Abstract
Importance
Nonbattle injury (NBI) among deployed US service members increases the burden on medical systems and results in high rates of attrition, affecting the available force. The possible causes and trends of NBI in the Iraq and Afghanistan wars have, to date, not been comprehensively described.
Objectives
To describe NBI among service members deployed to Iraq and Afghanistan, quantify absolute numbers of NBIs and proportion of NBIs within the Department of Defense Trauma Registry, and document the characteristics of this injury category.
Design, Setting, and Participants
In this retrospective cohort study, data from the Department of Defense Trauma Registry on 29 958 service members injured in Iraq and Afghanistan from January 1, 2003, through December 31, 2014, were obtained. Injury incidence, patterns, and severity were characterized by battle injury and NBI. Trends in NBI were modeled using time series analysis with autoregressive integrated moving average and the weighted moving average method. Statistical analysis was performed from January 1, 2003, to December 31, 2014.
Main Outcomes and Measures
Primary outcomes were proportion of NBIs and the changes in NBI over time.
Results
Among 29 958 casualties (battle injury and NBI) analyzed, 29 003 were in men and 955 were in women; the median age at injury was 24 years (interquartile range, 21-29 years). Nonbattle injury caused 34.1% of total casualties (n = 10 203) and 11.5% of all deaths (206 of 1788). Rates of NBI were higher among women than among men (63.2% [604 of 955] vs 33.1% [9599 of 29 003]; P < .001) and in Operation New Dawn (71.0% [298 of 420]) and Operation Iraqi Freedom (36.3% [6655 of 18 334]) compared with Operation Enduring Freedom (29.0% [3250 of 11 204]) (P < .001). A higher proportion of NBIs occurred in members of the Air Force (66.3% [539 of 810]) and Navy (48.3% [394 of 815]) than in members of the Army (34.7% [7680 of 22 154]) and Marine Corps (25.7% [1584 of 6169]) (P < .001). Leading mechanisms of NBI included falls (2178 [21.3%]), motor vehicle crashes (1921 [18.8%]), machinery or equipment accidents (1283 [12.6%]), blunt objects (1107 [10.8%]), gunshot wounds (728 [7.1%]), and sports (697 [6.8%]), causing predominantly blunt trauma (7080 [69.4%]). The trend in proportion of NBIs did not decrease over time, remaining at approximately 35% (by weighted moving average) after 2006 and approximately 39% by autoregressive integrated moving average. Assuming stable battlefield conditions, the autoregressive integrated moving average model estimated that the proportion of NBIs from 2015 to 2022 would be approximately 41.0% (95% CI, 37.8%-44.3%).
Conclusions and Relevance
In this study, approximately one-third of injuries during the Iraq and Afghanistan wars resulted from NBI, and the proportion of NBIs was steady for 12 years. Understanding the possible causes of NBI during military operations may be useful to target protective measures and safety interventions, thereby conserving fighting strength on the battlefield.
This cohort study describes nonbattle injury among US service members deployed to Iraq and Afghanistan, quantifies absolute numbers of nonbattle injuries and proportion of nonbattle injuries within the Department of Defense Trauma Registry, and documents the characteristics of this injury category.
Key Points
Question
What are the causes and trend of nonbattle injury among US service members deployed to Iraq and Afghanistan?
Findings
In a cohort study of US military casualties among service members evacuated from Iraq and Afghanistan, nonbattle injury accounted for approximately one-third of total casualties and 11.5% of all deaths. The proportion of nonbattle injury was consistent and predictable.
Meaning
These findings document the significance and magnitude of nonbattle injury in the deployed environment; prevention of nonbattle injury could reduce a portion of the injury burden sustained during war.
Introduction
Nonbattle injury (NBI) in deployed US military service members increases the burden on the military health care system, reduces the available fighting force, and has a preventable component.1,2,3,4,5,6 Leading causes are attributed to physical training, falls, and sports injuries.4,5,7 Nonbattle injury among deployed forces may have different possible causes, deplete medical resources, increase costs, decrease mission capabilities, and result in long-term disability for injured service members.1,2,4,5
Historically, NBI has contributed to morbidity and mortality during military operations,8,9,10 accounting for 13% of hospital admissions during the Vietnam War11 and 25% during Operation Desert Shield and Operation Desert Storm.12 Half of all US service member deaths during Operation Desert Shield were attributed to NBI.13 During the wars in Iraq and Afghanistan, NBI has continued to be a significant burden. Using aeromedical evacuation records, Patel et al14 demonstrated that 33% of medical evacuations of US Army soldiers from the combat theater of operations resulted from NBI.
