Abstract
Importance
Physicians who are mothers face challenges with equal distribution of domestic duties, which can be an obstacle in career advancement and achieving overall job satisfaction.
Objectives
To study and report on the association between increased domestic workload and career dissatisfaction and if this association differed between proceduralists and nonproceduralists.
Design, Setting, and Participants
Data for this study were gathered from April 28 to May 26, 2015, via an online survey of 1712 attending physician mothers recruited from the Physician Moms Group. Statistical analysis was performed from August 25, 2017, to November 20, 2018.
Main Outcomes and Measures
Univariate analysis was performed for respondents who reported sole responsibility for 5 or more vs fewer than 5 main domestic tasks. Independent factors associated with career dissatisfaction or a desire to change careers were identified using a multivariate logistic regression model.
Results
Of the 1712 respondents, most were partnered or married (1698 [99.2%]), of which 458 (27.0%) were in procedural specialties. Overall, respondents reported having sole responsibility for most domestic tasks, and there were no statistically significant differences between procedural and nonprocedural groups. Physician mothers in procedural specialties primarily responsible for 5 or more domestic tasks reported a desire to change careers more often than those responsible for fewer than 5 tasks (105 of 191 [55.0%] vs 114 of 271 [42.1%]; P = .008). This difference was not noted in physician mothers in nonprocedural specialties. In multivariate analysis of the proceduralist cohort, primary responsibility for 5 or more tasks was identified as a factor independently associated with the desire to change careers (odds ratio, 1.5; 95% CI, 1.0-2.2; P = .05).
Conclusions and Relevance
Physician mothers report having more domestic responsibilities than their partners. For proceduralist mothers, self-reported higher levels of domestic responsibility were associated with career dissatisfaction. Increasing numbers of mothers in the medical workforce may create a demand for more equitable distribution and/or outsourcing of domestic tasks.
This survey study of physician mothers examines the association between increased domestic workload and career dissatisfaction, and whether this association differs between proceduralists and nonproceduralists.
Key Points
Question
Is increased domestic workload, particularly for proceduralists, associated with career dissatisfaction among physicians who are mothers?
Findings
In this survey study, physician mothers in procedural specialties who were solely responsible for 5 or more domestic tasks reported a desire to change careers more often than did those responsible for fewer than 5 tasks (55.0% vs 42.1%).
Meaning
For proceduralist mothers, self-reported higher levels of domestic responsibility were associated with career dissatisfaction; increasing numbers of mothers in the medical workforce may create a demand for more equitable distribution and/or outsourcing of domestic tasks.
Introduction
In 2016, the graduating classes from all medical schools in the United States were 50% female.1 Unfortunately, despite equal enrollment in medical schools, women are still underrepresented in procedural and surgical specialties. Of all graduating medical students, only 14% of women apply to surgical residencies compared with 33% of men, and many female residents are concentrated in internal medicine, family medicine, and pediatrics.2,3 Trainees with concerns regarding fertility and work-life balance are more likely to consider what they perceive to be more lifestyle-compatible fields.4 Accordingly, prior work has shown that physician mothers in procedural specialties are more likely than their peers in nonprocedural specialties to require assisted reproduction, to have short maternity leave, and to have difficulty arranging coverage for missed work.5
Studies have shown that, irrespective of sex, physicians with children tend to be less satisfied with their careers than those without children.6 The association between career satisfaction and work performance or career advancement is complex, and it is difficult to distinguish the cause from the outcome. However, studies in organizational psychology have shown that career satisfaction plays a significant role in the promotion of “citizenship” behaviors or the creation of a more supportive and productive work environment for those around them that can subsequently have a positive influence on performance and career trajectories.7 For many physician mothers, career satisfaction is intertwined with work-life challenges, partially because of the competing burden of domestic responsibilities.6,8 Female surgeons are more likely than their male colleagues to be in dual-career relationships and are also more likely to have children at earlier phases of their career.4 These factors may result in a greater burden of domestic responsibilities that could hinder early academic productivity and advancement to leadership positions. Similarly, female physicians in academic family medicine cite significant challenges in balancing responsibilities between work and home and child care.9
It is currently unknown whether these specific challenges integrating work and family life are different for physician mothers in procedural specialties and those in nonprocedural specialties, and if these challenges are associated with career dissatisfaction. Thus, the aim of this study was to characterize domestic responsibilities and their association with career dissatisfaction using a large, nationwide sample of physician mothers in both procedural and nonprocedural specialties.
