Abstract
Objective:
To compare the longitudinal course of family functioning in offspring of parents with bipolar disorder (BD), offspring of parents with non-BD psychopathology, and offspring of healthy control parents (HC).
Method:
Offspring of BD parents (256 parents and 481 offspring), non-BD parents (82 parents and 162 offspring) and HC parents (88 parents and 175 offspring) ages 7–18 at intake, from the Bipolar Offspring Study (BIOS), were followed for an average of 4.3 years. Family functioning was evaluated using the child- and parent-reported Family Adaptability and Cohesion Scale-II (FACES II) and the Conflict Behavior Questionnaire (CBQ). The data was analyzed using multivariate multilevel regression, generalized linear estimating equation models, and path analysis.
Results:
Families of BD parents and parents with non-BD psychopathology showed lower cohesion and adaptability and higher conflict as compared with HC families. There were no significant differences in cohesion and adaptability between the families of parents with psychopathology. The effect of parental psychopathology on family functioning was mediated by parental psychosocial functioning, and to a lesser extent, offspring disorders. In all three groups, parent-reported family conflict was significantly higher than child-reported conflict. Across groups, family cohesion decreased over follow-up, whereas conflict increased.
Conclusion:
Any parental psychopathology predicted family impairment. These results were influenced by the offspring’s age and were mediated by parental psychosocial functioning, and to a lesser degree, by offspring psychopathology. These findings emphasize the need to routinely assess family functioning in addition to psychopathology and provide appropriate interventions to both parents and offspring.
Keywords: bipolar disorder, family functioning, family conflict, longitudinal study
Introduction:
Bipolar Disorder (BD) is a recurrent illness that affects 1–3% of youth and is associated with significant negative psychosocial consequences and increased risk for legal problems, substance abuse, and suicidal behaviors1,2. The family environment plays a critical role throughout development—both as a risk and protective factor 3, and family distress can both exacerbate and result from BD symptoms4. The study of family functioning in youth at high familial risk for BD is crucial to inform assessment and preventive interventions for these populations5.
To our knowledge, there are 16 studies in youth with BD and 6 studies in youth with BD-parents; most are cross-sectional and assess family functioning from the perspective of either the parent or the offspring. The studies that focused on families of youth with BD have mostly found higher levels of conflict and expressed emotion (EE: critical, hostile, or emotionally over-involved attitudes) and lower cohesion (emotional bonding) and adaptability (the family’s ability to modify its structure, relationships and rules in response to circumstances) when compared to HC 6,7. However, extant studies have not found differences in family functioning between youth with BD and youth with non-BD psychopathology (e.g., major depression or behavioral disorders) 8, raising the question of whether families of youth with BD are characterized by distinct patterns of family impairment, or whether such impairment is associated with psychopathology more generally.
To date, only 3 studies have evaluated family functioning longitudinally in BD youth 9–11. These studies showed poorer mood outcome over 2 years among youth whose families reported higher conflict at baseline9,11. BD youth in families with high levels of EE demonstrated greater mood improvement in Family Focused Therapy (FFT) than those with high levels of EE who received a comparison intervention 10. In one of these studies, cohesion, adaptability and conflict were significantly correlated with depression scores among BD adolescents11.
Six cross-sectional studies focus on the family functioning of BD parents (see Table S1, available online). Most report higher conflict and lower cohesion in families with a BD parent, particularly when the offspring also had psychopathology 12. No studies compare the family functioning of parents with BD to parents with non-BD psychopathology.
Research on family functioning in adults with BD indicates that: worse family functioning is associated with more past suicide attempts; 13 manic episodes are temporally associated with poorer family functioning than depressive episodes; 14 and improvement in mood symptoms is correlated with better family functioning 15. In sum, longitudinal studies in adults show that family functioning is associated with clinical course, predicting both severity and relapse risk.16–18
Limitations in the studies conducted to date include that they were largely cross-sectional and included small samples; did not always include control groups, or only included control groups of HC subjects. Few evaluated the ratings of both parents and youth regarding family functioning, and did not always consider the effects of confounding variables (e.g. parents’ psychopathology, socio-economic status). Finally, longitudinal studies were of brief duration, in the context of treatment studies, and rarely blind to child and parental diagnosis.
The Pittsburgh Bipolar Offspring Study (BIOS) is an ongoing longitudinal study, currently in its 17th year, of offspring of parents with BD (n=388) and community controls (n=250). Our prior publications show that offspring of parents with BP are at high risk to develop unipolar depression, anxiety disorders, behavior problems, suicidal ideation, substance abuse and early-onset BD spectrum disorders2,19. The goal of the current study is to longitudinally compare family functioning among the offspring of parents with BD, offspring of parents with non-BD psychopathology and offspring of HC parents. All measures are assessed separately from the perspective of both offspring and parent.
First, we hypothesized (Hypothesis 1) that families of parents with BD, particularly those in which the offspring have psychopathology, will show higher conflict, lower cohesion and lower adaptability than HC parents. Because we believe that these family functioning indices reflect global familial impairment associated with parental psychopathology, we expect that (Hypothesis 2) families with a parent with BD and families with a parent with non-BD psychopathology will both have impaired family functioning compared to the healthy control group, however they will not differ from one another. Third (Hypothesis 3), we hypothesized that psychosocial functioning and presence of psychopathology in both offspring and parents will predict family functioning. Finally, given that epidemiological studies indicate family conflict tends to increase and family cohesion decrease throughout adolescent development20,21, we hypothesize that (Hypothesis 4) levels of these variables will change over follow-up.