Despite the historical burden of NBI, research has focused primarily on the incidence and prevention of battle injury (BI). Thus, NBI in recent conflicts has not been rigorously characterized. Previous research on NBI has focused on the anatomical region injured, aggregate rates of NBI in conjunction with medical disease,15,16 and investigations specific to single military services.5,7,17,18,19,20 Aside from the 12-year analysis by Patel et al,14 previous analyses of NBI have examined only limited periods.
Because NBI constitutes a potentially preventable drain on deployed military forces, data identifying specific deployment-related NBI risks may be helpful to inform Department of Defense leadership for consideration of existing or potentially new safety policies for deployed operational theaters. Thus, we performed a comprehensive analysis of the possible causes and trend of NBI sustained by service members during combat operations in Iraq and Afghanistan.
Methods
Patient Population
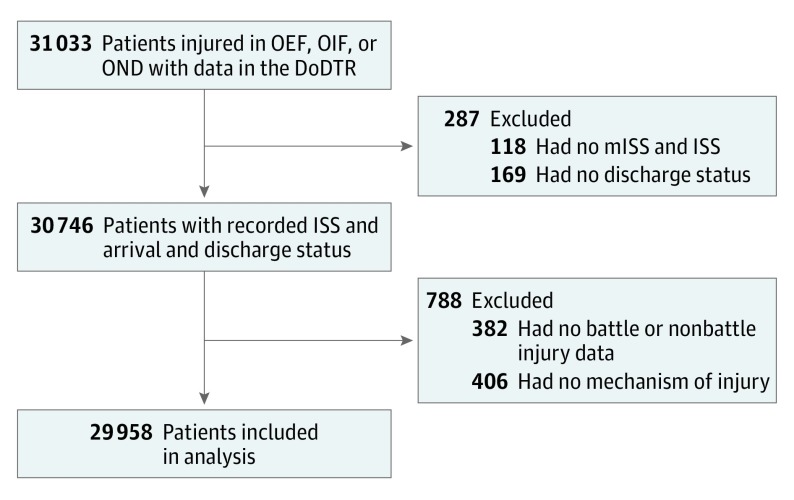
We conducted a retrospective analysis of all service members injured and presenting alive to a Role 3 medical treatment facility (R3MTF) in Iraq (Operation Iraqi Freedom [OIF] and Operation New Dawn [OND]) and Afghanistan (Operation Enduring Freedom [OEF]) from January 1, 2003, through December 31, 2014. We used data extracted from the Department of Defense Trauma Registry (DoDTR).21,22,23 A total of 29 958 casualties met study inclusion criteria (Figure 1). Patients who were evacuated for disease or psychological care were excluded. This study was conducted in accordance with a protocol reviewed and approved by the US Army Medical Research and Materiel Command Institutional Review Board (M-10563). The requirement to obtain informed consent was waived by the US Army Medical Research and Materiel Command Institutional Review Board as allowed under 32 CFR 219.116(d).
Figure 1. Study Population.
DoDTR indicates Department of Defense Trauma Registry; ISS, injury severity score; mISS, military injury severity score; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; and OND, Operation New Dawn.
Study Definitions
The injury characteristics included classification as BI or NBI, primary mechanism and type of injury, and dominant body region injured. Battle injury was defined as any injury occurring from battle-related activities or hostile actions. Nonbattle injury was defined as any injury not directly attributable to hostile action or terrorist activity, including unintentional and/or self-inflicted injuries.24 Mechanisms of injury were categorized as (1) explosion (aerial bomb, explosively formed projectile, improvised explosive device, person-borne improvised explosive device, vehicle-borne improvised explosive device, or rocket-propelled grenade); (2) gunshot wound; (3) motor vehicle crash (MVC); (4) helicopter or airplane crash; and (5) other mechanisms, such as sports, machinery or equipment, fall, chemical, electrical, and fire or flame. Types of injury were categorized as penetrating, blunt, burn, and other or unknown. Injury severity was measured using the injury severity score and the military injury severity score.24
Ideally, the incidence density rate (also known as the person-time incidence rate) of NBI would be calculated as the number of injuries caused by noncombat trauma events divided by the total number of service members at risk in a period. However, because the DoDTR is a registry for trauma-induced injury, the required denominator data (overall number of service members deployed) used to calculate NBI incidence rate are not collected. Therefore, the proportion of individuals with NBI among total casualties presenting to the R3MTFs was used as a primary outcome measure.
Statistical Analysis
Statistical analysis was performed from January 1, 2003, to December 31, 2014. Descriptive statistics characterized the demographics and injuries of the patients. Categorical variables were presented as frequencies and percentages and tested using the χ2 test. Continuous variables were expressed as means and SDs or medians and interquartile ranges (IQRs) and were tested using the t test or Mann-Whitney test when appropriate. The regression analysis of proportion of NBIs over time by quarters was conducted to test for linear trend. The weighted moving average was also applied. The proportion of NBIs was compared among different strata of demographics (eg, sex and race/ethnicity) and injury characteristic variables (eg, mechanism and type of injury). We also investigated the changes in proportion of NBIs over time during the study period using time series analysis with autoregressive integrated moving average (ARIMA), which is more appropriate for data with autocorrelation and is better suited for revealing trends and forecasting the NBI rate.
