Abstract
Cognitive workload data of members of the cardiac surgery team can be measured intraoperatively and stored for later analysis. We present a case of a near-miss (medication error) that underwent root cause analysis using workload data. Heart rate variability data, representing workload levels, were collected from the attending surgeon, attending anesthesiologist, and lead perfusionist using wireless heart rate monitors. An episode of cognitive overload of the anesthesiologist due to a distractor was associated with the preventable error. Additional studies are needed to better understand the role of psychophysiological data in enhancing surgical patient safety.
Keywords: Cognitive workload, root cause analysis, cardiac surgery, team workload, heart rate variability
Graphical Abstract
Central Picture Legend: Cognitive task analysis of CABG
Central Message: Team cognitive workload data may be useful in supplementing traditional root causeanalysis
Perspective Statement
Limitations of root cause analysis are leading to introduction of innovative approachesto enhance learning.
Introduction
The concept of mental workload (MWL) is multidimensional—encompassing cognitive workload, mental strain, and mental effort—and captures the overall load imposed by performing a specific task on the operator [1]. Recent advances in cognitive sciences are being leveraged to assess in real-time dynamic changes in MWL of surgeons and other team members [2]. When MWL is excessive, a state of cognitive overload ensues with associated performance degradation and errors [3, 4, 5]. The aim of this manuscript is to illustrate an example of how MWL data may be incorporated into root cause analysis of clinical incidents to enhance the understanding of the human factors that affect surgical quality and safety.
Root cause analysis of a cardiac surgery near-miss
(i). Clinical case
A patient with multivessel coronary artery disease not amenable to percutaneous coronary intervention underwent a three-vessel coronary-artery bypass surgery (CABG) using cardiopulmonary bypass and cardioplegic arrest. Upon successful weaning from cardiopulmonary bypass, the leader of the surgical team asked the anesthesia team for administration of protamine for heparin reversal. The junior anesthesia resident, working under the cardiac anesthesia attending who was present in the room, administered the entire dose of protamine as a single intravenous push. The sudden reversal of heparin with a bolus of protamine required a quick response from the three team principals from cardiac surgery, anesthesiology and perfusion aimed at: (a) minimizing the risk of thrombosis of the arterial cannula still inside the aorta by its rapid removal; (b) considering the potential need for return on cardiopulmonary bypass following repeat heparinization in case of refractory vasoplegic shock; (c) need for quick repeat cannulation of the aorta and right atrium and (d) need to make adequate pharmacologic resources available (e.g. epinephrine, ephedrine, methylene blue) to counter protamine reaction and provide inotropic support, according to our own crisis checklist protocol [5]. Fortunately, no protamine reaction was observed and the patient was discharged home on postoperative day 5 without complications.
(ii). Root cause analysis
Root cause analysis is a systematic approach to identifying errors in workflow (including near-misses) and is relied on extensively for quality improvement in healthcare [6]; additionally, it is intended to generate solutions to prevent similar errors from occurring in the future [7]. During root cause analysis of our near miss case, the anesthesia resident that administered the bolus of protamine stated that she was not aware of the best practice for protamine administration, including test dose and slow infusion over several minutes. The anesthesia teaching faculty staffing the case was also managing the overall flow of cases for the entire operating room and, immediately prior to the protamine administration error, had been involved in a stressful argument with operating room staff on case flow and scheduling priorities.
(iii). Mental workload data
The root case analysis used data on physiological metrics of MWL (Heart Rate Variability – HRV) that was being recorded for the case as part of a NIH-funded research study [8]. HRV analysis is the most frequently utilized real-time physiological measure of surgeons’ intraoperative cognitive workload [2]. HRV data were collected from three team members—attending surgeon, attending anesthesiologist, and lead perfusionist—during the course of the surgery. Each team member was equipped with a wireless heart rate monitor (Polar H10 sensors, Polar Electro Inc., Finland) that transmitted data via Bluetooth to a Polar V800 watch. Heart rate data was archived for subsequent data analysis; none of the team members had access to these data in real-time. Although the team members were equipped with heart rate monitors, they were otherwise unaware of their own MWL state because this information was not being fed back to them in any way during the case. Of all HRV components, the low frequency / high frequency (LF/HF) ratio has been used extensively as an indicator of sympathovagal balance, and higher values are reflective of higher states of MWL [9,10].