Method:
The methods employed in BIOS are described in detail in prior publications 2. Briefly, BIOS recruited 481 offspring of 256 parents with Diagnostic and Statistical Manual, Version-IV (DSM-IV) BDI or BDII and 337 offspring of 170 community control parents. For the present analyses, we examined two subgroups of the control group: 1. offspring (n=162) of parents (n=82) with non-BD psychopathology, 2. Offspring (n=175) of psychiatrically healthy parents (n=88) (HC). Offspring enrolled between ages 7–18 years were included in these analyses. Subjects were assessed every 2.1 years on average and had a median of 3.0 assessments with 4.3 years of follow-up. The overall retention rate for the study through the last follow-up assessment included in these analyses is 94%. Parents with BD were recruited through advertisements (53%), adult BD research studies (31%), and outpatient clinics (16%). Control parents were ascertained by random-digit dialing and were group matched for age, sex and neighborhood to the parents with BD.
Parents and offspring consented for their participation. Exclusion criteria for parents included current or lifetime diagnoses of schizophrenia or intellectual disability; mood disorders secondary to substance abuse, medical conditions that interfered with study participation; and living more than 200 miles from Pittsburgh. Exclusion criteria for the control group were the same, with the additional criterion that neither biological parent had BD or a first-degree relative with BD. All offspring of each eligible parent between the ages 7–18 were included unless they were deemed unable to complete the assessments (e.g., intellectual disability).
Instruments:
Parents and participating biological co-parents (34%) were assessed by direct interview using the Structured Clinical Interview for DSM-IV22. The psychiatric history of non-participating co-parents was obtained from the participating parent using the Family-History Research Diagnostic Criteria23.
To establish the child’s diagnosis at baseline and follow-up visits, parents and offspring were interviewed using the Schedule for Affective Disorders and Schizophrenia for School Age Children-Present and Lifetime Version (K-SADS P/L) for non-mood disorders and the K-SADS Mania Rating Scale and the depression items from the KSADS-Present Version, which assess symptoms during the worst week over the past month 24,25. K-SADS symptom ratings and diagnoses were based on consensus ratings incorporating all available data. Assessments were conducted by trained interviewers, and reviewed by a child psychiatrist. Interviewers and psychiatrists were blind to parental diagnoses.
The κ statistic for inter-rater reliability, conducted by having all raters review and independently rate audio-recorded interviews, was 0.86 for BD-spectrum disorders (presence/absence of any BD spectrum disorder), 0.77 for BD-I/II vs. BD not otherwise specified vs. no BD, 0.64 for major depressive episode, 0.71 for any depressive episode, 0.86 for attention-deficit hyperactivity disorder, 0.78 for anxiety disorders, 0.84 for oppositional defiant disorder and/or conduct disorder, and 1.0 for substance use disorders.
Parents and offspring completed self- and parent-report scales of psychopathology and functioning at each follow-up assessment. Socioeconomic status was determined using the Hollingshead scale 26. We used the Children’s Global Assessment Scale (CGAS) as a basic quantification of functioning at home and school for offspring and the Global Assessment of Functioning (GAF) to rate parental psychosocial functioning 27,28.
Family functioning was evaluated using the Conflict Behavior Questionnaire (CBQ)29 and the Family Adaptability and Cohesion Scale (FACES II)30. These instruments have been widely used and are reliable and valid29,31.
The Conflict Behavior Questionnaire (CBQ)29 assesses perceived parent-child communication and conflict, and was completed by parents (about their child) and offspring (separate reports about mother and father). The questionnaire contains 20 true/false statements. Some statements cover the respondent’s appraisal of their relative’s behavior [e.g. “My teenager acts impatient when I talk,” (rated by the parent) “My mother is bossy when we talk” (rated by the child)]; some cover the respondent’s perception of interactions with their relative (e.g. “We argue a lot about rules”). Items are summed to generate a total conflict score (range: 0–20; higher scores indicate more negative communication).
The Family Adaptability and Cohesion Evaluation Scale II (FACES-II)30 was completed by parents and offspring older than 7. It includes 30 statements rated on a scale of 1 (almost never) to 5 (almost always). The scale yields 2 subscale scores: 1. Cohesion:-Defined as emotional bonding among family members. It includes variables such as internal boundaries, coalitions, time, space, friends, interests and recreation, and ranges from 15 (more disengaged) to 80 (more connected). Sample items include: “Family members are supportive of each other during difficult times”; “Family members know each other’s close friends”. 2. Adaptability: Defined as the ability of the family system to change its structure, role relationships, and rules in response to situational and developmental needs 32. The adaptability score ranges from 15 (rigid family patterns) to 70 (flexible family patterns). Sample items include: “Children have a say in their discipline”; “When problems arise, we compromise”. Higher scores on both cohesion and adaptability represent less impairment in family functioning30.
Statistical Methods
Baseline between-group comparisons of demographic, clinical, and family history variables were made via ANOVA, chi-square tests, and Kruskal-Wallis nonparametric tests as appropriate. The primary outcome measures modeled were the FACES-II cohesion and adaptability scores (child and parent reports) and the CBQ total score (parent-report and child-report about mother and father) as measured repeatedly before the offspring reached age 18. Multilevel multivariate linear regression was used to model the intercorrelated FACES-II outcomes and account for within-subject and within-family clustering across repeated measurements. Specifically, factors that varied at the subject-level such as age at assessment and presence of both biological parents in household were modeled at the first level, whereas factors that varied at the family-level such as parental diagnostic grouping and socioeconomic status were modeled at the second level. Because CBQ total scores were severely right-skewed (most scores were zero or quite low) and nonremediable by mathematical transformation, gamma regression (employing a natural logarithm link function after +1 transformation) was used to compare groups on CBQ scores with calculation of robust standard errors (i.e., generalized estimating equations) since attempts to fit generalized linear mixed regressions failed to converge.
