Abstract
To address the opioid overdose epidemic in the United States, states have implemented policies to reduce inappropriate opioid prescribing. These policies could affect the coincident heroin overdose epidemic by either driving the substitution of heroin for opioids or reducing simultaneous use of both substances. We used IMS Health’s National Prescription Audit and government mortality data to examine the effect of these policies on opioid prescribing and on prescription opioid and heroin overdose death rates in the United States during 2006–13. The analysis revealed that combined implementation of mandated provider review of state-run prescription drug monitoring program data and pain clinic laws reduced opioid amounts prescribed by 8 percent and prescription opioid overdose death rates by 12 percent. We also observed relatively large but statistically insignificant reductions in heroin overdose death rates after implementation of these policies. This combination of policies was effective, but broader approaches to address these coincident epidemics are needed.
In 2014, overdose deaths related to prescription opioids and heroin claimed the lives of more than 28,000 people in the United States, accounting for the majority of total drug poisoning deaths.1 Prescription opioid–related overdose deaths increased dramatically after 1999, nearly quadrupling over the next decade.2 These overdose deaths paralleled a quadrupling of the amount of opioids prescribed,3 as professional pain management societies called for and state regulations encouraged more liberal use of opioids for chronic, noncancer pain.4 Heroin overdose deaths also increased, more than tripling between 2010 and 2014.1
In response, many states have enacted policies to control inappropriate opioid prescribing and thereby reduce overdose deaths. A growing body of recent scientific evidence suggests that state-level policies—such as mandatory provider use of prescription drug monitoring programs (PDMPs)—might reduce prescribing practices that increase overdose risk.5 These programs consist of state-based electronic databases that collect data on controlled prescription drugs dispensed by pharmacies and, in some states, by dispensing physicians. They contain information about patients’ controlled substance prescription history that can help providers identify risk factors for opioid-related fatal overdose, such as receipt of opioids from multiple sources and total prescribed opioid dosage.6 However, in states without policies requiring review of PDMP data, providers use the data infrequently.7 Al though laws mandating provider review of these data do not guarantee that all prescribers will comply, dramatic increases in providers’ use of them have been demonstrated following implementation of these laws. For example, in Kentucky, where mandated PDMP use was implemented in July 2012, the number of provider requests for patients’ prescription history reports increased from 811,000 in 2011 to nearly4.6 million in 2013.5
In some states, certain pain clinics have provided opioids and other controlled prescriptions to patients in large quantities and without medical evaluation or justification. Pain clinic laws attempt to decrease inappropriate prescribing through requirements such as registration of pain clinics with the state, physician ownership of the clinics, prescribing restrictions, and record-keeping requirements.
It is possible that mandated use of PDMP data and pain clinic laws reduce the frequency with which opioids are prescribed or, more specifically, reduce dosages or amounts of opioids prescribed to individuals at risk for overdose and, in turn, reduce overdose deaths. At the same time, publications in mainstream media8–10 and in the scientific literature11,12 have advanced the idea that opioid prescribing policies have unintentionally driven demand for heroin (a drug with similar effects) as people search for “a cheaper, more accessible high.”10
To implement effective prevention strategies, many of which are implemented at the state level, it is important to understand whether and how opioid prescribing policies affect prescribing and overdose deaths. To this end, we examined whether opioid prescribing policies had the intended positive impact on prescribing and prescription drug overdose deaths and whether they unintentionally created harms by increasing heroin overdose deaths.
Study Data And Methods
We performed a difference-in-differences analysis of state-level data with intervention and comparison states, a method widely used to identify the impact of policies.13,14 We used eight-year (2006–13) state-level panel data for states that implemented opioid prescribing policies and comparison states that did not implement these policies during this time period.
