Abstract
Objective
To describe the technique and analyze the outcomes of joint‐preserving surgical treatments which included anatomical reconstruction or alignment correction for talar malunions or nonunions, and avoid development of degenerative changes in the adjacent joints.
Methods
Eight patients who had painful talar malunions or nonunions treated between 2009 and 2015 were included in this retrospective study. The mean age of the patients was 35.6 years, with patients aged from 18 to 58 years. Two patients had talar neck fractures and six had talar body fractures. According to a classification of post‐traumatic talar deformities, five patients were classified as type I (malunion and/or residual joint displacement), two as type II (nonunion with displacement), and one as type III (malunion with partial avascular necrosis [AVN]). Of these patients, six cases were treated with an osteotomy through the malunited fracture or removal of the pseudarthrosis, and two cases were corrected by supramalleolar or calcaneal osteotomies owing to complete disappearance of the former fracture lines. The follow‐up evaluation methods included the 36‐Item Short Form Health Survey (SF‐36) score, the American Orthopaedic Foot and Ankle Society (AOFAS) score, range of motion (ROM), and radiological analysis. The differences between postoperative scores and preoperative scores were evaluated statistically with the paired Student's t‐test. Significance was assumed at P < 0.05.
Results
The mean follow‐up time was 25.6 months. No wound healing problems or infections were observed. Solid union was obtained without redislocation in all cases, and with no signs of development or progression of AVN. At a mean of 25.6 months (range, 16–36 months) after reconstruction, all patients were satisfied with the result. The mean AOFAS score increased from 30.0 ± 7.0 pre‐operatively to 86.5 ± 7.8 post‐operatively (P < 0.001), the mean SF‐36 score increased from 38.8 ± 4.1 to 81.4 ± 7.7 (P < 0.001), and the average ROM (tibiotalar joint) increased from 40.5° ± 8.7° to 43.9° ± 7.2° (P < 0.05).
Discussion
Joint‐preserving procedures for talar malunions or nonunions can bring about satisfactory outcomes, and the appropriate procedure should be adopted according to different types of post‐traumatic deformities.
Keywords: Correction osteotomy, Fracture, Malunion, Nonunion, Talus
Introduction
The talus has a unique anatomical shape and function. As a “bony meniscus” without direct muscle attachments, it functions as the junction between the lower leg and the foot1. The talus contributes to three essential joints of the foot and approximately two‐thirds of its surface is covered by cartilage. Talus fractures account for less than 1% of all fractures2. The malunion rate of talus fractures varies from 9 to 47%3. Given the immense importance of the anatomical integrity of the talus and its joints, malunions or nonunions after talar fractures almost invariably lead to disabling impairment of global foot function.
The most common deformity after malunion of a talus fracture is varus malalignment of the talar neck4, 5. Varus malalignment of the talar neck results in substantial shortening of the medial column, with resulting locking of the hindfoot in varus and internal rotation6. Malalignment of 2 mm at the talar neck can lead to considerable load redistribution between the posterior, middle, and anterior facets of the subtalar joints7.
Talar body fractures and malunions can be divided into central and peripheral fractures1. Central fractures of the talar body are typically produced by high‐energy forces, while peripheral fractures (talar process fractures) result from shearing forces, such as force during subtalar dislocations8, 9. Malunions and nonunions of central talar fractures are frequently caused by inadequate reduction and fixation, or non‐operative treatment of displaced talar body fractures, while peripheral fractures of the lateral or posterior process may be overlooked in the wake of subtalar dislocations or other injuries10, 11. Even minor step‐offs of 2 mm in the talar body will produce significant load shifts within the affected joint, potentially leading to post‐traumatic arthritis7. Any axial deviation of the talar body will inevitably lead to a 3‐dimensional malposition of the hindfoot, severely affecting overall foot function. Malunions of the lateral talar process may rapidly give rise to subtalar arthritis7. In addition to malposition and instability caused by malunion and nonunion, the impact during the initial injury that produces a talar body fracture will inevitably result in chondrocyte death, further contributing to the development of post‐traumatic arthritis7.
Avascular necrosis (AVN) of the talar body is a specific complication after talar fractures. Its occurrence depends on the degree of initial dislocation and the overall severity of the injury12, 13. Undisplaced talar body fractures (Marti type II) are associated with AVN in 5%–44% of patients, while displaced talar body fractures (Marti types III and IV) carry an overall risk of approximately 50%1.
Clinical studies have demonstrated that patients with talar malunions have poor outcomes related to overload of the lateral foot with painful callus formation on the lateral plantar side14, 15. Patients who present with substantially reduced range of motion (ROM) in the subtalar and midtarsal joints often suffer pain and rigidity in the foot with cavovarus alignment. The talar neck malalignment may increase the chance of post‐traumatic osteoarthritis in the peritalar joint, which subsequently may result in substantial disability in daily activities14, 16.
