored replantation in the subgroup with single-finger amputation (excluding thumb) distal to the PIP joint. In single-digit amputations proximal to the PIP joint, a patient-specific treatment plan should be formulated based on the patient’s occupation, personal needs, and motivation.
Finding only a marginal difference in MCP joint motion between patients with revision amputation vs replantation who sustained thumb-only amputations, with all other functional and PRO measures statistically equivalent, was unexpected and difficult to explain. It may be that, even with a short thumb, opposition can still be attained through other intact digits in an isolated thumb injury, especially when a large portion of the muscle and insertion of the opponens pollicis and flexor pollicis brevis are intact. Our data excluded patients with total thumb amputation at or proximal to the MCP joint, precluding comparison between patients with no thumb vs those with some remaining thumb length. A previous study42 comparing revision amputation and replantation in patients with distal to MCP thumb amputation reported similar functional results and ADL measures between the 2 cohorts and postulated that motivated patients can adapt to thumb amputations.42,43 Similarly, patients included in the present study were willing to return to the clinic more than 1 year after treatment to participate in more than 1 hour of surveys and functional tests. These participants were likely highly motivated patients who were invested in their recovery, heightening their chances of successful adaptation after thumb revision amputation. However, because not every patient is optimally motivated, we recommend replantation of all thumb amputations when possible because of its importance in opposition and overall hand function.
Limitations
To our knowledge, this is the first and largest multicenter study designed to compare both PROs and functional outcomes after revision amputation and replantation. Our study has some limitations. Because of the retrospective nature of this study, we were unable to collect baseline factors, and we were unable to account for all aspects of treatment, such as rehabilitation, complications, or other unmeasured confounders, which may have introduced bias. Some subgroup analyses were limited by inadequate power because of the relative rarity of certain injury patterns, which may have been insufficient to reach statistical significance. Another limitation inherent to retrospective studies is potential selection bias given the strong preferences for revision amputation or replantation by surgeon and center, leading to small sample size of some cohorts, such as the replantation group in the United States. A future prospective multicenter study can address the above limitations.
Conclusions
Patients with thumb, distal single finger, and 3 or more fingers amputated may have improved PROs when treated with replantation rather than revision amputation. In the remaining injury patterns, a patient-specific plan should be formulated based on the patient’s occupation, his or her motivation, and the technical feasibility of the procedure. Furthermore, a national traumatic digit injury management guideline that clearly delineates patients who may have better outcomes with replantation vs revision amputation is required to optimize patient outcomes. A cost-effectiveness analysis is warranted to further elucidate the long-term cost-utility of both procedures. For a replantation to be successful, technical capability, perioperative care, hand therapy, and postoperative follow-up are necessary. Therefore, tertiary referral hand centers equipped with such resources need to be designated by region.
eTable. Factors Associated With Type of Treatment
References
- 1.Chase RA. Costs, risks, and benefits of hand surgery. J Hand Surg Am. 1983;8(5, pt 2):644-648. doi: 10.1016/S0363-5023(83)80233-0 [DOI] [PubMed] [Google Scholar]
- 2.Giladi AM, McGlinn EP, Shauver MJ, Voice TP, Chung KC. Measuring outcomes and determining long-term disability after revision amputation for treatment of traumatic finger and thumb amputation injuries. Plast Reconstr Surg. 2014;134(5):746e-755e. doi: 10.1097/PRS.0000000000000591 [DOI] [PubMed] [Google Scholar]
- 3.Conn JM, Annest JL, Ryan GW, Budnitz DS. Non–work-related finger amputations in the United States, 2001-2002. Ann Emerg Med. 2005;45(6):630-635. doi: 10.1016/j.annemergmed.2004.10.012 [DOI] [PubMed] [Google Scholar]
