Key Points
Question
How effective are point-of-care audio instructions, visual instructions, and in-person training at enabling laypeople to control hemorrhage using a tourniquet, and will they retain this skill?
Findings
In this randomized clinical trial, 465 participants were randomized to 4 arms to evaluate tourniquet application, and 303 (65.25) were assessed for retention 3 to 9 months after completing their training. Bleeding control training (88% correct application) was superior to control (16%) while flashcards (20%) and audio kits (23%) were not, and 3 to 9 months after training, 256 (55%) correctly applied a tourniquet.
Meaning
In-person training is currently the most efficacious means of enabling bystanders to control hemorrhage; however, investigating refresher training or improved point-of-care instructions is critical.
Abstract
Importance
Several national initiatives have emerged to empower laypersons to act as immediate responders to reduce preventable deaths from uncontrolled bleeding. Point-of-care instructional interventions have been developed in response to the scalability challenges associated with in-person training. However, to our knowledge, their effectiveness for hemorrhage control has not been established.
Objective
To evaluate the effectiveness of different instructional point-of-care interventions and in-person training for hemorrhage control compared with no intervention and assess skill retention 3 to 9 months after hemorrhage control training.
Design, Setting, and Participants
This randomized clinical trial of 465 laypersons was conducted at a professional sports stadium in Massachusetts with capacity for 66 000 people and assessed correct tourniquet application by using different point-of-care interventions (audio kits and flashcards) and a Bleeding Control Basic (B-Con) course. Non-B-Con arms received B-Con training after initial testing (conducted from April 2017 to August 2017). Retesting for 303 participants (65%) was performed 3 to 9 months after training (October 2017 to January 2018) to evaluate B-Con retention. A logistic regression for demographic associations was performed for retention testing.
Interventions
Participants were randomized into 4 arms: instructional flashcards, audio kits with embedded flashcards, B-Con, and control. All participants received B-Con training to later assess retention.
Main Outcomes and Measures
Correct tourniquet application in a simulated scenario.
Results
Of the 465 participants, 189 (40.7%) were women and the mean (SD) age was 46.3 (16.1) years. For correct tourniquet application, B-Con (88% correct application [n = 122]; P < .001) was superior to control (n = 104 [16%]) while instructional flashcards (n = 117 [19.6%]) and audio kit (n = 122 [23%]) groups were not. More than half of participants in point-of-care arms did not use the educational prompts as intended. Of 303 participants (65%) who were assessed 3 to 9 months after undergoing B-Con training, 165 (54.5%) could correctly apply a tourniquet. Over this period, there was no further skill decay in the adjusted model that treated time as either linear (odds ratio [OR], 0.98; 95% CI, 0.95-1.03) or quadratic (OR, 1.00; 95% CI, 1.00-1.00). The only demographic that was associated with correct application at retention was age; adults aged 18 to 35 years (n = 58; OR, 2.39; 95% CI, 1.21-4.72) and aged 35 to 55 years (n = 107; OR, 1.77; 95% CI, 1.04-3.02) were more likely to be efficacious than those older than 55 years (n = 138).
Conclusions and Relevance
In-person hemorrhage control training for laypersons is currently the most efficacious means of enabling bystanders to act to control hemorrhage. Laypersons can successfully perform tourniquet application after undergoing a 1-hour course. However, only 54.5% retain this skill after 3 to 9 months, suggesting that investigating refresher training or improved point-of-care instructions is critical.
Trial Registration
ClinicalTrials.gov Identifier: NCT03479112
This randomized clinical trial evaluates the effectiveness of different instructional point-of-care interventions and in-person training for hemorrhage control and assesses skill retention 3 to 9 months after hemorrhage control training.
Introduction
Trauma is the leading cause of mortality in the United States for individuals younger than 45 years and uncontrolled hemorrhage is the leading cause of preventable deaths.1,2 Recent military experience has shown that rapid intervention and control of extremity hemorrhage with tourniquets improves survival rates, decreasing preventable deaths by more than 50%.3,4,5,6 Emergency medical service (EMS) units average 7 minutes from the time of a “911” call to arriving on the scene, and longer delays have occurred due to scene safety concerns for arriving EMS personnel.7,8 Longer EMS response times have been associated with worse outcomes in patients with trauma and research suggests that laypersons who are trained in first-aid can, and will, effectively provide care to people with injuries.8,9 To shorten this gap between injury and care, several national initiatives aimed at translating the military experience to civilian trauma care have therefore focused on empowering laypersons to become immediate responders to control hemorrhage before the arrival of professional first responders.9 Programs, such as the White House National Security Council’s “Stop the Bleed,” the American College of Surgeons (ACS) Hartford Consensus, and the Federal Emergency Management Agency’s “You are the Help until Help arrives,” all call for educating and empowering the public in bleeding control.10,11,12,13 However, major questions remain regarding the type, frequency, and format of training needed to competently prepare nonmedical personnel for hemorrhage control.14,15,16 Recent mass casualty incidents, such as the Las Vegas, Nevada, and Parkland, Florida, mass shootings, further necessitate improved prehospital interventions to reduce mortality from trauma.8,17,18,19
The Bleeding Control Basic (B-Con) course is the ACS’s bleeding control training curriculum designed for the public to enable laypersons to act as immediate responders. The course objectives include recognizing life-threatening bleeding, proper techniques to apply pressure to wounds, and, when appropriate and available, applying extremity tourniquets.10,12 While B-Con is now being commonly taught to the public, to our knowledge its efficacy among nonmedical personnel has not been well documented. Furthermore, prior research on first aid and basic life support courses have demonstrated significant skill decay over time.20,21,22,23 B-Con’s effectiveness has yet to be formally evaluated immediately after laypersons are trained or the retention of the knowledge and skills over time.
