Abstract
Considerable research and public discourse on family caregiving portrays it as a stressful and burdensome experience with serious negative health consequences. A landmark study by Schulz and Beach that reported higher mortality rates for strained spouse caregivers has been widely cited as evidence for the physical health risks of caregiving and is often a centerpiece of advocacy for improved caregiver services. However, 5 subsequent population-based studies have found reduced mortality and extended longevity for caregivers as a whole compared with noncaregiving controls. Most caregivers also report benefits from caregiving, and many report little or no caregiving-related strain. Policy reports, media portrayals, and many research reports commonly present an overly dire picture of the health risks associated with caregiving and largely ignore alternative positive findings. As the pool of traditional family caregivers declines in the coming years, a more balanced and updated portrayal of the health effects of caregiving is needed to encourage more persons to take on caregiving roles, and to better target evidence-based services to the subgroup of caregivers who are highly strained or otherwise at risk. Recommendations are discussed for research that will better integrate and clarify both the negative and potential positive health effects of informal caregiving.
Keywords: Caregiving, Caregivers, Mortality, Population-based studies
Our country is in the early stages of an unprecedented explosion in the number of older adults who will be living at home with physical disabilities or serious cognitive impairments. The need to provide adequate care to these vulnerable older adults is a major challenge facing our society on many levels. The assumption of our current health care system is that close family members will provide the majority of day-to-day assistance and manage the wide array of problems that confront these older adults with disabilities. However, most health care delivery models focus primarily on individual patients and do not properly engage, educate, or support family caregivers or other informal care providers (Gillick, 2013; Wolff & Roter, 2008). Furthermore, despite the projected increase in the need for caregivers (Centers for Disease Control and Prevention [CDC], 2010), the pool of available family caregivers is expected to decline in the coming years due to smaller and more dispersed families as a result of decades of reduced fertility rates, lower marriage rates, higher divorce rates, and greater geographic mobility.
For those who take on caregiving roles, the prevailing view from the research literature, public policy statements, and the lay public is that becoming an informal caregiver for a disabled family member is often a chronically stressful experience that can become overwhelming and may even become hazardous to the caregiver’s own health. Meta analyses and other systematic reviews typically conclude that caregivers are more likely to experience depressive symptoms and have poorer physical health outcomes when compared with various samples of noncaregivers (Pinquart & Sörensen, 2003; Schulz & Sherwood, 2008; Vitaliano, Zhang, & Scanlon, 2003). The commonly accepted and converging viewpoint, therefore, is that while the need for informal caregivers is rapidly increasing, the pool of potentially available caregivers is actually shrinking, and the caregiving role is both stressful and hazardous to the caregivers’ health (CDC, 2010). A breaking point in this critical resource appears to be inevitable in the near future.
This Forum article aims to re-examine some of the existing evidence on the health effects of caregiving, focusing in particular on one commonly cited claim that family caregiving is associated with an increased risk for mortality. We will discuss important methodological concerns on the definition of caregiving, the composition of different caregiving subgroups, the sampling of caregivers, and the sampling and recruitment of appropriate noncaregiving comparison groups. An important goal is to contribute to a more updated and balanced portrayal of the health effects of caregiving in the research literature, lay media, and public policy realm.
Who Are Informal Caregivers?
The defining characteristics of an informal caregiver typically include being a person who provides some type of unpaid, ongoing assistance with activities of daily living (ADLs) or instrumental activities of daily living (IADLs) to a person with a chronic illness or disability. This is in contrast to formal caregivers, such as home health aides, who are paid for their professional services. Different studies, however, vary in their methods for defining who qualifies as a caregiver and for measuring and confirming the types of assistance provided. In some studies, caregivers are simply the co-residing spouses of persons with dementia who report providing some informal care (e.g., Kiecolt-Glaser et al., 2003; von Känel et al., 2006). Other studies more explicitly confirm that caregivers are persons who provide help with one or more ADLs or IADLs (e.g., Brown et al., 2009; Fredman et al., 2010; Schulz & Beach, 1999). Telephone survey studies have defined caregiving by asking specific questions about providing some form of assistance to a family member with a chronic illness or disability (e.g., Roth et al., 2013) or to an older adult who was unable to manage independently without help (e.g., Pruchno et al., 2008).
In addition to some definitional differences across studies, there is also considerable variability on many caregiving-related factors. Caregivers differ in the relationships they have with their care recipients (e.g., spouse, adult child, other relative, in-law, neighbor or friend), their living arrangements (e.g., co-residing vs. not living with the care recipient), whether the person is a “primary” caregiver or someone who provides more secondary and supplemental support, the clinical conditions of the care recipients (e.g., dementia, frailty, stroke, etc.), and other indicators of the extent and involvement in providing care. Studies differ substantially on these dimensions, and on whether certain types of caregivers are explicitly included or excluded. From a public policy perspective, it would be helpful to define the broad population of caregivers, then identify variables or specific caregiving subtypes within that broad population that are under investigation, and limit the generalizations to the specific subtype(s) being examined.
Under What Circumstances is Caregiving Stressful?
Informal family caregiving is often described as a burdensome role that has all of the hallmarks of a chronic stress experience (Schulz & Sherwood, 2008). The burden associated with caregiving has been assessed for decades using a measure developed by Zarit, Reever, and Bach-Peterson (1980) in their seminal paper that has now been cited over 2,800 times. Schulz and Beach (1999) followed in this tradition and stated that “there is a strong consensus that caring for an elderly individual with disabilities is burdensome and stressful” and that “although family caregivers perform an important service for society and their relatives, they do so at considerable cost to themselves (p. 2215).”
