Abstract
Importance
Developmental dyslexia (DD) is a specific learning disability of neurobiological origin whose core cognitive deficit is widely believed to involve language (phonological) processing. Although reading is also a visual task, the potential role of vision in DD has been controversial, and little is known about the integrity of visual function in individuals with DD.
Objective
To assess the frequency of visual deficits (specifically vergence, accommodation, and ocular motor tracking) in children with DD compared with a control group of typically developing readers.
Design, Setting, and Participants
A prospective, uncontrolled observational study was conducted from May 28 to October 17, 2016, in an outpatient ophthalmology ambulatory clinic among 29 children with DD and 33 typically developing (TD) children.
Main Outcomes and Measures
Primary outcomes were frequencies of deficits in vergence (amplitude, fusional ranges, and facility), accommodation (amplitude, facility, and accuracy), and ocular motor tracking (Developmental Eye Movement test and Visagraph eye tracker).
Results
Among the children with DD (10 girls and 19 boys; mean [SD] age, 10.3 [1.2] years) and the TD group (21 girls and 12 boys; mean [SD] age, 9.4 [1.4] years), accommodation deficits were more frequent in the DD group than the TD group (16 [55%] vs 3 [9%]; difference = 46%; 95% CI, 25%-67%; P < .001). For ocular motor tracking, 18 children in the DD group (62%) had scores in the impaired range (in the Developmental Eye Movement test, Visagraph, or both) vs 5 children in the TD group (15%) (difference, 47%; 95% CI, 25%-69%; P < .001). Vergence deficits occurred in 10 children in the DD group (34%) and 5 children in the TD group (15%) (difference, 19%; 95% CI, –2.2% to 41%; P = .08). In all, 23 children in the DD group (79%) and 11 children in the TD group (33%) had deficits in 1 or more domain of visual function (difference, 46%; 95% CI, 23%-69%; P < .001).
Conclusions and Relevance
These findings suggest that deficits in visual function are far more prevalent in school-aged children with DD than in TD readers, but the possible cause and clinical relevance of these deficits are uncertain. Further study is needed to determine the extent to which treating these deficits can improve visual symptoms and/or reading parameters.
This cohort study assesses the frequency of visual deficits (specifically vergence, accommodation, and ocular motor tracking) in children with developmental dyslexia compared with a control group of typically developing readers.
Key Points
Question
Are deficits in visual function more frequent in children with developmental dyslexia than in typically developing readers?
Findings
In this cohort study, school-aged children with developmental dyslexia exhibited more deficits in visual function—vergence, accommodation, and/or ocular motor tracking—than did a nonrandomized control group of typically developing children.
Meaning
These findings suggest that visual function deficits contribute to reading acquisition in children with developmental dyslexia.
Introduction
Developmental dyslexia (DD) is a reading disorder that emerges in childhood. The primary deficit involves impaired single-word decoding, word recognition, and spelling, which may affect the a child’s reading rate, comprehension, and written expression later on. The disorder is generally viewed as stemming from a core linguistic deficit in phonological processing; the recommended interventions are educational and are theoretically guided by this premise.1 Although experts have historically dismissed claims that visual processing might contribute meaningfully to the deficits present in DD,2,3 vision therapy has been recommended for decades by behavioral optometrists to improve purported visual symptoms.4,5,6
Vision therapy is based on the premise that correcting peripheral visual deficits (specifically vergence, accommodation, and ocular motor tracking) will improve reading performance, yet there is a dearth of controlled studies documenting that such deficits are more common in children with DD, much less whether treating them could improve reading. A well-documented accounting of whether visual deficits are more prevalent in children with DD is thus a necessary prerequisite to any controlled evaluation of interventions to correct such deficits.
The primary goal of this study, therefore, was to assess the prevalence and nature of visual deficits in children with dyslexia and compare them with a control group of typically developing (TD) readers. We sought to provide initial estimates of what visual functions specifically are affected in children with DD, the frequency and magnitude of any abnormal findings, and whether these deficits cluster in a subgroup of readers with dyslexia or are more evenly distributed across the population.
Methods
Study Design and Participants
A prospective, uncontrolled, group comparison observational study was conducted from May 28 to October 17, 2016. Children who received a diagnosis of DD were recruited from a hospital-based clinic, and a control group of TD readers were recruited from patients receiving standard eye examinations in the same hospital, as well as by flyers and word of mouth. Informed written assent was obtained from each participant, and informed written consent was obtained from each parent or guardian. The ethics committee of Boston Children’s Hospital approved the research protocol. The entire study was conducted according to the principles of the Declaration of Helsinki.7
Inclusion criteria for the DD group were diagnosis of DD, 7 to 11 years of age, best-corrected visual acuity better than or equal to 20/25 in each eye, and residing within 120 km (75 miles) of the research site. Exclusion criteria were diagnosis of attention-deficit/hyperactivity disorder documented by questionnaires, IQ less than 70, diagnosis of a comorbid neurodevelopmental disorder (eg, autism spectrum disorder, brain malformation, or neurogenetic disorder) or medical illness, history of eye surgery, structural anomalies of the anterior or posterior segment of the eye or medical condition that could affect the ability to participate in the study, or other ocular pathologic conditions. The inclusion and exclusion criteria for the TD group were the same except that the child must not have received a diagnosis of DD or extra reading support within either general or special education. Of 50 potentially eligible children identified with DD, 29 agreed to participate and completed the evaluation. Thirty-three children participated in the TD group.