Methods
A sample of female physician mothers was recruited from the Physician Moms Group (PMG), as previously reported.10 At the time of the study, there were 14 518 members. A link to an anonymous, secure questionnaire was posted on the PMG Facebook page on April 28, 2015, and remained active for 4 weeks until May 26, 2015. Repeated submissions were limited by IP address. The study was reviewed by the University of Massachusetts and Brigham and Women’s Hospital Institutional Review Boards and was found to be exempt because of the anonymous nature of the survey. Participants provided written informed consent.
Data analyses for the current study were limited to currently practicing US attending physicians. Procedural specialties were defined as all surgical specialties, anesthesiologists, gastroenterologists, and obstetricians-gynecologists. Surgical specialties included all surgical subspecialties as well as obstetricians-gynecologists. Practice setting was categorized as academic, private, locum tenens, rural, or community based. Other demographic data collected included age, race/ethnicity, marital status, current practice type and location, full-time equivalent, spouse or partner’s occupation, number of children, income, and years in practice. Missing values were excluded by line.
Data on 11 total tasks were gathered. Statistical analysis was performed from August 25, 2017, to November 20, 2018. Five tasks were chosen as the cutoff to develop comparison groups. Univariate analysis was performed using χ2 tests. A multivariate logistic regression model was created to study the association of partner occupation with the respondents’ desire to switch to a less demanding career or specialty while controlling for potential confounders. Variables were chosen based on contextual plausibility and statistical significance on initial univariate analysis. All P values were from 2-sided tests, and results were deemed statistically significant at P ≤ .05. All analyses were performed using the computing environment R (R Development Core Team).
Results
There were 2363 respondents to the survey with an estimated response rate of at least 16.3%, calculated using the total number of PMG members at the time of the survey (14 518). We could not determine the true response rate given the inability to determine the number of PMG users who saw the survey. Analysis was limited to 1930 respondents who were attending physicians, of which 1430 (74.1%) were in nonprocedural specialties and 500 (25.9%) were in procedural specialties. After excluding respondents with missing line items, there was a total of 1712 attending physicians: 1250 (73.0%) from nonprocedural specialties and 462 (27.0%) from procedural specialties. Demographic data are shown in Table 1, grouped by specialty (procedural vs nonprocedural) and number of primary domestic tasks (<5 vs ≥5).
Table 1. Demographic Characteristics of Respondents.
| Characteristic | Nonprocedural (n = 1250) | Procedural (n = 462) | ||||
|---|---|---|---|---|---|---|
| <5 Tasks, No. (%) (n = 620) | ≥5 Tasks, No. (%) (n = 630) | P Value | <5 Tasks, No. (%) (n = 271) | ≥5 Tasks, No. (%) (n = 191) | P Value | |
| Age, y | ||||||