There is no doubt that, in many cases, it is stressful to have a close family member who is afflicted with a chronic illness or disability. However, it is not always clear that the responsibilities and activities that accompany providing help to those individuals with disabilities lead to an increase on the overall level of stress. Having a close family member, such as a spouse or an elderly parent, with dementia or some other serious disability can lead to stress or depressive symptoms regardless of whether the unaffected family member is providing care to the family member with the disability (Amirkhanyan & Wolf, 2003). Lazarus and Folkman (1984) provided a classic definition of stress as a “particular relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering well-being (p. 19).” Under this definition, people may not appraise situations as stressful if they are confident they have sufficient resources to manage those situations. If family members or other acquaintances freely choose to provide help to a disabled person within the scope of their knowledge and resources and without any perceptions of new threats, then this type of informal caregiving may not meet this conceptual definition of a stressful situation.
Multiple population-based studies indicate that many family caregivers, in fact, report little or no strain associated with providing caregiving assistance. Schulz and Beach (1999) found that 44% of the spouse caregivers in their sample reported “no strain” in association with caregiving tasks, while 56% reported either “some strain” or “a lot of strain.” Using similar questions for both spouse and nonspouse caregivers, Roth and colleagues (2009) found that 33% of caregivers reported “no strain” and only 17% reported “a lot of strain.” A recent survey by the National Opinion Research Center (2014) found that 83% of caregivers viewed it as being a positive experience.
The conceptual framework underlying the assertion that caregiving is stressful and hazardous to one’s health is based on an integration of sociological (e.g., Pearlin et al., 1981), psychological (e.g., Lazarus & Folkman, 1984), and physiological (e.g., McEwen, 1998) models of the impact of stress on health. Specifically, when caregiving demands exceed psychological or social resources to cope, immunological and neuroendocrine disruptions may occur that can increase one’s risk of health decline. This stress process model, however, should be complemented and balanced by the healthy caregiver hypothesis (Fredman et al., 2010), which asserts that healthier persons are more likely to become caregivers and to remain in caregiving roles over time, and by evolutionary models that describe biological mechanisms by which health benefits might be obtained from prosocial behavior (Brown & Brown, 2014). Theoretical models that focus primarily on the stressful aspects of caregiving are also based on an assumption that caregivers are more stressed than noncaregivers. However, only a few studies (e.g., Fredman et al., 2010; Gallagher-Thompson et al., 2006; Wahbeh et al., 2008) have actually compared caregivers and noncaregivers on self-reported measures of stress.
Caregivers would be expected to experience high levels of stress when they do not have sufficient internal (information, skills, coping behaviors) and external (finances, help from other family, formal care) resources to adapt to caregiving situations. Providing care in a progressively deteriorating situation over a long period of time, with little or no choice or hope for relief, such as caring for a spouse with Alzheimer’s disease, would likely qualify as a stressful situation, but one that is probably not representative of most family caregivers. Caregivers might also be at increased risk if they have pre-existing health conditions that compromise their responses to stress. Many caregivers experience both positive experiences and some strain simultaneously (Beach et al., 2000; Harmell, Chattillion, Roepke, & Mausbach, 2011). Lawton, Moss, Kleban, Glicksman, and Rovine (1991) asserts that caregivers may experience both emotional distress and psychological satisfaction and growth, effects that are not assumed to be different ends of one continuum. Indeed, the positive experiences of caregiving could potentially buffer against some of the possible stress-related health consequences.
To be connected through caring relationships with other human beings, especially within one’s own family, is a common human experience that is desired by virtually everyone. Providing care for an older family member or friend with a chronic illness or disability is an increasingly common and important type of caring relationship. We assert that the “caregiving-is-stressful” assumption is an overly narrow, simplified, and limited view on these types of human relationships. Multiple perspectives, from research on altruism, volunteerism, and evolutionary perspectives on prosocial behavior, are currently emerging to provide a broader and more balanced view on the range of caregiving experiences and health outcomes (Brown & Brown, 2014).
Is Caregiving Associated With Poorer Health for Caregivers?
There is a large literature that indicates caregivers, as a general group, are more likely to report symptoms of depression and other indicators of psychological distress than noncaregivers (Pinquart & Sörensen, 2003; Roth et al., 2009; Schulz & Sherwood, 2008). Many studies also suggest that caregivers have poorer physical health when compared with various samples of noncaregivers (Pinquart & Sörensen, 2003; Vitaliano, Zhang, & Scanlon, 2003), and several investigations specifically restricted to dementia caregivers have reported higher inflammatory burden and other biomarkers of poorer health in these caregivers compared with various noncaregiving comparison groups (Gouin et al. 2012; Kiecolt-Glaser et al., 2003; Lovell & Wetherell, 2011; von Känel et al., 2006). Unfortunately, the vast majority of studies on the physical health and biomarker correlates of family caregiving have relied on clinical or convenience samples, where markedly different recruitment methods are usually used for the caregiving and noncaregiving comparison groups.