Procedure
Participants were invited to the laboratory for a visit of approximately 2 hours, during which psychoeducational testing, a comprehensive eye examination, and visual function measures were performed as detailed herein.
Measures
Psychoeducational Testing
Psychoeducational testing included documentation of IQ (2-subtest version of the Wechsler Abbreviated Scale of Intelligence–II) and of single-word reading and spelling (Woodcock Reading Mastery Test, Word Identification and Word Attack subtests, and Test of Written Spelling).
Vision Testing
Vision testing included a standard eye examination including pupil dilation and cycloplegic refraction. A detailed description of the assessments of visual function—vergence, accommodation, and ocular motor tracking—is provided in the eAppendix in the Supplement. In brief, vergence was assessed for amplitude, fusional ranges, and facility. Accommodation was assessed for amplitude, facility, and accuracy. Ocular motor tracking was assessed using 2 methods: a printed test involving numbers oriented vertically and horizontally (Developmental Eye Movement [DEM] test) and an infrared eye tracking test performed during reading activities (Visagraph). These assessments were performed with appropriate refractive correction in place and in free space.
eTable 1 in the Supplement details the diagnoses for vergence and accommodation deficits and their corresponding criteria.8,9,10,11 For the ocular motor tracking parameters, DEM and Visagraph, scores below the 25th percentile for the TD group were considered abnormal in the absence of well-established criteria in the literature. For measures of accommodation performed monocularly, the value from the eye with the lowest performance was used for analysis.
Statistical Analysis
Group differences in demographic characteristics, psychoeducational performance, vision, and visual function assessments were assessed by t tests for continuous variables and χ2 tests for categorical variables. For continuous variables, F tests based on univariate analysis of variance and 2-way analysis of covariance (ANCOVA) were performed to evaluate group differences, adjusting for age, sex, and IQ differences as appropriate. All 95% CIs were calculated using the Wilson method.12 A 2-sided P < .01 was used to address type I errors due to multiple outcome analyses and testing.13 Statistical analysis was performed using SPSS Statistics, version 23.0 (IBM Corp).
Results
Participant Characteristics
The Table shows the demographic and psychometric characteristics of the participants in both groups. The DD group was somewhat older (mean [SD] age, 10.3 [1.2] years vs 9.4 [1.4] years) and had a higher proportion of boys than the TD group (19 [66%] vs 12 [36%]), as is typical; the TD group had a higher proportion of Asian children than the DD group (17 [52%] vs 0). The mean (SD) IQ for the DD group was in the average range (104.97 [12.05]), but the mean (SD) IQ for the TD group was in the high average range (117.88 [10.83]). There were group differences in reading and spelling (Word Identification, t = 12.32; Word Attack, t = 9.2; and Spelling, t = 8.45; all P < .001), which remained highly significant after adjusting for IQ (Word Identification, F = 101.07; Word Attack, F = 48.92; and Spelling, F = 39.65; all P < .001). All parametric analyses for the vision measures were adjusted for age and sex. Using ANCOVA, we did not find IQ to be a significant covariate or to change the findings in a meaningful way, so it was not included as a covariate for the vision measures.
Table. Demographic Characteristics and Performance of Psychoeducational Measures of Developmental Dyslexia and Typical Reading Groups.
| Characteristic | Individuals With Developmental Dyslexia (n = 29) | Typically Developing Readers (n = 33) |
|---|---|---|
| Age, mean (SD), y | 10.3 (1.2) | 9.4 (1.4) |
| Male, No. (%) | 19 (66) | 12 (36) |
| Race, No. (%) | ||
| White | 29 (100) | 16 (48) |
| Asian | 0 | 17 (52) |
| Psychoeducational Test Scores at Time of Study | ||
| WRMT Word Identification | ||
| Mean (SD) | 87.55 (15.65) | 122.58 (15.94) |
| Median (range) | 89 (55-112) | 127 (95-145) |
| WRMT Word Attack | ||
| Mean (SD) | 87.55 (9.43) | 111.33 (11.73) |
| Median (range) | 86 (63-112) | 110 (92-134) |
| Test of written spelling | ||
| Mean (SD) | 80.93 (13.44) | 110.91 (14.36) |
| Median (range) | 82 (45-105) | 111 (83-140) |
| WASI-II estimated IQ | ||
| Mean (SD) | 104.97 (12.05) | 117.88 (10.83) |
| Median (range) | 105 (83-133) | 118 (95-138) |
| Psychoeducational Test Scores at Time of Clinical Evaluation | ||
| Elapsed time since evaluation, y | ||
| Mean (SD) | 1.68 (1.17) | NA |
| Median (range) | 1.72 (0.16-4.15) | NA |
| WRMT Word Identificationa | ||
| Mean (SD) | 80.62 (10.68) | NA |
| Median (range) | 81.00 (55-102) | NA |
| WRMT Word Attackb | ||
| Mean (SD) | 83.88 (7.11) | NA |
| Median (range) | 83.50 (70-98) | NA |
Abbreviations: NA, not applicable; WASI-II, Wechsler Abbreviated Scale of Intelligence–second edition; WRMT, Woodcock Reading Mastery Test.