The independent variable in each model was the trichotomous parent grouping variable “BD parent vs. parent with non-BD psychopathology vs. healthy parent.” All models controlled for age to account for an observed gradual degradation in family functioning as subjects aged. Models further controlled for demographic factors on which groups significantly differed at the 0.1 level (e.g., socioeconomic status and presence of both biological parents in household; see Results). Lastly, models controlled for offspring psychopathology using the trichotomous grouping variable (BD vs. non-BD psychopathology vs. healthy). Monte Carlo simulation indicated that given the sample size and covariates in the above models, group contrasts with Cohen’s d = 0.21 (small effect) or larger could be detected with 80+% power.
Models were also fit testing interactions between the parent and offspring psychopathology effects, but the interactive effects were nonsignificant. All pairwise comparisons implemented a Tukey-Kramer adjustment to account for multiple comparisons. As a final stage of the analysis, a repeated measures path analysis using a generalized estimating equations scheme was fit to ascertain the extent to which repeatedly assessed offspring psychopathology (any Axis-I disorder vs. none), offspring functioning (measured by CGAS), and parent functioning (measured by GAF) mediated the effects of parent diagnostic grouping on the FACES-II and CBQ family functioning scores over time. To ensure that the temporal precedence assumption of statistical mediation held, mediator data were used to predict family functioning outcomes at the next assessment (median of 2.1 years later). All submodels covaried for age at the time of the FACES-II/CBQ assessment (group-by-age interactions and quadratic effects were tested but found to be nonsignificant).
Multilevel regression and mediation path models were fit using Mplus 5 (code archived in Figure S1, available online); all other analyses were performed using SAS 9.4.
Results:
The offspring of BD parents and the offspring of parents with non-BD psychopathology did not significantly differ on any demographic factors (Table 1). The offspring of HCs had significantly higher mean SES and were more likely to live with both biological parents than both the offspring of BD and non-BD psychopathology. Mothers’ ages at offspring birth were also older in the HC group. Offspring with BD parents had significantly higher rates of BD spectrum, depressive, and anxiety disorders than both the offspring of parents with non-BD psychopathology and HC, and significantly higher rates of ADHD and DBD than HC at baseline. The offspring of parents with non-BD psychopathology also had significantly higher rates of depressive and anxiety disorders, ADHD, and DBD than HC. With the exception of substance abuse, the offspring of BD parents showed significantly higher rates of all parental psychiatric disorders than the offspring of parents with non-BD psychopathology. There were no-between offspring group differences in those who had one parent vs. two parents with psychopathology. Offspring who did not have longitudinal data (n= 45) had significantly lower SES and younger age of mother and father at time of birth, they were less likely to be white or live with both biological parents, and they were more likely to have a depression (p-values < 0.02). The parental groups did not significantly differ in likelihood of having follow-up data or in number of follow-up assessments.
Table 1.
Demographic and Clinical Factors
| Offspring of bipolar Parents (n=481) | Offspring of Parents w/ Nonbipolar Psychopathology (n=162) | Offspring of Healthy Parents (n=175) | Test Statistics | |||||
|---|---|---|---|---|---|---|---|---|
| Demographics | Mean | SD | Mean | SD | Mean | SD | Stat | p |
| Intake Age | 15.4 | 2.6 | 15.5 | 2.4 | 15.5 | 2.2 | K-W χ2=1.66 |
0.4 |
| Hollingshead Socioeconomic Status | 34.11 | 14.0 | 33.51 | 12.3 | 42.22 | 13.9 | K-W χ2=48.49 |
<0.0001 |
| Mother’s Age at Offspring’s Birth | 27.21 | 5.9 | 28.31,2 | 6.2 | 29.22 | 5.3 | F=8.31 | 0.0003 |
| Father’s Age at Offspring’s Birth | 30.1 | 7.2 | 30.4 | 7.7 | 31.2 | 6.8 | F=1.56 | 0.2 |
| Number of Offspring in Family | 1.9 | 1.0 | 2.0 | 1.0 | 2.0 | 0.8 | Poisson χ2=1.24 |
0.5 |
| N | % | N | % | N | % | χ2 Stat | p | |
| Race (white) | 390 | 81.1 | 119 | 73.5 | 135 | 77.1 | 4.54 | 0.1033 |
| Sex (male) | 243 | 50.5 | 79 | 48.8 | 84 | 48.0 | 0.39 | 0.8242 |
| Living with Both Biological Parents | 2331 | 48.4 | 921 | 56.8 | 1322 | 75.4 | 37.97 | <0.0001 |
| Offspring Diagnoses | N | % | N | % | N | % | χ2 Stat | p |
| Any Bipolar Spectrum Disorder | 761 | 16.5 | 32 | 2.0 | 12 | 0.6 | 48.02 | <0.0001 |
| Any Non-Bipolar Axis-I Disorder | 3191 | 69.2 | 872 | 56.9 | 543 | 32.1 | 70.10 | <0.0001 |
| Any Depression | 1671 | 36.2 | 392 | 25.5 | 193 | 11.3 | 38.30 | <0.0001 |
| Any Anxiety | 1741 | 37.7 | 402 | 26.1 | 233 | 13.7 | 35.29 | <0.0001 |
| ADHD | 1531 | 33.2 | 371 | 24.2 | 222 | 13.1 | 25.98 | <0.0001 |
| Disruptive Behavior Disorder | 1301 | 28.2 | 341 | 22.2 | 152 | 8.9 | 25.95 | <0.0001 |
| Psychotic Disorder | 4 | 0.9 | 3 | 2.0 | 0 | 0 | Fisher’s Exact | 0.2 |
| Substance Use Disorder | 39 | 8.5 | 13 | 8.5 | 7 | 4.2 | 3.50 | 0.2 |
| Parent Diagnoses | N | % | N | % | N | % | χ2 | p-value |
| Any Anxiety | 366 | 76.1 | 95 | 58.6 | --- | --- | 18.18 | <0.0001 |
| ADHD | 120 | 25.0 | 13 | 8.0 | --- | --- | 21.16 | <0.0001 |
| Disruptive Behavior Disorder | 181 | 37.6 | 19 | 11.7 | --- | --- | 37.94 | <0.0001 |
| Psychotic Disorder | 96 | 20.0 | 4 | 2.5 | --- | --- | 28.22 | <0.0001 |
| Substance Use Disorder | 303 | 63.0 | 96 | 59.3 | --- | --- | 0.72 | 0.4 |
| Both Parents Any Axis-I Disorder | 225 | 46.8 | 61 | 37.7 | --- | --- | 124.12 | <0.0001 |
Note: Values with differing superscripts indicate that groups significantly differ after adjustment for multiple comparisons. ADHD = attention-deficit/hyperactivity disorder.