| 25-30 | 13 (2.1) | 12 (1.9) | <.001 | 2 (0.7) | 1 (0.5) | .05 |
| 31-35 | 351 (56.6) | 302 (47.9) | 142 (52.4) | 84 (44.0) | ||
| 36-40 | 226 (36.5) | 241 (38.9) | 114 (42.1) | 85 (44.5) | ||
| >40 | 30 (4.8) | 75 (12.1) | 13 (4.8) | 21 (11.0) | ||
| Race/ethnicity | ||||||
| White | 427 (68.9) | 440 (69.8) | .76 | 189 (69.7) | 133 (69.6) | .07 |
| Black | 18 (2.9) | 25 (4.0) | 9 (3.3) | 15 (7.9) | ||
| Hispanic | 15 (2.4) | 17 (2.7) | 9 (3.3) | 5 (2.6) | ||
| Asian | 117 (18.9) | 108 (17.4) | 43 (15.9) | 32 (16.8) | ||
| Other | 43 (6.9) | 40 (6.5) | 21 (7.7) | 6 (3.1) | ||
| Marital status | ||||||
| Married | 617 (99.5) | 613 (97.3) | .03 | 268 (98.9) | 185 (96.9) | .06 |
| Divorced | 1 (0.2) | 4 (0.6) | 0 | 4 (2.1) | ||
| Domestic partnership | 2 (0.3) | 8 (1.3) | 3 (1.1) | 2 (1.0) | ||
| Separated | 0 | 4 (0.6) | 0 | 0 | ||
| Widowed | 0 | 1 (0.2) | 0 | 0 | ||
| Current practice location | ||||||
| Academic | 234 (37.7) | 215 (34.1) | .78 | 94 (34.7) | 57 (29.8) | .10 |
| Community | 169 (27.3) | 180 (28.6) | 47 (17.3) | 38 (19.9) | ||
| Locum tenens | 2 (0.3) | 4 (0.6) | 1 (0.4) | 0 | ||
| NA | 7 (1.1) | 9 (1.5) | 3 (1.1) | 0 | ||
| Private | 194 (31.3) | 208 (33.5) | 117 (43.2) | 95 (49.7) | ||
| Rural | 14 (2.3) | 14 (2.3) | 9 (3.3) | 1 (0.5) | ||
| Work | ||||||
| Full-time | 494 (79.7) | 385 (61.1) | <.001 | 244 (90.0) | 155 (81.2) | .09 |
| Part-time | 126 (20.3) | 245 (38.9) | 27 (10.0) | 36 (18.8) | ||
| Spouse occupation | ||||||
| Physician | 136 (21.9) | 232 (36.8) | <.001 | 40 (14.8) | 58 (30.4) | <.001 |
| Surgeon | 20 (3.2) | 41 (6.5) | 18 (6.6) | 35 (18.3) | ||
| Employed part-time | 25 (4.0) | 20 (3.2) | 14 (5.2) | 4 (2.1) | ||
| Full-time professional | 316 (51.0) | 309 (49.8) | 139 (51.3) | 83 (43.5) | ||
| Stay-at-home father | 108 (17.4) | 18 (2.9) | 54 (19.9) | 7 (3.7) | ||
| Student | 15 (2.4) | 7 (1.1) | 6 (2.2) | 4 (2.1) | ||
| Disabled | 0 | 3 (0.5) | 0 | 0 | ||
| Children, No. | ||||||
| 0 | 6 (1.0) | 4 (0.6) | <.001 | 7 (2.6) | 0 | .004 |
| 1 | 237 (38.2) | 180 (28.6) | 92 (33.9) | 51 (26.7) | ||
| 2 | 284 (45.8) | 304 (49.0) | 121 (44.6) | 97 (50.8) | ||
| ≥3 | 93 (15.0) | 143 (23.1) | 51 (18.8) | 43 (22.5) | ||
| Gross household income, $ | ||||||
| <100 000 | 4 (0.6) | 7 (1.1) | <.001 | 2 (0.7) | 1 (0.5) | .20 |
| 100 000-199 999 | 153 (24.7) | 116 (18.4) | 24 (8.9) | 21 (11.0) | ||
| 200 000-299 999 | 237 (38.2) | 197 (31.8) | 68 (25.1) | 41 (21.5) | ||
| 300 000-399 999 | 116 (18.7) | 152 (24.5) | 81 (29.9) | 47 (24.6) | ||
| 400 000-499 999 | 58 (9.4) | 66 (10.6) | 51 (18.8) | 30 (15.7) | ||
| 500 000-749 999 | 40 (6.5) | 70 (11.3) | 37 (13.7) | 41 (21.5) | ||
| 750 000-999 000 | 12 (1.9) | 22 (3.5) | 8 (3.0) | 10 (5.2) | ||
| Provide >50% of household income | ||||||
| Yes | 430 (69.4) | 342 (54.3) | <.001 | 53 (19.6) | 64 (33.5) | .001 |
| No | 190 (30.6) | 288 (45.7) | 218 (80.4) | 127 (66.5) | ||
| Years in practice | ||||||
| 0-2 | 149 (24.0) | 132 (21.0) | <.001 | 94 (34.7) | 44 (23.0) | .002 |
| 3-4 | 217 (35.0) | 154 (24.4) | 79 (29.2) | 55 (28.8) | ||
| 5-6 | 146 (23.5) | 164 (26.5) | 63 (23.2) | 43 (22.5) | ||
| ≥7 | 108 (17.4) | 180 (29.0) | 35 (12.9) | 49 (25.7) | ||
Abbreviation: NA, not applicable.