An alternative to training all laypersons in bleeding control is using point-of-care instructional devices. Their use is exemplified by automatic external defibrillators (AEDs), which have been broadly implemented with proven effectiveness when used by laypersons using the simple point-of-care instructions without having to familiarize themselves with the device before use.24,25 Studies of point-of-care instructions for hemorrhage control have shown a promising increase in laypeople’s ability to apply tourniquets correctly without prior training, but to our knowledge, there have been no randomized clinical prospective studies comparing these interventions.26 If point-of-care educational devices can be effective, the focus of national campaigns can shift from the need to train as many members of the public as possible to a more widespread national dissemination of bleeding control kits with embedded point-of-care educational devices.
In this context, the objectives of this study were to (1) evaluate the effectiveness of different instructional point-of-care interventions and the B-Con course compared with the control and (2) evaluate the retention of B-Con training skills over time. We hypothesized that laypersons’ application of a combat application tourniquet (CAT) with different point-of-care instructional devices (either an audio kit or flashcards) will be superior to no intervention and comparable with the B-Con course. We also hypothesized that at 3 to 9 months, B-Con would continue to be superior to the control but that there would be skill decay over time.
Methods
Study Design
This is a prospective randomized clinical trial (RCT) following the Consolidated Standards of Reporting Trials guidelines.27 Partners Healthcare institutional review board approval was obtained for this study. As this trial only examined the effect of interventions on clinicians and not on patients, the institutional review board’s recommendation was to not preregister this trial on clinicaltrials.org, as this research did not meet the US Food and Drug Administration Amendments Act or International Committee of Medical Journal Editors clinical trials registration requirements. However, to comply with journal requirements, we registered this trial with ClinicalTrials.gov (NCT03479112) prior to publication. The primary outcome was the correct application of a tourniquet in each study arm and at retention testing. Secondary outcomes included time to tourniquet application and reasons for incorrect tourniquet application.
Study Participants
All participants were employees of a single stadium’s operations team (security, parking, food/beverage, and stadium operations). Employees were paid by the stadium at their usual hourly rate for the 4-hour period during which the trial and training occurred. Participation in B-Con training was a requirement of their employer. However, participation in the trial was optional and participants could withdraw consent at any time. Inclusion criteria was any volunteer employee who was age 18 years or older. Those with self-reported prior hemorrhage control training in each arm were excluded from the final analysis. Oral informed consent was obtained from all participants. Retention testing was completed at the beginning of an employee’s shift before the start of events. All instructors were either physicians, registered nurses, or emergency medical technicians and were registered instructors for the ACS B-Con course.
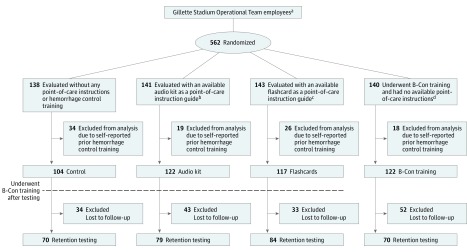
Study Protocol
Participants were randomized into 1 of 4 study arms: an audio kit with visual aids on the device (audio kit), instructional flashcards, B-Con, and a control group who received no training and had no access to any point-of-care educational prompts (Figure 1). We used permutated block randomization such that for every 4 participants who entered the staging area, 1 was assigned to each of the 4 arms. After randomization, investigators observed participants’ group assignments to direct the participant to the correct intervention/control room. Participants were blinded to what they would encounter in each intervention/control room.
Figure 1. Consolidated Standards of Reporting Flowchart for Enrollment, Randomization, and Evaluation of Participants in the Public Access and Tourniquet Training Study (PATTS) Trial.
aThe Gillette Stadium Operational Team includes employees who work in access control, as parking staff members, in food and beverage operations, or in general stadium operations.
bAudio kit point-of-care instructions included a combination of audio instructions and pictorial diagrams describing hemorrhage control techniques.
cFlashcards are a pictorial diagram with accompanying text describing hemorrhage control techniques.
dThe American College of Surgeons Bleeding Control for the Injured (B-Con), which is a 1-hour combined lecture and hands-on skills hemorrhage control training course.
After listening to the study description and giving informed consent, participants completed pretraining questionnaires that detailed their demographic data and any prior first-aid training. Participants with prior first-aid training were asked via questionnaire whether it involved hemorrhage control training, and a priori per protocol, those who reported prior hemorrhage control training proceeded through the trial but were excluded from the analysis. The reason for excluding these participants after randomization was that the self-reported hemorrhage control training status of participants was not identified until data entry into the database (Trial Protocol in Supplement 1).