At present, reorientating arthrodesis of the ankle, subtalar, and/or talonavicular joints are the main salvage procedures after talar malunions with joint involvement10. Although these procedures frequently result in substantial improvement, none of them will restore normal foot function. Joint‐preserving corrections aim at regaining a maximum of function while correcting the deformity and reducing pain. At the same time, the measure can avoid the development of degenerative changes in the adjacent joints. This article describes and analyzes the outcomes of procedures, including anatomic reconstruction or restoring alignment of lower limbs by supramalleolar and calcaneus osteotomies for talar malunions and nonunions; it also presents an overview of indications and techniques for joint‐preserving surgical procedures in complex conditions.
Patients and Methods
Between January 2009 and September 2015, eight patients who had painful talar malunions or nonunions were treated in our institution (Table 1). All patients were included and reviewed in this retrospective study. The mean age of the patients was 35.6 years, with patients aged from 18 to 58 years. This study comprised two talar neck fractures and six talar body fractures. According to the classification of post‐traumatic talar deformities (Zwipp and Rammelt, 2003, Table 2), five patients were classified as type I, two as type II and one as type III.
Table 1.
Demographic data for eight patients with talar malunions or nonunions
| Patient | Sex | Age (years) | Initial fracture | Deformity type (Zwipp) | Time of delay (months) | Surgery | Follow‐up (months) |
|---|---|---|---|---|---|---|---|
| 1 | M | 38 | Body | I | 16 | AR + BG | 26 |
| 2 | F | 18 | Body | II | 10 | AR + BG | 33 |
| 3 | F | 33 | Body | I | 20 | AR + BG | 28 |
| 4 | M | 49 | Body | I | 18 | SO + CO | 36 |
| 5 | F | 36 | Neck | I | 19 | AR + BG | 16 |
| 6 | F | 21 | Body | I | 9 | AR + BG | 27 |
| 7 | M | 58 | Neck | II | 11 | AR + BG | 18 |
| 8 | M | 32 | Body | II | 13 | SO + CO | 21 |
| Mean ± SD | 35.6 ± 13.3 | 14.5 ± 4.3 | 25.6 ± 7.0 |
AR, anatomical reconstruction; BG, bone graft; CO, calcaneal osteotomies; F, female; M, male; SO, supramalleolar osteotomies.
Table 2.
Classification of post‐traumatic talar deformities (Zwipp and Rammelt, 2003)
| Type | Talar deformities |
|---|---|
| Type I | Malunion and/or joint displacement |
| Type II | Nonunion with joint displacement |
| Type III | Types I/II with partial AVN |
| Type IV | Types I/II with complete AVN |
| Type V | Types I/II with septic AVN |
AVN, avascular necrosis.
Of these patients, six cases were treated with an osteotomy through the malunited fracture or removal of the pseudoarthrosis, and internal fixation was achieved with screws and additional bone grafting if necessary; two cases were corrected by supramalleolar or calcaneus osteotomies owing to the complete disappearance of the former fracture lines.
Physical Examinations and Imaging Study
Patients were physically examined by clinical assessment of the hindfoot while standing. Severe pain and tenderness around the ankle and hindfoot were observed in all patients, especially after walking. Six varus deformities and 1 valgus deformity could be observed only under physiologic load. Only one patient had no varus or valgus deformity. Toe walking helped to evaluate the calcaneus position. Hindfoot stability was assessed with routine physical examination. The function of joint‐crossing tendons was tested, in particular the peroneal tendons in the varus ankle, and the posterior tibial tendon in the valgus ankle. The ROM of the ankle joint was measured clinically using a goniometer placed along the lateral border of the leg and foot. All patients presented with substantially decreased range of motion in tibiotalar joint. The forefoot was assessed with regard to a plantar flexed first ray, forefoot supination, and toe deformities.
Radiographic assessment of peritalar instability includes anteroposterior (AP), lateral, and mortise views of the ankle and the dorsoplantar view of the foot. All radiographs were taken with weight‐bearing to assess the functional deformities of the hindfoot. To assess the calcaneus position in relationship to the longitudinal axis of the tibia, the Saltzman view (hindfoot alignment view) were taken. One single‐photon emission computed tomography (CT) scan was done to understand the deformity and to plan the osteotomies, particularly for biplanar corrections. According to the X‐rays, five patients had talar malunion and/or joint displacement, two had talar nonunion with joint displacement, and one had talar malunion or nonunion with partial AVN. CT scan further confirmed the X‐ray results.
Magnetic resonance imaging (MRI) was used to confirm the presence of talar AVN and to determine the extent of necrosis.