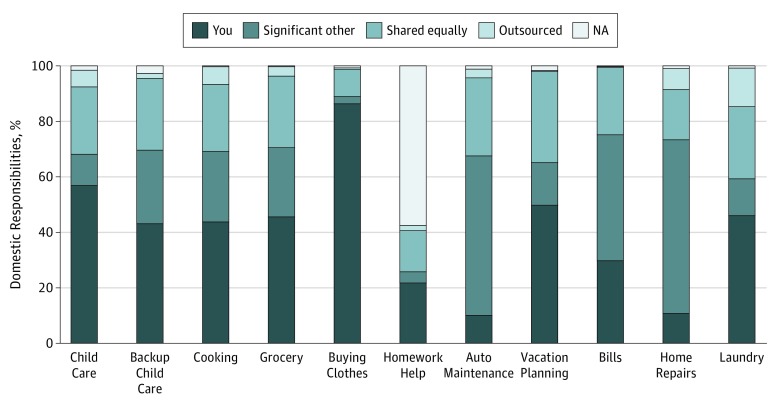
Breakdown of Domestic Tasks
Overall, physician mothers reported having sole responsibility for most domestic tasks compared with their spouse or partner, including routine child care plans (980 of 1712 [57.2%] vs 191 of 1712 [11.2%]), back-up or emergency child care plans (744 of 1712 [43.5%] vs 451 of 1712 [26.3%]), cooking (752 of 1712 [43.9%] vs 435 of 1712 [25.4%]), shopping for groceries (786 of 1712 [45.9%] vs 425 of 1712 [24.8%]), shopping for children’s clothing (1480 of 1712 [86.4%] vs 47 of 1712 [2.7%]), vacation planning (859 of 1712 [50.2%] vs 260 of 1712 [15.2%]), helping with homework (379 of 1712 [22.1%] vs 66 of 1712 [3.9%]), and laundry (794 of 1712 [46.4%] vs 225 of 1712 [13.1%]) (Figure). By contrast, physician mothers reported that their spouses or partners were more likely to have sole responsibility for home repairs (1072 of 1712 [62.6%] vs 188 of 1712 [11.0%]), finances (777 of 1712 [45.4%] vs 514 of 1712 [30.0%]), and automobile maintenance (984 of 1712 [57.5%] vs 175 of 1712 [10.2%]). There were no significant differences in the breakdown of domestic tasks in procedural vs nonprocedural specialties.
Figure. Breakdown of Domestic Responsibilities.
NA indicates not applicable.
Subgroup Analysis Based on Procedural Status
Physician mothers in nonprocedural specialties who were primarily responsible for 5 or more domestic tasks were compared with those who were responsible for fewer than 5 domestic tasks (Table 1). Of the 1712 physician mothers surveyed, 821 (48.0%) reported that they were primarily responsible for 5 or more domestic tasks compared with 891 (52.0%) who reported they were responsible for fewer than 5 tasks. Nonproceduralists who were primarily responsible for 5 or more tasks were significantly more likely to be older, unmarried or unpartnered or partnered to a physician or surgeon, and have more than 1 child. They were also more likely to be working part-time, have a gross household income more than $300 000 annually, contribute less than 50% of the household income, and have been in practice 5 or more years.
Physician mothers in procedural specialties who were primarily responsible for 5 or more domestic tasks were compared with those who were responsible for fewer than 5 domestic tasks, and multiple significant differences were found between the 2 groups on bivariate analysis (Table 1). Physicians in procedural specialties who were primarily responsible for 5 or more domestic tasks were significantly more likely to be partnered to a physician or surgeon and have more than 1 child. They were also more likely to contribute more than 50% of the household income and have been in practice 7 or more years.
Domestic Tasks and Career Satisfaction
Univariate analysis was performed separately for both the procedural and nonprocedural groups to determine whether having sole responsibility for 5 or more domestic tasks compared with fewer than 5 domestic tasks was associated with career dissatisfaction, defined as a greater desire to switch to a less demanding career or specialty (Table 2). For nonproceduralists, there was no association between increased primary domestic responsibility and career dissatisfaction (<5 tasks, 202 of 620 [32.6%] vs ≥5 tasks, 204 of 630 [32.4%]; P > .99). By contrast, among proceduralists, those who were primarily responsible for 5 or more domestic tasks were significantly more likely to have a desire to change careers compared with those who perform fewer than 5 domestic tasks (105 of 191 [55.0%] vs 114 of 271 [42.1%]; P = .008). The association between increased primary domestic responsibility and desire to switch to a less demanding career or specialty was conserved when a subgroup analysis was performed for surgical specialties (Table 3).