Participants in the B-Con arm underwent the course first, while participants in the other study arms were tested in separate rooms. Bleeding Control Basic training consisted of a lecture followed by hands-on skills training. Participants were taught how to call for help, assess those affected, identify the location of life-threatening bleeding and apply pressure, pack a wound, and/or apply a tourniquet. In each testing room, an observer read a scenario and a mannequin with a leg amputation moulage on the floor that represented a person with an injury had a bleeding control kit available near it (eAppendix 1 in Supplement 2). All kits contained a CAT and different arms contained different point-of-care educational devices; in the control and B-Con arms, the kits contained only a tourniquet; in the flashcard arm, the kit contained an instructional card (eAppendix 2 in Supplement 2) with text and images describing the steps of tourniquet application; and in the audio kit arm, the kit contained an audio guide along with visual aids similar to the instructional card (eAppendix 3 in Supplement 2). These educational prompts are commercially available and can be found in some publicly accessible bleeding control kits. The audio guide mimics an AED by telling the user the next steps verbally while the visual cues (found on both the audio guide and flashcards) confer with diagrams and word how to control bleeding while using a tourniquet. To mimic a real-world interaction, participants were not told how to use the contents of the kit, only that “you notice a bleeding control kit on the wall.” No specific prompting was done to call attention to flashcards or audio instructions if they were present. The observer then told the participants to proceed and inform them when they believed that they were done. Timing began at that time. No feedback was given by the observer to the participant during this testing phase.
The observer recorded whether tourniquet application was correct, which was determined by a sufficient distance above the injury that was defined as at least 2 inches proximal to the amputation; adequate tightness of the tourniquet; and a time to application of fewer than 7 minutes, based on prior pilot studies.26 Tightness was assessed by the observer attempting to forcefully slide an instrument between the tourniquet and mannequin. If the application was not correct, the observer recorded which element was incorrect. In the audio guide and flashcard arm, observers also noted whether participants used the point-of-care instructions. Following the ethical principles of educational trials, all participants in the control, audio kit, and flashcard arms underwent B-Con training, currently regarded as a standard, immediately after testing. We wanted to ensure that all employees were provided a formal program of instruction that included both a didactic and practical component.
To evaluate B-Con’s durability, we performed retention testing on participants between October 2017 and January 2018. This period allowed for testing participants at a minimum of 3 months posttraining to a maximum of 9 months posttraining. Participants were evaluated in the same manner as the initial testing, had no available point-of-care instructions, and were not retrained before undergoing retention testing.
Study materials, including mannequins, audio kits, and flash cards, were purchased through the support of the Gillian Reny Stepping Strong Center for Trauma Innovation. The tourniquets that were used for testing in the study had been previously donated by North American Rescue. No monetary or in-kind support was sought or provided by device manufacturers or the ACS.
Statistical Analysis
The main outcome in the study was the dichotomous outcome of “correct tourniquet application.” During the initial testing phase, the proportion of participants who correctly applied a tourniquet in the 3 intervention arms was compared with the control using 3 pairwise 2-sided Fisher exact tests of the 3 interventions to control in an intent-to-treat analysis (as randomized).
To analyze retention, we performed 2 pairwise comparisons: (1) all participants tested at retention vs initial controls to identify long-term efficacy (correct tourniquet application) compared with no training and (2) participants tested at retention vs initial testing in the B-Con randomized arm to identify if there was a significant skill decay 3 to 9 months after training. Generalized estimating equations z tests were used in these pairwise tests to account for the repeated measures on participants who were in both the initial and retention phases.28
The Wilcoxon rank sum test was used to compare time with correct tourniquet application across arms (restricted to participants in each arm who correctly applied the tourniquet). Demographic variables for each intervention arm vs control and retention vs control were compared using Wilcoxon rank sum tests for continuous variables and 2-sided Fisher exact tests for categorical variables.
For the retention testing, we also performed logistic regression analysis to identify any demographic associations with correct tourniquet application. This model assessed for an association between days since training to retention testing, allowing for a nonlinear effect. It also assessed for different effects due to the original (randomized) arm in initial testing in case the combination of randomized arm and then B-con training had differential effects on correct tourniquet application (although our a priori hypothesis was that there would be no difference). Age was divided into a categorical variables, creating 3 groups using previously defined age breaks: young adult (age 18-35 years), middle-aged adult (age 35-55 years), and older adult (age >55 years).29
For initial testing in the RCT, using a 2-sided Fisher exact test for each of the 3 main pairwise comparisons, a total of 412 participants (103 in each study arm) were required to detect a difference of 22% or more increase in an intervention arm to control with 80% power and a 2-sided α level of 1.67%. This sample size calculation is based on an expected control group proportion of correct application of 20% and flashcard proportion of correct application of 44% based on prior studies.26,30 Besides the 3 pairwise comparisons for the initial testing in the randomized arms, we performed 2 primary pairwise comparisons of retention follow-up testing vs B-Con and control. Thus, to ensure an overall type I error rate of 5% for the 5 primary pairwise comparisons, we used a Bonferroni corrected 1.00% type I error rate. For the retention testing, our goal was to obtain a minimum of 60% follow-up to decrease the potential for selection bias.
A P value of less than .05 was used to indicate statistical significance for Bonferroni corrected pairwise comparisons and the demographic associations obtained using logistic regression. Data were analyzed using Stata, version 14.1 (StataCorp).
Results
Characteristics of Participants
Of the 562 individuals who participated, 97 reported prior hemorrhage control training and were excluded. A total of 465 individuals were included in the analysis based on the inclusion criteria. The participants were randomized into 4 study arms (Figure 1). We observed no statistically significant (P > .05) difference in age, sex, and maximum attained educational level among the different arms, while the B-Con arm had a nonstatistically significant lower proportion of participants with prior first-aid training (Table 1). A higher proportion of men (n = 274 [58.7%]) than women participated in the study overall. One-hundred eleven participants (21.7%) reported that their highest level of education was high school or less, 189 (40.7%) had some college, 128 (27.5%) had a bachelor’s degree, and 36 (7.7%) had an advanced degree.