Surgical Technique
Patient position and surgical approach depended on the type and location of the deformity. For malunions or nonunions fractures of the talar neck we used an anteromedial approach, which allowed exposure of the ankle and talonavicular joints. For correction of malunions or nonunions of the talar body, a medial malleolar osteotomy was performed.
Procedure of Anatomic Reconstruction
All patients were in the supine position, under general anesthesia during surgery. Surgery was carried out with a tourniquet being placed at the ipsilateral thigh. According to the preoperative analysis, an anteromedial incision was carried out in a curved manner, starting approximately 3 cm above the medial malleolus and extending to the navicular tuberosity (Fig. 1). The medial joint capsule was opened, and the talar neck and anterior dome were exposed. Fibrous adhesions around the talus were released. Most talar body fractures would need an additional medial malleolar osteotomy to reliably access and reduce the malunited fragments. The holes for re‐fixation of the medial malleolus with two screws were predrilled at that stage. After completion of the procedures, the cartilage status was assessed by thorough inspection and probing of all accessible parts. Loose, nonviable fragments were excised. We treated solid malunions with correctional osteotomy along the former fracture plane. We performed a complete resection of the pseudarthrosis until viable bone became visible in cases with nonunion (Fig. 2). Anatomic realignment of the talar body with reconstruction of the ankle and subtalar joints was checked visually through the bilateral approaches. The fragments were fixed temporarily with K‐wires. Realignment of the talar body was controlled fluoroscopically. The resulting defect was filled with autologous bone grafting from the ipsilateral iliac crest or allograft bone grafting.
Figure 1.
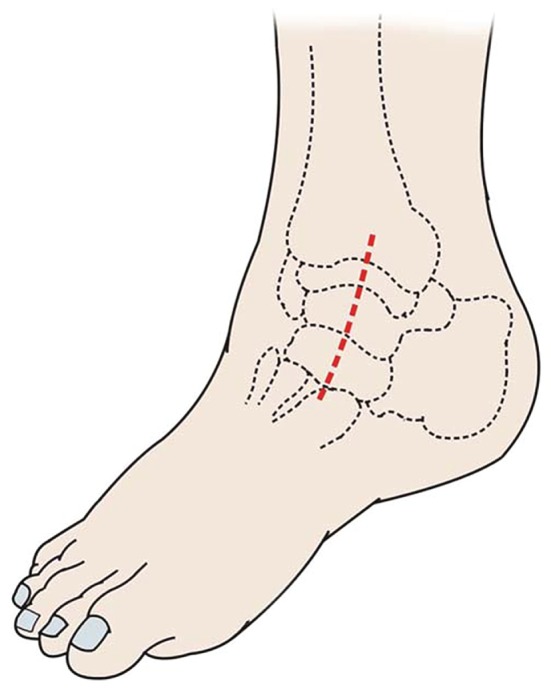
An anteromedial incision starting approximately 3 cm above the medial malleolus and extending to the navicular tuberosity.
Figure 2.
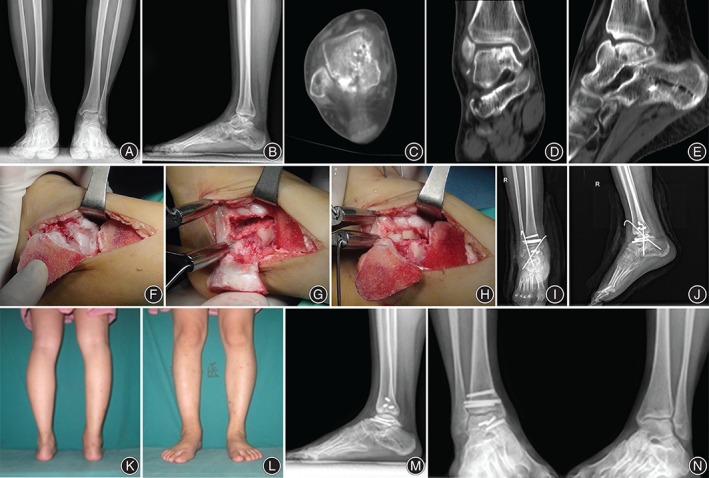
Reconstruction of a displaced talar nonunion (type II deformity). An 18‐year‐old woman presented with a talar nonunion and displacement at the talar body 10 months after a car accident. X‐rays in anteroposterior and lateral position with weight‐bearing (A, B) and computed tomography scans (C–E) were taken before the operation. The fracture had been overlooked initially. Treatment consisted of debridement of the pseudarthrosis (F, G) and allograft bone grafting (H). X‐rays after surgery showed a congruent joint reconstruction (I, J). At follow‐up after 1 year, the patient was pain free and had normal function of the ankle and subtalar joints (K–N).