Longitudinal Analyses
FACES-II:
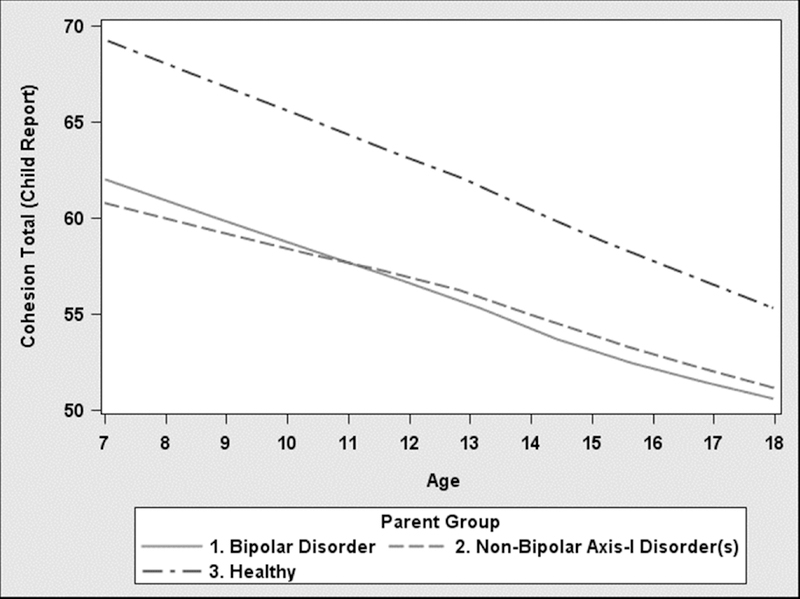
Overall, as expected in hypothesis 4, average FACES-II cohesion scores (Figure 1a) across all groups declined substantially as subjects aged (ps<0.0001), while FACES-II adaptability scores remained fairly constant (the remaining longitudinal plots of cohesion, adaptability and conflict are depicted in Figure S2, available online). Intercept-only mixed linear regressions of difference-scores between parent and child FACES-II indicated that parents reported significantly higher FACES-II cohesion and adaptability than did the children (both ps<0.0001).
Figure 1a.
Longitudinal Course of Cohesion, Child report
Within-subject-assessment correlation between follow-up FACES-II scores reported by the same respondent was quite high (Spearman r = 0.67–0.69), and correlation between scores reported by different respondents, but measuring the same domain (i.e., cohesion or adaptability), was moderately high (Spearman r = 0.36–0.53). For those reasons, multilevel multivariate linear regression was used to model the intercorrelated FACES-II outcomes and account for within-subject and within-family clustering across repeated measurements. As estimated in hypotheses 1 and 2, both parental groups of BD and non-BD psychopathology did not significantly differ from one another on any FACES-II score (ps>0.2), but had significantly lower mean cohesion and adaptability scores than HC across both child and parent reports (ps<0.02; Table 2).
Table 2.
Longitudinal Family Functioning and Conflict Models
| Multilevel Multivariate Linear Model | Least Square Means (SE) | Group Contrast | Cohen’s d | Z | p | ||
| FACES Subscales | 1. Offspring of bipolar Parents (n=481) | 2. Offspring of Parents w/ Non-bipolar Psychopathology (n=162) | 3. Offspring of Healthy Parents (n=175) | ||||
| Cohesion Child Report | 54.9 (0.5)a | 55.6 (1.0)a | 60.0 (0.8)b | 1 vs. 3 | 0.46 | 5.46 | <0.0001 |
| 2 vs. 3 | 0.39 | 3.65 | 0.0001 | ||||
| Adaptability Child Report | 43.0 (0.4)a | 42.8 (0.7)a | 45.4 (0.5)b | 1 vs. 3 | 0.28 | 3.81 | 0.0001 |
| 2 vs. 3 | 0.31 | 3.09 | 0.001 | ||||
| Cohesion Parent Report | 56.1 (0.7)a | 57.0 (1.0)a | 62.3 (0.8)b | 1 vs. 3 | 0.60 | 6.20 | <0.0001 |
| 2 vs. 3 | 0.57 | 4.48 | <0.0001 | ||||
| Adaptability Parent Report | 43.8 (0.5)a | 44.2 (0.7)a | 46.2 (0.6)b | 1 vs. 3 | 0.34 | 3.14 | 0.0008 |
| 2 vs. 3 | 0.33 | 2.29 | 0.01 | ||||
| Generalized Estimating Equations | Least Square Means (SE) | Group Contrast | Cohen’s d | Z | p | ||
| CBQ Subscales | 1. Offspring of bipolar Parents (n=481) | 2. Offspring of Parents w/ Non-bipolar Psychopathology (n=162) | 3. Offspring of Healthy Parents (n=175) | ||||
| Total Score Child about Mother | 3.8 (1.0)a | 3.8 (1.1)a | 2.6 (1.1)b | 1 vs. 3 | 0.29 | 4.05 | <0.0001 |
| 2 vs. 3 | 0.32 | 3.46 | 0.0003 | ||||
| Total Score Child about Father | 4.5 (1.1)a | 4.7 (1.1)a | 3.5 (1.1)b | 1 vs. 3 | 0.20 | 2.49 | 0.006 |
| 2 vs. 3 | 0.26 | 2.29 | 0.01 | ||||
| Total Score Parent Summary | 6.5 (1.0)a | 5.7 (1.1)a | 3.8 (1.1)b | 1 vs. 3 | 0.51 | 6.45 | <0.0001 |
| 2 vs. 3 | 0.44 | 4.44 | <0.0001 | ||||
Note: Values with differing superscripts (a or b) indicate that groups significantly differ after adjustment for multiple comparisons. Models covaried for age at assessment, presence vs. absence of both biological parents in household, age of mother at time of offspring birth, offspring diagnostic grouping (bipolar disorder (BD) vs. non-BD psychopathology vs. healthy), and socioeconomic status. CBQ = Conflict Behavior Questionnaire; FACES = Family Adaptability and Cohesion Scale-II.; SE = standard error..
