ABSTRACT
Intellectual disability and autism spectrum disorder are neurodevelopmental disorders that emerge during the developmental period. A significant barrier that impedes the social adaptation of individuals with these disorders is the exhibition of problem behaviors, such as self-injurious, stereotyped, and aggressive/destructive behaviors. In recent years, these problem behaviors have been collectively referred to as “challenging behavior,” in accordance with the contention that they result from an interaction between the individual and his or her social environment. Evidence-based psychosocial interventions that adopt the functional approach to treating challenging behavior are increasing. However, in order to effectively implement such interventions in educational settings and welfare facilities, it is essential to develop staff training programs and usable psychometric assessments. Accordingly, a brief overview of research studies on challenging behavior that have been conducted in Japan, as well as the various support systems that are available to individuals who exhibit challenging behavior, are presented in this article. The discussion makes it apparent that, in order to improve treatment systems in Japan that are aimed at addressing challenging behavior, it is necessary to establish not only better staff training programs, but also reliable and valid assessments measuring challenging behavior that can be readily used by teachers and parents. On the basis of this discussion, it is proposed that technological advancements must be applied to psychosocial approaches in the study of problem behaviors, in order to develop assessment system using software applications and automatic measurement system of target behaviors using sensing technology.
Keywords: autism spectrum disorder, challenging behavior, functional approach, intellectual disability, problem behaviors
CHALLENGING BEHAVIOR: AN INTRODUCTION
Intellectual disability (ID) is a neurodevelopmental disorder that is characterized by significantly impaired intellectual and adaptive functioning. It is defined in terms of an Intelligence Quotient (IQ) under 70 as well as deficits in adaptive behaviors that affect daily functioning.1 Autism spectrum disorder (ASD), on the other hand, refers to a cluster of neurodevelopmental disorders that includes autism, Asperger syndrome, and other related conditions. ASD is characterized by problems in social communication and social interaction, as well as restricted and repetitive patterns of behavior, interests, or activities.1
The prevalence of problem behaviors such as self-injurious behavior, stereotyped behavior, and aggressive/destructive behaviors is high in people with ID and ASD. It is recognized as a significant impediment to social adaptation in such individuals. In recent years, the term “Challenging Behavior” (CB) has been commonly used in research studies that examine problem behaviors associated with developmental disabilities such as ID and ASD. However, CB is not a diagnosis; instead, it refers to behaviors that pose as a challenge to service providers, family members, or caregivers. Varied definitions of CB differentially include behaviors that physically harm either the person exhibiting them or others, destroy their living or working environment, occur frequently, and cannot be rectified by others.2, 3 Such behaviors often result from an interaction between personal and environmental factors. In turn, CB in persons with ID and ASD acts as a major barrier against social adaptation and as a major issue in welfare and medical care, which results in further problems such as abuse and long-term hospitalization. Therefore, the purpose of this article is to consolidate existing research findings on CB as well as information about support systems that are available for individuals with CB in Japan, in order to delineate new directions for future work in this field.
DEFINITIONS AND PREVALENCE
Every policy related to CB treatment and support is founded on sound definitions and epidemiological data. In this regard, it is important to note that the concept of CB has developed, not as a medical or biological definition, but as a social one. Coinage of the term CB was influenced by the information disseminated by the International Classification of Functioning, Disability and Health (ICF); it entered scientific parlance in the UK in lieu of the term “problem behavior” in the 1980s. This led to a change in perception that it is not only personal factors, but also social and environmental factors, that cause the problem behaviors exhibited by individuals with ID.
The prevalence of CB has implications for the education of various professionals and paraprofessionals, as well as for the training of staff and parents. Similarly, the age of people with CB and whether they live with their families of origin has implications for the planning of necessary services. All in all, investigating the prevalence of CB and the factors associated with it, have potential practical consequences.4
Prevalence rates of CB in individuals with ID range from 5 to 15% across educational, health, and social-care services5; however, significant variations in prevalence rates were evidenced in this epidemiological study. These variations may be attributable to differences in the age of the participants, sampling procedure, data collection method, type of behavioral scales used, and adopted definitions of problem behavior, across the many studies that it entailed. Indeed, population-based studies use different assessments to measure CB: Holden and Gitlesen6 used the Challenging Behavioral Survey (CBS)7; Myrbakk and Von Tetzchner8 used the Abnormal Behavior Checklist (ABC)9; Lundqvist10 used the Behavior Problem Inventory (BPI)11; and Bowring et al.12 used the Behavior Problem Inventory-Short Form (BPI-S).13, 14 Such assessments and scales measuring problem behaviors and CB have limited utility in the Japanese context because they have been standardized for use in foreign countries; further, population-based investigations of the validity and utility of such assessments are rarely conducted in Japan.
DEFINITIONS OF CB AND ITS PREVALENCE IN JAPAN
In Japan, the term “severe behavioral disorder” represents behavior patterns that are quite similar to those that are otherwise referred to as CB. The term emerged in a context where some residents of facilities for people with intellectual disabilities exhibited problem behaviors that were extremely difficult to treat. This group differs from those defined by psychiatric diagnoses because the definition of severe behavioral disorder is based on the presentation of behaviors that are directly harmful (e.g., biting, headbutting), indirectly harmful (e.g., sleep disorders, identity preservation), or harmful to the self. Further, such behaviors are not only exhibited at a significantly high frequency and in a disruptive manner, but are also difficult to treat within the child-rearing environment.15 It is also perceived as a concept that is primarily established in a context where there is a need to provide comprehensive treatment for the individual.
The Criteria for Determining Severe Problem Behavior (CDSPB) is a rating scale, consisting of 11 domains, that specifies the criteria using which severe problem behaviors should be determined (Table 1). The use of the CDSPB started in 1993 in a national undertaking led by the Japanese Ministry of Health and Labor. Each domain is scored in three stages, depending on the presence or absence of behavior as well as its frequency (1 point, 3 points, 5 points). A score higher than 10 points, out a maximum of 55 points, is indicative of severe problem behaviors, whereas those with scores higher than 20 points could be eligible to enroll in the Special Needs Project, which provides intensive interventions and welfare services.
Table 1. Domains measured by the Criteria for Determining Severe Problem Behavior (CDSPB) and their operational definitions.