STATE-LEVEL OPIOID PRESCRIBING POLICIES
Theories that opioid prescribing policies reduce prescription opioid–related deaths or inadvertently increase heroin demand and overdose deaths rely on reduced prescription opioid access as an explanatory mechanism. Thus, we focused on state-level policies that could affect opioid prescribing and supply. These policies are laws and regulations requiring providers to follow opioid prescribing guidelines,15 pain clinic laws (which govern the ownership, operation, and practices of clinics providing pain management services where practitioners prescribe opioids or other controlled substances to a large proportion of patients),16 and mandated provider review of information from prescription drug monitoring programs before prescribing opioids. We excluded Good Samaritan laws, which are policies intended to increase access to naloxone for opioid overdose reversal, and drug take-back programs because they are not known to affect opioids available for abuse and diversion.17 We reviewed multiple sources for information on state-level opioid-related laws and regulations and timing of implementation from Westlaw, reports from the National Alliance for Model State Drug Laws,18 and reports from the PDMP Center of Excellence at Brandeis University.5
DRUG OVERDOSE DEATHS
We used National Vital Statistics System Multiple Cause of Death mortality files from the National Center for Health Statistics, Centers for Disease Control and Prevention, to obtain the number of heroinand prescription opioid–related overdose deaths, overdose deaths related to unspecified narcotics, overdose deaths related to unspecified drugs, and “pending” deaths (for which the cause or manner of death could not be determined by the close of the time for filing) for each state during the period 2006–13.19 See additional details in the online Appendix.20
OPIOID PRESCRIBING
We used IMS Health’s National Prescription Audit to obtain information on prescribed opioids dispensed between 2006 and 2013. The National Prescription Audit provided estimates of prescriptions for each state based on a representative sample of approximately 57,000 retail pharmacies that dispense nearly 80 percent of all prescriptions in the United States, including opioids paid by commercial insurance, Medicaid, Medicare, and cash.21
State-specific annual opioid prescribing rates were calculated as milligrams prescribed in morphine milligram equivalents (MMEs) per state resident per year. Additional details about this calculation appear in the Appendix.20
STATES IMPLEMENTING POLICIES AND COMPARISON STATES
We included thirty-eight states and the District of Columbia in the final analysis. States were excluded because of concerns about the reliability of death rates based on very low numbers of heroin deaths (ten states)22 or marked reduction in reporting drug-specific overdose deaths to the National Center for Health Statistics during the period (New Mexico). We excluded Washington State because of its unique mandate to follow prescribing guidelines; this would have introduced complexity in identifying controls and calculating inferences statistics in difference-in-differences analyses.23
Of the thirty-eight states in our analysis, seven states implemented pain clinic laws between 2006 and 2013 (see Appendix Exhibit A1).20 Of these seven, four mandated provider review of PDMP data at or about the same time as their pain clinic laws took effect.
STATISTICAL ANALYSIS
We modeled the effect of mandatory provider review of PDMP data and pain clinic laws on state-level MMEs per population and on heroin, prescription opioid, and combined drug overdose death rates using a two-way fixed effects approach. The two-way fixed effects model includes both state and year fixed effects and is a generalized approach to difference-in-differences modeling.24 These models included relevant time varying covariates, which are described in detail below.
Two categories of intervention states—those implementing both mandated provider review of PDMP data and pain clinic laws and those implementing pain clinic laws alone—were modeled separately. Because every state implementing mandated provider review of PDMP data implemented pain clinic laws at a similar point in time, we were unable to model the effects of mandated provider review of PDMP data alone. The start of the policy period was defined as the year in which the policy was implemented, if within the first half of a calendar year, or as the year following policy implementation, if implemented during the second half of a calendar year. We controlled for state-level time-varying factors that might affect heroin and prescription opioid overdose deaths, including opioid prescribing rates, pending death rates, and totals of unspecified narcotic and unspecified drug overdose death rates. We included state-specific linear time trends to account for unobserved state-level factors that evolve over time.
In addition, states experiencing increased overdose rates may have taken steps to expand access to medication-assisted treatment with opioid agonists for opioid use disorder, which could reduce opioid overdose rates. Therefore, we conducted a sensitivity analysis including estimates for state-level per population buprenorphine treatment capacity. See additional details in the Appendix.20
We conducted all analyses using Stata/SE software, version 13.1.
LIMITATIONS
Our findings were subject to several limitations. First, we did not examine state laws or regulations requiring providers to follow opioid prescribing guidelines because we found only one state implementing such rules.