The time series analysis fitted the quarterly proportion of NBI data from 2003 to 2014 using an ARIMA model to estimate future NBI rates. Trend stationarity was examined using the autocorrelation function and tested by the Dickey-Fuller test.25 Autocorrelations at various lags with Ljung-Box χ2 statistics were used to test for white noise or uncorrelated random variables with a mean of zero and no correlation between its values at different times.26 The values p, d, and q in the ARIMA model were selected to represent the number of autoregressive lags (p), level of differences (d), and moving average (q). Estimations and corresponding 95% CIs were also presented. Statistical significance was determined at the P < .05 level (2-sided). All data were analyzed using SAS, version 9.4 (SAS Institute Inc).
Results
Patient Population
A total of 29 958 service members injured in Iraq and Afghanistan are described in the Table. Most of the patients were men (29 003 [96.8%]), with a median age at injury of 24 years (IQR, 21-29 years). Most service members who were injured were from the US Army (22 154 [74.0%]), followed by the US Marine Corps (6169 [20.6%]), and were injured in OIF and OND (18 754 [62.6%]). Among the 16 512 patients with documented race/ethnicity, 11 625 (70.4%) were white. Overall, the most common primary mechanisms of injury were explosion (15 414 [51.5%]), followed by gunshot wounds (4447 [14.8%]) and MVCs (2196 [7.3%]). The dominant type of injury was blunt (16 266 [54.3%]), followed by penetrating (11 958 [39.9%]). Overall mortality (BI + NBI) was 6.0% (n = 1788) in this cohort.
Table. Characteristics of the Patients and Their Combat-Related Injuriesa.
| Characteristic | All (N = 29 958) | Battle Injury (n = 19 755) | Nonbattle Injury (n = 10 203) | P Valueb |
|---|---|---|---|---|
| Sex | ||||
| Male | 29 003 (96.8) | 19 404 (98.2) | 9599 (94.1) | <.001 |
| Female | 955 (3.2) | 351 (1.8) | 604 (5.9) | |
| Age at injury, median (IQR), y | 24 (21-29) | 24 (21-28) | 25 (21-31) | <.001 |
| Race/ethnicityc | ||||
| White | 11 625/16 512 (70.4) | 7645/10 402 (73.5) | 3980/6110 (65.1) | <.001 |
| Black | 1725/16 512 (10.4) | 826/10 402 (7.9) | 899/6110 (14.7) | |
| Hispanic | 878/16 512 (5.3) | 557/10 402 (5.4) | 321/6110 (5.3) | |
| Other | 2284/16 512 (13.8) | 1374/10 402 (13.2) | 910/6110 (14.9) | |
| Theater of operation | ||||
| OEF | 11 204 (37.4) | 7954 (40.3) | 3250 (31.9) | <.001 |
| OIF | 18 334 (61.2) | 11 679 (59.1) | 6655 (65.2) | |
| OND | 420 (1.4) | 122 (0.6) | 298 (2.9) | |
| Branch of serviced | ||||
| US Army | 22 154 (74.0) | 14 474 (73.3) | 7680 (75.3) | <.001 |
| US Air Force | 810 (2.7) | 273 (1.4) | 537 (5.3) | |
| US Marine Corps | 6169 (20.6) | 4585 (23.2) | 1584 (15.5) | |
| US Navy | 815 (2.7) | 421 (2.1) | 394 (3.9) | |
| Primary mechanism of injury | ||||
| Explosion | 15 414 (51.5) | 15 178 (76.8) | 236 (2.3) | <.001 |
| Gunshot wounds | 4447 (14.8) | 3719 (18.8) | 728 (7.1) | |
| Motor vehicle crash | 2196 (7.3) | 275 (1.4) | 1921 (18.8) | |
| Helicopter or plane crash | 267 (0.9) | 98 (0.5) | 169 (1.7) | |
| Other or unknown | 7634 (25.5) | 485 (2.5) | 7149 (70.1) | |
| Primary type of injury | ||||
| Penetrating | 11 958 (39.9) | 10 010 (50.7) | 1948 (19.1) | <.001 |
| Blunt | 16 266 (54.3) | 9186 (46.5) | 7080 (69.4) | |
| Burn | 994 (3.3) | 479 (2.4) | 515 (5.0) | |
| Other or unknown | 740 (2.5) | 80 (0.4) | 660 (6.5) | |
| Dominant body regione | ||||
| Head and neck | 10 965 (36.6) | 8412 (42.6) | 2553 (25.0) | <.001 |
| Face | 5836 (19.5) | 4727 (23.9) | 1109 (10.9) | <.001 |
| Thorax | 3694 (12.3) | 2838 (14.4) | 865 (8.5) | <.001 |
| Abdomen | 4427 (14.8) | 3607 (18.3) | 820 (8.0) | <.001 |
| Extremities | 14 798 (49.4) | 9271 (46.9) | 5527 (54.2) | <.001 |
| External | 20 397 (68.1) | 15 531 (78.6) | 4866 (47.7) | <.001 |
| Injury Severity score, median (IQR) | ||||
| Civilian (ISS) | 5 (2-10) | 6 (2-14) | 4 (1-5) | <.001 |
| Military (mISS) | 5 (2-13) | 6 (2-18) | 4 (1-5) | <.001 |
| Mortality | 1788 (6.0) | 1582 (8.0) | 206 (2.0) | <.001 |
Abbreviations: IQR, interquartile range; ISS, injury severity score; mISS, military injury severity score; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OND, Operation New Dawn.