| No | Domains | Operational definition | 1 Point | 3 Points | 5 Points |
| 1 | Severe self-injury | Self-injury to such an extent that a) the flesh can be seen or b) the head becomes deformed | 1–2 times weekly | 1–2 times daily | Throughout the day |
| 2 | Severe aggression | Aggression that causes injury to others, such as by means of biting, kicking, punching, pulling hair, or head thrusting |
1–2 times monthly | 1–2 times weekly | Several times a day |
| 3 | Severe stereotyped/restricted behaviors | Stereotyped/restricted behaviors that cannot be stopped even when others intervene; examples include a) removing one’s clothes, despite strong instructions to the contrary, b) refusing to go out, and c) returning to places that might be hundreds of meters away in order to pick up something |
1–2 times weekly | 1–2 times daily | Several times a day |
| 4 | Severe propertydestruction | Destruction of property in such a manner that it is hazardous to him/her and the surroundings; examples include a) breaking glass, furniture, doors, cups, or glasses, and b) tearing one’s clothes |
1–2 times monthly | 1–2 times weekly | Several times a day |
| 5 | Severe sleepdisturbances | Disrupted sleep cycles and an inability to stay in bed, which results in aggression towards others or destruction of property |
1–2 times monthly | 1–2 times weekly | Nearly every day |
| 6 | Severe feedingproblem | a) overeating, b) repeated regurgitation of food, c) eating nonnutritive, nonfood substances (e.g., feces, spike nails, stones), or d) avoidant/restrictive food intake |
1–2 times weekly | Nearly every day | Nearly every day |
| 7 | Severe problems in elimination | a) Kneading, throwing, and smearing feces, and b) repeated compulsive voiding of urine or feces |
1–2 times monthly | 1–2 times weekly | Nearly every day |
| 8 | Extremehyperactivity | a) Jumping around in a manner that poses danger to the body and/or life, b) running around when not under direct supervision, or c) climbing onto dangerous and high structures such as balcony handrails |
1–2 times monthly | 1–2 times weekly | Nearly every day |
| 9 | Unbearable screaming and crying | a) Unbearable screaming, and b) crying/wailing that lasts for hours |
Nearly every day | Througout the day | Constantly |
| 10 | Sustained intensepanic | Sustained bouts of intense panic that cannot be calmed by others | (Mark if applicable) | ||
| 11 | Explosive tantrums | Exhibiting explosive behaviors when others warn him/her, even when it pertains to trivial issues that occur in daily life | (Mark if applicable) |
A research study conducted in 1989 on children with behavioral disorders reported that people with severe behavioral disorders constituted 9.4% of the residents of the following four types of facilities that were surveyed: inpatient facilities for children with intellectual disabilities, inpatient correctional facilities for people with intellectual disabilities, facilities for individuals with autism, and facilities for individuals with severe disabilities. Similarly, the proportion of inpatients at facilities for people with intellectual disabilities who scored 10 points or more on the CDSPB, was found to be 12.1% in a study conducted by Mishima et al.,16 and 13.8% in a study conducted by Inoue et al.17
As mentioned earlier, the use of the term “severe behavior disorder” in Japan was created as part of changes in public policy; scores on the CDSPB were used as the eligibility criteria for obtaining welfare service certification. However, the criteria defining severe behavioral disorders have changed with developments in support systems. In recent years, CDSPB has been transformed into a new measure called the “Behavior Problem - Related Items.” The reliability and validity of these measures have to be tested because their items and cut-off scores have been adjusted based on changes in the welfare system. Therefore, it is necessary to develop a Japanese version of such scales that are predominantly used in the assessment of CB, in order to advance epidemiological and cross-cultural research entailing Japanese samples.
The scales that have been predominantly used in population-based studies on CB are the ABC and the BPI. The ABC is a standardized behavior rating scale that was developed for assessing problem behaviors in people with developmental disabilities as well as to evaluate the effectiveness of medications designed for such individuals. This assessment consists of 58 items that are classifiable into the following five subscales: (I) Irritability, Agitation, and Crying (15 items); (II) Lethargy and Social Withdrawal (16 items); (III) Stereotypic Behavior (7 items); (IV) Hyperactivity/Noncompliance (16 items); and (V) Inappropriate Speech (4 items). The BPI, on the other hand, is a 29-item checklist that assesses self-injurious, stereotyped, and aggressive/destructive behavior in persons with ID. The BPI was originally developed to aid in the screening and classification of self-injurious and stereotyped behavior in epidemiological studies; it was later expanded to include acts of aggression against others.18 Two variations of this assessment, namely, the BPI and the BPI-01, as well as a short version, namely, the BPI-S, have been developed and are currently being used for research purposes in Europe, the United States, Asia, etc.
The BPI-01 is a 52-item respondent-based behavior rating instrument that assesses self-injurious, stereotyped, and aggressive/destructive behaviors in individuals with ID and other developmental disabilities. Items are rated on a frequency scale and a severity scale.11 The BPI-S is a scale derived from BPI-01 that was developed with the objective of simplifying item content and language. Out of a total of 30 items, 15 items are identical to those found in the BPI-01, whereas the other 15 either contain excerpts from the BPI-01 items or are an integration of two or more items. Similar to the BPI-01, the BPI-S consists of three subscales, thereby rendering it a clinically useful and convenient assessment in the evaluation of the frequency and severity of problem behaviors.
We adapted the BPI-01 and the BPI-S to the Japanese context; subsequently, they examined the reliability and validity of the BPI-S for those with CB and ID.19 A total of 82 individuals with ID who were enrolled in welfare offices, and 232 individuals with ID who were either hospitalized or students of special schools, comprised the sample that participated in the study that examined the reliability and validity of the BPI-S, respectively. In order to evaluate test-retest reliability, intraclass correlation coefficients (ICC) were calculated for each subscale, as well as the total frequency and severity scores; the ICC exceeded 0.9. ICC, which were also computed to examine the interrater reliability of the scale, was found to range between 0.518 and 0.821. In order to examine the validity of the BPI-S, we compared the total frequency score of the composite BPI-S score, across the different severity groups of ID; a significant difference emerged between the most severe and mild to moderate groups.
In order to examine criterion validity, total scores on the Japanese version of the BPI-S were correlated against total scores on the CDSPB and the Abnormal Behavior Checklist-Japanese version (ABC-J),20 using Spearman’s correlation; total score on the Japanese version of the BPI-S evidenced a significant correlation of moderate strength with total scores on the CDSPB (r = .499) and the ABC-J (r = .699). These findings show that the BPI-S Japanese version is a useful and simple quantitative measure that can aid in the evaluation of CB in those with ID and ASD, with adequate reliability and validity. Additionally, it is expected that these measures will be utilized in epidemiological studies and cross-cultural research necessitating data from Japan.
RISKS ASSOCIATED WITH CHALLENGING BEHAVIORS AND LONG-TERM PROGNOSIS
Recent researchers have examined not only the prevalence of CB but also related risks and its long-term prognosis. Lundqvist10 investigated the prevalence of problem behaviors among people with ID and identified possible risk markers. Sixty-two percent of the ID population (n = 915) were found to have some problem behaviors (e.g., self-injurious, stereotyped, or aggressive/destructive behavior), and 18.7% of the ID population were found to have problem behaviors that could be identified as CB at the level that is restricted to social participation. As risk markers of CB were pointed out the severity of ID, autism, night sleep disturbances, sensory hypersensitivity, communication dysfunction, social deficits, psychiatric involvement, ingestion of psychotropic medication,10repetitive and restricted behaviors and interests, and overactivity/impulsivity.21
CB have been shown to persist of individuals across various age groups.22,23,24,25,26,27,28,29,30,31,32,33 The prevalence of more demanding CB increasing in people between 10 and 20 years, is highest in people between 20 and 40 years, and then decreasing.6 However, the changes in the prevalence of CB with age has different results depending on the type of CB, the results are not always consistent. Davies and Oliver33 analyzed statistically published data regarding the age-related prevalence of aggression and self-injury in persons with intellectual disability. The results indicated that the prevalence of self-injury rises significantly with age into late teens\early twenties before decreasing. Also, the prevalence of aggression was shown a similar pattern but this was less clear. Considering that the persistence of CB has been reported even in children younger than 4 years,34 it is important to examine the developmental trajectory of CB from early childhood.35
In order to examine the developmental trajectories of CB, it might be worthwhile to consider the various stages of schooling as life stages, even though educational systems differ across countries. Individuals with ID and/or ASD have difficulties during periods of transition between life stages. Indeed, several studies have underscored the difficulties associated with the transitions that occur during the primary school years,36, 37 the secondary school years,38 and the post-school years.39 However, there has been no examination of the transitions that occur during the different stages of school life, in individuals who exhibit CB. Indeed, CB can serve as an obstacle that prevents one from accessing community-based services and lead to social exclusion by means of institutionalization.40 Therefore, education/welfare services have to be committed to the prevention of CB and the implementation of necessary interventions that can address young children’s CB.41 Since most of the studies in this area are conducted in the US and UK, it is necessary to examine developmental trajectories that correspond to the Japanese education/welfare system.