Second, some authors have posited an association between the reformulation of OxyContin to include tamper-resistant features and increases in heroin use.25 However, it is difficult to assess the independent effect of this change given that the reformulation of OxyContin affected all states at the same time (late 2010). Given that this change was a common effect to all states in the analysis, it did not bias our difference-in-differences estimates of the other policy impacts.
Third, the IMS Health data do not adequately capture opioids dispensed directly by providers, including those in pain clinics, so findings regarding the effect of pain clinic laws on opioid prescribing should be interpreted with particular caution. However, this limitation would not affect our ability to detect a difference in the more distal outcome of overdose deaths in states implementing pain clinic laws.
Fourth, estimates of buprenorphine treatment capacity might underrepresent the overall capacity for medication-assisted treatment with opioid agonists because methadone is not included. However, potential methadone capacity based on number of operating opioid treatment programs remained relatively stable during the study period compared with substantial changes in potential buprenorphine treatment capacity.26
Fifth, because most opioid-related policy interventions were implemented relatively recently, we were able to include only limited postintervention time, which could have reduced our ability to identify long-term intended and unintended effects of these polices. For example, reducing exposure to prescription opioids could reduce subsequent heroin use at a later point, but there was insufficient postintervention time in our analysis to observe this effect.
Sixth, the absence of an overall association between opioid prescribing policies and mean heroin overdose rates does not rule out the possibility that some people used heroin because of decreased availability of opioids after opioid prescribing policies took effect.
Several factors might have affected prescription opioid and heroin overdose death reporting in states over time. A substantial proportion of drug overdose death reports do not include the specific drug or drugs involved in the overdose (25 percent in 2008–10),27 and this proportion varies widely by state. Unknown factors, such as funding available for drug overdose surveillance, might also have affected drug-specific reporting. To some extent, these factors were controlled for in our analysis using state fixed effects and statespecific time trends and by including unspecified drug overdose deaths and pending investigation deaths in the models.
Eleven states were excluded because of limitations in available drug overdose data. It is difficult to speculate how the results would have differed if we had included all states. Policy effects would be muted in at least ten of these states with relatively small numbers of deaths. The effect of including New Mexico is unclear, since it was excluded because of inconsistency in measurement of the key outcomes over time.
It is possible that variation in drug-specific reporting was related to implementation of opioid prescribing policies. Specifically, increased concern about overdose deaths in some states might have led to both policy development and to increased vigilance in identifying heroin and prescription opioid overdose deaths through surveillance. This could lead to artificial increases in heroin-related, prescription opioid–related, and combined drug overdose death rates associated with prescription opioid policies, which would bias findings of decreased overdose deaths associated with policies toward the null.
Study Results
TRENDS IN OPIOID PRESCRIBING
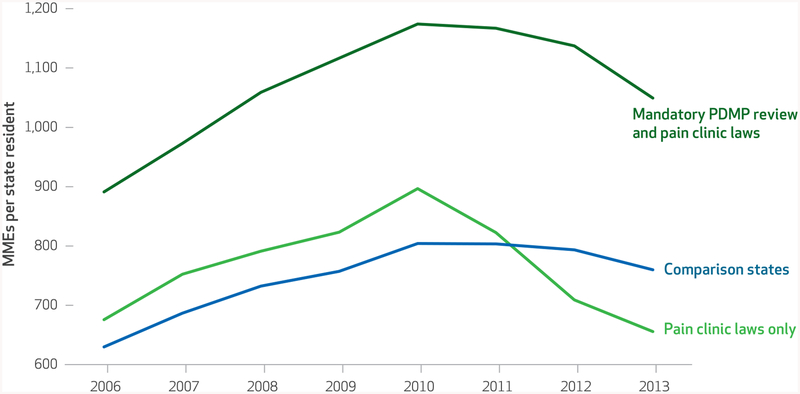
Overall, opioid prescribing rates paralleled opioid overdose death rates during 2006–13. On average across all states, prescribing rates per state resident increased from 660 MMEs in 2006 to 849 MMEs in 2010 (a 28.5 percent increase) and decreased after 2010 (data not shown). The prescribing rate declined to 781 MMEs in 2013, an 8 percent decrease compared to 2010 (data not shown). Throughout the study period, prescribing rates were highest among states that ultimately implemented both mandatory prescription drug management program review and pain clinic laws (Exhibit 1). Prescribing rates declined more sharply from 2010 to 2013 in states implementing both policies (10.6 percent decrease) and in those implementing pain clinic laws only (26.9 percent decrease) than in states not implementing either policy (5.5 percent decrease).