Table 2. Desire to Switch to a Different Career or Specialty.
| Desire to Switch to Less Demanding Career or Specialty | Nonprocedural (n = 1250) | Procedural (n = 462) | ||||
|---|---|---|---|---|---|---|
| <5 Tasks, No. (%) (n = 620) | ≥5 Tasks, No. (%) (n = 630) | P Value | <5 Tasks, No. (%) (n = 271) | ≥5 Tasks, No. (%) (n = 191) | P Value | |
| Yes | 202 (32.6) | 204 (32.4) | >.99 | 114 (42.1) | 105 (55.0) | .008 |
| No | 418 (67.4) | 426 (67.6) | 157 (57.9) | 86 (45.0) | ||
Table 3. Surgeon-Specific Desire to Switch to a Different Career or Specialty.
| Desire to Switch to Less Demanding Career or Specialty | Nonsurgical (n = 1357) | Surgical (n = 355) | ||||
|---|---|---|---|---|---|---|
| <5 Tasks, No. (%) (n = 681) | ≥5 Tasks, No. (%) (n = 676) | P Value | <5 Tasks No. (%) (n = 210) | ≥5 Tasks No. (%) (n = 145) | P Value | |
| Yes | 226 (33.2) | 227 (33.6) | .95 | 90 (42.9) | 82 (56.6) | .02 |
| No | 455 (66.8) | 449 (66.4) | 120 (57.1) | 63 (43.4) | ||
Adjusted Analysis of the Procedural Group
A multivariate logistic regression analysis was performed in the procedural physician mothers cohort to identify independent factors associated with the desire to switch to a less demanding career or specialty (Table 4). Variables included in the model were age, practice type, total household income, years of experience, spouse or partner occupation, and having primary responsibility for 5 or more domestic tasks. Primary responsibility for 5 or more domestic tasks was found to be the only factor independently associated with a desire to switch to a less demanding career or specialty (odds ratio, 1.5; 95% CI, 1.0-2.2; P = .05).
Table 4. Multivariate Logistic Regression Analysis of Variables Associated With Career Dissatisfaction for Proceduralists.
| Variable | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Primarily responsible for ≥5 domestic tasks | 1.5 (1.0-2.2) | .05 |
| Age | 1.0 (0.7-1.4) | .98 |
| Practice type | 1.0 (0.9-1.2) | .41 |
| Total income | 0.9 (0.8-1.1) | .22 |
| Years in practice | 1.2 (0.9-1.4) | .17 |
| Spouse or partner’s occupation status | 0.9 (0.8-1.0) | .13 |
Discussion
In this study, we found that physician mothers in procedural and surgical specialties who self-report primary responsibility for significant domestic needs are also more likely to report a desire to change careers compared with those who have more even division of domestic tasks. This association was not present among nonprocedural physician mothers.
Our results are consistent with previous findings by other investigators. A 2011 survey study demonstrated substantial differences in the experience of female and male surgeons and showed that women were more likely to have work-family conflicts and higher incidence of burnout and emotional exhaustion.2 Similarly, in a smaller 2017 survey study, women surgeons were found to be disproportionately more responsible for household functions than were male surgeons despite a higher proportion of female surgeons being married to a full-time working professional.1 A systematic review of the literature on female physicians and work-family conflict demonstrated the significant weight of family issues on career choice and also found that parenthood had a negative association with career trajectories, particularly for surgeons.11
Respondents in nonprocedural specialties did not report a significant desire to switch careers or specialty regardless of the amount of responsibilities they had at home. A survey study of primary care and nonsurgical physicians in 2000 showed that parental status was not associated with burnout in female physicians.12 The reasons for this difference are unclear; however, physician mothers who choose what they believe to be a more lifestyle-compatible specialty may be more satisfied when their expectations of their time commitment to parenting and work-life balance is met.