Inoue and Gomi42 investigated the developmental trajectory of severe and long-term CB by analyzing changing presentations of CB in 47 people with ID. For this purpose, parents of these individuals were required to retrospectively respond to the CDSPB, for each life stage, ranging from early childhood to adulthood. Results showed that the highest total score on the CDSPB was recorded for the period of adolescence, when each subject had attended either junior high school or high school for special needs. Additionally, as a result of analysis conducted for each type of behavior disorder, the time at which CB first appeared and the seriousness of life transition were found to differ across participants. In particular, issues with regard to food, excretion, sleep pattern, hyperactivity and obsessive behaviors tended to increase up to the age of 3 years. Therefore, the appearance of these types of behaviors in early childhood could predict more severe CB in later years. Preventive approach for such children with a high risk of developing severe challenging behavior, and intensive care for severe challenging behavior in early adolescence, rendered by a multi-disciplinary team, is therefore very important.
FUNCTIONAL APPROACHES TO ADDRESSING CHALLENGING BEHAVIOR
CB in individuals with ID is now regarded as the result of a complex interaction between biological, developmental, and environmental factors.43 NICE guidelines on CB5 provide many approaches that are likely to reduce the risk of CB. Also, NICE recommended that medication not be used as a first-line intervention for CB.
In recent years, many psychosocial approaches have been studied with the objective of addressing CB in individuals with ASD and ID. Functional approaches to addressing CB are recognized as an evidence-based intervention strategy in many reviews of literature on the respective subject.44,45,46,47,48 The objective of analysis of function of behavior is to identify the reason why a person behaves the way that he or she does, by identifying the “Antecedent” that elicits the “Behavior” and the “Consequence” that serves as a reinforcer in maintaining it.
Antecedent influences on behavior constitute a great range of social and physical stimuli, ranging from ecological conditions (e.g., temperature, density), anxiety-producing events (e.g., a fight), physiological conditions (e.g., illness, pain, hunger, exhaustion), types and styles of requests and instructions. The effects of antecedent events are idiosyncratic; therefore, it is important for functional assessments to be precise in identifying the specific antecedent influences that elicit CB in a given child.49
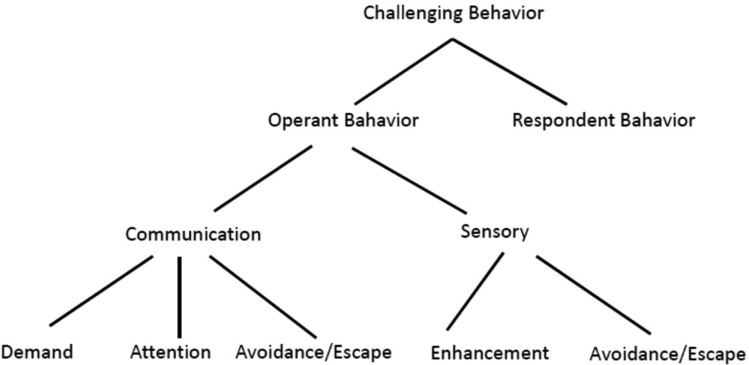
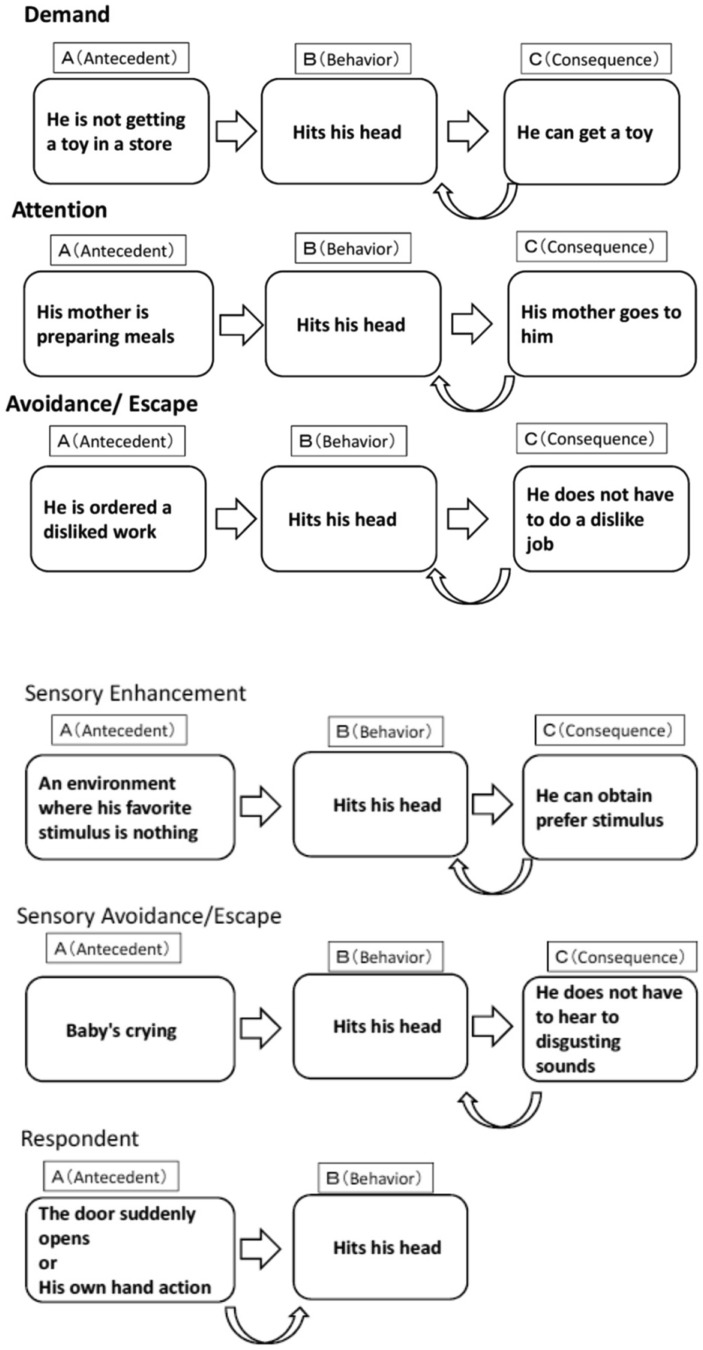
When the functional approach is applied as an intervention, CB can be reduced by changing the antecedent event that triggers CB. Moreover, it is also an approach to teach appropriate alternative behaviors (e.g., communication, leisure activities, task engagement behavior, etc.), without reinforcing problem behaviors. Functional assessment makes it possible to dispense with interpretations and theorizing of observed behavior, which may, in many cases, be inaccurate (e.g., the self-injurious behavior of striking his head is caused by stress). Inoue50 classified the functions of CB into the two following types (Fig. 1): operant behavior which is spontaneously elicited by the consequence of a behavior, and respondent behavior that is elicited by an antecedent. In addition, operant behaviors can divided into three, based on the communication-related functions that they serve: (1) demand function (i.e., I want you to do it), (2) attention function (i.e., I want your attention), (3) avoidance/ escape function (i.e., I do not want to do it). They can also be classified into the following two functions, based on the sensory functions that they serve: (1) sensory enhancement function (i.e., immersion in a favorite sensation) and (2) sensory avoidance/escape function (i.e., masking a bad feeling). Figure 2 illustrates an application of the aforementioned classification by using an example of the six functions of the self-injurious behavior of hitting one’s head.
Fig. 1.
Functional classification of challenging behavior.
Fig. 2.
Illustration of functional classification of challenging behavior using the example of hitting one’s own head.
Several techniques or program based on the functional approach emphasize the use of reinforcement to increase the occurrence of more adaptive or appropriate behaviors, and, at the same time removing applying punishment in CB. Differential reinforcement technique is a reinforcement technique designed to reduce the occurrence of CB while increasing the use of more adaptive, communicative, or appropriate behaviors. There are the following four differential reinforcement techniques to treat CB: differential reinforcement of incompatible behavior (DRI), differential reinforcement of alternative behavior (DRA), differential reinforcement of other behavior (DRO), and differential reinforcement of low rates of responding (DRL).