Table 1. Demographic Dataa.
| Characteristic | No. (%) | |||||
|---|---|---|---|---|---|---|
| Overall (n = 465) |
Control (n = 104) |
Audio Kit (n = 122) |
Flashcards (n = 117) |
B-Con (n = 122) |
Retention Tested (n = 303) |
|
| Age, mean (SD), y | 46.3 (16.1) | 45.4 (15.4) | 46.9 (17.5) | 48.2 (15.6) | 44.7 (15.5) | 49.7 (14.9) |
| Female sexb | 189 (40.7) | 50 (48.1) | 43 (35.3) | 49 (41.9) | 47 (38.5) | 126 (41.6) |
| Education level | ||||||
| High school or less | 111 (23.9) | 21 (20.2) | 22 (18.0) | 33 (28.2) | 35 (28.7) | 72 (23.8) |
| Some college education | 189 (40.7) | 40 (38.5) | 55 (45.1) | 51 (43.6) | 43 (35.3) | 115 (37.9) |
| College degree | 128 (27.5) | 35 (33.7) | 35 (28.7) | 23 (19.7) | 35 (28.7) | 86 (28.4) |
| Advanced degree | 36 (7.7) | 7 (6.7) | 10 (8.2) | 10 (8.6) | 9 (7.4) | 29 (9.6) |
| Prior first-aid training without hemorrhage control training | 233 (50.1) | 233 (50.1) | 67 (54.9) | 66 (56.4) | 46 (37.7) | 161 (53.1) |
Abbreviation: B-Con, Bleeding Control Basic.
There were no statistically significant differences (P > .05) in demographics for each treatment arm and retention compared with the control (using a Bonferroni correction for multiple testing for each variable).
Two participants did not complete the survey question on sex.
Of the original 465 participants, 303 (65%) were assessed for retention. Sixty-six of the 162 (40.7%) who could not be retested no longer worked at the stadium during the retention testing phase. Exclusion of those who no longer worked at the stadium resulted in a retesting rate of 75.9%. At retention testing, there was no statistically significant (P > .05) difference between the demographics of those in the control group and those who were reassessed (Table 1). There was also no statistically significant difference between those who were lost to follow-up and control (P > .05). The range of time that retention testing was performed since training was 87 to 267 days (mean [SD], 188.9 [44.5]).
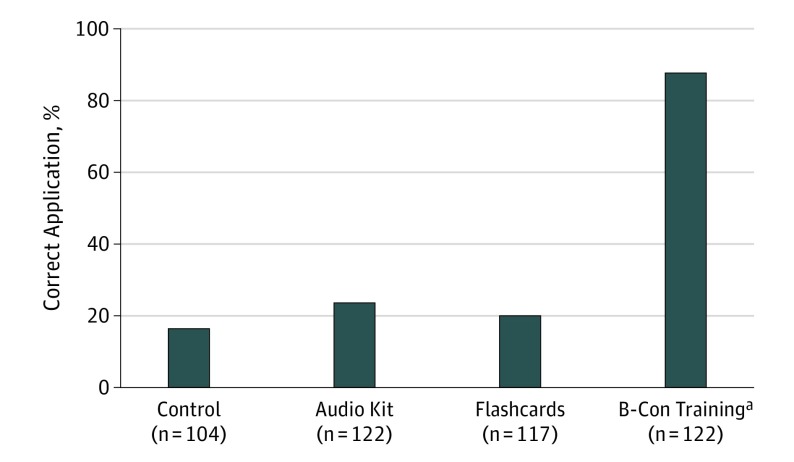
Effect of Different Interventions on Tourniquet Application
The B-Con arm had a higher proportion of correct tourniquet applications (87.7%; 95% CI, 81.8-93.6) compared with the control group (16.3%; 95% CI, 9.1-23.6; P < .001). We identified no difference in successful tourniquet application between the audio kit (23.0%; 95% CI, 15.4-30.5) and flashcard (19.7%; 95% CI, 12.3-27.0) arms compared with the control arms (16.3%; 95% CI, 9.1-23.6; P > .05) (Figure 2). Only 39 (32%) and 54 participants (43.4%) in the audio guide and flashcard groups, respectively, used the point-of-care prompts in the simulated emergency scenario.
Figure 2. Proportion of Correct Tourniquet Application at Initial Testing.
aStatistically significant (Bonferroni-corrected with P < .05) when compared with the control. B-Con indicates Bleeding Control Basic.
The median (interquartile range) time to correct tourniquet application was significantly longer than the control (47 seconds [30-54 seconds]) for both the audio kit (72.5 seconds [47-108.5 seconds]; P = .01) and flashcard arms (59 seconds [53-113 seconds]; P = .02), while there was no difference between the control and B-Con arm (43 seconds [33-52 seconds]; P = .92).
Reasons for Incorrect Tourniquet Application
Eighty percent to 89% of incorrect tourniquet applications in all arms were attributable to the tourniquet being applied too loose to be effective, with no difference between the intervention arms and control (P > .05). The flashcard (n = 41 [43.6%]; P = .02) and B-Con arm (n = 4 [26.7%]; P < .001) decreased the rate of incorrect anatomical application compared with the control (n = 74 [67.8%]) but the audio kit (n = 53 [56.4%]; P = .42) was not significantly different. Only 3 participants overall took more than 7 minutes to apply a tourniquet; no difference between the control and any of the intervention arms for this measure could be identified (control, 1; audio kit, 1; flashcards, 0; B-Con, 1; P > .05). The flashcards (n = 33 [35%]; P < .001) and B-Con (n = 1 [6.7%]; P < .001) both resulted in a lower proportion of multiple reasons for incorrect tourniquet application compared with the control (n = 55 [63.2%]) while the audio kit (n = 48 [51.1%]; P = .34) was not significantly different.