Population-based studies that compare caregivers with noncaregivers who have been recruited and enrolled with similar procedures are surprisingly rare, and only a few population-based studies have examined physiological or biomarker correlates of caregiving status. Such studies would be useful for better controlling some of the confounds that potentially contaminate comparisons of convenience samples. A review paper published in 2011 identified 42 papers up to that date on caregiving and biomarkers (Lovell & Wetherell, 2011). Interestingly, 41 of those 42 papers used convenience samples, and only 5 had samples of over 100 caregivers. A large majority of these studies were comparisons of dementia caregivers to poorly characterized noncaregiving controls. Dementia caregivers may experience more problems than other caregiving subgroups (Ory, Hoffman, Yee, Tennstedt, & Schulz, 1999), but they represent only a small proportion of all informal caregivers (National Alliance for Caregiving and AARP, 2009).
An important limitation of much of the research on the physical health and biomarker correlates of caregiving is that the noncaregiving controls in these studies are almost always recruited from different sources, such as through newsletters and social groups where socially active individuals are asked to “volunteer” to participate in a research project. Consequently, the finding of poorer health for the caregivers from such studies is equivalent to the finding of better health among the socially active volunteers. That is, in many convenience sample comparisons in the caregiving literature, the health risks of caregiving are confounded with the health benefits of volunteerism (Okun, Yeung, & Brown, 2013). The results from studies of convenience samples are further qualified by findings that convenience samples of caregivers report more physical health problems and depressive symptoms in comparison to noncaregivers than population-based comparisons of these samples (Pinquart & Sörensen, 2003; Pruchno et al., 2008). In short, there is very little evidence from well-controlled population-based studies that family caregivers, as a general group, have poorer objective physical health than suitable noncaregiving comparison groups. There is considerable evidence that caregivers experience symptoms of emotional distress, but some of this may be a result of observing a family member struggling with a serious or disabling medical condition (Amirkhanyan & Wolf, 2003; Monin & Schulz, 2009) and not because of any stress involved in providing care to that person.
Is Caregiving Associated With Increased Risk for Mortality?
A widely cited publication on the deleterious health effects of caregiving comes from the landmark study of the mortality rates for the spouses of participants in the population-based Cardiovascular Health Study (CHS) (Schulz & Beach, 1999). This study compared spouses of CHS participants without disability to three groups of spouses of CHS participants with disabilities: (a) spouses of disabled persons but no help being provided, (b) spouses of disabled persons and help being provided but with no caregiving strain reported, and (c) spouses of disabled persons, help being provided, and some caregiving strain reported. The strained spouse caregivers were found to be 63% more likely to die in the subsequent 4-year follow-up period than the spouses of nondisabled partners (covariate-adjusted relative risk (RR) = 1.63, 95% confidence interval (CI) = 1.00–2.65). Importantly, the spouses who were providing care but reported no caregiving strain had mortality rates that were similar to spouses of non-disabled partners (RR = 1.08, 95% CI = 0.61–1.90).
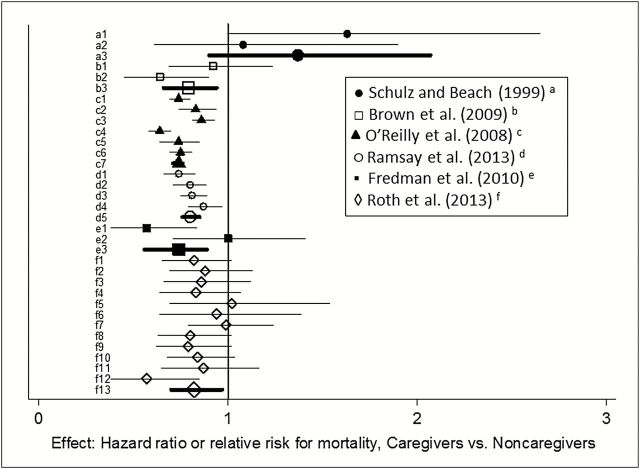
Figure 1 illustrates the effects of the Schulz and Beach (1999) analyses along with five subsequent population-based studies of the impact of caregiving on mortality. Additional descriptive information on these six studies is summarized in Table 1. A hazard ratio (HR) or RR > 1 indicates an increase in mortality for caregivers compared with a noncaregiving referent group, whereas an HR or RR < 1 indicates a lower mortality rate for the caregivers. For each study, thin lines are used in Figure 1 to illustrate effects reported in the original articles for specific caregiving subgroups, and thick lines are included at the bottom of each study panel to indicate overall caregiving effects.
Figure 1.
Effect sizes from survival analyses of caregivers versus noncaregivers. Thin lines represent caregiving subgroup effects reported in the original articles. Thick lines represent overall caregiving effects either reported in the Fredman and colleagues (2010) and Roth and colleagues (2013) articles or calculated based on the subgroup information reported in the other articles. a1: 179 strained spouse caregivers; a2: 138 nonstrained spouse caregivers; a3: 317 strained and nonstrained caregivers; b1: 306 spouses providing 1–14hr of care; b2: 338 spouses providing 14 or more hours of care; b3: 644 spouses providing any care to a spouse with ADL/IADL impairment; c1: 58,075 women providing 1–19hr of care; c2: 15,141 women providing 20–49hr of care; c3: 25,757 women providing 50+ hr of care; c4: 40,606 men providing 1–19hr of care; c5: 9519 men providing 20–49hr of care; c6: 15,786 men providing 50+ hr of care; c7: 162,884 men and women providing any care; d1: 12,033 women providing 1–19hr of care; d2: 5,876 women providing 20 or more hours of care; d3: 9,751 men providing 1–19hr of care; d4: 3,744 women providing 20 or more hours of care; d5: 31,404 men and women providing any care; e1: 219 female caregivers reporting low caregiving-related stress; e2: 156 female caregivers reporting high caregiving-related stress; e3: 375 female caregivers; f1: 1,993 White caregivers; f2: 1,510 African American caregivers; f3: 1,163 caregivers reporting no strain; f4: 1,748 caregivers reporting moderate strain; f5: 578 caregivers reporting high strain; f6: 537 spouse caregivers reporting moderate or high strain; f7: 1,915 caregivers providing less than 14hr of care; f8: 1,588 caregivers providing 14 or more hours of care; f9: 2,219 female caregivers; f10: 1,284 male caregivers; f11: 786 spousal caregivers; f12: 1,197 adult child caregivers; f13: 3,503 caregivers (all subgroups included).