DRI delivers reinforcement upon the occurrence of behavior that is physically incompatible with or cannot be exhibited at the same time as the inappropriate behavior. For example, if the hand fapping behavior having sensory enhancement function, then teach manipulate toys using their hand. DRA is similar to DRI, except that alternative behaviors are not necessarily incompatible behaviors. It is important that the reinforcement of alternative behavior used in DRA is more powerful than the reinforcement of CB. DRO delivers reinforcement for any appropriate behavior whenever a targeted CB does not occur during a specific period of time. Therefore, there is a wide range of alternative appropriate behaviors. Any appropriate behavior exhibited at the end of that interval is reinforced, as long as the targeted CB did not occur. The time to be reinforced is gradually extended to reduce CB. DRL establishes a criterion limit an acceptable rate or duration for CB. For example, if the student engages loud three times during a 20-minute interval in which the criterion is set at no more than 5 times, then he receives reinforcement. These criteria will be gradually changed.
Functional communication training (FCT)51 based on the differential reinforcement technique is the most widely used and many previous studies have demonstrated its effectiveness.52 The National Professional Development Center on Autism Spectrum Disorder noted that because FCT is an evidence-based practice (EBPs), there should be a focus on promoting its use by practitioners.53 Firstly, FCT identifies the function that maintains CB. After the function of a CB has been identified, subjects are taught to use alternative communication strategies that serve the same function as the CB. By replacing CB with appropriate social communication, can improve the quality of daily communications.
EXPANSION BEYOND SPECIAL EDUCATION
The desirable outcomes of functional approach that were demonstrated by several early studies54,55,56 contributed to the inclusion of functional assessment in the Individuals with Disabilities Education Act that was passed in the United States in 1997. In 1998, the Division for Early Childhood (DEC) of the Council for Exceptional Children (CEC) clearly underscored the importance of using functional approach. Many subsequent studies have shown that functional approach in the resolution of CB in young children with autism is an effective strategy that can be implemented by school staff, family members, and community service providers.57, 58
Functional approaches, incorporated by schools in many districts and school systems in North America, Canada, and European countries, are referred to as Positive Behavioral Interventions and Supports (PBIS).59 In the United States, positive, action, intervention, and support were introduced, in accordance with the amendments made to the Individuals with Disabilities Education Act (IDEA) in 1997; this act served as a major factor in expanding interventions and support systems available to those with ID, beyond what special education could offer.
The School-Wide Positive Behavioral Interventions and Supports (SWPBIS) is a school system that supports evidence-based practice, by applying PBIS to support all school students, rather than only those exhibiting problem behaviors.59 In this manner, SWPBIS aims to prevent problem behavior, guide appropriate social behavior, impart appropriate actions, use multitiered systems of support to match students’ needs with action support, and apply data-based problem-solving techniques.60, 61
In contradistinction to the United States, functional assessment of CB and implementation of SWPBIS are not required by education-related laws in Japan. Nevertheless, Okubo, Fukunaga, and Inoue62 developed a consultation model for school support that utilizes a functional approach, by collaborating with university consultation agencies and elementary schools. In their research, they attempted to improve in-school support system by implementing the following: (1) implementation of workshops on understanding and providing support for individuals with developmental disorders and CB, and (2) maintenance of records of action taken by school staff and the sharing of support information. As a result of such efforts, the frequency of appropriate behaviors and task-engagement behavior of students was found to have increased; further, CB was also found to have decreased. In addition, it became possible to transfer the role of implementing individual support from university staff and parents to school staff. Despite such efforts, there are only a few local governments and schools in Japan that promote functional approaches to addressing CB; practical research in administrative district units and school units is therefore warranted.
STAFF TRAINING
It has been shown that the behavior of direct care staff is important for the success and maintenance of support plans aimed at addressing CB.63, 64 However, CB cause emotional reactions such as fear, anger, and irritation in the staff involved65, 66; this emotional reaction is associated with increased stress, which tends to result in burnout among staff.67, 68 In addition, it has been pointed out that staff’s shortage of knowledge affects their level of anxiety, job turnover rate, and burnout rate, and results in the improper management of behavior problems65, 69; there is also concern that it increases the likelihood of abuse.70, 71
Chung, Corbett, & Cumella,72 studied burnout among staff who work with individuals with severe behavioral disabilities. The results of the studies showed that exhaustion due to burnout was linked to a lack of specialized training and training institutes, number of years of experience, lack of cooperation among supporters, and a lack of training in the use of advanced technology.
The need to train support staff who serve clients with ID and CB is widely acknowledged. Studies examining the effectiveness of such interventions with staff workers have indeed contributed to the development of evidence-based programs that are aimed at imparting the necessary knowledge and intervention skills.73 Early training programs were conducted with the objective of training staff workers in functional assessment and effective behavior management techniques that would enable them to manage CB; many such functional and PBIS-related approaches, which were conducted using a single-case research design, were found to be effective in the management of CB. However, the findings of a recent meta-analytic research study pointed out that, although many staff training programs are effective in changing the behavior of staff workers, there is little evidence that they improve the behavior of individuals with CB.74 In recent years, research that emphasizes not only the acquisition of knowledge and skills, but also emotional control and changes in relationships with the target individual, has been increasing. For example, Mindfulness-Based Positive Behavior Support (MBPBS), which combines PBS with mindfulness training in order to help staff workers cope with stress, has been developed. Singh et al.75 evaluated the effects of an MBPBS course designed for caregivers. The results showed that the course was effective in reducing caregiver psychological stress, lower caregiver turnover, and a gradual reduction and elimination of the use of physical restraints in the management of aggressive behaviors in clients.
In Japan, a 12-hour training program for caregivers of individuals with severe behavioral disabilities (basic course), which combines lectures and exercises, was started nationwide in 2013; in 2014, a practical course was incorporated into the 12-hour program. Further, since 2015, the training program has been implemented in all the 47 prefectures in Japan. In 2016, the number of graduates who had completed this basic training program totaled 20,000, whereas the number of graduates who had undertaken the practical course exceeded 10,000; the training program has also been expanded to include a wider range of individuals than the original target group.76 However, there is no evidence to attest to the effectiveness of these staff training programs that have been conducted in Japan.
We developed a training program that could train Japanese staff in the implementation of functional approach for individuals with a severe behavioral disorder.77 The training program was administered to a total of 17 participants who had provided support to another person with behavioral disorders for more than 1 year. This staff training program consisted of 5 sessions; all participants were required to attend more than two-thirds of the program. Each participant was taking care of more than one individual with a severe behavioral disorder during the course of the program. From the first to forth session, the training consisted of lectures and exercises about functional assessment. In these exercises, each participant was required to prepare their own intervention plan. Further, between sessions, participants practiced the implementation of their intervention plan with their cases and recorded problem behaviors. In the fifth session, they were required to present a report about the respective individual that they had been working with. The Knowledge of Behavioral Principle as Applied to Children (KBPAC),78 the Aberrant Behavior Checklist-Japanese version (ABC-J), the Criterion for Determining Severe Problem Behavior (CDSPB), and the Pervasive Developmental Disorders Autism Society Japan Rating Scale-Short Form (PARS-SF),79 were administered to the staff, both before and after the program. Significant differences in the expected direction emerged on each of these measures. The results of this study suggest that it is important to not only improve staff knowledge about the functional approach and their mental health, but also simultaneously address the CB of their respective subjects. In future research on the effectiveness of staff training in addressing CB, it is necessary to not only reduce CB in the subject, but also improve staff knowledge, skills, emotional control, stress levels, and the quality of interaction with their subjects.