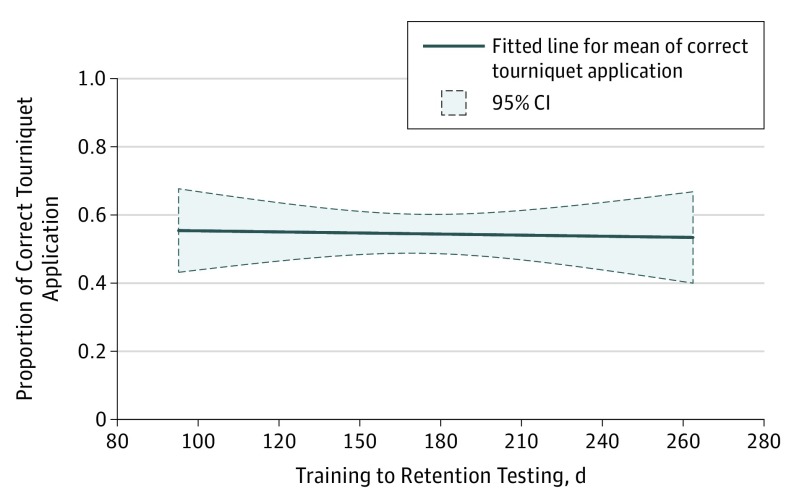
Retention Testing 3 to 9 Months After Training
The overall proportion of correct tourniquet application at retention testing was 54.5% (n = 303), which was significantly higher than the control (n = 104 [16.4%]; P < .001). Comparing those tested within an hour of receiving training (n = 122 [88.7%]) with those tested 3 to 9 months after receiving training (n = 303 [54.5%]), there was a significant skill decay (P < .001). Comparing control at baseline vs retention testing, we would need to train 2.62 (95% CI, 2.02-3.74) laypersons (“number needed to treat”) to have 1 correctly applied tourniquet. However, within the time frame of 87 to 267 days during which the participants were retested, there was no further skill decay. The adjusted logistic model allowed for nonlinear skill decay by including linear (odds ratio [OR], 0.98; 95% CI, 0.95-1.03) and quadratic (OR, 1.00; 95% CI, 1.00-1.00) effects of time, which were not significantly different (P = .74 for the 2 df test that both linear and quadratic effects equal 0) (Figure 3).
Figure 3. Proportion of Correct Tourniquet Application During Retention Testing Over 3 to 9 Months.
In the logistic regression model, the only variable associated with correct tourniquet application was age group, with young adults aged 18 to 35 years (n = 58 [67.2%]; OR, 2.39; 95% CI, 1.21-4.72) and middle-aged adults (n = 107 [59.8%]; OR, 1.77; 95% CI, 1.04-3.02) more likely to correctly apply a tourniquet compared with older adults (n = 138 [44.9%]) (Table 2). Education, sex, and prior first-aid training were not associated with increased or decreased odds of correct tourniquet application. Similar to the unadjusted model, days since training to retesting within the model showed no evidence of further skill decay over the testing interval range of 87 to 267 days.
Table 2. Multiple Logistic Regression Assessing for Demographic Associations With Correct Tourniquet Application at Retention Testing.
| Characteristic | Unadjusted Proportion of Correct Tourniquet Application, No. (%) | Adjusted Odds Ratio (95% CI) | P Value |
|---|---|---|---|
| Age group, y | |||
| Older adult (>55) (n = 138) | 62 (44.9) | 1 [Reference] | .02 |
| Middle aged adult (35-55) (n = 107) | 64 (59.8) | 1.74 (1.02-2.96) | |
| Young adult (18-35) (n = 58) | 39 (67.2) | 2.35 (1.19-4.64) | |
| Highest level of education | |||
| High school or less (n = 72) | 41 (56.9) | 1 [Reference] | .44 |
| Some college education (n = 115) | 61 (53.0) | 0.88 (0.47-1.64) | |
| Bachelor’s degree (n = 86) | 52 (60.5) | 1.14 (0.59-2.22) | |
| Advanced degree (n = 29) | 11 (37.9) | 0.54 (0.22-1.36) | |
| Sex | |||
| Female (n = 126) | 72 (57.1) | 1 [Reference] | .55 |
| Male (n = 177) | 93 (52.5) | 0.86 (0.53-1.40) | |
| Prior first-aid training without hemorrhage control training | |||
| No self-reported prior training (n = 142) | 78 (54.9) | 1 [Reference] | .72 |
| Prior self-reported first-aid training (n = 161) | 87 (54.0) | 1.09 (0.67-1.79) | |
| Training to retention testing, da | |||
| Linear effect | NA | 0.98 (0.95-1.03) | .46 |
| Mean (SD) | 188.9 (44.5) | NA | |
| Quadratic effect | NA | 1.00 (1.00-1.00) | .47 |
| Intervention arm at initial testing | |||
| Control (n = 70) | 32 (45.7) | 1 [Reference] | .32 |
| Audio kit (n = 79) | 46 (58.2) | 1.75 (0.89-3.43) | |
| Flashcards (n = 84) | 46 (54.8) | 1.58 (0.81-3.08) | |
| B-Con training (n = 70) | 41 (58.6) | 1.77 (0.88-3.56) |
Abbreviations: B-Con, Bleeding Control Basic; NA, not applicable.