CBQ:
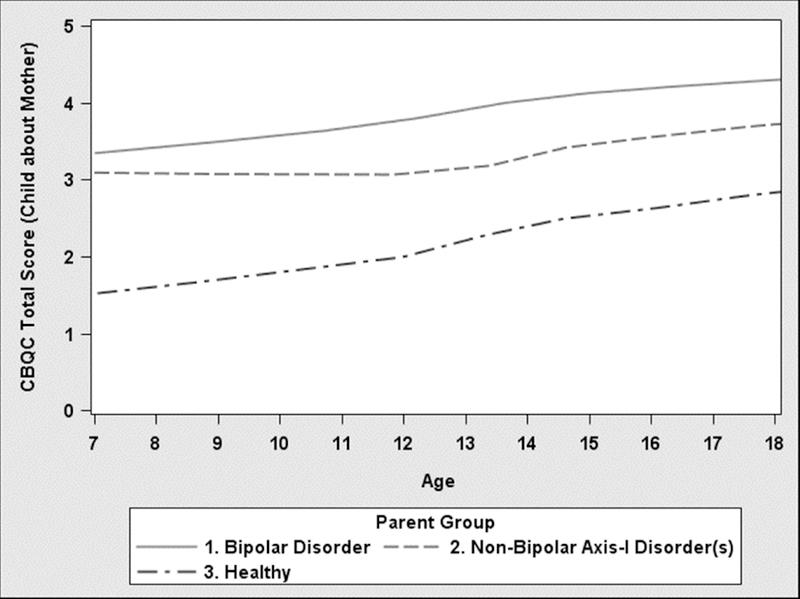
Across all groups, as predicted in hypothesis 4, conflict levels increased substantially as subjects aged (ps<0.0001) (Figure 1b). Intercept-only mixed linear regressions of differences between parent and child CBQ scores indicated that parents’ ratings of conflict were significantly more severe than offspring’s (ps<0.0001).
Figure 1b.
Longitudinal Course of Conflict, Child Report About Mother
Correlation between follow-up CBQ scores as reported by different respondents was relatively low (Spearman r = 0.24–0.43). Consistent with hypothesis 2, the regression indicated that across all subscales, parents with BD and non-BD psychopathology did not significantly differ from one another but had significantly higher CBQ scores than HC parents (ps<0.02; Table 2).
Mediational Path Analysis
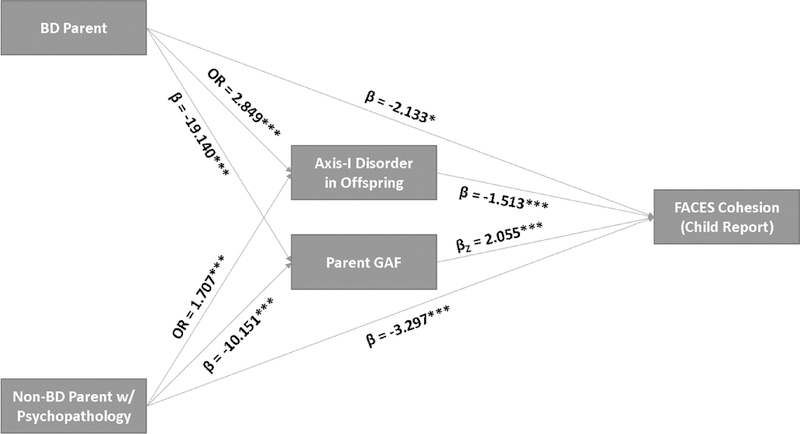
The general design of the mediation path analysis for the FACES-II cohesion child-report submodel is shown in Figure 2 (the six remaining submodel diagrams for cohesion, adaptability and conflict are depicted in Figure S3, available online). Below, we report a summary of findings from the mediation model; more rigorous statistical interpretations of this model are included in the supplementary material (see Supplement 1, available online).
Figure 2. Mediational Path Analysis.
Note: β = regression coefficient for categorical predictor; βZ = standardized regression coefficient for continuous predictor; BD = bipolar disorder; FACES = Family Adaptability and Cohesion Scale-II; GAF = Global Assessment of Functioning; OR = odds ratio
The BD parent group did not significantly directly differ from the non-BD psychopathology parent group in any FACES-II or CBQ measures (as was the case in the previous models). Parent’s psychopathology significantly predicted the mediator effects of offspring psychopathology and parent GAF (ps<0.001). Offspring CGAS did not significantly mediate the parent diagnostic grouping effect; thus, this effect was removed from the model. Consistent with hypothesis 3, results showed that parent GAF scores significantly mediated the parent diagnostic grouping effects on all FACES-II and CBQ outcomes, and offspring psychopathology significantly mediated the parent diagnostic grouping effects on all CBQ and child-reported FACES-II outcomes (ps<0.03) (see Table S2, available online). Overall, the BD parent total effects (direct effects + mediated effects) were larger than the non-BD psychopathology parent total effects in all seven submodels (see Figure 2 and Figure S3, available online). However, this contrast was only significant in the CBQ parent summary score submodel. The full mediation model had a root mean square error of approximation (RMSEA) of 0.019, comparative fit index (CFI) of 0.997, and Tucker-Lewis index (TLI) of 0.982, indicating good model fit (see Supplement 1, available online, for more information on goodness of fit).