DEVELOPMENT OF ASSESSMENTS AND TREATMENTS FOR CHALLENGING BEHAVIOR THAT UTILIZE TECHNOLOGY
Conventionally, a questionnaire such as the ABC has been used as a therapeutic index in the treatment of behavior disorders through drug therapy. Questionnaires such as the ABC are useful for a general assessment of CB; however, it is not a suitable means to continuously track changes in the target CB, during the implementation of a behavioral intervention. Further, when it comes to the treatment of CB, behavior analysis experts observe and record the function, frequency, duration, and intensity of the CB. Behavioral observation can be undertaken using various strategies, ranging from observation of behavior as it occurs in reality to video-recorded data. In order to establish the reliability of data, the interrater reliability between two independent sets of recordings is typically evaluated.
In recent years, many interventions addressing CB have been mainstreamed in various environments such as schools, homes, and facilities; an obstacle faced by such interventions pertains to difficulties in accurately and objectively recording behaviors that occur in daily situations. It is not easy for laypersons such as family members, teachers, and facility staff, who are not trained experts in behavior analysis, to accurately record behaviors in daily situations; further, research on improving the reliability of such data has hardly been carried out. Mozingo, Smith, Riordan, Reiss, and Bailey80 showed that training staff workers and management resulted in an increase in the accuracy in recordings of the frequency of CB. However, introducing such training prior to interventions that equip staff to deal with CB is likely to be a burden them; therefore, it is necessary to develop the necessary technology that can adequately replace staff training.
Traditionally, behavioral observation required that behaviors be handwritten on recording paper; however, in recent years, such practices have been replaced by new technologies that utilize electronic devices and software. For example, Observer XT was developed to aid in the behavioral observation of autism and intellectual disability81; however, the primary purpose of the Observer XT is not for use in research studies.82 The Observer XT records behavior by analyzing video data using the behavior-specific code that has been encoded in the software. Unfortunately, however, such technology appears to be unsuitable for daily use by non-specialists. The Autism Tracker Pro, Behavior Tracker Pro, and other similar technologies are commercially available behavior-recording applications that can be used on smartphones and tablets. The Autism Tracker Pro is a family-oriented application that allows one to record the presence or absence of specific behaviors, mood level, meal intake, and other aspects of a child’s day-to-day activities in a calendar format, which can be also be visually presented as a graph. Behavior Tracker Pro, on the other hand, is an application for caregivers that can comprehensively record a specific behavior’s frequency, duration, interval periods, and preceding and subsequent events; the collected data can be visually presented as a graph. Although the Behavior Tracker Pro is an excellent multifunctional application, the steps that are involved in starting the application and entering one’s observations of the target behavior are complicated.
Development of a behavior-recording application: “Observations”
In order for non-experts to record behaviors that occur in daily situations, the input screen should be simple, easy to start, and allow recorders to input their observations quickly, either when the action occurs, during work, or at regular intervals. The scatter plot83 is a popular paper-based method of recording patterns of occurrences of daily behavior. More specifically, it entails a recording table in which the vertical axis represents the time of day and the horizontal axis represents the date; the observer can easily record behaviors by checking the squares that represent the time period during which the target behavior occurred.
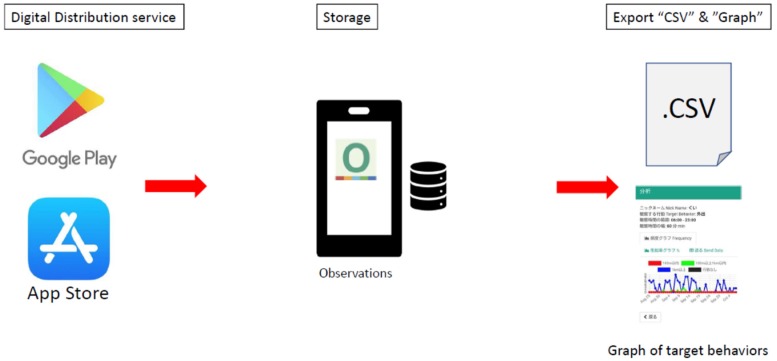
Inoue, Nakatani, Higashino84 developed “Observations,” which is as a smartphone application that non-experts can use to quickly record behaviors that occur in environments such as one’s home and school; the recordings can subsequently be presented as a graph and shared with experts as a scatter plot. This application is compatible with two versions of Android operating software (for Android devices) and iOS (for i-Phones and i-Pads); it can be downloaded from the respective distribution sites of each OS and can be used with many devices such as smartphones, tablets, and personal computers. Figure 3 provides an outline of the system by which the application maintains a record of challenging behaviors. This application was designed to complete one recording operation within a span of 10 seconds after the application launches. In other words, the application was designed in such a manner that the time between the start of the application and input of data is as close as possible to the time required to manually place a handwritten check sign on a recording paper.
Fig. 3.
Steps involved in recording challenging behavior using the software application, “Observations.”
The functions of the application involve the following processes: specifying relevant details such as target behavior and observation time, categorizing behaviors according to observations, and converting data into graphs to display the results of the analysis. The entered data are stored and accumulated in each device in the required “.csv” format; editing, processing, and analysis of the data can be performed on a personal computer. We analyzed two sets of data to investigate the characteristic features of the individuals whose target behaviors were recorded, as well as the issues that might have emerged when the application was operated by non-developer users. The first dataset pertained to cases in which adolescent children with ASD and their parents recorded adaptive behaviors at home; the other dataset pertained to recordings of challenging behaviors that were provided by multiple staff workers, employed at welfare offices. In the first case, where data was to be collected in the home environment, data was obtained in response to e-mails that were sent to participants (i.e., 4 children and 4 mothers), eight times every two months; throughout the period of data collection, recordings were entered in terms of units of time. Additionally, semi-structured interviews conducted with the children and their mothers enhanced our understanding of the end-user experience as well as the demands that are associated with the use of the application.
In the case of data that was to be obtained from welfare offices, 8 staff members recorded data on an application form whereas 39 others recorded data on paper; recordings marked on the application form were entered into the software application, following which paper-based recordings were also entered. A limitation of this application is that, because it has independent data management functions for each installed device, there is no function that allows data that have been entered from multiple devices to be aggregated and synchronized. For this reason, multiple staff members working in welfare facilities who attend to the same patient will be required to use the same device. Indeed, Marcu et al.85 have attributed the superiority of technology as a recording method to the ease of sharing, utilization, and dissemination of information. Staff members who choose to record their observations using the application benefit from the fact that it can automatically display the entered information as a graph; however, such possibilities may be hindered by difficulties associated with cooperative input of recordings among staff members. Another obstacle pertains to the fact that many Japanese welfare offices do not have rules about the management of records using mobile devices. In order to encourage the widespread utilization of this application in schools and facilities, it is necessary to propose rules that regulate appropriate information management in the workplace and mandate the upgrading of the application’s functions.
Development of an evaluation system that uses sensing technology to support individuals with severe behavioral disorders
In order to effectively treat CB, it is necessary to accurately count the occurrence of the target behavior. However, unlike the task of measuring certain components in a sample of blood tissue, it is difficult to accurately measure CB. In daily practice, recording CB is a subjective exercise that is typically undertaken by the caregiver; applications such as “Observations” have been developed with the objective of simplifying such tasks. However, even these methods render it impossible to accurately record behavior over a period of several days if the frequency with which CB are exhibited tends to be remarkably large. Therefore, it is necessary to develop technologies that can automatically measure CB.