Exhibit 1.
Opioid prescribing rates by state policy category SOURCES IMS Health’s National Prescription Audit, 2006–13; state populations obtained from CDC WONDER (Wide-ranging Online Data for Epidemiologic Research), 2006–13. NOTES MME is morphine milligram equivalent. PDMP is prescription drug monitoring program.
TRENDS FOR OPIOID, HEROIN, AND COMBINED DRUG OVERDOSE DEATHS
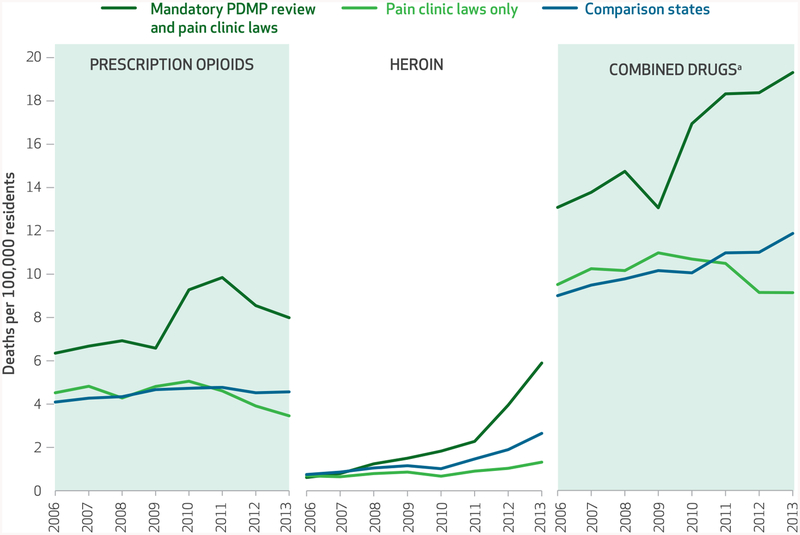
Overall prescription opioid overdose death rates increased beginning in 2006 and reached a peak in 2011 at 5.40 per 100,000 residents. These rates decreased for the first time in 2012 to 5.05 per 100,000 and stayed at about that level with a rate of 5.09 per 100,000 in 2013 (data not shown). Prescription opioid overdose death rates were substantially higher in states that ultimately implemented both pain clinic laws and mandatory PDMP review than in comparison states or in states implementing pain clinic laws only (Exhibit 2). Prescription opioid–related overdose death rates decreased more sharply in both categories of intervention states than in comparison states.
Exhibit 2.
Drug overdose death rates by state policy category SOURCES National Vital Statistics System Multiple Cause of Death mortality files, 2006–13, from the National Center for Health Statistics; state populations obtained from CDC WONDER (Wide-ranging Online Data for Epidemiologic Research), 2006–13. NOTE PDMP is prescription drug monitoring program. aCombined drugs include prescription opioids, heroin, and unspecified drugs.
Heroin overdose death rates increased among all states during 2006–13 (from 0.72 to 2.69 per 100,000 residents). In 2006, heroin overdose death rates were similar in states that did and did not implement opioid prescribing policies. Death rates increased in all categories of states beginning in 2008. Compared with states not implementing either type of prescription opioid policy, heroin overdose death rates increased less sharply in states that ultimately implemented pain clinic laws only and more sharply in states that ultimately implemented both mandatory PDMP review and pain clinic laws (Exhibit 2).
Combined drug overdose death rates predominantly reflected trends in opioid-related overdose death rates (Exhibit 2).
