Abstract
Background/Objective:
The likelihood that an older person will sustain an injury increases as the number of falls increase, but it is unknown whether or how the risk of an injury from a specific fall varies as the number of falls increase. Our objective was to evaluate the relationship between the number of falls and risk of injury after a specific fall.
Design:
Prospective cohort study.
Setting:
Greater New Haven, Connecticut.
Participants:
Probability sample of 1103 community-living persons aged 72 years or older.
Measurements:
Falls and fall-related injuries were ascertained monthly for 3 years using a fall calendar and follow-up telephone interviews.
Results:
Of the 606 participants with a fall, 164 (27.0%) had at least 1 fall with a serious injury, while 455 (75.1%) had at least 1 fall with any injury; and the mean (SD; range) number of falls, falls with serious injury, and falls with any injury were 2.6 (2.3; 1-18), 0.3 (0.6; 0-4), and 1.4 (1.4; 0-9), respectively. On a per participant basis, the risk of a serious injury and any injury increased progressively as the number of falls increased (P<.001). On a per fall basis, the risk of a serious injury and any injury increased from 1 to 2 falls, but then decreased from 2 to 3-4 falls and from 3-4 to ≥ 5 falls, although these differences were not statistically significant. The results were consistent for women and men and for analyses that evaluated the proportion of falls with injuries.
Conclusion:
Among community-living older persons, the risk of injury from a specific fall did not differ as the number of falls increased. Falls appear to operate independently in terms of conferring risk for an injury in the setting of multiple falls.
Keywords: longitudinal study, older persons, falls, injuries
Falls are common and potentially morbid events in the lives of older persons. Each year, about 30% of community-living older persons fall, and 20-30% of those who fall suffer moderate to severe injuries.1–5 Among persons ≥65 years, falls are the leading cause of fatal and nonfatal injuries.6 Fall injuries are independently associated with subsequent disability in important activities, such as bathing and shopping, and with increased risk of long-term nursing home admissions.7, 8
Falls are not independent events.5, 9 After a first fall, the likelihood of having another fall within a year is 66%.10 However, whether fall-related injuries are independent events is uncertain. A noninjurious fall may make one more vulnerable to an injury after a subsequent fall, perhaps through a decline in fall-related efficacy or an increase in fear of falling.11, 12 Alternatively, older persons who fall frequently may learn how to fall more safely, reducing the likelihood of an injury after a subsequent fall.
The objective of the current study was to determine whether the risk of injury from a specific fall varies as the number of falls increase. Because women are more likely to be injured after a fall than men,2, 4 we also evaluated potential sex differences. We used high quality data from a large population-based study of older men and women with nearly complete ascertainment of falls and injuries over a 3-year period. Elucidating the relationship between the number of falls and risk of injury after a specific fall may help to inform the care of older persons who sustain multiple falls.
METHODS
Study Population
Participants were members of Project Safety, a probability sample of community-living persons, ≥72 years, living in New Haven, Connecticut in 1989.13 Among those eligible, 1,103 (79%) agreed to participate and were enrolled in the cohort. Enrollees did not differ significantly from those who declined to participate in terms of age, sex, or percent living in senior housing.4
Data Collection
Baseline assessments were completed in participants’ homes by trained research nurses using standard instruments.13 Clinical data included self-reported, physician-diagnosed chronic conditions, such as myocardial infarction, stroke, arthritis, diabetes mellitus, cancer, Parkinson’s disease, and previous fractures. Body-mass index was calculated based on information provided by participants. Cognitive status was assessed with the Mini-Mental State Examination (MMSE).14
Ascertainment of falls and injuries
Falls were ascertained each month for 3 years using a “fall calendar”, which was completed by participants daily and then mailed back to the project office at the end of the month.4 Participants were contacted by telephone if the calendars were not returned or if a fall was recorded. Proxies were contacted if participants seemed confused or could not be reached after 5 attempts. The completion rate for the fall calendars and/or telephone contacts was 99%. During the follow-up telephone interview, participants were asked about any falls (injurious and noninjurious) that occurred during the previous month. Serious injuries included fractures and joint dislocations; head injuries resulting in the loss of consciousness and hospitalization; joint injuries, other than dislocations, that resulted in hospitalization or decreased activity; and internal injuries resulting in hospitalization. These injuries were confirmed from a combination of hospital records, emergency department records, and participants’ reports using a previously described algorithm.4 The other participant-reported injuries were considered as non-serious.
Statistical Analysis
Baseline characteristics were compared between participants who had ≥1 falls versus no falls during follow-up and subsequently between women and men who had ≥1 falls. Among participants with a fall, the proportion of falls with a serious injury and any injury (serious and non-serious) and mean number of fall-related serious injuries and any injuries were estimated.