Data are presented as number (percentage) of patients unless otherwise indicated.
P values were calculated with the use of a χ2, t test, or Wilcoxon Mann-Whitney test as appropriate.
A total of 13 446 patients (44.9%) had no race/ethnicity data available.
Missing data (n = 10).
A total of 1 to 6 injured body regions per patient. For battle injuries and nonbattle injuries, dominant body region categories were tested as mutually exclusive categorical variables.
Proportion of NBI
Of the 29 958 patients admitted to R3MTFs, 10 203 patients sustained injuries from nonbattle activities, accounting for 34.1% of casualties (Table). Comparative analyses indicated a higher proportion of NBIs among women than among men (63.2% [604 of 955] vs 33.1% [9599 of 29 003]; P < .001) (Figure 2A and eTable 1 in the Supplement) and among black patients (52.1% [899 of 1725]) than among Hispanic patients (36.6% [321 of 878]) and white patients (34.2% [3980 of 11 625]); P < .001 (Figure 2B and eTable 1 in the Supplement). The extent of NBI varied by theater of operation: OND exhibited a greater proportion of NBIs (71.0% [298 of 420]) than did OIF (36.3% [6655 of 18 334]) and OEF (29.0% [3250 of 11 204]; P < .001) (Figure 2C and eTable 1 in the Supplement). Although the Army and Marine Corps had higher absolute numbers of NBI-associated casualties, a higher proportion of NBIs was observed in the Air Force (66.3% [539 of 810]) and Navy (48.3% [394 of 815]) compared with the Army (34.7% [7680 of 22 154]) and Marine Corps (25.7% [1584 of 6169]; P < .001) (Figure 2D and eTable 1 in the Supplement).
Figure 2. Proportion of Nonbattle Injury (NBI).
BI indicates battle injury; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; and OND, Operation New Dawn. P < .001 for all.
The proportion of NBIs was higher among those who experienced an MVC (87.5% [1921 of 2196]) and helicopter or airplane crash (63.3% [169 of 267]) compared with those who experienced explosions (1.5% [236 of 15 414]), whereas 16.4% of gunshot wounds (728 of 4447) were from nonbattle activities (P < .001) (Figure 2E and eTable 1 in the Supplement). The proportion of NBIs was highest for burns (51.8% [515 of 994]), blunt trauma (43.5% [7080 of 16 266]), and other or unknown trauma (89.2% [660 of 740]), while the primary mechanisms of injury in BI were penetrating trauma (83.7% [10 010 of 11 958]) and blunt injury (56.5% [9186 of 16 266]; P < .001) (Figure 2F and eTable 1 in the Supplement).
The proportion of NBI varied across injured body regions, ranging from 18.5% for the abdomen (820 of 4427) to 37.3% for the extremities (5527 of 14798) and was highest for the extremities, followed by external injuries, including those to the skin and soft tissue (23.9% [4866 of 20 397]; P < .001) (Figure 2G and eTable 1 in the Supplement). Injuries to the extremities accounted for 5527 patients with an NBI (54.2%) and external injuries accounted for 4866 of 20 397 body regions in patients with an NBI (47.7%) (Table). Nonbattle injuries were less severe than BIs, with a median injury severity score of 4 (IQR, 1-5) vs 6 (IQR, 2-14) (P < .001) and a median military injury severity score of 4 (IQR, 1-5) vs 6 (IQR, 2-18) (P < .001) (Table). Nonbattle injuries were less likely to produce multiple trauma; 1165 of 10 203 patients with NBIs (11.4%) vs 6853 of 19 755 patients with BIs (34.7%) were injured in 3 or more body regions (P < .001) (eFigure 1 in the Supplement).