A chisel was directed along the fracture plane. To determine the amount of distraction and rotational correction required of the talar head with regard to the talar body, we used a Hintermann distractor which was applied between two K‐wires, and allowed manipulation of the distracting forces and rotational movement until an appropriate correction of the forefoot was achieved. Once the desired position was achieved, the size of the graft was determined by measuring using a ruler. Human cancellous allograft blocks were used on a routine basis for interposition as the required size of graft was not considered critical for revascularizati. As a standard approach, two screws provided the required stability after the correcting osteotomy and graft insertion.
Procedure of Supramalleolar and Calcaneus Osteotomies
Before surgery, the correction was planned on the AP, lateral, or the Saltzman view radiographs. The tibial articular surface (TAS) angle (normal value, 91°–93°) was measured. Supramalleolar osteotomies would be performed for the patient with a varus or valgus deformity of the ankle, while the varus or valgus TAS angle was more than 4°. Calcaneus osteotomies would be performed for the patient with varus or valgus deformity of the calcaneus or hindfoot in the Saltzman view. After the supramalleolar osteotomie, a plate would be used for fixation. After the calcaneus osteotomie, at least two screws were used for rigid fixation. The aims of supramalleolar or calcaneal osteotomies were to realign the hindfoot, to transfer the ankle joint under the weight‐bearing axis, and to normalize the direction of the force vector of the triceps surae. An open or closing wedge osteotomy from medially or laterally, or, in severe deformities, a dome‐like osteotomy from anteriorly could be considered to achieve an overcorrection (Fig. 3). Any remaining deformity was addressed with an osteotomy of the calcaneus. The tuber calcanei were exposed through an oblique incision. A straight or Z‐shaped osteotomy was performed with the use of a saw and chisels, and the tuber was then moved medially or laterally as necessary. One or two screws were used for rigid fixation.
Figure 3.
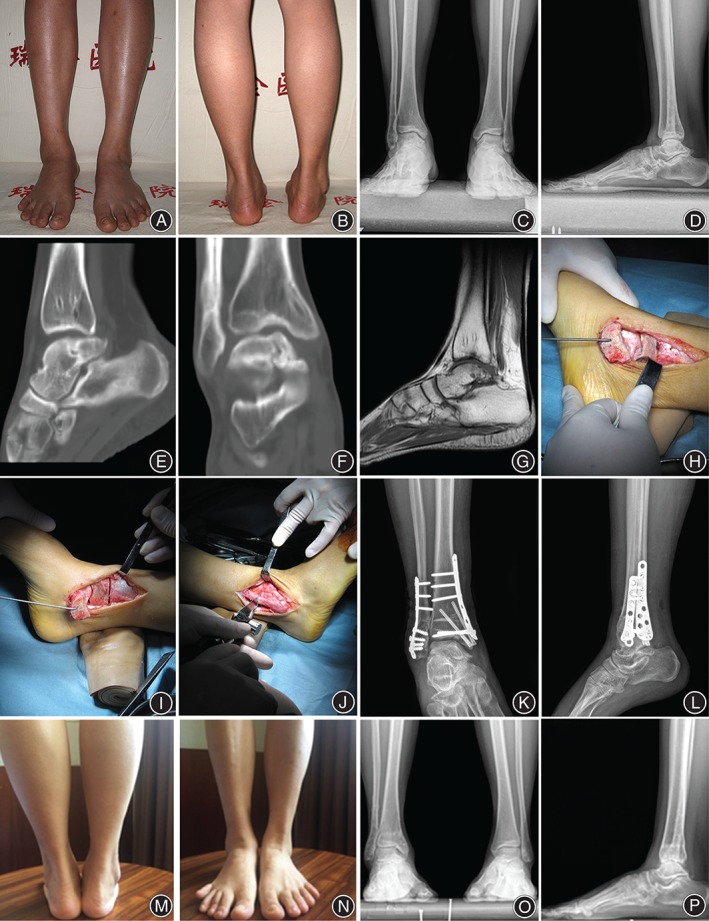
Correction of a displaced talar malunion (type I deformity). A 49‐year‐old man presented with a talar malunion and displacement at the talar body 18 months after a severe injury and the former fracture line almost disappeared. Appearance photo of anterior and posterior position with weight‐bearing (A, B), anteroposterior and lateral X‐rays (C, D), computed tomography scan (E, F), and magnetic resonance imaging (G) before operation show talar malunion with a fair joint facet, malalignment, and disappearance of the fracture lines. Treatment consisted of debridement of the ankle joint and supramalleolar or fibular osteotomies (H–J) and allograft bone grafting (I). X‐rays after surgery showed a congruent joint and a fair alignment (K, L). At follow‐up after 2 years, the patient was pain free and had normal function of the ankle and subtalar joints (M–P).