Table 1.
Summary of Population-Based Studies of the Impact of Caregiving on All-Cause Mortality
| Study | Total no. of citations/2014 citationsa | Key features of caregiver definition | Caregiving sample | Noncaregiving sample | Total N | No. of years of follow-up | Effect (e.g., Adj HR, RR) and 95% confidence interval |
|---|---|---|---|---|---|---|---|
| Schulz and Beach (1999) | 2,429/156 | Helped spouse; combined with strain of providing help; type of help or hrs/ week not specified | 179 strained caregivers of spouses with disabilities | 429 spouses of persons without a disability | 608 | 4.5 | 1.63 (1.00–2.65) |
| 138 unstrained caregivers of spouses with disabilities | 429 spouses of persons without a disability | 568 | 4.5 | 1.08 (0.61–1.90) | |||
| 317 caregivers of spouses with disabilities | 429 spouses of persons without a disability | 746 | 4.5 | 1.37b (0.90–2.07) | |||
| Brown and colleagues (2009) | 90/25 | Care recipient reported whether received help with one or more ADLs/IADLs from spouse, and number of hours/week spouse helped | 338 caregivers providing 14 or more hours of care to spouses with disabilities | 2,732 spouses providing 0hr of care for spouses with disabilities | 3,070 | 7 | 0.64 (0.45–0.90) |
| 306 caregivers providing 1–14hr of care to spouses with disabilities | 2,732 spouses providing 0hr of care for spouses with disabilities | 3,038 | 7 | 0.92 (0.69–1.24) | |||
| 655 caregivers providing any care to a spouse with ADL/IADL impairment | 2,732 spouses providing 0hr of care for spouses with disabilities | 3,387 | 7 | 0.79b (0.66–0.94) | |||
| O’Reilly and colleagues (2008) | 39/9 | Caregiver looks after or helps family member, friend, or neighbor because of long term physical or mental ill-health or disability | 162,884 Northern Ireland Census respondents who reported one or more hours of caregiving | 974,450 Northern Ireland Census respondents who reported no caregiving | 1,137,334 | 4 | 0.74b (0.71–0.76) |
| Ramsay, Grundy, and O’Reilly (2013) | 2/1 | Same definition as O’Reilly and colleagues (2008). | 31,393 English/Wales Census respondents who reported one or more hours of caregiving | 146,975 English/Wales Census respondents who reported no caregiving | 178,368 | 8 | 0.83b (0.79–0.88) |
| Fredman and colleagues (2010) | 34/5 | Caregiver helps a relative or friend with one or more ADLs/IADLs because the care recipient has physical, emotional, or cognitive limitations | 375 women providing care for a relative or friend with ADL/IADL impairment | 694 women who report no care for a person with ADL/IADL impairment | 1,069 | 8 | 0.74 (0.56–0.89) |
| Roth and colleagues (2013) | 4/4 | Caregiver provides care to family member with chronic illness or disability… may include watching family member, dressing, bathing, arranging care, or providing transportation | 3,503 caregivers for a family member with a chronic illness or disability | 3,503 noncaregivers matched on a propensity score from 15 demographic and health history variables | 7,006 | 6 | 0.82 (0.70–0.97) |
aNumber of citations according to Google Scholar on November 3, 2014.
bEstimates calculated from combining groups and effect sizes from the original articles.
Although not reported in the original Schulz and Beach (1999) article, an overall caregiving effect can be calculated by combining the effects reported in the article for the two spouse caregiving subgroups. When the mortality data for spouse caregivers with and without caregiving strain were combined and compared with the spouses of nondisabled CHS participants, the overall caregiving mortality effect was not statistically significant (RR = 1.37, 95% CI = 0.90–2.07, line a3 in Figure 1).
The five subsequent population-based mortality studies vary in their details, such as the specific caregiving questions used, who comprised the noncaregiving comparison group, the different caregiving subgroups examined, the covariates included in the analytic models, and the length of the follow-up period (4–8 years). There is, however, one consistent finding across all five subsequent population-based studies: Caregivers, as a general group, have significantly reduced mortality rates compared to their respective noncaregiving reference groups.
Brown and colleagues (2009) found that married persons in the HRS who provided 14 or more hours of care per week to their spouses with ADL or IADL problems had reduced mortality rates over a seven-year period compared to spouses who provided no such care after adjusting for care recipient variables and other demographics (adjusted HR = 0.64, 95% CI = 0.45–0.90, line b1 in Figure 1). Spouses who provided one to 14hr of care did not show a survival benefit (adjusted HR = 0.92, 95% CI = 0.69–1.24, line b2 in Figure 1), but when the overall caregiving effect was calculated, HRS spouse caregivers were found to have a significant survival advantage compared to the spouses who were providing no care (HR = 0.79, 95% CI = 0.66–0.94, line b3 in Figure 1). In this study, caregivers were identified by the person receiving help: that is, the care recipients reported whether their spouses helped them with ADLs or IADLs and the number of hours per week this help was provided. Thus, this definition reflects intensity according to the amount of time a caregiver helps, as opposed to caregiver-reported psychological strain (Fredman et al., 2010; Roth et al., 2013; Schulz & Beach, 1999). Moreover, care recipients with severe cognitive impairment were under-represented due to their inability to identify the amount of assistance provided, which may have resulted in a less-stressed sample of caregiver than other studies.