P = .74 for the overall 2 df test for a trend (linear or quadratic effect) for “days since training retention testing.”
Discussion
This RCT demonstrates that in-person hemorrhage control training is superior to current flashcards, audio kits, and no prior training. Currently, 87.7% of laypersons are able to correctly apply a CAT after undergoing a 1-hour course, and the group with instructional devices performed similar to the control group that had neither hemorrhage control training or access to instructional prompts. At follow-up 3 to 9 months after initial testing, 165 of 303 (54.5%) retained the ability to correctly apply a CAT.
Our results confirm that B-Con training is an effective way to train bystanders in bleeding control. An unexpected finding was the lack of further skill decay regardless of the timing of retention testing. This is contrary to literature about other first aid and basic life support skills that shows a continued degradation over time.21,22,23,31 Prior studies on bleeding control and tourniquet application have solely assessed correct application in military populations and hospital employees.32,33,34,35 This expands these findings to laypersons and supports the “call to arms” to engage all citizens in bleeding control programs by both governmental and nongovernmental organizations.
The 2 point-of-care prompts used in this trial were not superior to the control group in increasing the proportion of correct tourniquet application. This finding is inconsistent with prior observational studies conducted by Goolsby et al.26,30 This discrepancy is explained by a purposeful difference in methods. In the studies by Goolsby et al,26,30 participants were specifically presented with the point-of-care instructions and asked to use them, yielding a correct tourniquet rate of 44%. In this study, participants were presented with bleeding control kits that included instructions but were not prompted to use them, mimicking a real-world interaction. Automatic external defibrillators have been proposed as a model for integrating point-of-care instructions for bleeding control kits. However, AEDs require the user to follow instructional prompts to be activated and used, whereas tourniquets do not; thus, they may be applied even when an immediate responder ignores accompanying instructions. Survey results have shown that laypersons lack intuitive knowledge about the contents of bleeding control kits and how to use them without instruction.36 This lack of knowledge of bleeding control kits compared with AED kits, which two-thirds of the general public in urban areas are able to correctly identify, is likely rooted in the relative novelty of hemorrhage control training and the lack of public availability of bleeding control kits compared with widespread cardiopulmonary resuscitation (CPR) training and AED availability in the United States.37 While point-of-care instructions continue to be refined, our findings support focusing initially on identifying and formally training groups of individuals with the highest likelihood to encounter mass-casualty incidents: those who work in mass-gathering areas such as airports, malls, schools, stadiums and transportation hubs, an approach already validated with AED implementation.1,38,39
Incorrect tourniquet application was primarily due to a lack of tension, incorrect location, or some combination of the 2. These observations are consistent with prior studies that demonstrated that looseness, excess of slack in the CAT strap, or too few turns of the windlass were the most common reasons for failure.26,33 These findings support the need for real-time in-person feedback from instructors and help explain why the instructional prompts used in this study were not effective.
Our finding that 54.5% of participants at retention testing successfully applied the tourniquet is both promising and concerning. The 54.5% skill retention is greater than prior similar skills testing (CPR/AED) reported; however, it is unclear with what frequency or content refresher training must occur for an improved rate of knowledge retention.21,22,23,40 It is also unclear what the target retention rate should be for the population trained. While various bleeding control initiatives are ideologically important, we should invest in a national research agenda to identify these and other gaps in knowledge in parallel to implementation. Skill retention must be a key element of further community resilience-building initiatives.
Limitations
There are limitations to this study. It does not address whether laypersons understand when to apply other hemorrhage control techniques beyond tourniquets when the scenario is less clear. While B-Con teaches that pressure to the site of bleeding is often the first step and is effective at controlling many types of hemorrhage, this knowledge and choice in hemorrhage control technique application is difficult to evaluate in a simulated scenario. An additional limitation is that the study scenario does not mimic the stress and chaos of a true emergency, which might be better replicated with a high-fidelity simulation. Within this RCT, evaluators were not blinded, as they needed to assess each intervention arm, although given the magnitude of differences seen, this potential source of bias is minimal. The findings of this study are likely generalizable to the general population based on the demographics of the sample population, but a single-site study is a limitation. Finally, during retention testing, 35% of the original sample was lost to follow-up, which raises the potential for selection bias. A significant proportion of these participants could not be retested as they no longer worked for the stadium. Furthermore, the effect of this loss to follow-up is likely minimal as the demographics measured for followed-up participants and lost to follow-up did not vary significantly (Table 1; eTable in Supplement 2).
Future research on point-of-care educational devices for hemorrhage control should emulate the initial development of AED devices. The current iterations of AEDs, despite their underlying complexity, are intuitive to use by most laypersons, enabling them to be effective in real-world scenarios.41,42 While the point-of-care prompts were not effective in this trial, we believe that with further development and testing they may eventually be a critical component of a national strategy to minimize preventable deaths from trauma.43 Ultimately, just as reducing mortality from out of hospital cardiac arrest required improvements in each link in the chain of survival, a comprehensive effort to decrease death from trauma will require a similar multipronged, comprehensive strategy.44,45
Conclusions
Formal hands-on hemorrhage control training was found to be the most effective method to enable laypersons to control hemorrhage using a tourniquet. There is skill decay after training, with just over half correctly applying the tourniquet 3 to 9 months after training, but this remains superior to the control. The current iterations of point-of-care prompts require refinement and innovation to engage laypersons to effectively apply tourniquets.