For 29 children.
For 26 children.
Vision Measures
Refractive Error and Eye Alignment
The median cycloplegic refractive error did not differ between the 2 groups (DD group: 0.75 diopters [D] [range, 2.25 to –4.75 D]; TD group: 0.50 D [range, 1.75 to –3.75 D]). The distribution of eye alignment (based on the cover test) did not differ by group for distance or near (eTable 2 in the Supplement).
Vergence
Individual vergence measures, including the near point of convergence test and near fusional convergence ranges, were significantly reduced in the DD group (eTable 3 in Supplement). Furthermore, full criteria for a diagnosis of vergence deficit were met in twice as many children in the DD group (10 [34%]; 7 convergence excess and 3 convergence insufficiency) as in the TD group (5 [15%]; 4 convergence excess and 1 convergence insufficiency). This latter difference did not reach statistical significance (χ2 = 3.15; difference, 19%; 95% CI, –2.2% to 41%; P = .08).
Accommodation
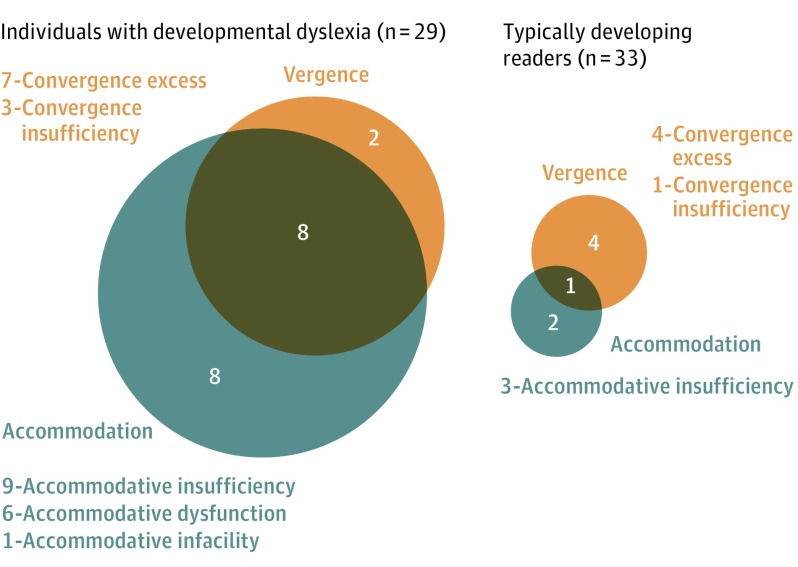
The proportion of children who met the criteria for a diagnosis of accommodation deficiency was higher in the DD group (16 [55%]; 9 accommodative insufficiency, 6 accommodative dysfunction, and 1 accommodative infacility) than in the TD group (3 [9%]; all accommodative insufficiency) (χ2 = 15.42; difference, 46%; 95% CI, 25%-67%; P < .001). An uncorrected refractive error greater than 0.75 D was present in 5 of 9 children in the DD group and 2 of 3 children in the TD group with accommodative insufficiency. The amplitude of accommodation (F = 13.67) and monocular accommodative facility (F = 18.11) also differed by group (P < .001 for both; eTable 4 in the Supplement). Overall, the number of children who had vergence and/or accommodation deficits was substantially higher in the DD group than in the TD group (18 [62%] vs 7 [21%]), as detailed in Figure 1.14
Figure 1. Distribution of Vergence and Accommodation Deficits Between Individuals With Developmental Dyslexia and Typically Developing Readers.
Overlapping circles indicate patients who had both vergence and accommodation deficits. The numerals in the circles indicate number of patients. The specific types of vergence and accommodation deficits are also detailed (χ2 = 15.6; difference, 41%; 95% CI, 18%-69%; P < .001).