Fredman and colleagues (2010) examined the mortality rates of older women enrolled in the Caregiver-Study of Osteoporotic Fractures. After adjusting for demographics, baseline health covariates, and general perceived stress, women who were also informal caregivers had significantly lower 8-year mortality rates than noncaregiving women (adjusted HR = 0.74, 95% CI = 0.56–0.89, line e3 in Figure 1). Caregivers were defined by whether they assisted a relative or friend with one or more ADLs or IADLs because that person had physical, psychological, or cognitive impairments. Perceived stress was assessed in all participants, thereby allowing comparisons of mortality rates in stressed caregivers and stressed noncaregivers to nonstressed noncaregivers. The Fredman and colleagues (2010) study is the only one summarized in Table1 and Figure 1 that was restricted to female caregivers only.
Using data from a national epidemiologic study, Roth and colleagues (2013) compared mortality rates for 3,503 caregivers who were individually matched with 3,503 noncaregivers using propensity scores derived from 15 demographic, health history, and health behavior variables. The propensity score method first calculated the probability of being a caregiver based on the 15 covariates, and then matched each actual caregiver with a noncaregiver who had the same propensity score. This method efficiently balanced the caregiver and noncaregiver groups on multiple confounders that could have otherwise biased the caregiving-mortality associations. The results indicated that caregivers had an 18% survival advantage over a 6-year period compared to the propensity-matched noncaregivers (HR = 0.82, 95% CI = 0.70–0.97, line f13 in Figure 1). Several caregiving subgroups were also analyzed based on caregiver gender, race, relationship with the care recipient, and caregiving strain, and none of the subgroups showed significantly increased mortality relative to their own propensity-matched control group. Caregivers were defined by their self-report of currently providing care on on-going basis to a family member with chronic illness or disability, such as watching the family member, dressing, bathing, arranging care, or providing transportation. This broad definition captured persons who provided minimal caregiving (i.e., only “watching” their family member) along with those providing assistance with basic ADLs. Furthermore, assessment of hours/week caregiving and amount of caregiving strain provided comparisons with other studies (Schulz & Beach, 1999; Brown et al., 2009).
Additional analyses of large datasets thought to represent the entire population of Northern Ireland (O’Reilly et al., 2008) and England and Wales (Ramsay et al., 2013) have yielded similar survival benefits for caregivers compared to corresponding noncaregivers. The unusually narrow confidence intervals in Figure 1 for the effects from these studies reflect their very large sample sizes. Both of these studies defined caregivers according to respondents’ report of looking after or helping a family member, friend, or neighbor because of long-term physical or mental ill-health, disability, or problems related to old age. This definition did not address the tasks performed by the caregiver, although analyses did compare caregivers according to the number of hours per week that they provided care.
Although the Schulz and Beach (1999) study is often cited as a representative finding of increased mortality risk for caregivers compared to noncaregivers, it is important to clarify that those analyses were conducted only for spouses, and that increased mortality was only found for spouse caregivers who reported some caregiving strain. Two of the subsequent studies have further examined the effect of caregiving stress or strain on mortality, and neither has confirmed an increased mortality risk even for caregivers under high stress. Specifically, Fredman and colleagues (2010) found that caregivers reporting high caregiving-related stress did not show differences in mortality compared to noncaregiving women (adjusted HR = 1.00, 95% CI = 0.71–1.41, line e2 in Figure 1), whereas caregivers with low levels of caregiving-related stress had a significantly reduced risk of mortality compared to their noncaregiving counterparts (adjusted HR = 0.57, 95% CI = 0.38–0.84; line e1 in Figure 1). Similarly, Roth and colleagues (2013) found that caregivers reporting high caregiving strain did not differ in mortality when compared to their propensity-matched noncaregiving controls (adjusted HR = 1.02, 95% CI = 0.68–1.54, line f5 in Figure 1).
Media and Policy Representations of Caregiving and Health
Research reporting that caregiving is associated with increased mortality and other negative physical health effects, such as increased inflammation (Gouin et al., 2012; Kiecolt-Glaser et al., 2003), reduced immune system functioning (Lovell & Wetherell, 2011), and reduced telomere length (Epel et al., 2004), has been featured prominently in media reports, caregiver-oriented web pages, and in government and nonprofit organizations’ reports, usually to heighten concerns about caregiving and to emphasize the need for caregiver support services. Web pages for caregiver organizations commonly state that spouse caregivers have 63% higher mortality rates than noncaregivers (e.g., Rozman, 2013) and similar assertions have been made in Administration on Aging reports (e.g., Administration on Aging, 2012). Two different caregiving web sites have stated that caregiving can “take as much as 10 years off a family caregiver’s life” (Caregiver Action Network, 2012; Rozman, 2013). A September 2013 news report about a case of caregiver homicide and suicide included the statement that “those burdens are so great they can shave years off the life of caregivers, experts say. In fact, one study showed that, compared with others, caregiver spouses aged 66–96 had a 63% higher mortality rate” (Carroll, 2013). A prominent journalist (Sheehy, 2010) reported that “the most devoted family caretakers are at risk of dying first themselves.” It is extremely rare to find contrasting statements in such communications about caregiving and reduced mortality risk or potential health benefits. The message is clearly out that informal caregiving is, in general, a stressful obligation that is hazardous to the caregivers’ health. However, a more balanced view of the entire body of population-based studies, especially those examining actual mortality, appear to suggest a different overall conclusion.