Postoperative Management
Postoperatively, a short leg cast was applied for 2–3 weeks until the suture removal, which relieved early pain and allowed soft tissue recovery. ROM exercises of the forefoot were started at 24 h postoperatively. After the plaster was removed, functional exercises of the ankle and subtalar joints were started. Partial weight‐bearing was commenced as tolerated by the patients at 6 weeks postoperatively. Full weight‐bearing was allowed after radiographic evidence of bone union at an average of 14 weeks postoperatively.
Postoperative Evaluations
During the follow‐up, the hindfoot alignment, the bony union and the presence or absence of AVN of the talus were assessed. Radiographs were taken monthly in the first 3 postoperative months. Thereafter, patients were generally followed every 3 months, which changed to every 6 months 1 year later. In addition to the radiographs, the patients with severe type of deformity (type II and type III) were examined with CT scans to evaluate the arthritic changes, and MRI was used to evaluate the development of AVN. Meanwhile, patients were assessed with respect to subjective satisfaction, pain, early wound complications, level of activity, muscular and tendinous problems, and so on. The follow‐up evaluations included determination of the 36‐Item Short Form Health Survey (SF‐36) score, the American Orthopaedic Foot and Ankle Society (AOFAS) score, ROM evaluation, and radiological analysis. At the last follow‐up, the outcomes were recorded and compared with the preoperative data.
Statistic Analysis
Results were expressed with descriptive methods (mean, range). The differences between postoperative scores and preoperative scores were evaluated statistically with the paired Student's t‐test. Significance was assumed at P < 0.05.
Results
General Results
The mean duration of operations was 90 ± 14 min. The mean follow‐up duration was 25.6 months, with the minimum and maximum follow‐up time being 16–36 months, respectively, and all patients were satisfied with the result at the last follow‐up. The mean duration of bone healing was 15 ± 2 days.
Complications
There were no intraoperative complications. No blood transfusions were required, and no nerve lesions occurred. Wound healing occurred within 2 weeks of the surgery, without wound healing problems, including wound infections, dehiscence, wound edge necrosis, and breakdowns of the wound. No deep vein thromboses were seen. Solid union was obtained without re‐dislocation in all cases, with no signs of development or progression of AVN.
Outcomes
American Orthopaedic Foot and Ankle Society Score
The average AOFAS ankle‐hindfoot score significantly increased, from 30.0 ± 7.0 preoperatively to 86.5 ± 7.8 postoperatively (P < 0.001). All patients experienced substantial pain relief. According to the AOFAS rating system, the results were excellent in five patients, good in two patients, and fair in one patient at follow‐up (excellent was defined as a score of 85–100, good as 75–84, fair as 70–74, and poor as less than 70). No joint swelling, instability, or axial deformity of the affected joints was observed at the latest follow‐up physical examination. All patients were able to wear commercial shoes (see Table 3 and Fig. 4).
Table 3.
Comparisons of preoperative and postoperative data for eight patients with talar malunions or nonunions
| Patient | AOFAS score (points, maximum 100) | SF‐36 score (points, maximum 100) | ROM (°, tibiotalar joint) | |||
|---|---|---|---|---|---|---|
| Pre‐operation | Post‐operation | Pre‐operation | Post‐operation | Pre‐operation | Post‐operation | |
| 1 | 32 | 87 | 39 | 78 | 50 | 50 |
| 2 | 22 | 92 | 39 | 86 | 25 | 32 |
| 3 | 41 | 86 | 40 | 88 | 49 | 53 |
| 4 | 20 | 81 | 37 | 74 | 43 | 49 |
| 5 | 33 | 94 | 40 | 84 | 45 | 45 |
| 6 | 26 | 72 | 30 | 67 | 44 | 45 |
| 7 | 35 | 96 | 44 | 89 | 33 | 36 |
| 8 | 31 | 84 | 41 | 85 | 35 | 41 |
| Mean ± SD | 30.0 ± 8.0 | 86.5 ± 7.8 | 38.8 ± 4.1 | 81.4 ± 7.7 | 40.5 ± 8.7 | 43.9 ± 7.2 |
| P‐value | <0.001 | <0.001 | <0.05 | |||
AOFAS, American Orthopaedic Foot and Ankle Society; ROM, range of motion; SF‐36, 36‐item short form health survey.
Figure 4.
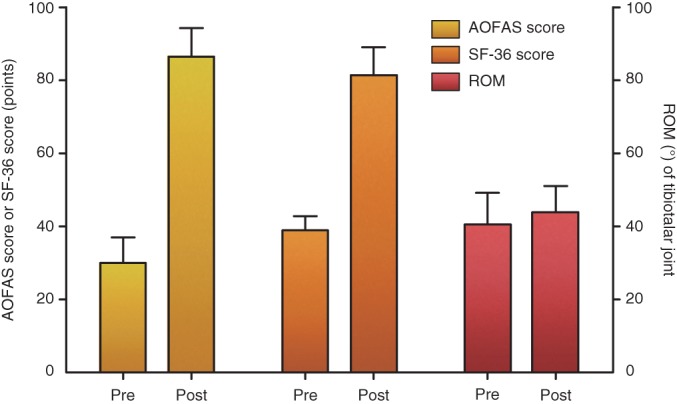
Comparisons of preoperative and postoperative data for eight patients with talar malunions or nonunions.