EFFECTS OF POLICIES ON OPIOID PRESCRIBING AND OPIOID-RELATED OVERDOSE DEATH RATES
The implementation of combined policies mandating PDMP use and pain clinic laws reduced the prescribing rates by 80.1 MMEs per state resident. Implementation of pain clinic laws alone did not significantly reduce opioid prescribing rates (Exhibit 3). Among states implementing both mandatory PDMP use and pain clinic laws, policy implementation was significantly associated with a reduction in the prescription opioid overdose death rate of 1.2 per 100,000 residents. Pain clinic laws alone did not have a significant effect on these rates, but there was a significant positive association between opioid MME prescribing rates and opioid overdose death rates (Exhibit 3).
Exhibit 3.
Estimated impact of opioid prescribing policies on state-level drug overdose death rates, 2006–13
| Outcome 1: opioid MME prescribing ratea | Outcome 2: prescription opioid overdose deaths | Outcome 3: heroin overdose deaths | Outcome 4: combined drug overdose deaths | |
|---|---|---|---|---|
| Mandatory PDMP review and pain clinic laws | −80.1** | −1.198** | −0.215 | −1.103** |
| Pain clinic laws only | −54.7 | −0.174 | −0.356 | −0.419 |
| Opioid MME prescribing ratea | —d | 0.006*** | −0.001 | 0.008*** |
| Pending death investigation rateb | —d | −0.145*** | −0.026 | −0.288*** |
| Prescription opioid death rateb | 8.0 | —d | 0.058 | —d |
| Lagged prescription opioid death rateb | 5.84 | —d | —d | —d |
| Unspecified deaths rateb,c | —d | −0.002 | −0.002 | —d |
SOURCES Authors’ analysis of data from IMS Health’s National Prescription Audit, 2006–13, and the National Vital Statistics System’s Multiple Cause of Death mortality files, 2006–13.
NOTES Marginal effects are reported. Robust standard errors clustered at the state level. MME is morphine milligram equivalent. PDMP is prescription drug monitoring program.
MMEs prescribed per state resident per year.
Deaths per 100,000 state residents.
Unspecified deaths are the totals of unspecified narcotics-related overdose deaths and unspecified drug-related overdose deaths.
The variable specified for the row was not used in modeling the outcome specified for the column.
p < 0:05
p < 0:01
EFFECTS OF POLICIES ON HEROIN OVERDOSE DEATH RATES
Neither combined PDMP and pain clinic laws nor pain clinic laws alone were associated with statistically significant reductions in heroin death rates. Opioid prescribing rates were also not significantly associated with heroin overdose death rates (Exhibit 3).
EFFECT ON COMBINED DRUG OVERDOSE DEATH RATES
Among states implementing both mandatory PDMP use and pain clinic laws, policy implementation was significantly associated with a reduction in the combined drug overdose death rate of −1.1 per 100,000 residents. There were also significant positive associations between MME prescribing rates and combined drug overdose death rates (Exhibit 3).
SENSITIVITY ANALYSIS: EFFECTS OF BUPRENORPHINE TREATMENT CAPACITY
Estimated buprenorphine treatment capacity per 10,000 population increased during the study period, with greater increases in states implementing mandatory PDMP review and pain clinic laws (from 0.81 to 10.18) than in states implementing pain clinic laws alone (from 1.26 to 5.25) or comparison states (from 1.74 to 6.06).20 However, the addition of estimated buprenorphine treatment capacity to the models did not result in significant changes in effects of opioid prescribing policies on overdose death rates. See additional details in the Appendix.20
Discussion
Our results suggest that some opioid prescribing policies had intended effects on opioid prescribing and overdose death rates. We found that mandated review of prescription drug monitoring program data combined with pain clinic laws was significantly associated with both decreased amounts of opioids prescribed and with decreased prescription opioid overdose deaths. However, mandated PDMP review was adopted only in states that also adopted pain clinic laws at or around the same time. Thus, it is not possible to clearly determine whether the combined implementation of the policies or mandated PDMP review drove the observed changes, although pain clinic laws alone appear to have a smaller, if any, effect on overdose deaths. Previous analyses have found that mandated PDMP review was associated with modest reductions in opioid prescriptions and more substantial decreases in opioids prescribed to patients receiving opioids from multiple prescribers.5
We found no evidence to support the assertion that policies to curb opioid prescribing are leading to heroin overdoses. Heroin overdose death rates increased during 2006–13 in states with and without prescription opioid policies, and they increased at a faster rate in states ultimately implementing both pain clinic laws and mandatory PDMP checks than in comparison states or in states implementing pain clinic laws alone. However, greater increases in heroin deaths in these states were evident by 2009, before the policies intended to reduce opioid prescribing took effect. If anything, the timing of the trends suggests that states implementing stronger combinations of opioid prescribing policies could have been doing so to address overdose deaths. When we analyzed these trends more rigorously in a regression framework, the estimated effects of pain clinic laws and combined polices were not statistically significant. In fact, these estimates suggest that the policies might actually reduce heroin overdose deaths.