Mortality was higher for BIs (1582 of 19 755 [8.0%]) than NBIs (206 [2.0%]; P < .001) (Table). Nonbattle injuries accounted for 206 of 1788 deaths (11.5%) in this cohort.
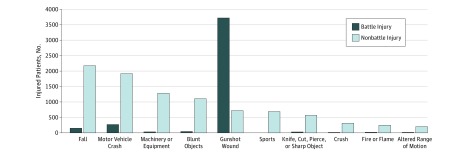
Possible Causes of NBIs
Mechanisms and types of injury were different between NBIs and BIs. Battle injuries were caused primarily by explosives (15 178 of 19 755 [76.8%]) and gunshot wounds (3719 of 19 755 [18.8%]) (Table and Figure 3). The most common causes of NBI were falls (2178 [21.3%]), MVC (1921 [18.8%]), machinery or equipment (1283 [12.6%]), blunt objects (1107 [10.8%]), gunshot wounds (728 [7.1%]), and sports (697 [6.8%]) (Figure 3 and eTable 2 in the Supplement). The top 10 causes of NBI in OEF, OIF, and OND were similar, with slight differences in rank-ordered frequency (eTable 2 in the Supplement).
Figure 3. Possible Causes of Nonbattle Injury and Battle Injury in US Service Members in the Afghanistan and Iraq Conflicts.
Distribution of common possible causes in Afghanistan and the Iraq War zone stratified by injury classification.
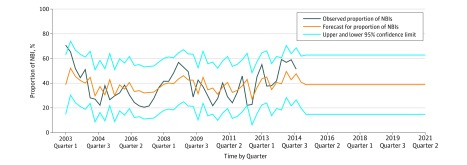
Trend in NBIs
The quarterly time plot of BI and NBI cases from January 2003 to December 2014 shows a generally decreasing trend in the number of BIs and NBIs (eFigure 2A in the Supplement). The observed proportion of NBI ranged from 20.6% to 70.8%, with a mean (SD) of 38.5% (13.1%) (eFigure 2B in the Supplement) or 38.8% (8.8%) using the weighted moving average method (eFigure 3 in the Supplement). The proportion of NBI decreased from 70% in 2003 to approximately 35% in 2006, then stabilized at approximately 35% (eFigure 3 in the Supplement). However, regression analysis shows that the proportion of NBIs over time by quarter did not significantly decrease (eFigure 3 in the Supplement).
In the time series analysis, the plot of the time series original data of proportion of NBIs (d = 0) showed that the data were stationary with the mean (SD) of 38.5% (13.0%) (Figure 4 and eFigure 4A and B in the Supplement). The autocorrelation function plot suggests that the change in proportion of NBIs was highly autocorrelated, with lag 1 or lag 2 (p = 1 or p = 2) models potentially being good models to describe this process (eFigure 4B in the Supplement). The partial autocorrelation function plot suggests that the best model for the moving average uses lag 1 (q = 1) (eFigure 4C in the Supplement). Two ARIMA models were suitable for estimation: ARIMA (1, 0, 1) model (Figure 4) and ARIMA (2, 0, 1) model (eFigure 5 in the Supplement). The ARIMA (1, 0, 1) model was selected (Figure 4 and eTable 3 in the Supplement), estimating that assuming stable battlefield injury risk conditions, the proportion of NBIs from 2015 to 2022 would be approximately 41.0% (95% CI, 37.8%-44.3%). Results from the ARIMA (2, 0, 1) model were similar (eFigure 5 in the Supplement). A detailed time series analysis is described in eTable 3 and eFigure 4 in the Supplement.
Figure 4. Time Series Analysis With Autoregressive Integrated Moving Average (1,0,1) Model.
Autoregressive integrated moving average (1,0,1) model with forecasting to 2022.
Discussion
This study provides a comprehensive characterization of NBIs occurring in military service members during the wars in Iraq and Afghanistan. Overall, we found that NBIs accounted for approximately one-third of total casualties and that this proportion was consistent and predictable.
Depending on the applied statistical method, we observed a consistent proportion of NBIs of 34% to 41% among injured service members during the conflicts. It can be assumed, given the nature of deployed tasks, that service members assigned to combat arms units are at higher risk for BIs than those who are in combat support roles, who would have higher rates of NBIs; however, all deployed service members likely have a similar risk for NBIs, implying that the exposure is the same for those in combat and those in supportive roles. We observed that in OND, the proportion of NBIs was significantly higher than that in OIF or OEF, likely reflecting military missions of sustainment, advising, and assisting Iraqi forces in security and peacekeeping as opposed to enemy engagement. This finding is not unexpected, given that the OND mission was stability operations. Rates of NBIs in OND may provide an estimation of the rates of NBIs in stability or peacekeeping missions; therefore, understanding and estimating the effect of NBIs can potentially aid operational and medical planning and inform future safety interventions.