36‐Item Short Form Health Survey Score
The physical and mental categories of the SF‐36 score showed substantial improvements postoperatively. The average summarized components of the physical and mental outcomes scores improved from 38.8 ± 4.1 to 81.4 ± 7.7 (P < 0.001). At latest follow‐up, all patients were satisfied with the results (see Table 3 and Fig. 4).
Range of Motion
Patients presented with substantially increased range of motion in the tibiotalar joint. The average ROM of the tibiotalar joint increased by 3.4° (from 40.5° ± 8.7° preoperatively to 43.9° ± 7.2° postoperatively, P < 0.05) (see Table 3 and Fig. 4).
Discussion
The unique anatomy of the talus, with its contribution to three essential joints of the foot and two‐thirds of cartilage coverage, makes its anatomical integrity and joint congruency indispensable for normal foot function17, 18. The common complications associated with talar fractures include skin necrosis, osteomyelitis, AVN of the talus, malunion, nonunion, and post‐traumatic arthritis. Among the complications, malunion may be more common19, 20. For talar malunions or nonunions, the operation should be performed as early as possible to avoid secondary traumatic arthritis. Treatment of talar malunions or nonunions is challenging, and few studies addressed anatomic reconstruction as an alternative to arthrodeses. Although arthrodeses reportedly provided substantial pain relief, functional impairment prevails and the long‐term outcome is limited due to the development of degenerative changes in the adjacent joints21, 22.
When and how do you select the procedure of arthrodeses or joint‐preserving corrections? The choice of the best treatment for post‐traumatic talar deformities depends on patient‐related factors, including the amount of post‐traumatic arthritis, AVN, infection, and the quality of bone stock, patient compliance and limiting comorbidities23. Joint‐preserving corrections aim at regaining a maximum of function while correcting the deformity and reducing pain. Secondary anatomical reconstruction and internal fixation with preservation of all three joints can be pursued in active, compliant patients with type I, II or III deformities (Table 2). In the presence of symptomatic arthritis, with poor patient compliance or bone stock, and relevant comorbidities such as poorly controlled diabetes mellitus, stage IIb peripheral vascular disease, or systemic immune deficiency, fusion of the affected joints with axial realignment is the treatment of choice. Because radiographic arthritis is not always clinically symptomatic, and malalignment of the talus and its joints will invariably lead to severe pain around the ankle and hindfoot, the decision to reconstruct or fuse one or more peritalar joints will frequently be made intraoperatively while directly assessing cartilage loss and probing cartilage quality. Therefore, both joint reconstruction and fusion must be discussed with the patient prior to surgery10. Early malunions and nonunions of talar process fractures can be salvaged by complete excision of the malunited fragments24, 25. However, symptomatic subtalar arthritis develops rapidly after these injuries and in situ fusion of the subtalar joint may become necessary12, 26. MRI is a powerful tool in the preoperative assessment of arthritis and necrosis. However, it is better to make a decision regarding the arthrodesis on the basis of the intraoperative observation, which provides direct visualization of the articular cartilage (Fig. 2). In the presence of a complete AVN and collapse of the talar body (type IV deformities), excision of all necrotic bone, autologous bone grafting, realignment, and fusion of the affected joint(s) is the treatment of choice. In cases of osteomyelitis (type V deformities) repeated debridement of infected and necrotic bone will result in a subtotal talectomy.
On the selection of surgical approach, the talar neck and head are exposed via an anteromedial approach. For full exposure of the talar body, a medial malleolar osteotomy is need (Fig. 5). The lateral part of the talar neck and body, including the lateral process and subtalar joint, are accessed via a curved or oblique anterolateral approach27. Posterior approaches are used for malunions of the posterior process or the posterior third of the talar body1, 24. In most cases, a posterolateral approach a complete overview of the posterior part of the talar body. The flexor hallucis longus muscle and tendon are held away medially, thus protecting the tibial neurovascular bundle.
Figure 5.