Ocular Motor Tracking
DEM Test
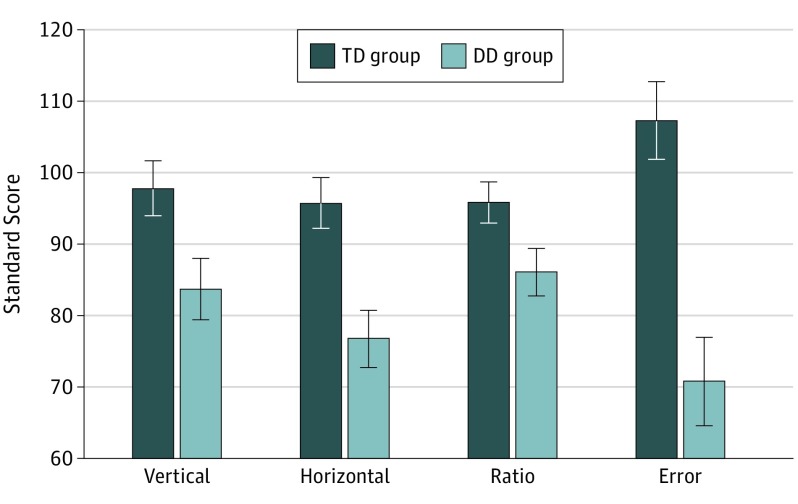
One child with DD was overwhelmed by the DEM task and could not complete it. For the DEM parameters (horizontal and errors), the DD group performed more poorly than the TD group, as seen from results of 2-way ANCOVA (Figure 2). The proportion of children from the DD group obtaining scores in the failing range for the DEM test was elevated for both the error (66%; χ2 = 10.70; P = .001) and horizontal (55%; χ2 = 6.22; P = .01) scores (eFigure 1A and B in the Supplement). Nearly half (13 of 29 [45%]) of the children in the DD group performed in the failing range for both the error and horizontal scores compared with only 1 child in the TD group (3%).
Figure 2. Mean (SE) Developmental Eye Movement Test Scores for the Typically Developing (TD) Readers and Individuals With Developmental Dyslexia (DD).
Vertical, F1,61 = 5.77; P = .02; horizontal, F1,61 = 12.09; P = .001; ratio, F1,61 = 4.72; P = .03; and error, F1,61 = 18.63; P < .001.
Visagraph
Data could not be obtained for 2 children in the DD group (1 child reading below the first grade reading level; the other owing to examiner error). The text was chosen based on the grade equivalent level from the Woodcock Reading Mastery Test Word Identification. For all 33 children in the TD group, the grade equivalent was at or above their current grade placement. Of the 27 children in the DD group, 16 had a grade equivalent at least 1 year below their current grade placement, and 11 had a grade equivalent at their current placement. Data were retained for analysis only if the reading comprehension questions were answered at or above 60% accuracy; all children except 1 in the DD group met this criterion. The mean (SD) reading comprehension was comparable across the groups (DD group below their grade placement, 85% [13.6%]; DD group at their grade placement, 81% [14.5%]; and TD group, 89% [10.1%]).
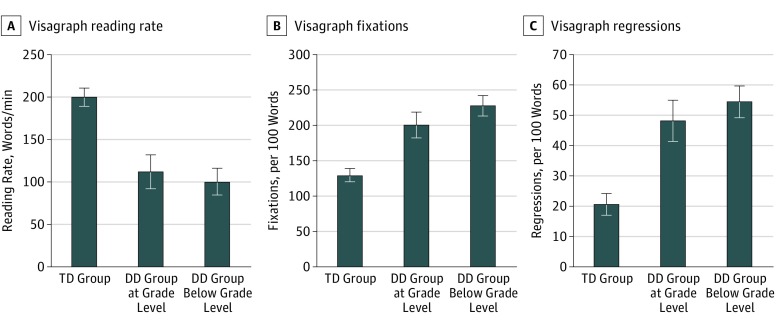
Both DD subgroups performed more poorly than the TD group on all Visagraph parameters but did not differ from each other as seen from the results of 2-way ANCOVA (Figure 3). Nine children in the DD group also completed the task with a text 1 level below their grade equivalent; their reading rate (F = 16.97), fixations (F = 18.40), and regressions (F = 13.65) were still poorer than those of controls (P < .01 with 2-way ANCOVA). As illustrated in eFigure 2A to C in the Supplement, the proportion of individuals with Visagraph impairments was greater in the DD group for reading rate (21 of 26 [81%]), fixations (16 of 26 [62%]), and regressions (15 of 26 [58%]) (reading rate, χ2 = 18.59; fixations, χ2 = 8.38; regressions, χ2 = 8.28; all P < .01). A total of 13 children (50%) in the DD group achieved scores in the impaired range for both fixations and regressions compared with only 5 children (15%) in the TD group. The DEM Horizontal score had a moderate correlation with all 3 Visagraph parameters (r = 0.49-0.51; P < .001; eTable 5 in the Supplement). Overall, 18 children in the DD group (62%) had scores in the impaired range on the DEM and/or Visagraph compared with only 5 children in the TD group (15%) (difference, 47%; 95% CI, 25%-69%; P < .001).