Discussion:
This longitudinal study examined family functioning in the families of children with at least one parent with BD. To our knowledge, this is the largest prospective high-risk offspring study to evaluate the family functioning of parents with BD in comparison to parents with non-BD psychopathology and HC parents. As hypothesized, after adjusting for the offspring’s level of psychopathology, families with BD parents and families of parents with non-BD psychopathology showed significantly lower levels of cohesion and adaptability and higher conflict in comparison with HC families. However, there were no significant differences in family functioning between families of BD parents and families of parents with non-BD psychopathology. Poorer family functioning was directly accounted for by the effects of parental psychopathology, and was also mediated by parental psychosocial functioning and offspring psychopathology. Finally, we found that in all three groups, family cohesion levels gradually decreased, and conflict levels increased from childhood into adolescence, as reported by both offspring and parents.
The following study limitations should be taken into account. First, ratings of family functioning are from parents and offspring with psychopathology, and therefore may be biased 33. Thus, standardized laboratory-based family interaction tasks of family functioning (e.g., McMaster Clinical Rating Scale) could minimize the potential for bias. Second, the results may not be generalizable to a more culturally diverse sample because our sample was mainly Caucasian. Third, though this is a prospective study, all diagnoses and estimates of age of onset are made retrospectively for the interval of time between assessments. Finally, given that BIOS is a naturalistic study in which the effects of treatment are confounded by indication, treatment was not included in the analyses.
Consistent with other studies, we found lower cohesion and adaptability and higher conflict in families of BD parents compared to HC 3,12. However, our results indicate that these differences are not specific to families with a BD parent because they were similar in families of parents with non-BD psychopathology. Similar to other studies, the correlations between parents’ and youths’ ratings on the CBQ and FACES-II were low to moderate, emphasizing the need for a thorough evaluation process that captures the different perspectives of youth and their parents 6,34.
Prior studies that focused on BD youth instead of BD parents have not found differences in family functioning between the families of BD youth and youth with non-BD psychopathology, again supporting the idea that family dysfunction is related to psychopathology in general rather than BD specifically 8,35.
The relationship between family functioning, psychopathology and psychosocial functioning are multidirectional and likely serve as both cause and consequence for one another36. Poor family functioning might lead to a “vicious cycle” of new onset or worsening of psychopathology, increased stress, and difficulties in coping with stress37, which further contributes to worsening of family functioning. We found that family functioning is directly affected by parental psychopathology, and is also mediated by parental psychosocial functioning and offspring’s psychopathology. According to our path analysis, the effect of child’s psychopathology on family functioning is significant but is smaller than the effect of parental psychopathology. These findings underscore the substantial impact that parental psychopathology has on family functioning above and beyond the offspring’s psychopathology. In fact, studies show that treatment for parents, even in the absence of treatment for offspring, may help ameliorate the offspring’s psychiatric symptoms 38. In our path-analysis model, the total effect of BD parents on familial functioning was larger than parents with non-BD psychopathology (figure 2), though this contrast was only significant in the parent CBQ sub-model. This might be explained by the fact that this model treats offspring diagnosis as a mediator dependent on parent diagnosis rather than a simple covariate. In doing so, the model accounts for the fact that parental BD leads to more offspring psychopathology than parental non-BD psychopathology, which eventually leads to more family dysfunction. Our meditational path analysis demonstrates for the first time in the literature the complex interplay between family functioning, parental psychopathology, parental psychosocial functioning, and offspring psychopathology. Hence, outcomes at the individual youth, parent and family levels may be positively impacted when clinicians assess and target these variables in treatment.
We found higher levels of conflict as reported by parents compared to their offspring in all three study groups. These results extend the findings of prior uncontrolled investigations among BD youth 6,35,39. A review paper that focused on parent-adolescent relationships suggested that daily conflicts are more distressing to parents than to adolescents 40. Also, parents may give greater meaning to conflictual interactions, interpreting them as rejections of their values or indicators of their failures as parents. In contrast, adolescents may see the conflicts as less significant 40. Thus, differences in perspective between youth and their parents regarding conflicts should be considered for both assessment and treatment purposes.
We found an age-related pattern, whereby family cohesion decreases, and conflict levels increase between ages 7–18 in all three parental groups. Interestingly, family adaptability tended to be constant over time, possibly indicating a trait-like index. To our knowledge, this is the first study to demonstrate that families with a parent (and in a proportion of cases, an offspring) with a psychiatric diagnosis show the same longitudinal patterns of family functioning and conflicts as healthy families, although with higher levels of conflict and lower cohesion and adaptability. These patterns are consistent with the literature on familial dynamics in the general population. Longitudinal studies of normative youth show a steady increase in family conflict between ages 14 to 18, during which there is an increase in adolescent autonomy and a decline in parent-child cohesion 20,21. The increase in conflicts and decrease in cohesion during the adolescent years is thought to be part of the normal maturation process that includes aspiration for independence, de-idealization of parents, and a shift of social orientation away from parents 41.
In summary, any type of parental psychopathology predicted family impairment. These results were influenced by the offspring’s age and were mediated by parental psychosocial functioning, and to a lesser degree, by offspring psychopathology. For the first time in the literature, our analysis showed that BD offspring, offspring of non-BD psychopathology parents and offspring of healthy parents have a similar age-related pattern in which family cohesion decreases and conflicts increase from age 7 to 18 years old. Thus, it is important to routinely assess family functioning in addition to individual psychopathology. This assessment should consider the developmental stage of the youth and the fact that family dynamics change over time. These factors are central for identifying and providing appropriate interventions to both parents and offspring.