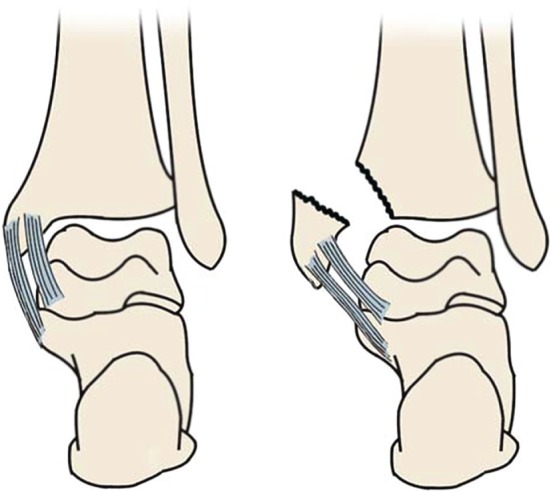
Diagrammatic depiction of medial malleolar osteotomy for talar malunions or nonunions.
Our group received appropriate management and gained satisfactory results. We provided a 25.6‐month follow‐up for the eight cases, including six cases of anatomic reconstruction and two cases of correction of alignment for talar malunions and nonunions, and evaluated the functional outcomes using the SF‐36 score, AOFAS score, ROM evaluation and radiological analysis. The function of the hindfoot improved significantly. The mean AOFAS ankle‐hindfoot score increased from 30.0 ± 7.0 to 86.5 ± 7.8 (P < 0.001). The mean SF‐36 score increased from 38.8 ± 4.1 to 81.4 ± 7.7 (P < 0.001). The mean ROM (tibiotalar joint) increased from 40.5° ± 8.7° to 43.9° ± 7.2° (P < 0.05). The mean postoperative AOFAS score was in accordance with other reports10, 20, 28. Most of our patients only had the majority of type I and type II deformities, for which reason anatomic reconstruction was performed. The operation was performed by senior surgeons and appropriate procedures were adopted, which also contributed to the favorable outcomes. Additional surgeries included hardware removal before the osteotomy in four cases. Additional lengthening of the Achilles tendon or the release of gastrocnemius muscle was required in four patients to achieve physiologic ROM. In one patient, an arthroscopy of the subtalar joint was performed to rule out posttraumatic osteoarthritis before the correctional osteotomy. To determine the amount of distraction and rotational correction required of the talar head with regard to the talar body, we used a Hintermann distractor, which was applied between two K‐wires, and allowed manipulation of the distracting forces and rotational movement until an appropriate correction of the forefoot was achieved.
Treatment of post‐traumatic malunions or nonunions following talar fractures is a challenging problem for the orthopedic surgeon. The secondary procedures in patients with painful malunited talar fracture include salvage procedures and an anatomic reconstruction of the talar bone29. The anatomic reconstruction has the major advantage in restoring the normal foot function in patients with preserved cartilage in peritalar joints and without evidence of extensile talar necrosis, collapse, or infection30. For young patients who have a talar malunion with a fair joint facet, malalignment, and disappearance of the fracture lines, supramalleolar or calcaneal osteotomies could be performed (Fig. 3).
Surgical treatment of joint‐preservation for talar malunions or nonunions can bring about satisfactory outcomes, and the appropriate procedure should be adopted according to different types of post‐traumatic deformities.
Disclosure: The authors no conflict of interest to declare.
References
- 1. Rammelt S, Zwipp H. Talar neck and body fractures. Injury, 2009, 40: 120–135. [DOI] [PubMed] [Google Scholar]
- 2. Santavirta S, Seitsalo S, Kiviluoto O, Myllynen P. Fractures of the talus. J Trauma, 1984, 24: 986–989. [DOI] [PubMed] [Google Scholar]
- 3. Fleuriau Chateau PB, Brokaw DS, Jelen BA, Scheid DK, Weber TG. Plate fixation of talar neck fractures: preliminary review of a new technique in twenty‐three patients. J Orthop Trauma, 2002, 16: 213–219. [DOI] [PubMed] [Google Scholar]
- 4. Baumhauer JF, Alvarez RG. Controversies in treating talus fractures. Orthop Clin North Am, 1995, 26: 335–351. [PubMed] [Google Scholar]
- 5. Canale ST, Kelly FB Jr. Fractures of the neck of the talus: long‐term evaluation of seventy‐one cases. J Bone Joint Surg Am, 1978, 60: 143–156. [PubMed] [Google Scholar]
- 6. Daniels TR, Smith JW, Ross TI. Varus malalignment of the talar neck: its effect on the position of the foot and on subtalar motion. J Bone Joint Surg Am, 1996, 78: 1559–1567. [DOI] [PubMed] [Google Scholar]
- 7. Sangeorzan BJ, Wagner UA, Harrington RM, Tencer AF. Contact characteristics of the subtalar joint: the effect of talar neck misalignment. J Orthop Res, 1992, 10: 544–551. [DOI] [PubMed] [Google Scholar]