Recent developments in sensing technology have resulted in the evolution of technologies that utilize various sensors. In accordance with these developments, we are currently developing a behavioral obstacle measurement system that uses sensing technology and are examining the practicality of using acceleration sensors and other similar sensors. By putting this research to practical use, objective indicators of behavioral improvements and the severity of CB can be derived from subjective data. The application of sensing technology in the measurement of behavioral disorders is epochal in the development of such assessment systems. Practical applications of this kind are expected to further promote research on the effects of drug therapy and behavioral interventions on CB. In addition to examining their therapeutic effects on an individual basis, such efforts are likely to contribute to a reduction in the dosage of drugs, elimination of long-term hospitalization, and hasten the return to social life, among individuals with behavior disorders. Psychosocial interventions that capitalize on the advantages of technology, such as systems that enable remote treatment of behavioral disorders, are expected to develop at a drastic rate in future years.
Acknowledgments
Acknowledgments: This research was supported by AMED under Grant Number JP18059499.
Footnotes
The author declares no conflict of interest.
REFERENCES
- 1.Association AP. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®): American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Emerson E,Bromley J. The form and function of challenging behaviours. J Intellect Disabil Res. 1995;39:388-98. 10.1111/j.1365-2788.1995.tb00543.x [DOI] [PubMed] [Google Scholar]
- 3.Qureshi H,Alborz A. Epidemiology of challenging behaviour. Ment Handicap Res. 1992;5:130-45. 10.1111/j.1468-3148.1992.tb00041.x [DOI] [Google Scholar]
- 4.Qureshi H. The size of the problem. Emerson E, McGill P, Mansell J, editors. Severe Learning Disabilities and Challenging Behaviours. London: Chapman and Hall; 1994. p.17-36.
- 5.NICE [Internet]. London: National Institute for Health and Care Excellence (NICE); c2019. [updated 2015; cited 2019 March 19]. Challenging behaviour and learning disabilities: prevention and interventions for people with learning disabilities whose behaviour challenges. Available from: https://www.nice.org.uk/guidance/ng11. [PubMed]
- 6.Holden B,Gitlesen J. A total population study of challenging behaviour in the county of Hedmark, Norway: Prevalence, and risk markers. Res Dev Disabil. 2006;27:456-65. 10.1016/j.ridd.2005.06.001 [DOI] [PubMed] [Google Scholar]
- 7.Alborz A,Emerson E,Kiernan C,Qureshi H Challenging behaviour survey: Individual Schedule. Manchester: Hester Adrian Research Centre; 1994. [Google Scholar]
- 8.Myrbakk E,von Tetzchner S. Psychiatric disorders and behavior problems in people with intellectual disability. Res Dev Disabil. 2008;29:316-32. 10.1016/j.ridd.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 9.Aman MG,Singh NN,Stewart AW,Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. Am J Ment Defic. 1985;89:485-91. [PubMed] [Google Scholar]
- 10.Lundqvist LO. Prevalence and risk markers of behavior problems among adults with intellectual disabilities: A total population study in Örebro County, Sweden. Res Dev Disabil. 2013;34:1346-56. 10.1016/j.ridd.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 11.Rojahn J,Matson JL,Lott D,Esbensen AJ,Smalls Y. The Behavior Problems Inventory: an instrument for the assessment of self-injury, stereotyped behavior, and aggression/destruction in individuals with developmental disabilities. J Autism Dev Disord. 2001;31:577-88. 10.1023/A:1013299028321 [DOI] [PubMed] [Google Scholar]
- 12.Bowring DL,Totsika V,Hastings RP,Toogood S,Griffith GM. Challenging behaviours in adults with an intellectual disability: A total population study and exploration of risk indices. Br J Clin Psychol. 2017;56:16-32. 10.1111/bjc.12118 [DOI] [PubMed] [Google Scholar]
- 13.Rojahn J,Rowe EW,Sharber AC,Hastings R,Matson JL,Didden R,et al. The Behavior Problems Inventory-Short Form for individuals with intellectual disabilities: Part I: development and provisional clinical reference data. J Intellect Disabil Res. 2012;56:527-45. 10.1111/j.1365-2788.2011.01507.x [DOI] [PubMed] [Google Scholar]
- 14.Rojahn J,Rowe EW,Sharber AC,Hastings R,Matson JL,Didden R,et al. The Behavior Problems Inventory-Short Form for individuals with intellectual disabilities: Part II: reliability and validity. J Intellect Disabil Res. 2012;56:546-65. 10.1111/j.1365-2788.2011.01506.x [DOI] [PubMed] [Google Scholar]
- 15.Behavior disabled children (person) research group. [Research on behavior improvement and treatment of children (persons) with severe behavior disorder]. Ministry of Health, Labor and Welfare, etc. database system.1989. Japanese.
- 16.Mishima T,Kawasaki Y,Iida M,Shinomiya M,Yokota K,Kanno A. A Clinical Study of Extremely Disruptive Behavior Disorders. Japanese J on Devel Disabil. 1999;21:202-13. Japanese. [Google Scholar]
- 17.Inoue M,Okada R,Ueda A,Adachi J,Tsujii M,Otsuka A,et al. Analysis of severe behavioral disorders in people from facilities for mental retardation. Seishin Igaku. 2011;53:639-45. Japanese with English Abstract. [Google Scholar]
- 18.Rojahn J,Polster LM,Mulick JA,Wisniewski JJ. Reliability of the behavior problems inventory. Journal of the Multihandicapped Person. 1989;2:283-93. 10.1007/BF01098170 [DOI] [Google Scholar]
- 19.Inada N,Inoue M,Gomi Y [Development of Japanese version of BPI-S (Behavior Problems Inventory‐Short Form) and examination of its reliability and validity]. 59th Annual Meeting of The Japanese Society for Child and Adolescent Psychiatry. 2018. Japanese.