Research, Practice, and Policy Implications
Over the past decades, research on caregiving has advanced from cross-sectional studies that generally found worse self-reported health status in caregivers compared to noncaregivers, to prospective, population-based studies that often find lower mortality and better health outcomes in caregivers. What lessons can be learned to design more scientifically rigorous studies of caregiving health outcomes in the future? The following recommendations are offered to integrate this updated review of studies on health effects of caregiving into research, practice, and policy.
1. More rigorous methods should be routinely employed in future studies on the health effects of caregiving. It is important to ensure in future research that caregivers and noncaregivers are selected from the same population. A volunteer sample of high functioning and socially active noncaregivers is unlikely to represent a suitable comparison group for a sample of caregivers because active volunteers tend to be healthier than the general population. Furthermore, evidence suggests that older adults who become caregivers are healthier than same-aged noncaregivers (McCann et al., 2004); thus, it is important to be aware of potential confounds due to selection differences and to minimize those confounds when possible. In large enough samples, propensity score matching can be done (Roth et al., 2013), but in smaller samples, use of propensity scores as a covariate adjustment, or matching on a smaller set of variables, could be used to achieve better balance. It is also known that caregiving status can change over time (McCann et al., 2004), so prospective studies should consider re-assessing and updating caregiving status at follow-up interviews, and to incorporate caregiving as a time- varying factor in the analyses of health outcomes. Because caregiving can be both psychologically challenging and provide gratification and a sense of purpose simultaneously (Beach et al., 2000), measurements of both positive and negative factors should be obtained. Measures of perceived stress, social support, and other resources should be obtained from both caregivers and noncaregivers in order to better quantify differences, and to better understand their complementary roles in shaping caregiving health outcomes.
2. Caregivers should be better recognized as integral to healthcare and viewed as partners by healthcare providers. An increasing number of aging Americans will become caregivers in the coming years. Many will have had no prior caregiving experience and will lack sufficient knowledge to prepare them for these roles. If providers see caregivers as being vulnerable and at risk for health care problems themselves, they may limit the extent to which they burden caregivers with more responsibilities to learn more about their care recipients’ problems and to assist with treatment implementation and adherence. More work to systematically include caregivers as medical visit companions and to provide them with helpful tools and information that would help them perform better in that role is needed (e.g., Wolff & Roter, 2008; Wolff et al., 2014). This work would be strengthened by a more balanced image of the caregiver as a resilient and capable ally, as opposed to characterizing caregivers as vulnerable and at-risk co-patients. Information about resources (e.g., education, skill building), as well as the health effects of caregiving, could be better disseminated to healthcare providers, who could then work more effectively with patients to identify, inform, and partner with their family caregivers. Indeed, communication and preparation for caregiving before it becomes a crisis has been found to reduce stress and family conflict (Ingersoll-Dayton et al., 2003).
3. Primary family caregivers should be supported with additional resources, including secondary caregivers. In many cases, the single primary family caregiver model needs to be supplemented and extended with additional resources. These resources could include economic relief, such as insurers compensating primary caregivers when institutional placements can be avoided and employers developing more accommodating policies that support family leaves of absence to assist aging parents. In addition, older adults with disabilities and their primary care providers should strive to achieve more integrated care and include informal care networks that extend beyond the single primary family caregiver. Having a network with both “primary” caregivers and “secondary” or supplemental caregivers would be beneficial in many cases. This could markedly extend the informal caregiving activities, including its challenges and health benefits, to other individuals within the family and even to persons outside of the care recipient’s family (e.g., friends, church-based volunteers, community health advisors).
4. Public statements, policy positions, and research articles should reflect a more updated and balanced view of caregiving. Family caregiving is stressful for some caregivers, and those caregivers should continue to receive valued supports such as respite care and evidence-based caregiver interventions. However, studies based on population-based samples using rigorous methods to control for confounding and that distinguish stress from caregiver status often show better health outcomes for caregivers. Those studies should be included in policy reports and research articles to present a more balanced and comprehensive view of the current state of caregiving research. Moreover, findings that show stress, but not caregiving status, is associated with poorer health outcomes (Fredman et al., 2010; Litzelman et al., 2014) provide justification for evidence-based stress-reduction programs and other supports. We can articulate the need for these services for caregivers without repeating and reinforcing a predominant narrative that providing care to a person with a disability is, in general, a highly stressful, overwhelming, and even dangerous activity. As described here, there is not an established finding that caregiving is associated with an increased risk for mortality. If anything, caregiving is associated with reduced mortality and increased longevity, possibly due to many underappreciated positive aspects of providing care to a loved one. The more balanced narrative could assist families to help older adults with disabilities live at home, with the best quality of life possible, and to do so with the full expectation of enjoying a gratifying caregiving experience.
Acknowledgments
The authors would like to thank Jin Huang for technical assistance in calculating the combined effect sizes and the corresponding 95% confidence intervals, and Orla Sheehan for her assistance in constructing Figure 1.