Prior prescription opioid misuse is an important risk factor for heroin use.28–31 Opioid prescribing is associated with opioid use and misuse, which are in turn associated with prescription opioid overdose and with heroin use and overdose. Thus, our results that showed a reduction in MMEs prescribed support the statistically insignificant association between these policies and reduced heroin overdose death rates.
Policy Implications
Mandated PDMP use and pain clinic laws may prevent opioid overdose deaths by reducing opioid use and abuse among people who have not previously used opioids. These policies may also reduce access to harmful amounts of prescribed opioids among patients at risk for overdose. In addition, these policies may reduce the number of people initiating heroin use in the longer term by reducing the number of people exposed to opioids both for use as prescribed and for nonmedical use. Our findings suggest that even though the existence of a PDMP might not prevent prescription opioid-related overdose deaths,32 providers’ routine use of PDMP data associated with mandated review could prevent prescription opioid–related overdose deaths. In addition, pain clinic laws could be effective in preventing prescription opioid–related overdose deaths, particularly in combination with mandated PDMP review and in jurisdictions where substantial proportions of opioids dispensed are prescribed in pain clinics. For example, in Florida, where it was reported that 98 of the 100 physicians dispensing the nation’s highest quantities of oxycodone from their offices practiced in 2010, deaths related to oxycodone were estimated to have decreased by 52 percent from 2010 to 2012 following the implementation of pain clinic laws.16
Consistent with a previously published analysis of data in one state,33 we did not find any evidence to support the concern that these opioid prescribing policies result in increased heroin-related overdose deaths. However, additional factors, including increased heroin supply, a population already widely exposed to prescription opioids, and increased mixing of highly potent illicitly manufactured fentanyl with heroin,34 are likely to continue to pose daunting challenges to the prevention of heroin overdose deaths. Along with the primary prevention approaches examined in this article, coordinated secondary and tertiary prevention approaches will likely be required to prevent overdose among people already dependent on prescription opioids or heroin. These might include making naloxone more available for overdose prevention,35 identifying people who are dependent on opioids or heroin, making effective opioid use disorder treatment services more widely available,36 and motivating individuals to seek effective treatment for opioid use disorder.37
Conclusion
Despite the potential link, our findings do not support the hypothesis that policies related to opioid prescribing were associated with increased heroin deaths during 2006–13. They suggest that other factors might be at play, potentially including widespread population exposure to prescription opioids as a result of increased opioid prescribing since 1999,3 and increased heroin supply, affordability, and purity since 2010.38,39 It is encouraging that policies intended to reduce inappropriate prescribing of opioids appear to be associated with reductions in opioid-related overdose deaths. ▪
Preliminary findings were presented at the National Rx Drug Abuse and Heroin Summit, in Atlanta, Georgia, March 30, 2016. The authors thank Noah Aleshire for assistance in identifying state legislation and Aleta Christensen for editorial assistance. The conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Supplementary Material
Footnotes
We found no evidence to support the assertion that policies to curb opioid prescribing are leading to heroin overdoses.
Contributor Information
Deborah Dowell, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (CDC), in Atlanta, Georgia..
Kun Zhang, National Center for Injury Prevention and Control, CDC..
Rita K. Noonan, Health Systems and Trauma Systems Branch of the National Center for Injury Prevention and Control, CDC..