Trial Protocol.
eAppendix 1. Simulation Scenario Read to Participants.
eAppendix 2. Flashcard Instructions in Bleeding Control Kit Describing Tourniquet Application Technique.
eAppendix 3. North American Rescue Bleeding Control Audio Guidance Kit.
eTable. Demographics of Different Arms at Retention Testing.
References
- 1.Berwick D, Downey A, Cornett E, eds. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. Washington, DC: National Academies Press; 2016. [PubMed] [Google Scholar]
- 2.Rhee P, Joseph B, Pandit V, et al. . Increasing trauma deaths in the United States. Ann Surg. 2014;260(1):13-21. [DOI] [PubMed] [Google Scholar]
- 3.Eastridge BJ, Mabry RL, Seguin P, et al. . Death on the battlefield (2001-2011): implications for the future of combat casualty care. J Trauma Acute Care Surg. 2012;73(6)(suppl 5):S431-S437. [DOI] [PubMed] [Google Scholar]
- 4.Kragh JF Jr, Walters TJ, Baer DG, et al. . Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1-7. [DOI] [PubMed] [Google Scholar]
- 5.Kotwal RS, Montgomery HR, Kotwal BM, et al. . Eliminating preventable death on the battlefield. Arch Surg. 2011;146(12):1350-1358. [DOI] [PubMed] [Google Scholar]
- 6.Kotwal RS, Howard JT, Orman JA, et al. . The effect of a golden hour policy on the morbidity and mortality of combat casualties. JAMA Surg. 2016;151(1):15-24. [DOI] [PubMed] [Google Scholar]
- 7.Mell HK, Mumma SN, Hiestand B, Carr BG, Holland T, Stopyra J. Emergency medical services response times in rural, suburban, and urban areas. JAMA Surg. 2017;152(10):983-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schenk E, Wijetunge G, Mann NC, Lerner EB, Longthorne A, Dawson D. Epidemiology of mass casualty incidents in the United States. Prehosp Emerg Care. 2014;18(3):408-416. [DOI] [PubMed] [Google Scholar]
- 9.Haider AH, Haut ER, Velmahos GC. Converting bystanders to immediate responders: we need to start in high school or before. JAMA Surg. 2017;152(10):909-910. [DOI] [PubMed] [Google Scholar]
- 10.Knudson MM, Velmahos G, Cooper ZR. Response to mass casualty events: from the battlefield to the Stop the Bleed campaign. Trauma Surg & Acute Care Open. 2016;1(1):1-3. doi: 10.1136/tsaco-2016-000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Federal Emergency Management Agency You are the help until help arrives. https://community.fema.gov/until-help-arrives. Accessed October 19, 2017.
- 12.American College of Surgeons BleedingControl.org—about us. http://www.bleedingcontrol.org/about-bc. Accessed July 17, 2017.
- 13.Jacobs LM; Joint Committee to Create a National Policy to Enhance Survivability from Intentional Mass Casualty and Active Shooter Events . The Hartford Consensus IV: a call for increased national resilience. Bull Am Coll Surg. 2016;101(3):17-24. [PubMed] [Google Scholar]
- 14.Zideman DA, Singletary EM, De Buck ED, et al. ; First Aid Chapter Collaborators . Part 9: first aid: 2015 International Consensus on First Aid Science with treatment recommendations. Resuscitation. 2015;95:e225-e261. [DOI] [PubMed] [Google Scholar]
- 15.Van de Velde S, Heselmans A, Roex A, Vandekerckhove P, Ramaekers D, Aertgeerts B. Effectiveness of nonresuscitative first aid training in laypersons: a systematic review. Ann Emerg Med. 2009;54(3):447-457, 457.e1-457.e5. [DOI] [PubMed] [Google Scholar]
- 16.He Z, Wynn P, Kendrick D. Non-resuscitative first-aid training for children and laypeople: a systematic review. Emerg Med J. 2014;31(9):763-768. [DOI] [PubMed] [Google Scholar]
- 17.Blair J, Schwiet K A study of active shooter incidents in the United States between 2000-2013. https://www.fbi.gov/file-repository/active-shooter-study-2000-2013-1.pdf/view. Accessed December 10, 2017.