- 20.Ono Y. Factor validity and reliability for the Aberrant behavior checklist-community in a Japanese population with mental retardation. Res Dev Disabil. 1996;17:303-9. 10.1016/0891-4222(96)00015-7 [DOI] [PubMed] [Google Scholar]
- 21.Davies LE,Oliver C. Self-injury, aggression and destruction in children with severe intellectual disability: Incidence, persistence and novel, predictive behavioural risk markers. Res Dev Disabil. 2016;49-50:291-301. 10.1016/j.ridd.2015.12.003 [DOI] [PubMed] [Google Scholar]
- 22.Cooper SA,Smiley E,Allan LM,Jackson A,Finlayson J,Mantry D,et al. Adults with intellectual disabilities: prevalence, incidence and remission of self-injurious behaviour, and related factors. J Intellect Disabil Res. 2009;53:200-16. 10.1111/j.1365-2788.2008.01060.x [DOI] [PubMed] [Google Scholar]
- 23.Cooper SA,Smiley E,Jackson A,Finlayson J,Allan L,Mantry D,et al. Adults with intellectual disabilities: prevalence, incidence and remission of aggressive behaviour and related factors. J Intellect Disabil Res. 2009;53:217-32. 10.1111/j.1365-2788.2008.01127.x [DOI] [PubMed] [Google Scholar]
- 24.Chadwick O,Kusel Y,Cuddy M,Taylor E. Psychiatric diagnoses and behaviour problems from childhood to early adolescence in young people with severe intellectual disabilities. Psychol Med. 2005;35:751-60. 10.1017/S0033291704003733 [DOI] [PubMed] [Google Scholar]
- 25.Kieman C,Alborz A. Persistence and change in challenging and problem behaviours of young adults with intellectual disability living in the family home. J Appl Res Intellect Disabil. 1996;9:181-93. 10.1111/j.1468-3148.1996.tb00108.x [DOI] [Google Scholar]
- 26.Emerson E,Kiernan C,Alborz A,Reeves D,Mason H,Swarbrick R,et al. Predicting the persistence of severe self-injurious behavior. Res Dev Disabil. 2001;22:67-75. 10.1016/S0891-4222(00)00062-7 [DOI] [PubMed] [Google Scholar]
- 27.Totsika V,Toogood S,Hastings RP,Lewis S. Persistence of challenging behaviours in adults with intellectual disability over a period of 11 years. J Intellect Disabil Res. 2008;52:446-57. 10.1111/j.1365-2788.2008.01046.x [DOI] [PubMed] [Google Scholar]
- 28.Taylor L,Oliver C,Murphy G. The chronicity of self‐injurious behaviour: a long‐term follow‐up of a total population study. J Appl Res Intellect Disabil. 2011;24:105-17. 10.1111/j.1468-3148.2010.00579.x [DOI] [Google Scholar]
- 29.Borthwick-Duffy SA. Epidemiology and prevalence of psychopathology in people with mental retardation. J Consult Clin Psychol. 1994;62:17-27. 10.1037/0022-006X.62.1.17 [DOI] [PubMed] [Google Scholar]
- 30.Murphy GH,Beadle-Brown J,Wing L,Gould J,Shah A,Holmes N. Chronicity of challenging behaviours in people with severe intellectual disabilities and/or autism: a total population sample. J Autism Dev Disord. 2005;35:405-18. 10.1007/s10803-005-5030-2 [DOI] [PubMed] [Google Scholar]
- 31.Kiernan C,Kiernan D. Challenging behaviour in schools for pupils with severe learning difficulties. Ment Handicap Res. 1994;7:177-201. 10.1111/j.1468-3148.1994.tb00126.x [DOI] [Google Scholar]
- 32.Crocker AG,Mercier C,Lachapelle Y,Brunet A,Morin D,Roy ME. Prevalence and types of aggressive behaviour among adults with intellectual disabilities. J Intellect Disabil Res. 2006;50:652-61. 10.1111/j.1365-2788.2006.00815.x [DOI] [PubMed] [Google Scholar]
- 33.Davies L,Oliver C. The age related prevalence of aggression and self-injury in persons with an intellectual disability: A review. Res Dev Disabil. 2013;34:764-75. 10.1016/j.ridd.2012.10.004 [DOI] [PubMed] [Google Scholar]
- 34.Green V,Oreilly M,Itchon J,Sigafoos J. Persistence of early emerging aberrant behavior in children with developmental disabilities. Res Dev Disabil. 2005;26:47-55. 10.1016/j.ridd.2004.07.003 [DOI] [PubMed] [Google Scholar]
- 35.Berkson G. Early development of stereotyped and self-injurious behaviors: II. Age trends. Am J Ment Retard. 2002;107:468-77. [DOI] [PubMed] [Google Scholar]
- 36.McIntyre LL,Eckert TL,Fiese BH,DiGennaro Reed FD,Wildenger LK. Family concerns surrounding kindergarten transition: A comparison of students in special and general education. Early Child Educ J. 2010;38:259-63. 10.1007/s10643-010-0416-y [DOI] [Google Scholar]
- 37.Stormont M,Beckner R,Mitchell B,Richter M. Supporting successful transition to kindergarten: general challenges and specific implications for students with problem behavior. Psychol Sch. 2005;42:765-78. 10.1002/pits.20111 [DOI] [Google Scholar]
- 38.Makin C,Hill V,Pellicano E. The primary-to-secondary school transition for children on the autism spectrum: A multi-informant mixed-methods study. Autism & Developmental Language Impairments. 2017;2:1-18 10.1177/2396941516684834 [DOI] [Google Scholar]
- 39.Davies MD,Beamish W. Transitions from school for young adults with intellectual disability: parental perspectives on “life as an adjustment”. J Intellect Dev Disabil. 2009;34:248-57. 10.1080/13668250903103676 [DOI] [PubMed] [Google Scholar]
- 40.Oliver C,Murphy GH,Corbett JA. Self-injurious behaviour in people with mental handicap: a total population study. J Ment Defic Res. 1987;31:147-62. [DOI] [PubMed] [Google Scholar]
- 41.Dunlap G,Strain PS,Fox L,Carta JJ,Conroy M,Smith BJ,et al. Prevention and intervention with young children’s challenging behavior: perspectives regarding current knowledge. Behav Disord. 2006;32:29-45. 10.1177/019874290603200103 [DOI] [Google Scholar]
- 42.Inoue M,Gomi Y The developmental process of severe behavior disorder in the long term. 9th Annual Autism Conference. 2015.
- 43.Langthorne P,McGill P,O’Reilly M. Incorporating “motivation” into the functional analysis of challenging behavior: on the interactive and integrative potential of the motivating operation. Behav Modif. 2007;31:466-87. 10.1177/0145445506298424 [DOI] [PubMed] [Google Scholar]
- 44.Doehring P,Reichow B,Palka T,Phillips C,Hagopian L. Behavioral approaches to managing severe problem behaviors in children with autism spectrum and related developmental disorders: a descriptive analysis. Child Adolesc Psychiatr Clin N Am. 2014;23:25-40. 10.1016/j.chc.2013.08.001 [DOI] [PubMed] [Google Scholar]
- 45.Heyvaert M,Saenen L,Campbell JM,Maes B,Onghena P. Efficacy of behavioral interventions for reducing problem behavior in persons with autism: an updated quantitative synthesis of single-subject research. Res Dev Disabil. 2014;35:2463-76. 10.1016/j.ridd.2014.06.017 [DOI] [PubMed] [Google Scholar]
- 46.Horner RH,Carr EG,Strain PS,Todd AW,Reed HK. Problem behavior interventions for young children with autism: a research synthesis. J Autism Dev Disord. 2002;32:423-46. 10.1023/A:1020593922901 [DOI] [PubMed] [Google Scholar]
- 47.Machalicek W,O’Reilly MF,Beretvas N,Sigafoos J,Lancioni GE. A review of interventions to reduce challenging behavior in school settings for students with autism spectrum disorders. Res Autism Spectr Disord. 2007;1:229-46. 10.1016/j.rasd.2006.10.005 [DOI] [Google Scholar]
- 48.Montgomery J,Martin T,Shooshtari S,Stoesz BM,Heinrichs DJ,North S,et al. Interventions for challenging behaviours of students with autism spectrum disorders and developmental disabilities: A synthesis paper. Exceptionality Education International. 2014;23:2-21. [Google Scholar]
- 49.Dunlap G,Fox L. Function-based interventions for children with challenging behavior. J Early Interv. 2011;33:333-43. 10.1177/1053815111429971 [DOI] [Google Scholar]
- 50.Inoue M. [The practice of functional approach for behavioral problems of children with developmental disorders]. Psychiatria et neurologia paediatrica Japonica. 2017;58:15-22. Japanese. [Google Scholar]
- 51.Carr EG,Durand VM. Reducing behavior problems through functional communication training. J Appl Behav Anal. 1985;18:111-26. 10.1901/jaba.1985.18-111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Andzik NR,Cannella-Malone HI,Sigafoos J. Practitioner-implemented functional communication training: A review of the literature. Res Pract Persons Severe Disabl. 2016;41:79-89. 10.1177/1540796916633874 [DOI] [Google Scholar]