Figure 3. Mean (SE) Visagraph Eye Tracker Parameters in Typically Developing (TD) Readers and Individuals With Developmental Dyslexia (DD).
A, Reading rate, F2,59 = 15.63; P < .001. B, Fixations, F2,59 = 16.12; P < .001. C, Regressions, F2,59 = 14.64; P < .001. In the DD group, 15 children had a reading proficiency at grade level, and 11 children had a reading proficiency below grade level. For all 3 parameters, both DD subgroups performed more poorly than the TD group (P < .001) but not different from each other.
Distribution of Visual Function Deficits Within the DD Group
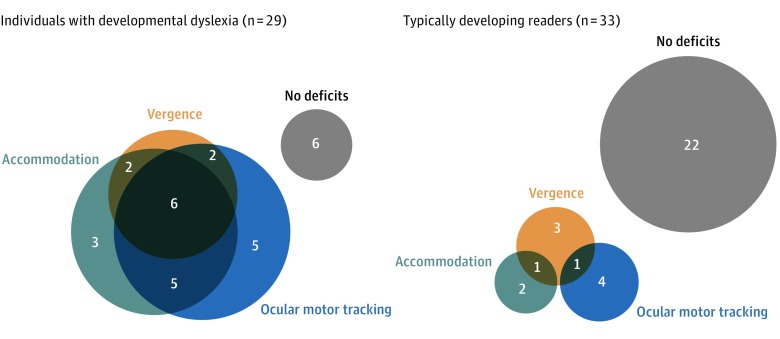
Of the 29 children with DD, 23 (79%) had a deficit in 1 or more domain compared with only 11 (33%) in the TD group. Among the children in the DD group, deficits were observed in more than 1 domain in 15 children (52%) and in 1 domain in 8 children (28%) (Figure 4).14
Figure 4. Distribution of Visual Function Deficits Between Individuals With Developmental Dyslexia (DD) and Typically Developing (TD) Readers.
The numerals in the circles indicate number of patients. The DD group had more deficits (79%) than the TD control group, and the deficits (33%) clustered in subgroups of individuals with DD (χ2 = 13.18; difference, 46%; 95% CI, 23%-69%; P < .001).
Discussion
The goals of this study were to determine whether deficits in peripheral visual function (vergence, accommodation, and ocular motor tracking) are more prevalent in children with DD. Specifically, it addressed which functions were most prominently affected, the frequency and magnitude of abnormal findings, and whether deficits clustered in a subgroup or were more evenly distributed across the DD group.
The prevalence of visual deficits was high among children with DD; 23 (79%) met the criteria for a diagnosis of deficit in 1 or more domains of vergence, accommodation, and/or tracking compared with only 11 children in the TD group (33%). Accommodation and ocular motor tracking were significantly impaired in children in the DD group, as were differences in 3 specific measures of vergence (but not in overall impairment of vergence.) These deficits were not equally distributed across the DD group. A total of 15 of the children in the DD group (52%) had deficits in more than 1 domain, 8 (28%) had deficits in 1 domain, and 6 (21%) did not have deficits.
The potential role of vision deficits in DD has been controversial, and it has been argued that specific vision-related deficits are no more prevalent in individuals with DD than in the general population.3 The lack of a control group in prior clinical studies has also been criticized.15 In the present prospective controlled study, however, we documented a higher prevalence of vision deficits in a well-characterized group of children with DD. Nevertheless, the contribution of these deficits remains uncertain.
Vergence
Although convergence insufficiency has been viewed as a potential problem in children with reading deficits,16,17 the frequency of children who met the criteria for a diagnosis of vergence deficit was unexpectedly similar in our DD and TD groups. Moreover, in both groups, the deficit was much more likely to involve convergence excess than convergence insufficiency, which was infrequent in our sample. Prior studies of vergence in DD have mostly assessed performance on vergence tests rather than documenting a clinical diagnosis; hence, their findings are not directly comparable to ours.18,19,20 Consistent with such studies,18,19,21,22 we did find statistically significant differences on individual vergence tests, including the near point of convergence, positive fusional ranges at near, and vergence facility. Several studies reported a diagnosis of vergence deficit in children who had a generic learning disability but not necessarily dyslexia.22,23 Ygge et al,20 however, did not document diagnoses of vergence deficit even on individual tests for children with dyslexia.
Accommodation
More than half the children in the DD group (16 [55%]) met the criteria for a diagnosis of accommodation deficit compared with only 3 (9%) in the TD group. Approximately two-thirds of these children in the DD group had accommodative insufficiency, and the rest had generalized accommodative dysfunction. At the level of individual tests, the amplitude of accommodation was lower in the DD group than in the TD group, consistent with other studies.18,24 Children in the DD group recorded fewer cycles on the monocular and binocular accommodative facility test, indicating that their accommodation dynamics were slower to react than those of the TD group.