Results and Discussion
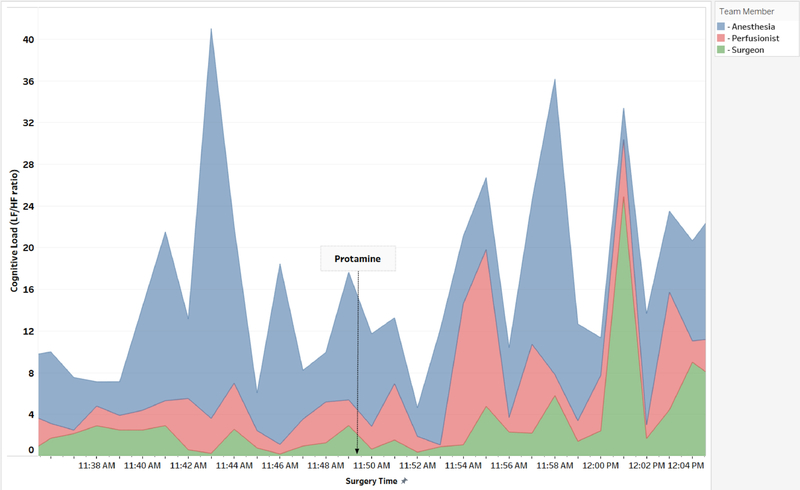
Figure 1 demonstrates the changes in HRV of the anesthesia attending, surgical attending and lead perfusionist throughout the case. Prior to the error, an isolated cognitive overload state can be observed (HRV LF/HF ratio of 37; normal is <2.5) for the anesthesiologist correlating with the subjective emotions (frustration/anger) resulting from the argument with operating room staff. Following the error, around the time stamp of 12:01, the cognitive workload of all three team members rises synchronously following the announcement of premature completion of the protamine administration by the trainee. The synchronous mirroring observed at this time could be indicative of team cohesion and strategy shift, absent elsewhere in the case when a mutual awareness may not have been present.
Figure 1:
Dynamic changes in the low frequency / high frequency ratio heart rate variability measurement of the anesthesia attending (blue), surgical attending (green) and lead perfusionist (red) throughout the case. Prior to the error (labelled ―Protamine‖), an isolated cognitive overload state can be observed (HRV LF/HF ratio of 37; normal is <2.5) for the anesthesiologist. Following the error, the cognitive workload of all three team members rises synchronously.
Conclusions
The conflicting demands on the attention of the teaching anesthesiologist and the high emotions (frustration and anger) caused a temporary cognitive overload state which interfered with the completion of resident teaching and was a factor in the preventable medication error. The high teaching demands of this case, where a novice cardiac anesthesia resident was being mentored through the first cardiac case, should have taken precedence over conflicting demands of flow management in the operating room, which acted as a disrupting distraction. While this error could be easily dismissed as due to the resident’s lack of experience and the attending’s lack of teaching, employing root cause analysis by incorporating a reliable physiological indicator of cognitive workload illustrates that the latter—lack of teaching on the part of the attending—is attributable to a temporarily ineffective mental state. The attending anesthesiologist would have been better equipped to take on the demands of teaching the novice resident were it not for the mental overload experienced as a result of prior high emotions and poor situation and plan awareness [11].
To the best of our knowledge, this is the first report of a root cause analysis that used cognitive workload data as a tool to offer an explanation towards ―why‖ the near-miss occurred. Despite the retrospective nature of root cause analysis relying on HRV data, this case illustrates a powerful potential debriefing tool to bring awareness and stimulate conversation among team members. Additionally, utilizing this approach in real time could introduce error detection and resolution opportunities.
While surgical teams do not currently have access to heart rate monitors and workload information according to current routine practice, collecting these data in the operating room represents a passive and non-invasive process. Real-time awareness of cognitive load, indicated by HRV measures, could be useful in determining the appropriate time to intervene during task flow with low risk of disruption [12]. In this specific case, monitoring the attending anesthesiologists’ cognitive load in real time could have indicated a state of cognitive overload, and initiated coping strategies to regulate that state prior to moving on to protamine administration. Doing so may have enabled the attending anesthesiologist to devote appropriate cognitive resources to mentoring and teaching the novice anesthesia resident, and thereby prevented this near-miss event entirely.