Our analysis demonstrates that the proportion of NBIs was consistent during the period studied and that the frequency of NBIs generally decreased over time; however, the proportion of NBIs did not decrease regardless of the statistical approach used. Although battlefield mortality and injury decreased during the study period, the proportion of NBIs did not decrease below 34%. The contribution of NBI to approximately one-third of the total casualty burden and force attrition suggests a need for pre-positioned and adaptable safety measures during military operations. Our data suggest that any processes that may have been applied to decrease NBIs were ineffective. We propose that for future conflicts, rates of NBIs should be closely monitored and targeted safety interventions should be rapidly deployed. In addition, given the national focus on preventing death from trauma in military and civilian populations, preventability can be determined only with a better understanding of the cause of death. This data set and analysis are unable to provide that information but are important first steps in understanding how to potentially prevent injury from nonbattle activities, with the best preventive measure being injury prevention.
The mechanisms and types of injury are usually complex and possibly correlated with seasonality, particularly in Afghanistan, where overall casualty rates increase cyclically during the summer. Nonbattle injury trends are therefore difficult to estimate using traditional regression or weighted moving average analysis methods. This issue can be addressed with ARIMA time series analysis modeling, which is suitable for estimating future proportions of NBIs, assuming stable battlefield conditions. Using the available data from 2003 to 2014 that included all military services, we estimated the mean proportion of NBIs to be 41.0% (95% CI, 37.8%-44.3%). Injury patterns shifted from primarily combat injury to NBI in parallel with the shift from major combat operations to stability operations during OND. This suggests that the incidence of NBI is not necessarily a function of the combat environment and that active safety interventions may yield an even larger relative effect on the percentage of injuries that occur during stability operations. Implementation of strategically targeted preventive measures to decrease NBIs has the potential to unencumber the deployed health care system from preventable casualties, conserve resources for BI-associated deaths, and decrease combat zone attrition, mortality, and the cost of deployment health care.
Most of the top 10 causes of NBI may be modifiable or even preventable (Figure 3 and eTable 2 in the Supplement) given that falls account for nearly one-fourth of all NBIs (21.3%), followed by MVCs (18.8%). A total of 472 MVCs resulting in casualties significant enough to be captured in the DoDTR occurred in OEF (14.5% [472 of 3250] of all NBIs in OEF); 1423 such MVCs occurred in OIF (21.4% [1423 of 6655] of all NBIs in OIF) (eTable 2 in the Supplement). Further investigation into vehicle type, tactical situation, driver training, and proficiency may help to elucidate further preventive measures to decrease MVCs as a source of NBIs. Other possible causes of NBIs, such as machinery or equipment, blunt objects, gunshot wounds, sport, knives and sharp objects, crush, fire and flame, and any non–sports-related sprain, strain, or dislocation (altered range of motion) were also major possible causes of NBI. We suggest that these data may be useful to guide further analysis of the possible cause of injury within NBI categories, potentially leading to focused implementation of specific safety measures to help reduce NBI-related morbidity and mortality in future military operations.
Army and Marine personnel had higher absolute numbers of NBI-associated casualties but a lower proportion of NBIs compared with Navy and Air Force personnel. Because Army and Marine service members comprised most of the deployed force in this study, it is not surprising that BIs and NBIs are more numerous in these 2 branches of the armed forces. In addition, Army and Marine service members had a higher percentage of deployed personnel at risk for BIs, which may reflect occupational differences among services in these deployed operations. The proportion of NBIs was higher in the Air Force (66.3%) and Navy (48.3%) (eTable 1 in the Supplement), with the Air Force accounting for 5.3% (n = 537) and the Navy accounting for 3.9% (n = 394), of all NBIs (Table). Female service members similarly had a higher proportion of NBIs than BIs, also reflecting a population that was more likely to serve in combat support roles.
Our analysis demonstrated that 6.8% of NBIs were sports related and these proportions were higher in the Air Force (13.4% [72 of 536]) and Navy (9.6% [38 of 394]) than the Army (6.5% [500 of 7680]) and Marine Corps (5.5% [87 of 1592]). Although recreational sports activities support morale, welfare, and physical fitness while service members are deployed, sports-related injuries can potentially affect military missions. Because of the potentially preventable nature of this type of injury, preemptive measures to decrease troop attrition may be worthwhile and easy to implement.