Supplementary Material
Acknowledgments:
The authors would like to thank the studies’ participants and their families and to the Herman Dana Foundation which provided a stipend for the research activities of the corresponding author. The authors would also like to thank the statistical expert of this study, John Merranko, MS, of the Department of Psychiatry, Western Psychiatric Institute and Clinic, University of Pittsburgh.
Disclosures:
Dr. T. Goldstein has received grant funding from the National Institute of Mental Health (NIMH), the American Foundation for Suicide Prevention, the Brain and Behavior Research Foundation, and the University of Pittsburgh Clinical and Translational Science Institute, and royalties from Guilford Press.
Dr. Miklowitz has received research funding from the NIMH, the Brain and Behavior Research Foundation, the Attias Family Foundation, the Danny Alberts Foundation, the Carl and Roberta Deutsch Foundation, the Kayne Family Foundation, AIM for Mental Health, and the American Foundation for Suicide Prevention, and royalties from Guilford Press and John Wiley and Sons.
Dr. Axelson has served as a consultant to Janssen Research and has received grant support from Neuronetics and royalties from UpToDate.
Dr. B. Goldstein has received grant or research support from the Canadian Institutes of Health Research, the Brain and Behavior Research Foundation (NARSAD), the Ontario Ministry of Research and Innovation, the Ontario Mental Health Foundation, the Heart and Stroke Foundation of Canada, and Brain Canada.
Dr. Brent has received research support from the NIMH and has received royalties from Guilford Press, the electronic self-rated version of the C-SSRS from ERT, Inc., and UpToDate. He has received consulting fees from Psychological Medicine, Healthwise, and McKesson.
Dr. Hafeman has received grants from the NIMH and the Klingenstein Third Generation Foundation.
Dr. Sakolsky has received funding from the NIMH and has served as a consultant for the Prescriber’s Letter.
Dr. Diler has received grants from the NIMH.
Dr. Birmaher has received grants from the NIMH and has received royalties from Random House, UpToDate, and Lippincott, Williams, and Wilkins.
Dr. Shalev, Mr. Merranko, and Mss. Monk and Hickey report no biomedical financial interests or potential conflicts of interest.
Funding: This study was supported by the National Institute of Mental Health grant MH060952. This manuscript represents original material that has never been published before, is not under consideration for publication elsewhere, and has been approved by each author. The work was completed at Department of Psychiatry, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania.
Mr. Merranko served as the statistical expert for this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Drs. Amit Shalev, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA; Herman Dana Division of Pediatric psychiatry, Hadassah Hebrew University Medical Center, Jerusalem, Israel.
Mr. John Merranko, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Tina Goldstein, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Dr. David J. Miklowitz, Division of Child & Adolescent Psychiatry, UCLA Semel Institute, David Geffen School of Medicine, University of California, Los Angeles.
Dr. David Axelson, Children’s Hospital and The Ohio State University, Columbus.
Dr. Benjamin I. Goldstein, University of Toronto Faculty of Medicine, Ontario, Canada.
David Brent, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Mss. Kelly Monk, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Mary Beth Hickey, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Danella M. Hafeman, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Dara Sakolsky, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Rasim Diler, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
Boris Birmaher, Western Psychiatric Institute and Clinic, University of Pittsburgh School of Medicine, PA.
References
- 1.Pavuluri MN, Birmaher B, Naylor MW. Pediatric bipolar disorder: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. September 2005;44(9):846–871. [DOI] [PubMed] [Google Scholar]
- 2.Goldstein TR, Obreja M, Shamseddeen W, et al. Risk for suicidal ideation among the offspring of bipolar parents: results from the Bipolar Offspring Study (BIOS). Archives of suicide research: official journal of the International Academy for Suicide Research. 2011;15(3):207–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang KD, Blasey C, Ketter TA, Steiner H. Family environment of children and adolescents with bipolar parents. Bipolar disorders. April 2001;3(2):73–78. [DOI] [PubMed] [Google Scholar]
- 4.Kim EY, Miklowitz DJ, Biuckians A, Mullen K. Life stress and the course of early-onset bipolar disorder. Journal of affective disorders. April 2007;99(1–3):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miklowitz DJ, Chung B. Family-Focused Therapy for Bipolar Disorder: Reflections on 30 Years of Research. Family process. September 2016;55(3):483–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Timmins V, Swampillai B, Hatch J, et al. Correlates of Adolescent-reported and Parent-reported Family Conflict Among Canadian Adolescents With Bipolar Disorder. Journal of psychiatric practice. January 2016;22(1):31–41. [DOI] [PubMed] [Google Scholar]
- 7.Nader EG, Kleinman A, Gomes BC, et al. Negative expressed emotion best discriminates families with bipolar disorder children. Journal of affective disorders. June 2013;148(2–3):418–423. [DOI] [PubMed] [Google Scholar]
- 8.Du Rocher Schudlich TD, Youngstrom EA, Calabrese JR, Findling RL. The role of family functioning in bipolar disorder in families. Journal of abnormal child psychology. August 2008;36(6):849–863. [DOI] [PubMed] [Google Scholar]
- 9.Townsend LD, Demeter CA, Youngstrom E, Drotar D, Findling RL. Family conflict moderates response to pharmacological intervention in pediatric bipolar disorder. Journal of child and adolescent psychopharmacology. December 2007;17(6):843–852. [DOI] [PubMed] [Google Scholar]