Jason M. Hockenberry, Department of Health Policy and Management at Emory University, in Atlanta..
NOTES
- 1.Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64(50–51): 1378–82. [DOI] [PubMed] [Google Scholar]
- 2.Warner M, Hedegaard H, Chen L-H. Trends in drug-poisoning deaths involving opioid analgesics and heroin: United States, 1999–2012 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2014. December [cited 2016 Aug 9]. Available from: http://www.cdc.gov/nchs/data/hestat/drug_poisoning/drug_poisoning_deaths_1999-2012.pdf [Google Scholar]
- 3.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60(43): 1487–92. [PubMed] [Google Scholar]
- 4.Von Korff MR, Franklin G. Responding to America’s iatrogenic epidemic of prescription opioid addiction and overdose. Med Care. 2016;54(5):426–9. [DOI] [PubMed] [Google Scholar]
- 5.Prescription Drug Monitoring Program Center of Excellence at Brandeis. Mandating PDMP participation by medical providers: current status and experience in selected states [Internet]. Waltham (MA): The Center; 2014. Oct [cited 2016 Aug 9]. Available from: http://www.pdmpexcellence.org/sites/all/pdfs/COE_briefing_mandates_2nd_rev.pdf [Google Scholar]
- 6.Gwira Baumblatt JA, Wiedeman C, Dunn JR, Schaffner W, Paulozzi LJ, Jones TF. High-risk use by patients prescribed opioids for pain and its role in overdose deaths. JAMA Intern Med. 2014;174(5):796–801. [DOI] [PubMed] [Google Scholar]
- 7.Feldman L, Williams KS, Coates J, Knox M. Awareness and utilization of a prescription monitoring program among physicians. J Pain Palliat Care Pharmacother. 2011; 25(4):313–7. [DOI] [PubMed] [Google Scholar]
- 8.Gupta S Unintended consequences: why painkiller addicts turn to heroin. CNN [serial on the Internet]. 2015. Jan 3 [updated 2016 Jun 2; cited 2016 Aug 9]. Available from: http://www.cnn.com/2014/08/29/health/gupta-unintended-consequences/
- 9.Koebler J Study: heroin abuse increase may be due to prescription painkiller crackdown. U.S. News and World Report [serial on the Internet]. 2013. June 12 [cited 2016 Aug 9]. Available from: http://www.usnews.com/news/articles/2013/06/12/study-heroin-abuse-increase-may-be-due-to-prescription-painkiller-crackdown [Google Scholar]
- 10.Khazan O The new heroin epidemic. Atlantic [serial on the Internet]. 2014. October 30 [cited 2016 Aug 9]. Available from: http://www.theatlantic.com/health/archive/2014/10/the-new-heroin-epidemic/382020/ [Google Scholar]
- 11.Huecker MR, Shoff HW. The law of unintended consequences: illicit for licit narcotic substitution. West J Emerg Med. 2014;15(4):561–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rigg KK, Monnat SM. Comparing characteristics of prescription painkiller misusers and heroin users in the United States. Addict Behav. 2015;51:106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buckley J, Shang Y. Estimating policy and program effects with observational data: the “differences-in-differences” estimator. Pract Assess Res Eval. 2003;8(24). [Google Scholar]
- 14.French B, Heagerty PJ. Analysis of longitudinal data to evaluate a policy change. Stat Med. 2008;27(24): 5005–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franklin G, Sabel J, Jones CM, Mai J, Baumgartner C, Banta-Green CJ, et al. A comprehensive approach to address the prescription opioid epidemic in Washington State: milestones and lessons learned. Am J Public Health. 2015;105(3):463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson H, Paulozzi L, Porucznik C, Mack K, Herter B. Decline in drug overdose deaths after state policy change—Florida, 2010–2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):569–74. [PMC free article] [PubMed] [Google Scholar]
- 17.Gray JA, Hagemeier NE. Prescription drug abuse and DEA-sanctioned drug take-back events: characteristics and outcomes in rural Appalachia. Arch Intern Med. 2012; 172(15):1186–7. [DOI] [PubMed] [Google Scholar]