Our analytic plan was designed to address 4 distinct but related questions: (1) are persons who experience more falls more (or less) likely to experience at least one (serious) injury? (2) are persons who experience more falls more (or less) likely to experience a (serious) injury for each fall? (3) do persons who fall more have a larger (or smaller) number of (serious) injuries? and (4) is the proportion of falls that result in (serious) injury higher (or lower) for persons who fall more?
The risk of serious injury and any injury were estimated per participant (question 1) and per fall (question 2), respectively, by number of falls per participant (1, 2, 3-4, ≥5) and subsequently compared using binomial regression analysis, with participants having 1 fall serving as the reference group. For the per-fall analysis, generalized estimating equations applied to binomial regressions were used to account for the lack of independence of falls within participants. A similar analysis was performed on a per participant basis for number (question 3) and proportion (question 4) of falls with injuries by number of falls per participant except that linear regression was used, with participants having 1 fall serving as the reference group.
The analyses for risk of injury and for number and proportion of falls with injuries were repeated separately for women and men, and potential sex differences were evaluated through tests of statistical interaction. Because sample sizes were smaller, the number of falls per participant were categorized into 3 groups (1, 2, ≥3) instead of 4.
All analyses were performed using SAS 9.4.
RESULTS
The baseline characteristics of the study participants are provided in Table 1. Compared with those who had no falls, participants who had ≥1 falls during follow-up were older and had more chronic conditions and lower MMSE scores. Of the 606 participants with a fall, 164 (27.0%) had at least 1 fall with serious injury, while 455 (75.1%) had at least 1 fall with any injury; and the mean (SD; range) number of falls, falls with serious injury, and falls with any injury were 2.6 (2.3; 1-18), 0.3 (0.6; 0-4), and 1.4 (1.4; 0-9), respectively. Of the 1,553 falls, 206 (13.2%) resulted in serious injury, and 870 (56.0%) resulted in any injury.
Table 1.
Baseline Characteristics of Study Participants According to Falls During Follow-up
| Characteristic | All Participants N=1103 | One or more Falls N=606 | No Falls N=497 | P-value a |
|---|---|---|---|---|
| Age in years, mean (SD) | 79.6 (5.3) | 80.5 (5.6) | 78.5 (4.6) | <.001 |
| Female sex, n (%) | 804 (72.9) | 444 (73.3) | 360 (60.3) | .757 |
| Non-Hispanic white, n (%) | 926 (84.0) | 506 (83.5) | 420 (84.5) | .650 |
| Living alone, n (%) | 759 (68.8) | 432 (71.3) | 327 (65.8) | .050 |
| Education in years, mean (SD) | 9.6 (3.6) | 9.6 (3.7) | 9.5 (3.5) | .551 |
| Body-mass index (kg/m2), mean (SD) | 24.8 (4.6) | 24.8 (4.8) | 24.8 (4.3) | .961 |
| Number of chronic conditions, mean (SD) b | 1.3 (1.0) | 1.4 (1.0) | 1.2 (1.0) | <.001 |
| MMSE score, mean (SD) | 24.5 (4.4) | 24.1 (4.8) | 25.0 (3.7) | <.001 |
Abbreviation: SD, standard deviation; MMSE, Mini-Mental State Examination
The chi-square test was used for dichotomous variables, and t-test was used for continuous variables.
Includes myocardial infarction, stroke, arthritis, diabetes mellitus, cancer, Parkinson’s disease, and previous fractures.
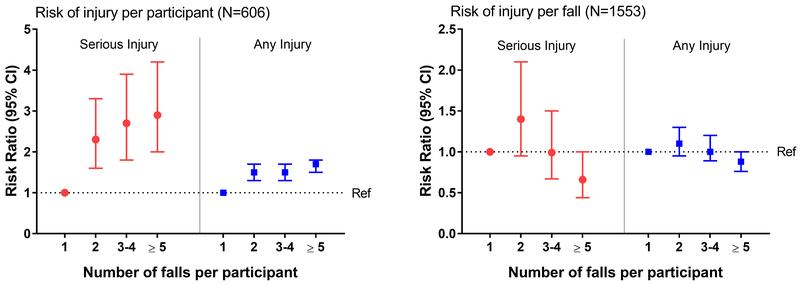
Figure 1 provides the risk of injury per participant and per fall by number of falls per participant. On a per participant basis, the risk of serious injury and any injury increased progressively as the number of falls increased (P<.001), but these increases were not linear. For each type of injury, the greatest increase occurred from 1 to 2 falls, although each of the risk ratios was statistically significant. On a per fall basis, the risk of serious injury and any injury increased from 1 to 2 falls, but then decreased from 2 to 3-4 falls and from 3-4 to ≥ 5 falls. Although none of the risk ratios were statistically significant, the overall associations between number of falls and risk of injury were statistically significant, with P-values of .005 and .026 for serious injury and any injury, respectively.