Unequal distribution of domestic labor has been documented as one of the factors behind the underrepresentation of women in academic leadership positions, slow career advancement, lower academic productivity of women, and poor recruitment of women to certain medical specialties.13 Women often cite a lack of sufficient time developing scientific knowledge and research as an impediment to performing clinical research and applying for prestigious research grants.14 Family-professional role conflicts are also cited as a significant factor in physician mothers’ limited time to expand their practice and increase their academic productivity.14 Female physicians are also less likely to work at university hospitals and research institutions.6
Women who choose medicine as a career are often highly motivated and goal oriented; however, many studies show that women, particularly those in procedural specialties, are less satisfied with their career choice, with increased rates of burnout and depression. A study at the Mayo Clinic showed that physicians who reported higher rates of recent work-home conflicts were more likely to report symptoms of emotional exhaustion and depersonalization, 2 important metrics of burnout from the Maslach Burnout Inventory.15 In a previously cited study on surgeons, female respondents were more likely to report that they would not become a surgeon or physician again if given the choice.2 Concerns regarding childbearing and the burden of domestic responsibilities fall harder on trainees who report more negative experiences in residency and higher levels of depression and stress than their male cohorts.16
Our study findings help identify key areas for positive interventions. Extended child care services during and beyond working hours, as well as increased flexibility in scheduling, will help both male and female physicians maintain more healthy and sustainable work-life integration. Particularly in the era of increasing dual-income households, parental leave should be emphasized rather than maternity leave. Fathers should be given equal opportunity to take advantage of career and scheduling flexibility that allows them the time to equitably participate in domestic responsibilities. Moreover, encouragement of more equitable division of household labor as well as outsourcing of domestic tasks can also reduce work-family conflicts in dual-physician households. For dual-career relationships in which work-family conflicts can adversely affect both parents, there should be education emphasizing effective time management skills, which often promotes the inclusion of those outside the immediate household, such as extended family members and professional care professionals. Above all, a culture shift is needed in and out of the workplace to view parenting and domestic tasks as shared responsibilities, particularly for dual-career couples. In some institutions, prorated tenure tracks have been implemented to support academic physicians achieve more flexible and family-friendly careers.17
Limitations
Our study has several limitations. The data are drawn from a group with voluntary membership, which can introduce bias; thus, the data may not be representative of all physician mothers. However, our study cohort does represent a broad geographic distribution, and our breakdown by specialty is similar to those in the most recent data from the Association of American Medical Colleges.18 The true response rate is impossible to determine, as it is not possible to find out what percentage of the PMG members saw the posting to the survey. Also, this was a retrospective survey, and recall bias may have influenced self-reported answers. Spouses and partners were not surveyed and may have introduced confirmation bias for those surveyed. The choice of 5 domestic tasks as the cutoff was loosely based on recent studies demonstrating overall sex distribution for unpaid work. Data from the Organization for Economic Cooperation and Development show that, averaged across all 34 member countries, men spend 9% of their total time per day on unpaid housework while women spend double that amount of time on the same activities.19 Another study using the European Social Survey of 20 European countries showed that men’s mean share of total housework is about 30%.20 Given these statistics, we chose 5 of 11 total tasks (roughly 45%) as the cutoff; however, this number may not accurately depict the total amount of hours spent on housework, as some duties are more or less time consuming than others. In addition, while our multivariable model does include multiple key variables thought to be possibly associated with career satisfaction, there may be other confounders that may otherwise account for our findings. Finally, we attempted to distinguish between proceduralists and nonproceduralists by grouping specialties as procedure heavy vs medical; however, there is significant variation among these fields, with some tracks within procedural specialties that are much more family friendly than others. This difference may warrant further study with more granular data on individual specialties and practice types.
Conclusions
Overall, physician mothers continue to carry more domestic responsibility than their spouses or partners, even when they are both physicians. Physician mothers in surgical specialties who claim sole responsibility for most domestic tasks are more likely to report a desire to change careers compared with those who claim responsibility for fewer than 5 domestic tasks. More equitable distribution and/or outsourcing of domestic tasks should be considered to sustain physician mothers in procedural and surgical specialties.