- 4.Urbaniak JR, Roth JH, Nunley JA, Goldner RD, Koman LA. The results of replantation after amputation of a single finger. J Bone Joint Surg Am. 1985;67(4):611-619. doi: 10.2106/00004623-198567040-00017 [DOI] [PubMed] [Google Scholar]
- 5.Morrison WA, O’Brien BM, MacLeod AM. Evaluation of digital replantation: a review of 100 cases. Orthop Clin North Am. 1977;8(2):295-308. [PubMed] [Google Scholar]
- 6.Sears ED, Shin R, Prosser LA, Chung KC. Economic analysis of revision amputation and replantation treatment of finger amputation injuries. Plast Reconstr Surg. 2014;133(4):827-840. doi: 10.1097/PRS.0000000000000019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boulas HJ. Amputations of the fingers and hand: indications for replantation. J Am Acad Orthop Surg. 1998;6(2):100-105. doi: 10.5435/00124635-199803000-00004 [DOI] [PubMed] [Google Scholar]
- 8.Boyle D, Parker D, Larson C, Pessoa-Brandão L. Nature, incidence, and cause of work-related amputations in Minnesota. Am J Ind Med. 2000;37(5):542-550. doi: [DOI] [PubMed] [Google Scholar]
- 9.Chang DH, Ye SY, Chien LC, Ma H. Epidemiology of digital amputation and replantation in Taiwan: a population-based study. J Chin Med Assoc. 2015;78(10):597-602. doi: 10.1016/j.jcma.2015.03.005 [DOI] [PubMed] [Google Scholar]
- 10.Dabernig J, Hart AM, Schwabegger AH, Dabernig W, Harpf C. Evaluation outcome of replanted digits using the DASH score: review of 38 patients. Int J Surg. 2006;4(1):30-36. doi: 10.1016/j.ijsu.2006.01.003 [DOI] [PubMed] [Google Scholar]
- 11.Hannah SD. Psychosocial issues after a traumatic hand injury: facilitating adjustment. J Hand Ther. 2011;24(2):95-102. doi: 10.1016/j.jht.2010.11.001 [DOI] [PubMed] [Google Scholar]
- 12.de Putter CE, Selles RW, Polinder S, Panneman MJ, Hovius SE, van Beeck EF. Economic impact of hand and wrist injuries: health-care costs and productivity costs in a population-based study. J Bone Joint Surg Am. 2012;94(9):e56. doi: 10.2106/JBJS.K.00561 [DOI] [PubMed] [Google Scholar]
- 13.Galanakos SP, Bot AG, Zoubos AB, Soucacos PN. Psychological and social consequences after reconstruction of upper extremity trauma: methods of detection and management. J Reconstr Microsurg. 2014;30(3):193-206. [DOI] [PubMed] [Google Scholar]
- 14.Gavrilova N, Harijan A, Schiro S, Hultman CS, Lee C. Patterns of finger amputation and replantation in the setting of a rapidly growing immigrant population. Ann Plast Surg. 2010;64(5):534-536. [DOI] [PubMed] [Google Scholar]
- 15.Arakaki A, Tsai TM. Thumb replantation: survival factors and re-exploration in 122 cases. J Hand Surg Br. 1993;18(2):152-156. doi: 10.1016/0266-7681(93)90094-V [DOI] [PubMed] [Google Scholar]
- 16.Holmberg J, Arner M. Sixty five thumb replantations: a retrospective analysis of factors influencing survival. Scand J Plast Reconstr Surg Hand Surg. 1994;28(1):45-48. doi: 10.3109/02844319409015994 [DOI] [PubMed] [Google Scholar]
- 17.Zumiotti A, Ferreira MC. Replantation of digits: factors influencing survival and functional results. Microsurgery. 1994;15(1):18-21. doi: 10.1002/micr.1920150107 [DOI] [PubMed] [Google Scholar]
- 18.Mehri N, Sadeghi-Bazergani H, Safaiean A. Epidemiological and clinical characteristics of traumatic hand and finger amputations in north western Iran: a single center experience. Bull Emerg Trauma. 2017;5(1):42-46. [PMC free article] [PubMed] [Google Scholar]
- 19.Reavey PL, Stranix JT, Muresan H, Soares M, Thanik V. Disappearing digits: analysis of national trends in amputation and replantation in the United States. Plast Reconstr Surg. 2018;141(6):857e-867e. doi: 10.1097/PRS.0000000000004368 [DOI] [PubMed] [Google Scholar]
- 20.Payatakes AH, Zagoreos NP, Fedorcik GG, Ruch DS, Levin LS. Current practice of microsurgery by members of the American Society for Surgery of the Hand. J Hand Surg Am. 2007;32(4):541-547. doi: 10.1016/j.jhsa.2006.12.006 [DOI] [PubMed] [Google Scholar]
- 21.Brown M, Lu Y, Chung KC, Mahmoudi E. Annual hospital volume and success of digital replantation. Plast Reconstr Surg. 2017;139(3):672-680. doi: 10.1097/PRS.0000000000003087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahmoudi E, Chung KC. Effect of hospital volume on success of thumb replantation. J Hand Surg Am. 2017;42(2):96-103.e5. doi: 10.1016/j.jhsa.2016.11.020 [DOI] [PubMed] [Google Scholar]