Ocular Motor Tracking
More than half of the children in the DD group (18 [62%]) exhibited ocular motor tracking deficits when reading nonlinguistic stimuli (DEM). They also showed elevated deficits in rate, fixations, and regressions on the Visagraph, even when reading text at their grade-equivalent level with adequate comprehension. Some have questioned whether DEM is a valid measure of saccadic eye movements.25,26 In our study, DEM horizontal gaze parameters had a moderate correlation with Visagraph parameters, supporting its utility as a clinical screener of ocular motor tracking in children.
Visual Function and Reading
Although this study documents a higher frequency of impaired visual function in children with DD, the association with the reading process is uncertain. Clinically, patients with accommodation deficits can report blurry vision at near, words coming in and out of focus, difficulty maintaining clear vision while reading, and difficulty switching focus from distance to near.27,28,29 Although the amplitude of accommodation of the DD group was not within a range expected to cause near-vision work-related blur or asthenopic symptoms, the push-up method we used overestimates amplitude of accommodation.30 Hence, the decrease in accommodation observed in the DD group could have been greater had objective measures been used, within a range that could cause difficulty sustaining clear near vision.30
Accommodative facility has been correlated with reading prowess in children in the first grade,31 and vergence facility correlated significantly with the reading rate among children with learning disabilities,22 but, again, the direction of causation and functional significance is uncertain. The Convergence Insufficiency Treatment Trials showed that eye exercises improved near work-related symptoms in children with reduced accommodation and convergence.8,32 In children with learning disabilities with nonstrabismic binocular vision anomalies, eye exercises improved vergence, accommodation, and tracking, but their effect on reading was not studied.33 Horizontal vergence training improved reading speed and positive fusional vergence in an uncontrolled trial in children with dyslexia and normal binocular vision.24 More evidence is needed to further establish the association between vergence and accommodation deficits and reading metrics.
Tracking has also been associated with reading. Horizontal DEM scores are correlated with the reading rate among children with dyslexia and poor readers.34,35 In addition, beginning readers exhibit more fixations, longer fixation duration, shorter saccades, and more regressions than skilled readers, but these deficits persist in children with dyslexia and are specific to reading.32,33,34,35,36,37 Because eye movements can be influenced by higher-order cognitive and linguistic demands, such visual deficits in children with dyslexia have been understood as effects of the reading deficits rather than as a low-order pure ocular motor deficit that might affect reading. Similarly, deficits in ocular motor skills in children with DD are comparable to those of reading age–matched controls (but inferior to those of typically reading chronological age controls), suggesting an immature ocular motor system in children with DD. Again, whether this result is a cause or an effect of reading impairment is uncertain.36
In our study, children in the DD group read texts corresponding to their single-word reading grade-equivalent level. Although their comprehension was adequate, they still made more fixations and regressions than children in the TD group. These results do not necessarily support a causal role for ocular motor deficits in children with dyslexia; instead, they document the presence of ocular motor deficits even when the children with dyslexia read passages at their reading level. Children with dyslexia with short visual spans had more rightward fixations in reading text but performed similarly to controls on a visual search task; these short visual spans influence ocular motor tracking in dyslexia.37 Such a mechanism could also account for the ocular motor deficits in our DD group, even when reading at their proficiency level.
Strengths and Limitations
The strengths of the study include the prospective, group comparison design and the well-defined group with dyslexia to ensure objective comparisons. The limitations are the relatively small sample size and unmasked examiners. The latter could be mitigated, in part, by the fact that most of the data were collected electronically and not amenable to examiner bias or influence.
Conclusions
This study demonstrates deficits in the visual functioning of children with dyslexia. Although this comparative study does not address any causal association of these deficits with reading performance, the findings support further investigation of visual function in dyslexia. We propose that assessment of vergence, accommodation, and eye movements may be helpful in the initial evaluation of children with dyslexia and will supplement the findings of a comprehensive ophthalmologic examination and a detailed literacy evaluation. The study further provides evidence that supports the design of controlled cohort studies to determine whether treatment of these deficits can bring about changes in visual symptoms and/or reading parameters.