References
- Administration on Aging. (2012, March 2). $1.3 billion to improve the health and independence of America’s older adults Retrieved from http://www.acl.gov/NewsRoom/Press_Releases/archive/2012/March/2012_03_02.aspx
- Amirkhanyan A. A., Wolf D. A. (2003). Caregiver stress and noncaregiver stress: Exploring the pathways of psychiatric morbidity. The Gerontologist, 43, 817–827.doi:10.1093/geront/43.6.817. [DOI] [PubMed] [Google Scholar]
- Beach S. R., Schulz R., Yee J. L., Jackson S. (2000). Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging, 15, 259–271.doi:10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- Brown R. M., Brown S. L. (2014). Informal caregiving: A reappraisal of effects on caregivers. Social Issues and Policy Review, 8, 74–102. doi:10.1111/sipr.12002 [Google Scholar]
- Brown S. L., Smith D. M., Schulz R., Kabeto M. U., Ubel P. A., Poulin M.,…, Langa K. M. (2009). Caregiving behavior is associated with decreased mortality risk. Psychological Science, 20, 488–494. doi:10.1111/j.1467-9280.2009.02323.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caregiver Action Network. (2012). Statistics on family caregivers and family caregiving. Retrieved from http://www.caregiveraction.org/statistics/ [Google Scholar]
- Carroll L. (2013, September 5). Alzheimer’s extracts a high price on caregivers, too . NBC News. Retrieved from http://www.today.com/health/alzheimers-extracts-high-price-caregivers- too-8C11070658 [Google Scholar]
- Centers for Disease Control and Prevention. (2010). Caregiving: A public health priority. Retrieved from http://www.cdc.gov/aging/caregivinghttp://www.cdc.gov/aging/caregiving [Google Scholar]
- Epel E. S., Blackburn E. H., Lin J., Dhabhar F. S., Adler N. E., Morrow J. D., Cawthon R. M. (2004). Accelerated telomere shortening in response to life stress. Proceedings of the National Academy of Sciences of the United States of America, 101, 17312–17315. doi:10.1073/pnas.0407162101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredman L., Cauley J. A., Hochberg M., Ensrud K. E., Doros G. (2010). Mortality associated with caregiving, general stress, and caregiving-related stress in elderly women: Results of caregiver-study of osteoporotic fractures. Journal of the American Geriatrics Society, 58, 937–943. doi:10.1111/j.1532-5415.2010.02808.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher-Thompson D., Shurgot G. R., Rider K., Gray H. L., McKibbin C. L., Kraemer H. C.,…, Thompson L. W. (2006). Ethnicity, stress, and cortisol function in Hispanic and non-Hispanic white women: A preliminary study of family dementia caregivers and noncaregivers. American Journal of Geriatric Psychiatry, 14, 334–342. [DOI] [PubMed] [Google Scholar]
- Gillick M. R. (2013). The critical role of caregivers in achieving patient-centered care. JAMA, 310, 575–576. doi:10.1001/jama.2013.7310 [DOI] [PubMed] [Google Scholar]
- Gouin J. P., Glaser R., Malarkey W. B., Beversdorf D., Kiecolt-Glaser J. (2012). Chronic stress, daily stressors, and circulating inflammatory markers. Health Psychology, 31, 264–268. doi:10.1037/a0025536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmell A. L., Chattillion E. A., Roepke S. K., Mausbach B. T. (2011). A review of the psychobiology of dementia caregiving: A focus on resilience factors. Current Psychiatry Reports, 13, 219–224. doi:10.1007/s11920-011-0187-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll-Dayton B., Neal M. B., Ha J. H., Hammer L. B. (2003). Collaboration among siblings providing care for older parents. Journal of Gerontological Social Work, 40, 51–66. doi:10.1300/j083v40n03_05 [Google Scholar]
- Kiecolt-Glaser J. K., Preacher K. J., MacCallum R. C., Atkinson C., Malarkey W. B., Glaser R. (2003). Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proceedings of the National Academy of Sciences, 100, 9090–9095. doi:10.1073/pnas.1531903100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton M. P., Moss M., Kleban M. H., Glicksman A., Rovine M. (1991). A two-factor model of caregiving appraisal and psychological well-being. Journal of Gerontology, 46, 181–189. doi:10.1093/geronj/46.4.P181 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1984). Stress, appraisal, and coping. New York, NY: Springer. [Google Scholar]
- Litzelman K., Witt W. P., Gangnon R. E., Nieto F. J., Engelman C. D., Mailick M. R., Skinner H. G. (2014). Association between informal caregiving and cellular aging in the survey of the health of Wisconsin: The role of caregiving characteristics, stress, and strain. American Journal of Epidemiology, 179, 1340–1352. doi:10.1093/aje/kwu066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovell B., Wetherell M. A. (2011). The cost of caregiving: Endocrine and immune implications in elderly and non elderly caregivers. Neuroscience and Biobehavioral Reviews, 35, 1342–1352. doi:10.1016/j.neubiorev.2011.02.007 [DOI] [PubMed] [Google Scholar]
- McCann J. J., Hebert L. E., Bienias J. L., Morris M. C., Evans D. A. (2004). Predictors of beginning and ending caregiving during a 3-year period in a biracial community population of older adults. American Journal of Public Health, 94, 1800–1806. doi:10.2105/ajph.94.10.1800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B. S. (1998). Protective and damaging effects of stress mediators. The New England Journal of Medicine, 338, 171–179. doi:10.1056/NEJM199801153380307 [DOI] [PubMed] [Google Scholar]