- 53.Franzone E. Overview of functional communication training (FCT) [Internet]. Madison: National Professional Development Center on Autism Spectrum Disorders, Waisman Center, University of Wisconsin; 2009. [cited 2019 May 30]. Available from: http://autismpdc.fpg.unc.edu/sites/autismpdc.fpg.unc.edu/files/imce/documents/Functional-Communication-Training-Complete10-2010.pdf. [Google Scholar]
- 54.Arndorfer RE,Miltenberger RG,Woster SH,Rortvedt AK,Gaffaney T. Home-based descriptive and experimental analysis of problem behaviors in children. Top Early Child Spec Educ. 1994;14:64-87. 10.1177/027112149401400108 [DOI] [Google Scholar]
- 55.Kamps DM,Ellis C,Mancina C,Wyble J,Greene L,Harvey D. Case studies using functional analysis for young children with behavior risks. Educ Treat Child. 1995;243-60. [Google Scholar]
- 56.Umbreit J. Functional assessment and intervention in a regular classroom setting for the disruptive behavior of a student with attention deficit hyperactivity disorder. Behav Disord. 1995;20:267-78. 10.1177/019874299502000407 [DOI] [Google Scholar]
- 57.Dunlap G,Fox L. A demonstration of behavioral support for young children with autism. J Posit Behav Interv. 1999;1:77-87. 10.1177/109830079900100202 [DOI] [Google Scholar]
- 58.Fox L,Benito N,Dunlap G Early intervention with families of young children with autism and behavior problems. Families and positive behaviour support: Addressing problem behaviour in family contexts Baltimore, MD: Paul H Brooks Publishing Co; 2002. [Google Scholar]
- 59.Sugai G,Horner RR. A promising approach for expanding and sustaining school-wide positive behavior support. School Psych Rev. 2006;35:245-60. [Google Scholar]
- 60.Crone DA,Horner RH Building positive behavior support systems in schools: Functional behavioral assessment. NY: Guilford Press; 2003. [Google Scholar]
- 61.George HP,Kincaid D,Pollard-Sage J Primary-tier interventions and supports. Handbook of positive behavior support. Berlin: Springer; 2009. p. 375-94. [Google Scholar]
- 62.Okubo K,Fukunaga A,Inoue M. [Behavioral support for aggressive/destructive behaviors of children with developmental disabilities in regular classes: Developing individual support and in-school support system]. Japanese J Speci educ. 2007; 45:35-48. Japanese. [Google Scholar]
- 63.Hastings RP. Staff in special education settings and behaviour problems: Towards a framework for research and practice. Educ Psychol.2005;25:207-21. . 10.1080/0144341042000301166 [DOI] [Google Scholar]
- 64.Hastings RP,Remington B. Rules of engagement: toward an analysis of staff responses to challenging behavior. Res Dev Disabil. 1994;15:279-98. 10.1016/0891-4222(94)90008-6 [DOI] [PubMed] [Google Scholar]
- 65.Bromley J,Emerson E. Beliefs and emotional reactions of care staff working with people with challenging behaviour. J Intellect Disabil Res. 1995;39:341-52. 10.1111/j.1365-2788.1995.tb00526.x [DOI] [PubMed] [Google Scholar]
- 66.Hatton C,Brown R,Caine A,Emerson E. Stressors, coping strategies and stress‐related outcomes among direct care staff in staffed houses for people with learning disabilities. Ment Handicap Res. 1995;8:252-71. 10.1111/j.1468-3148.1995.tb00161.x [DOI] [Google Scholar]
- 67.Jenkins R,Rose J,Lovell C. Psychological well-being of staff working with people who have challenging behaviour. J Intellect Disabil Res. 1997;41:502-11. 10.1111/j.1365-2788.1997.tb00743.x [DOI] [PubMed] [Google Scholar]
- 68.Rose D,Horne S,Rose JL,Hastings RP. Negative emotional reactions to challenging behaviour and staff burnout: two replication studies. J Appl Res Intellect Disabil. 2004;17:219-23. 10.1111/j.1468-3148.2004.00194.x [DOI] [Google Scholar]
- 69.Allen P,Pahl JM,Quine L Care staff in transition: The impact on staff of changing services for people with mental handicaps. Bernan Press (PA); 1990. [Google Scholar]
- 70.Emerson E,McGill P,Mansell J Severe learning disabilities and challenging behaviors: Designing high quality services. London: Chapman & Hall; 1994. [Google Scholar]
- 71.Romeo R,Knapp M,Tyrer P,Crawford M,Oliver-Africano P. The treatment of challenging behaviour in intellectual disabilities: cost-effectiveness analysis. J Intellect Disabil Res. 2009;53:633-43. 10.1111/j.1365-2788.2009.01180.x [DOI] [PubMed] [Google Scholar]
- 72.Chung MC,Corbett J,Cumella S. Relating staff burnout to clients with challenging behaviour in people with a learning difficulty: pilot study 2. Eur J Psychiatry. 1996;10:155-66. [Google Scholar]
- 73.van Oorsouw WMWJ,Embregts PJCM,Bosman AMT. Evaluating staff training: taking account of interactions between staff and clients with intellectual disability and challenging behaviour. J Intellect Dev Disabil. 2013;38:356-64. 10.3109/13668250.2013.826787 [DOI] [PubMed] [Google Scholar]
- 74.Knotter MH,Spruit A,De Swart JJW,Wissink IB,Moonen XMH,Stams GJM. Training direct care staff working with persons with intellectual disabilities and challenging behaviour: A meta-analytic review study. Aggress Violent Behav. 2018;40:60-72. 10.1016/j.avb.2018.03.005 [DOI] [Google Scholar]
- 75.Singh NN,Lancioni GE,Medvedev ON,Myers RE,Chan J,McPherson CL,et al. Comparative effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) and positive behavior support (PBS) in a randomized controlled trial. Mindfulness. 2018;1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shiga T,Gomi Y,Nobuhara K. [Research on the training for the supporter of severe behavioral disorders; Development of training programs and textbook for the practical course]. Nozomi-no-sono Kiyo. 2015;8:1-98 Japanese. [Google Scholar]
- 77.Kato M,Ida M,Ota M,Okamoto K,Fuji T,Inoue M The Effects of Staff Training Program for Individuals with Behavioral Disorders (1): Development of staff training program based on the functional analysis. 4th. Asian Cognitive Behavior Therapy (CBT) Conference. 2013.
- 78.O’Dell SL,Tarler-Benlolo L,Flynn JM. An instrument to measure knowledge of behavioral principles as applied to children. J Behav Ther Exp Psychiatry. 1979;10:29-34. 10.1016/0005-7916(79)90033-8 [DOI] [Google Scholar]
- 79.Ito H,Tani I,Yukihiro R,Adachi J,Hara K,Ogasawara M,et al. Validation of an interview-based rating scale developed in Japan for pervasive developmental disorders. Res Autism Spectr Disord. 2012;6:1265-72. 10.1016/j.rasd.2012.04.002 [DOI] [Google Scholar]
- 80.Mozingo DB,Smith T,Riordan MR,Reiss ML,Bailey JS. Enhancing frequency recording by developmental disabilities treatment staff. J Appl Behav Anal. 2006;39:253-6. 10.1901/jaba.2006.55-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Grieco F,Loijens L,Zimmerman P,Krips O,Spink A The Observer XT version 10.5. Wageningen: Noldus Information Technology; 2011.
- 82.Delgado C,Gonzalez-Gordon RG,Aragón E,Navarro JI. Different methods for long-term systematic assessment of challenging behaviors in people with severe intellectual disability. Front Psychol. 2017;8:17. 10.3389/fpsyg.2017.00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Touchette PE,MacDonald RF,Langer SN. A scatter plot for identifying stimulus control of problem behavior. J Appl Behav Anal. 1985;18:343-51. 10.1901/jaba.1985.18-343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Inoue M,Nakatani K,Higashino M. Development of behavior record application “Observations” for behavior problems. Jpn J Behav Anal.; in press. Japanese with English abstract. [Google Scholar]
- 85.Marcu G,Tassini K,Carlson Q,Goodwyn J,Rivkin G,Schaefer KJ,et al. Why do they still use paper?: understanding data collection and use in Autism education. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. ACM. 2013;3177-86. . 10.1145/2470654.2466436 [DOI] [Google Scholar]