Figure 1.
Risk of injury per participant and per fall by number of falls per participant. For risk of injury per participant, the risk of serious injury and any injury increased progressively as the number of falls increased (P<.001). For risk of injury per fall, the overall associations between number of falls and risk of injury were statistically significant, with P-values of .005 and .026 for serious injury and any injury, respectively. Ref: reference group.
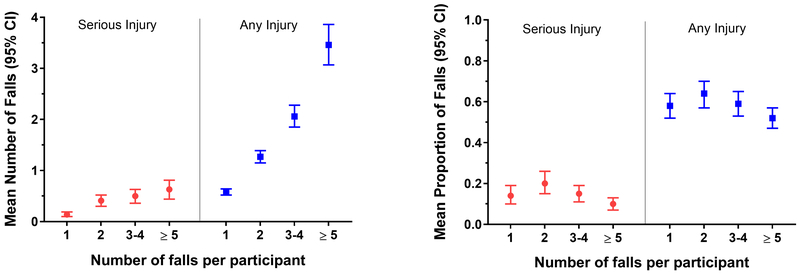
Figure 2 provides the number and proportion of falls with injuries on a per participant basis by number of falls per participant. As shown in the left panel, the mean number of falls with serious injuries and any injuries increased progressively as number of falls increased (P<.001), and each of the mean values differed statistically (P<.001) from that of the reference group (1 fall). As shown in the right panel, the mean proportion of falls with serious injuries and any injuries increased slightly from 1 to 2 falls, but then decreased slightly from 2 to 3-4 falls and from 3-4 to ≥ 5 falls. Neither the overall test for association nor any of the pairwise comparisons (with the reference group [1 fall]) were statistically significant.
Figure 2.
Number and proportion of falls with injuries per participant by number of falls per participant. The mean number of falls with serious injuries and any injuries increased progressively as number of falls increased (P<.001), and each of the mean values differed statistically (P<.001) from that of the reference group (1 fall). For mean proportion of falls, neither the overall test for association nor any of the pairwise comparisons (with the reference group [1 fall]) were statistically significant.
Of the 804 women, 444 (55.2%) had 1,166 falls, with 170 (14.6%) resulting in serious injury and 674 (57.8%) in any injury. Of the 299 men, 162 (54.2%) had 387 falls, with 36 (9.3%) resulting in serious injury and 196 (50.6%) in any injury. The baseline characteristics of women and men who had ≥1 falls during follow-up are provided in Supplementary Table S1. Compared with men, women were more likely to live alone and had a greater number of chronic conditions.
As shown in Supplementary Table S2, the results for risk of fall with injury per participant and per fall by number of falls per participant were generally comparable for women and men. Specifically, the relationship between number of falls per participant and risk of serious injury and any injury, respectively, did not differ between women and men, with P-values for interaction of .239 and .376 for the per participant results and .364 and .238 for the per fall results.
As shown in Supplementary Table S3, the relationship between number of falls per participant and number and proportion of falls with injuries on a per participant basis did not differ between women and men, with P-values for interaction of .541 and .292 for the number of falls results and .302 and .194 for the proportion of falls results.
DISCUSSION
In this prospective longitudinal study of community-living older persons, we confirmed that the risk and mean number of fall-related injuries increase progressively as the number of falls increase.2 In contrast, we found no evidence that the risk of injury from a specific fall or the proportion of falls with injuries differs as the number of falls increase. These findings were observed for serious injuries and any injuries and for women and men. Overall, our findings suggest that falls may operate independently in terms of conferring risk for an injury in the setting of multiple falls.
We found that the risk of injury from a specific fall increased modestly from 1 fall to 2 falls but decreased modestly for those with more falls, although these differences were not statistically significant. Comparable results were observed for the proportion of falls with injuries. Power was limited, however, to detect statistically significant reductions in the risk of injury for participants with 5 or more falls since they represented only about 8% of the study cohort.
The results of the current study are generally consistent with those of a prior study that followed 325 community-living persons aged 60 years or older with weekly ascertainment of falls and injuries for 1 year.2 Based on the results of these 2 studies, there is little evidence to support the notions that older persons who fall frequently learn how to fall more safely, thereby diminishing their risk of injury with each subsequent fall, or that multiple falls greatly increase vulnerability, thereby leading to an escalating risk of injury. Because the likelihood of sustaining an injury increases the more one falls, it may be prudent from a clinical and policy perspective to invest a disproportionate amount of fall prevention resources in older persons who fall most frequently, with the caveat that the benefit of preventing a first fall is likely as great as preventing subsequent falls in terms of reducing injuries.