- Monin J. K., Schulz R. (2009). Interpersonal effects of suffering in older adult caregiving relationships. Psychology and Aging, 24, 681–695. doi:10.1037/a0016355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving and AARP. (2009). Caregiving in the US. Bethesda, MD: National Alliance for Caregiving. [Google Scholar]
- National Opinion Research Center. (2014, May). Long term care in America: Expectations and realities. Retrieved from http://www.longtermcarepoll.org/PDFs/LTC%202014/AP-NORC-Long-Term%20Care%20in%20America_FINAL%20WEB.pdf [Google Scholar]
- O’Reilly D., Connolly S., Rosato M., Patterson C. (2008). Is caring associated with an increased risk of mortality? A longitudinal study. Social Science & Medicine (1982), 67, 1282–1290. doi:10.1016/j.socscimed.2008.06.025 [DOI] [PubMed] [Google Scholar]
- Okun M. A., Yeung E. W., Brown S. (2013). Volunteering by older adults and risk of mortality: A meta-analysis. Psychology and Aging, 28, 564–577. doi:10.1037/a0031519 [DOI] [PubMed] [Google Scholar]
- Ory M. G., Hoffman R. R., III, Yee J. L., Tennstedt S., Schulz R. (1999). Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. The Gerontologist, 39, 177–185. doi:10.1093/geront/39.2.177 [DOI] [PubMed] [Google Scholar]
- Pearlin L. I., Lieberman M. A., Menaghan E. G., Mullan J. T. (1981). The stress process. Journal of Health and Social Behavior, 22, 337–356. doi:10.2307/2136676 [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250–267. doi:10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Pruchno R. A., Brill J. E., Shands Y., Gordon J. R., Genderson M. W., Rose M., Cartwright F. (2008). Convenience samples and caregiving research: How generalizable are the findings? The Gerontologist, 48, 820–827. doi:10.1093/geront/48.6.820 [DOI] [PubMed] [Google Scholar]
- Ramsay S., Grundy E., O’Reilly D. (2013). The relationship between informal caregiving and mortality: An analysis using the ONS Longitudinal Study of England and Wales. Journal of Epidemiology and Community Health, 67, 655–660. doi:10.1136/jech-2012-202237 [DOI] [PubMed] [Google Scholar]
- Roth D. L., Haley W. E., Hovater M., Perkins M., Wadley V. G., Judd S. (2013). Family caregiving and all-cause mortality: Findings from a population-based propensity-matched analysis. American Journal of Epidemiology, 178, 1571–1578. doi:10.1093/aje/kwt225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth D. L., Perkins M., Wadley V. G., Temple E. M., Haley W. E. (2009). Family caregiving and emotional strain: Associations with quality of life in a large national sample of middle-aged and older adults. Quality of Life Research, 18, 679–688. doi:10.1007/s11136-009-9482-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozman D. (2013). Managing stress when you’re a caregiver. Care2. Retrieved from http://www.care2.com/greenliving/managing-stress-when-youre-a-caregiver.html
- Schulz R., Beach S. R. (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA, 282, 2215–2219. doi:10.1001/jama.282.23.2215 [DOI] [PubMed] [Google Scholar]
- Schulz R., Sherwood P. (2008). Physical and mental health effects of family caregiving. The American Journal of Nursing, 108(9 Suppl), 23–27. doi:10.1097/01.NAJ.0000336406.45248.4c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehy G. (2010, July 5). The caregiving boomerang. Newsweek, 156, 70–72. [Google Scholar]
- Vitaliano P. P., Zhang J., Scanlon J. M. (2003). Is caregiving hazardous to one’s health? A meta-analysis. Psychological Bulletin, 129, 946–972. doi:10.1037/e323652004-001 [DOI] [PubMed] [Google Scholar]
- von Känel R., Dimsdale J. E., Mills P. J., Ancoli-Israel S., Patterson T. L., Mausbach B. T., Grant I. (2006). Effect of Alzheimer caregiving stress and age on frailty markers interleukin-6, C-reactive protein, and D-dimer. Journal of Gerontology. Series A, Biological Sciences and Medical Sciences, 61, 963–969. doi:10.1093/gerona/61.9.963 [DOI] [PubMed] [Google Scholar]
- Wahbeh H., Kishiyama S. S., Zajdel D., Oken B. S. (2008). Salivary cortisol awakening response in mild Alzheimer disease, caregivers, and noncaregivers. Alzheimer Disease and Associated Disorders, 22, 181–183. doi:10.1097/WAD.0b013e31815a9dff [DOI] [PubMed] [Google Scholar]
- Wolff J. L., Roter D. L. (2008). Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Archives of Internal Medicine, 168, 1409–1415. doi:10.1001/archinte.168.13.1409 [DOI] [PubMed] [Google Scholar]
- Wolff J. L., Roter D. L., Barron J., Boyd C. M., Leff B., Finucane T. E.,…, Gitlin L. N. (2014). A tool to strengthen the older patient-companion partnership in primary care: Results from a pilot study. Journal of the American Geriatrics Society, 62, 312–319. doi:10.1111/jgs.12639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarit S. H., Reever K. E., Bach-Peterson J. (1980). Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist, 20, 649–655. doi:10.1093/geront/20.6.649 [DOI] [PubMed] [Google Scholar]