eAppendix. Methods
eTable 1. Vergence and Accommodation Deficit Diagnosis and their Diagnostic Criteria Based on a Battery of Visual Function Assessment
eTable 2. Cover Test Findings at Near
eTable 3. Vergence Clinical Test Results in Developmental Dyslexic and Typical Developing Readers
eTable 4. Accommodation Clinical Test Results in Developmental Dyslexic and Typical Developing Readers
eTable 5. Correlations Between Developmental Eye Movement Parameters and Visagraph Eye Tracker Parameters for all Subjects
eFigure 1. Distribution of Abnormal vs Normal DEM Scores
eFigure 2. Distribution of Abnormal vs Normal Performance on the Visagraph Eye Tracking Parameters
References
- 1.Eunice Kennedy Shriver National Institute of Child Health and Human Development Report of the National Reading Panel: Teaching Children to Read (00-4769). Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 2.Creavin AL, Lingam R, Steer C, Williams C. Ophthalmic abnormalities and reading impairment. Pediatrics. 2015;135(6):1057-1065. doi: 10.1542/peds.2014-3622 [DOI] [PubMed] [Google Scholar]
- 3.Handler SM, Fierson WM. Reading difficulties and the pediatric ophthalmologist. J AAPOS. 2017;21(6):436-442. doi: 10.1016/j.jaapos.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 4.Garzia RP, Nicholson SB. Visual function and reading disability: an optometric viewpoint. J Am Optom Assoc. 1990;61(2):88-97. [PubMed] [Google Scholar]
- 5.Hoffman LG. Incidence of vision difficulties in children with learning disabilities. J Am Optom Assoc. 1980;51(5):447-451. [PubMed] [Google Scholar]
- 6.Rosner J, Rosner J. Comparison of visual characteristics in children with and without learning difficulties. Am J Optom Physiol Opt. 1987;64(7):531-533. doi: 10.1097/00006324-198707000-00008 [DOI] [PubMed] [Google Scholar]
- 7.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 8.Convergence Insufficiency Treatment Trial (CITT) Study Group The Convergence Insufficiency Treatment Trial: design, methods, and baseline data. Ophthalmic Epidemiol. 2008;15(1):24-36. doi: 10.1080/09286580701772037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pediatric Eye Disease Investigator Group Home-based therapy for symptomatic convergence insufficiency in children: a randomized clinical trial. Optom Vis Sci. 2016;93(12):1457-1465. doi: 10.1097/OPX.0000000000000975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheiman M, Mitchell GL, Cotter S, et al. ; Convergence Insufficiency Treatment Trial Study Group . A randomized clinical trial of treatments for convergence insufficiency in children. Arch Ophthalmol. 2005;123(1):14-24. doi: 10.1001/archopht.123.1.14 [DOI] [PubMed] [Google Scholar]
- 11.Scheiman M, Wick B. Clinical Management of Binocular Vision: Heterophoric, Accommodative, and Eye Movement Disorders. 3rd ed Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 12.Brown LD, Cai TT, Dasgupta A. Interval estimation for a binomial proportion. Stat Sci. 2001;16(2):101-117. doi: 10.1214/ss/1009213286 [DOI] [Google Scholar]
- 13.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57(1):289-300. [Google Scholar]
- 14.Hulsen T, de Vlieg J, Alkema W. BioVenn—a web application for the comparison and visualization of biological lists using area-proportional Venn diagrams. BMC Genomics. 2008;9:488. doi: 10.1186/1471-2164-9-488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Academy of Pediatrics, Section on Ophthalmology, Council on Children with Disabilities; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists . Joint statement—learning disabilities, dyslexia, and vision. Pediatrics. 2009;124(2):837-844. doi: 10.1542/peds.2009-1445 [DOI] [PubMed] [Google Scholar]
- 16.Borsting E, Mitchell GL, Kulp MT, et al. ; CITT Study Group . Improvement in academic behaviors after successful treatment of convergence insufficiency. Optom Vis Sci. 2012;89(1):12-18. doi: 10.1097/OPX.0b013e318238ffc3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scheiman M, Mitchell GL, Cotter SA, et al. ; CITT-ART Investigator Group . Convergence Insufficiency Treatment Trial–Attention and Reading Trial (CITT-ART): design and methods. Vis Dev Rehabil. 2015;1(3):214-228. [PMC free article] [PubMed] [Google Scholar]
- 18.Evans BJ, Drasdo N, Richards IL. Investigation of accommodative and binocular function in dyslexia. Ophthalmic Physiol Opt. 1994;14(1):5-19. doi: 10.1111/j.1475-1313.1994.tb00550.x [DOI] [PubMed] [Google Scholar]
- 19.Latvala ML, Korhonen TT, Penttinen M, Laippala P. Ophthalmic findings in dyslexic schoolchildren. Br J Ophthalmol. 1994;78(5):339-343. doi: 10.1136/bjo.78.5.339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ygge J, Lennerstrand G, Rydberg A, Wijecoon S, Pettersson BM. Oculomotor functions in a Swedish population of dyslexic and normally reading children. Acta Ophthalmol (Copenh). 1993;71(1):10-21. doi: 10.1111/j.1755-3768.1993.tb04953.x [DOI] [PubMed] [Google Scholar]