- 8. Bibbo C, Anderson RB, Davis WH. Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases. Foot Ankle Int, 2003, 24: 158–163. [DOI] [PubMed] [Google Scholar]
- 9. Rammelt S, Goronzy J. Subtalar dislocations. Foot Ankle Clin, 2015, 20: 253–264. [DOI] [PubMed] [Google Scholar]
- 10. Rammelt S, Winkler J, Heineck J, Zwipp H. Anatomical reconstruction of malunited talus fractures: a prospective study of 10 patients followed for 4 years. Acta Orthop, 2005, 76: 588–596. [DOI] [PubMed] [Google Scholar]
- 11. Nyska M, Howard CB, Matan Y, et al. Fracture of the posterior body of the talus the hidden fracture. Arch Orthop Trauma Surg, 1998, 117: 114–117. [DOI] [PubMed] [Google Scholar]
- 12. Rammelt S, Winkler J, Grass R, Zwipp H. Reconstruction after talar fractures. Foot Ankle Clin, 2006, 11: 61–84. [DOI] [PubMed] [Google Scholar]
- 13. Zwipp H, Rammelt S. Secondary reconstruction for malunions and nonunions of the talar body. Foot Ankle Clin, 2016, 21: 95–109. [DOI] [PubMed] [Google Scholar]
- 14. Sproule JA, Glazebrook MA, Younger AS. Varus hindfoot deformity after talar fracture. Foot Ankle Clin, 2012, 17: 117–125. [DOI] [PubMed] [Google Scholar]
- 15. Monroe MT, Manoli A 2nd. Osteotomy for malunion of a talar neck fracture: a case report. Foot Ankle Int, 1999, 20: 192–195. [DOI] [PubMed] [Google Scholar]
- 16. Suter T, Barg A, Knupp M, Henninger H, Hintermann B. Surgical technique: talar neck osteotomy to lengthen the medial column after a malunited talar neck fracture. Clin Orthop Relat Res, 2013, 471: 1356–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hawkins LG. Fractures of the neck of the talus. J Bone Joint Surg Am, 1970, 52: 991–1002. [PubMed] [Google Scholar]
- 18. Lorentzen JE, Christensen SB, Krogsoe O, Sneppen O. Fractures of the neck of the talus. Acta Orthop Scand, 1977, 48: 115–120. [DOI] [PubMed] [Google Scholar]
- 19. Daniels TR, Smith JW. Talar neck fractures. Foot Ankle, 1993, 14: 225–234. [DOI] [PubMed] [Google Scholar]
- 20. Huang PJ, Cheng YM. Delayed surgical treatment for neglected or mal‐reduced talar fractures. Int Orthop, 2005, 29: 326–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long‐term results following ankle arthrodesis for post‐traumatic arthritis. J Bone Joint Surg Am, 2001, 83: 219–228. [DOI] [PubMed] [Google Scholar]
- 22. Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle: a study of madjacent joints. J Bone Joint Surg Br, 2003, 85: 994–998. [DOI] [PubMed] [Google Scholar]
- 23. Rammelt S, Zwipp H. Corrective arthrodeses and osteotomies for post‐traumatic hindfoot malalignment: indications, techniques, results. Int Orthop, 2013, 37: 1707–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Giuffrida AY, Lin SS, Abidi N, Berberian W, Berkman A, Behrens FF. Pseudo os trigonum sign: missed posteromedial talarfacet fracture. Foot Ankle Int, 2003, 24: 642–649. [DOI] [PubMed] [Google Scholar]
- 25. Langer P, Nickisch F, Spenciner D, Fleming B, DiGiovanni CW. In vitro evaluation of the effect lateral process talar excisionon ankle and subtalar joint stability. Foot Ankle Int, 2007, 28: 78–83. [DOI] [PubMed] [Google Scholar]
- 26. Sneppen O, Christensen SB, Krogsoe O, Lorentzen J. Fracture of the body of the talus. Acta Orthop Scand, 1977, 48: 317–324. [DOI] [PubMed] [Google Scholar]
- 27. Cronier P, Talha A, Massin P. Central talar fractures‐therapeutic considerations. Injury, 2004, 35: SB10–SB22. [DOI] [PubMed] [Google Scholar]
- 28. Rammelt S. Secondary correction of talar fractures: asking for trouble?. Foot Ankle Int, 2012, 33: 359–362. [DOI] [PubMed] [Google Scholar]
- 29. Ohl X, Harisboure A, Hemery X, Dehoux X. Long‐term follow‐up after surgical treatment of talar fractures: twenty cases with an average follow‐up of 7.5 years. Int Orthop, 2011, 35: 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Barg A, Suter T, Nickisch F, Wegner N, Hintermann B. Osteotomies of the talar neck for posttraumatic malalignment. Foot Ankle Clin, 2016, 21: 77–93. [DOI] [PubMed] [Google Scholar]