- 10.Miklowitz DJ, Axelson DA, George EL, et al. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. June 2009;48(6):643–651. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan AE, Judd CM, Axelson DA, Miklowitz DJ. Family functioning and the course of adolescent bipolar disorder. Behavior therapy. December 2012;43(4):837–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferreira GS, Moreira CR, Kleinman A, et al. Dysfunctional family environment in affected versus unaffected offspring of parents with bipolar disorder. The Australian and New Zealand journal of psychiatry. November 2013;47(11):1051–1057. [DOI] [PubMed] [Google Scholar]
- 13.Berutti M, Dias RS, Pereira VA, Lafer B, Nery FG. Association between history of suicide attempts and family functioning in bipolar disorder. Journal of affective disorders. March 01 2016;192:28–33. [DOI] [PubMed] [Google Scholar]
- 14.Uebelacker LA, Beevers CG, Battle CL, et al. Family functioning in bipolar I disorder. Journal of family psychology: JFP: journal of the Division of Family Psychology of the American Psychological Association (Division 43). December 2006;20(4):701–704. [DOI] [PubMed] [Google Scholar]
- 15.Weinstock LM, Keitner GI, Ryan CE, Solomon DA, Miller IW. Family functioning and mood disorders: a comparison between patients with major depressive disorder and bipolar I disorder. Journal of consulting and clinical psychology. December 2006;74(6):1192–1202. [DOI] [PubMed] [Google Scholar]
- 16.Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Archives of general psychiatry. March 1988;45(3):225–231. [DOI] [PubMed] [Google Scholar]
- 17.Kim EY, Miklowitz DJ. Expressed emotion as a predictor of outcome among bipolar patients undergoing family therapy. Journal of affective disorders. November 01 2004;82(3):343–352. [DOI] [PubMed] [Google Scholar]
- 18.Yan LJ, Hammen C, Cohen AN, Daley SE, Henry RM. Expressed emotion versus relationship quality variables in the prediction of recurrence in bipolar patients. Journal of affective disorders. December 2004;83(2–3):199–206. [DOI] [PubMed] [Google Scholar]
- 19.Birmaher B, Axelson D, Monk K, et al. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh Bipolar Offspring study. Archives of general psychiatry. March 2009;66(3):287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herrenkohl TI, Kosterman R, Hawkins JD, Mason WA. Effects of Growth in Family Conflict in Adolescence on Adult Depressive Symptoms: Mediating and Moderating Effects of Stress and School Bonding. Journal of Adolescent Health.44(2):146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinberg L Reciprocal relation between parent-child distance and pubertal maturation. Developmental psychology. 1988;24(1):122. [Google Scholar]
- 22.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Archives of general psychiatry. August 1992;49(8):624–629. [DOI] [PubMed] [Google Scholar]
- 23.Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Archives of general psychiatry. October 1977;34(10):1229–1235. [DOI] [PubMed] [Google Scholar]
- 24.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. July 1997;36(7):980–988. [DOI] [PubMed] [Google Scholar]
- 25.Axelson D, Birmaher BJ, Brent D, et al. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children mania rating scale for children and adolescents. Journal of child and adolescent psychopharmacology. Winter 2003;13(4):463–470. [DOI] [PubMed] [Google Scholar]
- 26.Hollingshead AB. Four factor index of social status. 1975.
- 27.Shaffer D, Gould MS, Brasic J, et al. A children’s global assessment scale (CGAS). Archives of general psychiatry. 1983;40(11):1228–1231. [DOI] [PubMed] [Google Scholar]
- 28.Association AP, Association AP. DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association; 2000;75:78–85. [Google Scholar]
- 29.Prinz RJ, Foster S, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of applied behavior analysis. 1979;12(4):691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Olson D, Tiesel J. FACES II: Linear scoring and interpretation. Available from: Life Innovations, Family Inventories Project, PO Box 1991;190:55440–50190. [Google Scholar]
- 31.Place M, Hulsmeier J, Brownrigg A, Soulsby A. The Family Adaptability and Cohesion Evaluation Scale (FACES): an instrument worthy of rehabilitation? Psychiatric Bulletin. 2005;29(6):215–218. [Google Scholar]
- 32.Olson D FACES IV and the Circumplex Model: Validation Study. Journal of marital and family therapy. 2011;37(1):64–80. [DOI] [PubMed] [Google Scholar]
- 33.Maoz H, Goldstein T, Goldstein BI, et al. The effects of parental mood on reports of their children’s psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. October 2014;53(10):1111–1122.e1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychological bulletin. March 1987;101(2):213–232. [PubMed] [Google Scholar]
- 35.Sullivan AE, Miklowitz DJ. Family functioning among adolescents with bipolar disorder. Journal of Family Psychology. 2010;24(1):60. [DOI] [PubMed] [Google Scholar]
- 36.Robinson E, Rodgers B, Butterworth P. Family relationships and mental illness. AFRC Issues. 2008:1–19. [Google Scholar]
- 37.Lavee Y, Olson DH. Family types and response to stress. Journal of Marriage and the Family. 1991;53(3):786–798. [Google Scholar]
- 38.Perlick DA, Jackson C, Grier S, et al. Randomized trial comparing caregiver-only family-focused treatment to standard health education on the 6-month outcome of bipolar disorder. Bipolar disorders. March 12 2018. [DOI] [PubMed] [Google Scholar]
- 39.Esposito-Smythers C, Birmaher B, Valeri S, et al. Child comorbidity, maternal mood disorder, and perceptions of family functioning among bipolar youth. Journal of the American Academy of Child and Adolescent Psychiatry. August 2006;45(8):955–964. [DOI] [PubMed] [Google Scholar]
- 40.Steinberg L We know some things: Parent–adolescent relationships in retrospect and prospect. Journal of research on adolescence. 2001;11(1):1–19. [Google Scholar]
- 41.Montemayor R Parents and Adolescents in Conflict: All Families Some of the Time and Some Families Most of the Time. The Journal of Early Adolescence. 1983;3(1–2):83–103. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.