- 23.Tessler O, Bartow MJ, Tremblay-Champagne MP, et al. Long-term health-related quality of life outcomes in digital replantation versus revision amputation. J Reconstr Microsurg. 2017;33(6):446-451. doi: 10.1055/s-0037-1601052 [DOI] [PubMed] [Google Scholar]
- 24.El-Diwany M, Odobescu A, Bélanger-Douet M, et al. Replantation vs revision amputation in single digit zone II amputations. J Plast Reconstr Aesthet Surg. 2015;68(6):859-863. doi: 10.1016/j.bjps.2015.02.033 [DOI] [PubMed] [Google Scholar]
- 25.Zhu H, Bao B, Zheng X. A comparison of functional outcomes and therapeutic costs: single-digit replantation versus revision amputation. Plast Reconstr Surg. 2018;141(2):244e-249e. [DOI] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang EY, Chung KC. Outcomes of trapeziectomy with a modified abductor pollicis longus suspension arthroplasty for the treatment of thumb carpometacarpal joint osteoarthritis. Plast Reconstr Surg. 2008;122(2):505-515. doi: 10.1097/PRS.0b013e31817d5419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chatterjee JS, Price PE. Comparative responsiveness of the Michigan Hand Outcomes Questionnaire and the Carpal Tunnel Questionnaire after carpal tunnel release. J Hand Surg Am. 2009;34(2):273-280. doi: 10.1016/j.jhsa.2008.10.021 [DOI] [PubMed] [Google Scholar]
- 29.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42(6):619-622. doi: 10.1097/00000637-199906000-00006 [DOI] [PubMed] [Google Scholar]
- 30.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23(4):575-587. doi: 10.1016/S0363-5023(98)80042-7 [DOI] [PubMed] [Google Scholar]
- 31.Waljee JF, Chung KC. Objective functional outcomes and patient satisfaction after silicone metacarpophalangeal arthroplasty for rheumatoid arthritis. J Hand Surg Am. 2012;37(1):47-54. doi: 10.1016/j.jhsa.2011.09.042 [DOI] [PubMed] [Google Scholar]
- 32.Sung NS, Crowley WF Jr, Genel M, et al. Central challenges facing the national clinical research enterprise. JAMA. 2003;289(10):1278-1287. doi: 10.1001/jama.289.10.1278 [DOI] [PubMed] [Google Scholar]
- 33.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand): the Upper Extremity Collaborative Group (UECG) [published correction appears in Am J Ind Med. 1996;30(3):372]. Am J Ind Med. 1996;29(6):602-608. doi: [DOI] [PubMed] [Google Scholar]
- 34.Nathan DG. Clinical research: perceptions, reality, and proposed solutions: National Institutes of Health Director’s Panel on Clinical Research. JAMA. 1998;280(16):1427-1431. doi: 10.1001/jama.280.16.1427 [DOI] [PubMed] [Google Scholar]
- 35.Ware JE Jr, Sherbourne CD. The MOS 36-Item Short Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30(6):473-483. doi: 10.1097/00005650-199206000-00002 [DOI] [PubMed] [Google Scholar]
- 36.Ware JE Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51(11):903-912. doi: 10.1016/S0895-4356(98)00081-X [DOI] [PubMed] [Google Scholar]
- 37.Alsaeed S, Alhomid T, Zakaria H, Alwhaibi R. Normative values of Two-Point Discrimination test among students of Princess Noura Bint Abdulrahman University in Riyadh. Int J Advanced Physiol Allied Sci. 2014;1(1):42-52. http://medical.cloud-journals.com/index.php/IJAPAS/article/view/Med-186. Accessed October 3, 2018. [Google Scholar]
- 38.Jones JM, Schenck RR, Chesney RB. Digital replantation and amputation: comparison of function. J Hand Surg Am. 1982;7(2):183-189. doi: 10.1016/S0363-5023(82)80085-3 [DOI] [PubMed] [Google Scholar]
- 39.Hattori Y, Doi K, Ikeda K, Estrella EP. A retrospective study of functional outcomes after successful replantation versus amputation closure for single fingertip amputations. J Hand Surg Am. 2006;31(5):811-818. doi: 10.1016/j.jhsa.2006.02.020 [DOI] [PubMed] [Google Scholar]
- 40.Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38(4):641-649. doi: 10.1016/j.jhsa.2012.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hung M, Tyser A, Saltzman CL, Wright Voss M, Bounsanga J, Kazmers NH. Establishing the minimal clinically important difference for the PROMIS and qDASH. J Hand Surg. 2018;43(9)(suppl):S22. doi: 10.1016/j.jhsa.2018.06.056 [DOI] [Google Scholar]
- 42.Goldner RD, Howson MP, Nunley JA, Fitch RD, Belding NR, Urbaniak JR. One hundred eleven thumb amputations: replantation vs revision. Microsurgery. 1990;11(3):243-250. doi: 10.1002/micr.1920110312 [DOI] [PubMed] [Google Scholar]
- 43.Brown PW. Less than ten: surgeons with amputated fingers. J Hand Surg Am. 1982;7(1):31-37. doi: 10.1016/S0363-5023(82)80010-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Factors Associated With Type of Treatment