- 21.Kapoula Z, Bucci MP. Postural control in dyslexic and non-dyslexic children. J Neurol. 2007;254(9):1174-1183. doi: 10.1007/s00415-006-0460-0 [DOI] [PubMed] [Google Scholar]
- 22.Quaid P, Simpson T. Association between reading speed, cycloplegic refractive error, and oculomotor function in reading disabled children versus controls. Graefes Arch Clin Exp Ophthalmol. 2013;251(1):169-187. doi: 10.1007/s00417-012-2135-0 [DOI] [PubMed] [Google Scholar]
- 23.Dusek W, Pierscionek BK, McClelland JF. A survey of visual function in an Austrian population of school-age children with reading and writing difficulties. BMC Ophthalmol. 2010;10:16. doi: 10.1186/1471-2415-10-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wahlberg-Ramsay M, Nordström M, Salkic J, Brautaset R. Evaluation of aspects of binocular vision in children with dyslexia. Strabismus. 2012;20(4):139-144. doi: 10.3109/09273972.2012.735335 [DOI] [PubMed] [Google Scholar]
- 25.Ayton LN, Abel LA, Fricke TR, McBrien NA. Developmental eye movement test: what is it really measuring? Optom Vis Sci. 2009;86(6):722-730. doi: 10.1097/OPX.0b013e3181a6a4b3 [DOI] [PubMed] [Google Scholar]
- 26.Webber A, Wood J, Gole G, Brown B. DEM test, Visagraph eye movement recordings, and reading ability in children. Optom Vis Sci. 2011;88(2):295-302. doi: 10.1097/OPX.0b013e31820846c0 [DOI] [PubMed] [Google Scholar]
- 27.Daum KM. Accommodative dysfunction. Doc Ophthalmol. 1983;55(3):177-198. doi: 10.1007/BF00140808 [DOI] [PubMed] [Google Scholar]
- 28.Hennessey D, Iosue RA, Rouse MW. Relation of symptoms to accommodative infacility of school-aged children. Am J Optom Physiol Opt. 1984;61(3):177-183. doi: 10.1097/00006324-198403000-00005 [DOI] [PubMed] [Google Scholar]
- 29.Levine S, Ciuffreda KJ, Selenow A, Flax N. Clinical assessment of accommodative facility in symptomatic and asymptomatic individuals. J Am Optom Assoc. 1985;56(4):286-290. [PubMed] [Google Scholar]
- 30.Anderson HA, Stuebing KK. Subjective versus objective accommodative amplitude: preschool to presbyopia. Optom Vis Sci. 2014;91(11):1290-1301. doi: 10.1097/OPX.0000000000000402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kulp MT, Schmidt PP. Visual predictors of reading performance in kindergarten and first grade children. Optom Vis Sci. 1996;73(4):255-262. doi: 10.1097/00006324-199604000-00007 [DOI] [PubMed] [Google Scholar]
- 32.Convergence Insufficiency Treatment Trial Study Group Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Arch Ophthalmol. 2008;126(10):1336-1349. doi: 10.1001/archopht.126.10.1336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hussaindeen JR, Shah P, Ramani KK, Ramanujan L. Efficacy of vision therapy in children with learning disability and associated binocular vision anomalies. J Optom. 2018;11(1):40-48. doi: 10.1016/j.optom.2017.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palomo-Alvarez C, Puell MC. Relationship between oculomotor scanning determined by the DEM test and a contextual reading test in schoolchildren with reading difficulties. Graefes Arch Clin Exp Ophthalmol. 2009;247(9):1243-1249. doi: 10.1007/s00417-009-1076-8 [DOI] [PubMed] [Google Scholar]
- 35.Northway N. Predicting the continued use of overlays in school children—a comparison of the Developmental Eye Movement test and the Rate of Reading test. Ophthalmic Physiol Opt. 2003;23(5):457-464. doi: 10.1046/j.1475-1313.2003.00144.x [DOI] [PubMed] [Google Scholar]
- 36.Bucci MP, Nassibi N, Gerard CL, Bui-Quoc E, Seassau M. Immaturity of the oculomotor saccade and vergence interaction in dyslexic children: evidence from a reading and visual search study. PLoS One. 2012;7(3):e33458. doi: 10.1371/journal.pone.0033458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prado C, Dubois M, Valdois S. The eye movements of dyslexic children during reading and visual search: impact of the visual attention span. Vision Res. 2007;47(19):2521-2530. doi: 10.1016/j.visres.2007.06.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Methods
eTable 1. Vergence and Accommodation Deficit Diagnosis and their Diagnostic Criteria Based on a Battery of Visual Function Assessment
eTable 2. Cover Test Findings at Near
eTable 3. Vergence Clinical Test Results in Developmental Dyslexic and Typical Developing Readers
eTable 4. Accommodation Clinical Test Results in Developmental Dyslexic and Typical Developing Readers
eTable 5. Correlations Between Developmental Eye Movement Parameters and Visagraph Eye Tracker Parameters for all Subjects
eFigure 1. Distribution of Abnormal vs Normal DEM Scores
eFigure 2. Distribution of Abnormal vs Normal Performance on the Visagraph Eye Tracking Parameters