Limitations
This study has limitations. The results should be interpreted in context with its research challenges. First, because this was a retrospective study, the accuracy of the data depends on complete and accurate documentation; this is a significant challenge in the deployed combat setting. Second, not all the injured patients were included in the DoDTR data. Before 2014, inclusion in the DoDTR required hospital admission to the R3MTF. Therefore, the DoDTR would demonstrate a selection bias for the more seriously injured, greatly understating the true size of the population with NBIs. Third, patients who died before reaching (or being admitted to) the R3MTF are not represented in the DoDTR, creating a survivorship bias. Starting in 2014, data from Role 2 medical treatment facilities were included in the data set; thus, the problem of survivorship bias may be reduced in future similar studies. Fourth, we were unable to report the incidence of NBI owing to lack of denominator data. Fifth, our data do not distinguish whether specific cases of NBI captured in the DoDTR data were preventable or modifiable. Sixth, evaluation of large data sets using numerous statistical analyses can increase the likelihood of discovering false-positive results using the conventional P value threshold of P < .05. However, a strength of the DoDTR is that data were collected prospectively by dedicated personnel on patients’ arrival to the R3MTF and validated using available medical records. In addition, statistically significant results may lack clinical significance and vice versa. Nevertheless, the objective of this analysis was to statistically characterize the features, magnitude, and outcomes of NBI in the deployed environment. Finally, there is likely an inverse association between BI and NBI that is affected by the nature and intensity of the military conflict. The proportion of NBIs reported here was derived from conflict periods featuring both large-scale combat operations and stability operations. Although the method and purpose can be replicated in future conflicts, the values for proportion of NBIs may vary depending on the nature and intensity of the conflict.
Conclusions
Approximately one-third of injuries during the Iraq and Afghanistan wars were NBIs, and the proportion of NBIs was steady for 12 years. Reductions in NBIs may require preventive measures to mitigate their identified causes. We suggest that understanding and monitoring in real time the causes, patterns, and trends of NBI in the deployed environment may be useful to guide targeted safety interventions and workforce utilization and may reduce a potentially preventable burden on the combat trauma care system during war.
eTable 1. Cumulative Incidence Rate of Battle Injury and Nonbattle Injury
eTable 2. Top 10 Possible Causes of NBI by Theater of Operation
eTable 3. ARIMA Model Fit
eFigure 1. Number of Injured Body Regions per Patient by Injury Classification
eFigure 2. Trends in Nonbattle Injury (NBI) Over Time
eFigure 3. Regression and Weighted Moving Average
eFigure 4. Trend and Correlation Analysis for Cumulative Proportion of NBI
eFigure 5. ARIMA (2,0,1) Model
References
- 1.Jones BH, Canham-Chervak M, Canada S, Mitchener TA, Moore S. Medical surveillance of injuries in the US military. Am J Prev Med. 2010;38(1)(suppl):S42-S60. [DOI] [PubMed] [Google Scholar]
- 2.Smith GS, Dannenberg AL, Amoroso PJ. Hospitalization due to injuries in the military. Am J Prev Med. 2000;18(3)(suppl):41-53. [DOI] [PubMed] [Google Scholar]
- 3.Injuries MV. the modern military epidemic. US Army Center for Health Promotion and Preventive Medicine. https://www.army.mil/article/25626/injuries_the_modern_military_epidemic. Published August 7, 2009. Accessed April 3, 2018.
- 4.Sanders JW, Putnam SD, Frankart C, et al. . Impact of illness and non-combat injury during Operations Iraqi Freedom and Enduring Freedom (Afghanistan). Am J Trop Med Hyg. 2005;73(4):713-719. [PubMed] [Google Scholar]
- 5.Eaton M, Marshall SW, Fujimoto S, Gould PL, Poole C, Richardson DB. Review of non-battle injuries in Air Force personnel deployed in support of Operation Enduring Freedom and Operation Iraqi Freedom. Mil Med. 2011;176(9):1007-1014. [DOI] [PubMed] [Google Scholar]
- 6.Withers BG, Erickson RL, Petruccelli BP, Hanson RK, Kadlec RP. Preventing disease and non-battle injury in deployed units. Mil Med. 1994;159(1):39-43. [PubMed] [Google Scholar]