Our study has many strengths. First, our study population was large and included a representative sample of community-living older persons. Second, with a mean age of nearly 80 years, our participants represented persons at highest risk of falls and injuries. Third, falls and injuries were ascertained monthly over a 3-year period with little loss to follow-up and a completion rate of nearly 100%.13 Fourth, our results were consistent for serious injuries and any injuries, for women and men, and for analyses that evaluated the risk of injury from a specific fall and the proportion of falls with injuries.
Our study also has several limitations. First, despite the large sample size, long duration of follow-up and nearly complete ascertainment of falls and injuries, power was limited, especially for the sex-specific analyses. Given the observed point estimates and relatively narrow confidence intervals, it is unlikely that the lack of association between number of falls and risk of fall injury on a per fall basis was due to low power. Second, because the data from this study are nearly 30 years old, they cannot account for secular changes in the risk, detection, evaluation and management of fall-related injuries in older persons. Although there is no reason to believe that the associations of interest change over time, our results should be confirmed using data from more contemporary studies. Third, information was not available on changes in physical activity, receipt of interventions, or exposure to other factors that may have altered vulnerability or opportunities for falls and fall-related injuries over the 3-year follow-up period. Finally, to reduce complexity, the analyses were restricted to only 1 injury per fall.
In summary, we found no evidence that the risk of injury from a specific fall differs as the number of falls increase. Among community-living older persons, falls appear to operate independently in terms of conferring risk for an injury in the setting of multiple falls.
Supplementary Material
Supplementary Table S1. Baseline Characteristics of Women and Men Who Had One or More Falls during Follow-up
Supplementary Table S2. Risk of Fall with Injury per Participant and per Fall by Number of Falls per Participant for Women and Men
Supplementary Table S3. Number and Proportion of Falls with Injuries per Participant by Number of Falls per Participant for Women and Men
ACKNOWLEDGMENTS
We thank Linda Leo-Summers, MPH, for creating the figures and Mary Tinetti, MD, the principal investigator of the parent study, for sharing the data.
The study was conducted at the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Gill is the recipient of an Academic Leadership Award (K07AG043587) from the National Institute on Aging.
Sponsor’s Role:
The sponsor had no role in the design or conduct of the study; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
We certify that this work is novel: the study shows that falls may operate independently in terms of conferring risk for an injury in the setting of multiple falls.
Conflicts of Interest:
The authors have no conflicts of interest.
REFERENCES
- 1.O’Loughlin JL, Robitaille Y, Boivin JF et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 1993;137:342–354. [DOI] [PubMed] [Google Scholar]
- 2.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol 1991;46:M164–M170. [DOI] [PubMed] [Google Scholar]
- 3.Sattin RW, Lambert Huber DA, DeVito CA et al. The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol 1990;131:1028–1037. [DOI] [PubMed] [Google Scholar]
- 4.Tinetti ME, Doucette J, Claus E et al. Risk factors for serious injury during falls by older persons in the community. J Am Geriatr Soc 1995;43:1214–1221. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). Self-reported falls and fall-related injuries among persons aged ≥ 65 years--United States, 2006. MMWR Morb Mortal Wkly Rep 2008;57:225–229. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Web–based Injury Statistics Query and Reporting System (WISQARS). http://www.cdc.gov/injury/wisqars/. Accessed April 12, 2018.
- 7.Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol Med Sci 1998;53A:M112–M119. [DOI] [PubMed] [Google Scholar]
- 8.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 1997;337:1279–1284. [DOI] [PubMed] [Google Scholar]
- 9.Close JC, Wesson J, Sherrington C et al. Can a tailored exercise and home hazard reduction program reduce the rate of falls in community dwelling older people with cognitive impairment: protocol paper for the i-FOCIS randomised controlled trial. BMC Geriatr 2014;14:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nevitt MC, Cummings SR, Kidd S et al. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 1989;261:2663–2668. [PubMed] [Google Scholar]
- 11.Tinetti ME, Mendes de Leon CF, Doucette JT et al. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol Med Sci 1994;49:M140–M147. [DOI] [PubMed] [Google Scholar]
- 12.Parry SW, Finch T, Deary V. How should we manage fear of falling in older adults living in the community? BMJ 2013;346:f2933. [DOI] [PubMed] [Google Scholar]
- 13.Tinetti ME, Liu WL, Claus EB. Predictors and prognosis of inability to get up after falls among elderly persons. JAMA 1993;269:65–70. [PubMed] [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Baseline Characteristics of Women and Men Who Had One or More Falls during Follow-up
Supplementary Table S2. Risk of Fall with Injury per Participant and per Fall by Number of Falls per Participant for Women and Men
Supplementary Table S3. Number and Proportion of Falls with Injuries per Participant by Number of Falls per Participant for Women and Men