- 18.Biddinger PD, Baggish A, Harrington L, et al. . Be prepared—the Boston Marathon and mass-casualty events. N Engl J Med. 2013;368(21):1958-1960. [DOI] [PubMed] [Google Scholar]
- 19.Campion EW, Morrissey S, Malina D, Sacks CA, Drazen JM. After the mass shooting in Las Vegas—finding common ground on gun control. N Engl J Med. 2017;377(17):1679-1680. [DOI] [PubMed] [Google Scholar]
- 20.Anderson GS, Gaetz M, Statz C, Kin B. CPR skill retention of first aid attendants within the workplace. Prehosp Disaster Med. 2012;27(4):312-318. [DOI] [PubMed] [Google Scholar]
- 21.Woollard M, Whitfeild R, Smith A, et al. . Skill acquisition and retention in automated external defibrillator (AED) use and CPR by lay responders: a prospective study. Resuscitation. 2004;60(1):17-28. [DOI] [PubMed] [Google Scholar]
- 22.Mpotos N, De Wever B, Cleymans N, et al. . Repetitive sessions of formative self-testing to refresh CPR skills: a randomised non-inferiority trial. Resuscitation. 2014;85(9):1282-1286. [DOI] [PubMed] [Google Scholar]
- 23.Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30-min video self-training: a controlled randomized study. Resuscitation. 2007;74(3):476-486. [DOI] [PubMed] [Google Scholar]
- 24.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347(16):1242-1247. [DOI] [PubMed] [Google Scholar]
- 25.Page RL, Joglar JA, Kowal RC, et al. . Use of automated external defibrillators by a U.S. airline. N Engl J Med. 2000;343(17):1210-1216. [DOI] [PubMed] [Google Scholar]
- 26.Goolsby C, Branting A, Chen E, Mack E, Olsen C. Just-in-time to save lives: a pilot study of layperson tourniquet application. Acad Emerg Med. 2015;22(9):1113-1117. [DOI] [PubMed] [Google Scholar]
- 27.Schulz KF, Altman DG, Moher D, Group C; CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726-732. [DOI] [PubMed] [Google Scholar]
- 28.Lipsitz SR, Fitzmaurice GM, Orav EJ, Laird NM. Performance of generalized estimating equations in practical situations. Biometrics. 1994;50(1):270-278. [PubMed] [Google Scholar]
- 29.Petry NM. A comparison of young, middle-aged, and older adult treatment-seeking pathological gamblers. Gerontologist. 2002;42(1):92-99. [DOI] [PubMed] [Google Scholar]
- 30.Goolsby C, Chen E, Branting A, et al. . Analysis of layperson tourniquet application using a novel color-coded device. Disaster Med Public Health Prep. 2016;10(2):274-280. [DOI] [PubMed] [Google Scholar]
- 31.Saraç L, Ok A. The effects of different instructional methods on students’ acquisition and retention of cardiopulmonary resuscitation skills. Resuscitation. 2010;81(5):555-561. [DOI] [PubMed] [Google Scholar]
- 32.Jacobs LM, Burns KJ. Tourniquet application training for individuals with and without a medical background in a hospital setting. J Trauma Acute Care Surg. 2015;78(2):442-445. [DOI] [PubMed] [Google Scholar]
- 33.Baruch EN, Kragh JF Jr, Berg AL, et al. . Confidence-competence mismatch and reasons for failure of non-medical tourniquet users. Prehosp Emerg Care. 2017;21(1):39-45. [DOI] [PubMed] [Google Scholar]
- 34.Schreckengaust R, Littlejohn L, Zarow GJ. Effects of training and simulated combat stress on leg tourniquet application accuracy, time, and effectiveness. Mil Med. 2014;179(2):114-120. [DOI] [PubMed] [Google Scholar]
- 35.Unlu A, Kaya E, Guvenc I, et al. . An evaluation of combat application tourniquets on training military personnel: changes in application times and success rates in three successive phases. J R Army Med Corps. 2015;161(4):332-335. [DOI] [PubMed] [Google Scholar]
- 36.Hegvik JR, Spilman SK, Olson SD, Gilchrist CA, Sidwell RA. Effective hospital-wide education in hemorrhage control. J Am Coll Surg. 2017;224(5):796-799.e1. [DOI] [PubMed] [Google Scholar]
- 37.Gonzalez M, Leary M, Blewer AL, et al. . Public knowledge of automatic external defibrillators in a large US urban community. Resuscitation. 2015;92:101-106. [DOI] [PubMed] [Google Scholar]
- 38.Folke F, Lippert FK, Nielsen SL, et al. . Location of cardiac arrest in a city center: strategic placement of automated external defibrillators in public locations. Circulation. 2009;120(6):510-517. [DOI] [PubMed] [Google Scholar]
- 39.Winkle RA. The effectiveness and cost effectiveness of public-access defibrillation. Clin Cardiol. 2010;33(7):396-399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baruch EN, Benov A, Shina A, et al. . Does practice make perfect? prospectively comparing effects of 2 amounts of practice on tourniquet use performance. Am J Emerg Med. 2016;34(12):2356-2361. [DOI] [PubMed] [Google Scholar]
- 41.Mosesso VN Jr, Shapiro AH, Stein K, Burkett K, Wang H. Effects of AED device features on performance by untrained laypersons. Resuscitation. 2009;80(11):1285-1289. [DOI] [PubMed] [Google Scholar]
- 42.Kragholm K, Wissenberg M, Mortensen RN, et al. . Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med. 2017;376(18):1737-1747. [DOI] [PubMed] [Google Scholar]
- 43.Rasmussen TE, Kellermann AL. Wartime Lessons—Shaping a National Trauma Action Plan. N Engl J Med. 2016;375(17):1612-1615. [DOI] [PubMed] [Google Scholar]
- 44.Blom MT, Beesems SG, Homma PC, et al. . Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation. 2014;130(21):1868-1875. [DOI] [PubMed] [Google Scholar]
- 45.Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the “chain of survival” concept. a statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation. 1991;83(5):1832-1847. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.
eAppendix 1. Simulation Scenario Read to Participants.
eAppendix 2. Flashcard Instructions in Bleeding Control Kit Describing Tourniquet Application Technique.
eAppendix 3. North American Rescue Bleeding Control Audio Guidance Kit.
eTable. Demographics of Different Arms at Retention Testing.