- 7.Madson AQ, Tucker D, Aden J, Hale RG, Chan RK. Non-battle craniomaxillofacial injuries from U.S. military operations. J Craniomaxillofac Surg. 2013;41(8):816-820. [DOI] [PubMed] [Google Scholar]
- 8.Blood CG, Jolly R. Comparisons of disease and nonbattle injury incidence across various military operations. Mil Med. 1995;160(5):258-263. [PubMed] [Google Scholar]
- 9.Garfield RM, Neugut AI. Epidemiologic analysis of warfare. JAMA. 1991;266(5):688-692. [PubMed] [Google Scholar]
- 10.Wojcik BE, Hassell LH, Humphrey RJ, Davis JM, Oakley CJ, Stein CR. A disease and non-battle injury model based on Persian Gulf War admission rates. Am J Ind Med. 2004;45(6):549-557. [DOI] [PubMed] [Google Scholar]
- 11.Hardaway RM., III Viet Nam wound analysis. J Trauma. 1978;18(9):635-643. [DOI] [PubMed] [Google Scholar]
- 12.Writer JV, DeFraites RF, Keep LW. Non-battle injury casualties during the Persian Gulf War and other deployments. Am J Prev Med. 2000;18(3)(suppl):64-70. [DOI] [PubMed] [Google Scholar]
- 13.Writer JV, DeFraites RF, Brundage JF. Comparative mortality among US military personnel in the Persian Gulf region and worldwide during Operations Desert Shield and Desert Storm. JAMA. 1996;275(2):118-121. [PubMed] [Google Scholar]
- 14.Patel AA, Hauret KG, Taylor BJ, Jones BH. Non-battle injuries among U.S. Army soldiers deployed to Afghanistan and Iraq, 2001-2013. J Safety Res. 2017;60:29-34. [DOI] [PubMed] [Google Scholar]
- 15.Hollingsworth AC, Bowley DM, Lundy JB. The operative burden of general surgical disease and non-battle injury in a deployed military treatment facility in Afghanistan. Mil Med. 2016;181(9):1065-1068. [DOI] [PubMed] [Google Scholar]
- 16.Wilson CD. Disease and non-battle injury (DNBI) have always caused much greater morbidity. J R Army Med Corps. 2013;159(3):135. [DOI] [PubMed] [Google Scholar]
- 17.Hauret KG, Taylor BJ, Clemmons NS, Block SR, Jones BH. Frequency and causes of nonbattle injuries air evacuated from operations iraqi freedom and enduring freedom, US Army, 2001-2006. Am J Prev Med. 2010;38(1)(suppl):S94-S107. [DOI] [PubMed] [Google Scholar]
- 18.Belmont PJ Jr, Goodman GP, Waterman B, DeZee K, Burks R, Owens BD. Disease and nonbattle injuries sustained by a US Army Brigade Combat Team during Operation Iraqi Freedom. Mil Med. 2010;175(7):469-476. [DOI] [PubMed] [Google Scholar]
- 19.Kauvar DS, Cancio LC, Wolf SE, Wade CE, Holcomb JB. Comparison of combat and non-combat burns from ongoing US military operations. J Surg Res. 2006;132(2):195-200. [DOI] [PubMed] [Google Scholar]
- 20.Skeehan CD, Tribble DR, Sanders JW, Putnam SD, Armstrong AW, Riddle MS. Nonbattle injury among deployed troops. Mil Med. 2009;174(12):1256-1262. [DOI] [PubMed] [Google Scholar]
- 21.Blackbourne LH, Grathwohl K, Eastridge B, MacDonald DL, Holcomb JB. Optimizing transport of postoperative damage control patients in the combat zone. US Army Med Dep J. 2007;(Jan-Mar):11-16. [PubMed] [Google Scholar]
- 22.Eastridge BJ, Jenkins D, Flaherty S, Schiller H, Holcomb JB. Trauma system development in a theater of war. J Trauma. 2006;61(6):1366-1372. [DOI] [PubMed] [Google Scholar]
- 23.Blackbourne LH, Baer DG, Eastridge BJ, et al. . Military medical revolution [published correction appears in J Trauma Acute Care Surg. 2013;74(2):705]. J Trauma Acute Care Surg. 2012;73(6)(suppl 5):S388-S394. [DOI] [PubMed] [Google Scholar]
- 24.Le TD, Orman JA, Stockinger ZT, et al. . The Military Injury Severity Score (mISS). J Trauma Acute Care Surg. 2016;81(1):114-121. [DOI] [PubMed] [Google Scholar]
- 25.Dickey DA, Fuller WA. Distribution of the estimators for autoregressive time series with a unit root. J Am Stat Assoc. 1979;74(366):427-431. doi: 10.2307/2286348 [DOI] [Google Scholar]
- 26.Ljung GM, Box GEP. On a measure of lack of fit in time series models. Biometrika. 1978;65(2):297-303. doi: 10.2307/2335207 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Cumulative Incidence Rate of Battle Injury and Nonbattle Injury
eTable 2. Top 10 Possible Causes of NBI by Theater of Operation
eTable 3. ARIMA Model Fit
eFigure 1. Number of Injured Body Regions per Patient by Injury Classification
eFigure 2. Trends in Nonbattle Injury (NBI) Over Time
eFigure 3. Regression and Weighted Moving Average
eFigure 4. Trend and Correlation Analysis for Cumulative Proportion of NBI
eFigure 5. ARIMA (2,0,1) Model