References
- 1.Baptiste D, Fecher AM, Dolejs SC, et al. Gender differences in academic surgery, work-life balance, and satisfaction. J Surg Res. 2017;218:99-107. doi: 10.1016/j.jss.2017.05.075 [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011;146(2):211-217. doi: 10.1001/archsurg.2010.310 [DOI] [PubMed] [Google Scholar]
- 3.Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex differences in academic rank in US medical schools in 2014. JAMA. 2015;314(11):1149-1158. doi: 10.1001/jama.2015.10680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scully RE, Stagg AR, Melnitchouk N, Davids JS. Pregnancy outcomes in female physicians in procedural versus non-procedural specialties. Am J Surg. 2017;214(4):599-603. doi: 10.1016/j.amjsurg.2017.06.016 [DOI] [PubMed] [Google Scholar]
- 5.Davids JS, Scully RE, Melnitchouk N. Impact of procedural training on pregnancy outcomes and career satisfaction in female postgraduate medical trainees in the United States. J Am Coll Surg. 2017;225(3):411-418.e2. doi: 10.1016/j.jamcollsurg.2017.05.018 [DOI] [PubMed] [Google Scholar]
- 6.Buddeberg-Fischer B, Stamm M, Buddeberg C, et al. The impact of gender and parenthood on physicians’ careers—professional and personal situation seven years after graduation. BMC Health Serv Res. 2010;10:40. doi: 10.1186/1472-6963-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson CA, Johnson BE, Liese BS. Dual-doctor marriages: career development. Fam Med. 1992;24(3):205-208. [PubMed] [Google Scholar]
- 8.Bateman TS, Organ DW. Job satisfaction and the good soldier: the relationship between affect and employee “citizenship.”. Acad Manage J. 1983;26(4):587-595. doi: 10.5465/255908 [DOI] [Google Scholar]
- 9.Schrager S, Kolan A, Dottl SL. Is that your pager or mine: a survey of women academic family physicians in dual physician families. WMJ. 2007;106(5):251-255. [PubMed] [Google Scholar]
- 10.Scully RE, Davids JS, Melnitchouk N. Impact of procedural specialty on maternity leave and career satisfaction among female physicians. Ann Surg. 2017;266(2):210-217. doi: 10.1097/SLA.0000000000002196 [DOI] [PubMed] [Google Scholar]
- 11.Treister-Goltzman Y, Peleg R. Female physicians and the work-family conflict. Isr Med Assoc J. 2016;18(5):261-266. [PubMed] [Google Scholar]
- 12.Bakken LL, Sheridan J, Carnes M. Gender differences among physician-scientists in self-assessed abilities to perform clinical research. Acad Med. 2003;78(12):1281-1286. doi: 10.1097/00001888-200312000-00018 [DOI] [PubMed] [Google Scholar]
- 13.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K; The SGIM Career Satisfaction Study Group . The work lives of women physicians: results from the physician work life study. J Gen Intern Med. 2000;15(6):372-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reed DA, Enders F, Lindor R, McClees M, Lindor KD. Gender differences in academic productivity and leadership appointments of physicians throughout academic careers. Acad Med. 2011;86(1):43-47. doi: 10.1097/ACM.0b013e3181ff9ff2 [DOI] [PubMed] [Google Scholar]
- 15.Dyrbye LN, West CP, Satele D, Sloan JA, Shanafelt TD. Work/home conflict and burnout among academic internal medicine physicians. Arch Intern Med. 2011;171(13):1207-1209. doi: 10.1001/archinternmed.2011.289 [DOI] [PubMed] [Google Scholar]
- 16.Serrano K. Women residents, women physicians and medicine’s future. WMJ. 2007;106(5):260-265. [PubMed] [Google Scholar]
- 17.Fox G, Schwartz A, Hart KM. Work-family balance and academic advancement in medical schools. Acad Psychiatry. 2006;30(3):227-234. doi: 10.1176/appi.ap.30.3.227 [DOI] [PubMed] [Google Scholar]
- 18.Association of American Medical Colleges 2016 Physician specialty data report. https://www.staging.aamc.org/data/workforce/reports/457712/2016-specialty-databook.html. Accessed October 19, 2017.
- 19.Organization for Economic Cooperation and Development Balancing paid work, unpaid work and leisure. http://www.oecd.org/gender/data/balancingpaidworkunpaidworkandleisure.htm. Published July 3, 2014. Accessed September 20, 2018.
- 20.Fahlen S. Equality at home—a question of career? housework, norms, and policies in a European comparative perspective. Demogr Res. 2016;35(38):1411-1440. doi: 10.4054/DemRes.2016.35.48 [DOI] [Google Scholar]