- 18.National Alliance for Model State Drug Laws. Prescription drug abuse, addiction and diversion: overview of state legislative and policy initiatives, a three part series, part 2: state regulation of pain clinics and legislative trends relative to regulating pain clinics [Internet]. Santa Fe (NM): NAMSDL; 2014. [cited 2016 Aug 9]. Available from: http://www.namsdl.org/NAMSDL%20Part%202%20Revised%20April%204%202014.pdf
- 19.Centers for Disease Control and Prevention. CDC WONDER: Multiple Cause of Death data, 2006–2013 [Internet]. Atlanta (GA): CDC; 2015. [cited 2016 Aug 9]. Available from: http://wonder.cdc.gov/mcd.html [Google Scholar]
- 20.To access the Appendix, click on the Appendix link in the box to the right of the article online. [Google Scholar]
- 21.IMS Health. National Prescription Audit [Internet]. Collegeville (PA): IMS Health; [cited 2016 Aug 9]. (HSRN Data Brief). Available from: https://www.imshealth.com/files/web/IMSH%20Institute/NPA_Data_Brief-.pdf
- 22.National Center for Health Statistics. Compressed mortality file, 1999–2011 [Internet]. Hyattsville (MD): NCHS; 2014. Jul 28 [cited 2016 Aug 9]. Available from:http://ww.cdc.gov/nchs/data/mortab/1999-2011CMFDocumentation_8_5_14.pdf
- 23.Angrist JD, Pischke J-S. Mostly harmless econometrics: an empiricist’s companion. Princeton(NJ): Princeton University Press; 2008. [Google Scholar]
- 24.Wooldridge JM. Econometric analysis of cross section and panel data. Second edition Cambridge (MA): MIT Press; 2010. October. [Google Scholar]
- 25.Cicero TJ, Ellis MS, Surratt HL. Effect of abuse-deterrent formulation of OxyContin. N Engl J Med. 2012; 367(2):187–9. [DOI] [PubMed] [Google Scholar]
- 26.Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication–assisted treatment. Am J Public Health. 2015;105(8):e55–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS. State variation in certifying manner of death and drugs involved in drug intoxication deaths. Acad Forensic Pathol. 2013; 3(2):231–7. [Google Scholar]
- 28.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132(1–2):95–100. [DOI] [PubMed] [Google Scholar]
- 29.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7): 821–6. [DOI] [PubMed] [Google Scholar]
- 30.Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2013. August [cited 2016 Aug 9]. Available from: http://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm [Google Scholar]
- 31.Cicero TJ, Ellis MS, Harney J. Shifting patterns of prescription opioid and heroin abuse in the United States. N Engl J Med. 2015;373(18):1789–90. [DOI] [PubMed] [Google Scholar]
- 32.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med. 2011;12(5): 747–54. [DOI] [PubMed] [Google Scholar]
- 33.Kennedy-Hendricks A, Richey M, McGinty EE, Stuart EA, Barry CL, Webster DW. Opioid overdose deaths and florida’s crackdown on pill mills. Am J Public Health. 2016; 106(2):291–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Increases in fentanyl drug confiscations and fentanylrelated overdose fatalities [Internet]. Atlanta (GA): CDC; 2015. Oct 26 [cited 2016 Aug 9]. Available from: http://emergency.cdc.gov/han/han00384.asp [Google Scholar]
- 35.Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen Alaward A, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–6. [DOI] [PubMed] [Google Scholar]
- 37.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–61. [DOI] [PubMed] [Google Scholar]
- 38.Drug Enforcement Administration. National drug threat assessment summary 2014 [Internet]. Washington (DC): Department of Justice, Drug Enforcement Administration; 2014. Nov [cited 2016 Aug 9]. Available from: https://www.dea.gov/resource-center/dir-ndta-unclass.pdf [Google Scholar]
- 39.Office of National Drug Control Policy. National Drug Control Strategy: data supplement 2014 [Internet]. Washington (DC): Executive Office of the President of the United States, Office of National Drug Control Policy; 2014. [cited 2016 Aug 9]. Available from: https://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/ndcs_data_supplement_2014.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.