In the event that future research corroborates the relevancy and utility of incorporating such technology, this method could be adopted into routine care readily. Overall this case illustrates the potential usefulness of cognitive datasets for improvement of patient safety. Future work should incorporate additional HRV and psychophysiological measures and evaluate real-time solutions based on cognitive state.
Disclosure
The case recording was approved by the local Institutional Review Board (IRB). All involved research subjects signed an IRB-approved informed consent form. Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number R01HL126896. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the AATS Surgical Patient Safety Course 2018, June 29–30, 2018 Renaissance Boston Waterfront Hotel, Boston, MA
References
- 1.Patel VL, Kannampallil TG, Shortliffe EH. Role of Cognition in Generating and Mitigating Errors. BMJ Qual Saf 2015;24:468–474 [DOI] [PubMed] [Google Scholar]
- 2.Dias RD, Ngo-Howard MC, Boskowski MT, Zenati MA, Yule SJ. Systematic Review of Measurement Tools to Assess Surgeons’ Intraoperative Cognitive Workload. Br J Surg 2018;105(5):491–501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yerkes RM, Dodson JD. The Relation of Strength of Stimulus to Rapidity of Habit Formation. J Comp Neurol Psychol 1908;18:459–482. [Google Scholar]
- 4.Grantcharov PD, Boillat T, Elkabant S, Rivas H. Acute Mental Stress and Surgical Performance. BJS Open 2018. DOI: 10.1002/bjs5.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tarola CL, Hirji S, Yule SJ, Gabany JM, Zenati A, Dias RD, Zenati MA. Cognitive Support to Promote Shared Mental Models during Safety-Critical Situations in Cardiac Surgery. Proceedings, 2018 IEEE Conference on Cognitive and Computational Aspects of Situation Management (CogSIMA), June 12–14, 2018, Boston, MA, pp. 83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu AW, Lipshutz AKM, Pronovost PJ. Effectiveness and Efficiency of Root Cause Analysis in Medicine. JAMA 2008; 299: 685–687. [DOI] [PubMed] [Google Scholar]
- 7.Kellogg KM, Hettinger Z, Shah M, et al. Our current approach to root cause analysis: is it contributing to our failure to improve patient safety? BMJ Qual Saf 2017; 26: 381–387. [DOI] [PubMed] [Google Scholar]
- 8.Dias RD, Conboy HM, Gabany JM, Clarke LA, Osterweil LJ, Avrunin GS, Arney D, Goldman JM, Riccardi G, Yule SJ, Zenati MA. Development of an Interactive Dashboard to Analyze Cognitive Workload of Surgical Teams During Complex Procedural Care. Proceedings, 2018 IEEE Conference on Cognitive and Computational Aspects of Situation Management (CogSIMA), June 12–14, 2018, Boston, MA, pp. 77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rowe DW, Sibert J, Irwin D. Heart rate variability: indicator of user state as an aid to human-computer interaction. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems April 1998:18–23 DOI: 10.1145/274644.274709. [DOI] [Google Scholar]
- 10.Castaldo R, Melillo P, Bracale U, et al. Acute mental stress assessment via short term HRV analysis in healthy adults: A systematic review with meta-analysis. Biomed Signal Process Control 2015; 18: 370–377. [Google Scholar]
- 11.Endsley MR. Toward a Theory of Situation Awareness in Dynamic Systems. Hum Factors 1995;37:32–64 [Google Scholar]
- 12.Dias RD, Conboy HM, Gabany JM, et al. Intelligent Interruption Management System to Enhance Safety and Performance in Complex Surgical and Robotic Procedures In: Stoyanov D et al. (eds) OR 2.0 Context-Aware Operating Theaters, Computer Assisted Robotic Endoscopy, Clinical Image-Based Procedures, and Skin Image Analysis. CARE 2018, CLIP 2018, OR 2.0 2018, ISIC 2018. Lecture Notes in Computer Science, vol 11041 Springer; DOI: 10.1007/978-3-030-01201-4 [DOI] [PMC free article] [PubMed] [Google Scholar]