Abstract
Objective
Cervical artificial disc replacement (CADR) is a new technology in cervical spine surgery. However, CADR may result in paravertebral ossification (PO) after surgery and affect the mobility of the related spinal segments. The present widely used assessment method based on X‐ray tomography cannot provide the position information of PO, and also PO detection rates by X‐ray are low. The incidence of PO varies dramatically between studies. This study built a novel classification system based on cervical computer tomography (CT) scan to re‐evaluate the incidence of PO and its influence on CADR, and also analyzed the predisposing factors of PO.
Methods
In this retrospective study, 71 patients (from January 2004 to December 2009) who received cervical artificial disc replacement in our hospital were enrolled, and 82 cervical segments were replaced by Bryan discs. The range of motion (ROM) of the related cervical segments and scores of neurological symptoms (neck disability index [NDI] and Japanese Orthopaedic Association [JOA] scores) for both pre‐surgery and last follow‐up were acquired, respectively. After the establishment of a novel grading system for PO based on CT scan, we analyzed the CT images acquired before surgery and at the last time follow‐up. Occurrence and distribution of PO at both time points were calculated. ROM between pre‐surgery and post‐surgery was compared by paired t‐test stratified by PO stages. One‐way ANOVA was used to compare NDI and JOA scores between high‐grade and low‐grade PO groups after surgery. The χ2‐test was used to evaluate the risk (odds ratio) of predisposing factors in developing high‐grade PO after surgery.
Results
The CT‐based classification system has good inter‐observer and intra‐observer reliability. The detection rate of PO by CT scan is higher than for traditional X‐ray examination. The incidence of low‐grade PO in all 82 segments at last follow‐up is 32.9%. The occurrences of high‐grade PO at preoperational and last follow‐up time are 15.9% and 67.1%, respectively. The high‐grade PO is mainly distributed around the uncovertebral joint. The pre‐surgery and post‐surgery ROM are similar in patients with low‐grade PO at last follow‐up time (9.80° ± 3.65° vs 10.03° ± 3.73°, P = 0.801); however, in patients with high‐grade PO the post‐surgery ROM decreases significantly compared to the pre‐surgery ROM (9.73° ± 4.03° vs 6.63° ± 4.21°, P < 0.001). There is no statistical difference for JOA and NDI scores after surgery between high‐grade and low‐grade PO patients at final follow‐up (P = 0.264, P = 0.703). The χ2‐test indicates that patients with preoperational existence of PO have a high risk of high‐grade PO after surgery (OR = 4, P = 0.012).
Conclusions
The novel CT image‐based PO classification system has good intra‐observer reliability. The incidence of PO after Bryan cervical disk replacement is relative high, and the high‐grade PO is mainly distributed at the uncovertebral joint. The high‐grade PO will affect the ROM after surgery; however, it does not affect the neurologic symptoms.
Keywords: Cervical artificial disc replacement, Classification, Paravertebral ossification, Range of motion
Introduction
The number of patients suffering from radiculopathy and/or myelopathy from cervical disc herniation and/or cervical spondylosis has increased dramatically. Anterior cervical discectomy and fusion (ACDF) has been a successful treatment for several decades, and it prevents post‐surgery kyphosis and neck pain. Although technical advances in ACDF have led to better recovery and fewer complications after surgery, concern remains that the fused segments will have little motion and there is potential for subsequent adjacent level disc degeneration. Hence, techniques to preserve the motions of the cervical spine after surgery are being developed. Cervical artificial disc replacement (CADR) is a relatively new technique in cervical spine surgery. The degenerated cervical discs are replaced by the cervical artificial discs during the CADR surgery without causing the adverse effects of the traditional ACDF surgery1. Compared with ACDF surgery, CADR will maintain the physiological range of motion and also preserve the disc height of the surgery segments. In addition to being less damaging to physiologically motion than fusion, CADR also has the advantage of diminishing the adjacent segments’ stress transfer, which will lower the incidence of adjacent segment degeneration disease2, 3, 4. Due to the kinematics advantages in CADR surgery, cervical artificial disc technology has been developing rapidly, there are now several such metal‐on‐metal or metal‐on‐plastic cervical prostheses. To date, several thousand operations have taken place worldwide.
However, with the extensive use of cervical artificial discs, some adverse outcomes of CADR have raised concern among clinicians. The major concerns relating to implanting a motion‐preserving prosthesis are the potential loss of motion and even autofusion in related segments. In several multicenter trials, paravertebral ossification (PO), which includes heterotopic ossification and osteophytes, was observed after cervical artificial disc implantations5, 6. In a study attempting to assess the role of PO in CADR reported by Yi et al., three different types of cervical artificial disk were examined retrospectively in 170 patients; the overall incidence of PO was 40.6%, and the occurrence rate was 21% in the Bryan cervical disc group, 52.5% in the Mobi‐C group, and 71.4% in the ProDisc‐C group7. In a 4‐year follow‐up prospective study, Suchomel et al. reported that significant PO was present in 45% of cervical disk implants and segmental ankylosis in another 18% just 4 years after CADR intervention8. Although the PO does not affect the neurological outcomes, it may develop to bony blocks and will decrease the postoperational range of motion (ROM) and can even lead to complete ankylosis of the affected segments, which will diminish all the advantages of CADR over ACDF and conflict with the motion preserving benefit of CADR1, 7, 8, 9, 10, 11.
The current most widely used classification system for PO is McAfee classification, which is based on X‐ray tomography12, and this classification divides PO into five categories. However, based on this classification system, the incidence of PO is unexpectedly high and varies from 0% to 94.1% in studies aiming to assess the occurrence rate of PO7, 8, 11, 13, 14, 15, which means that the incidence of PO has a certain heterogeneity in these studies5, 16. The McAfee classification itself may be the reason for the high heterogeneity in the PO occurrence rate. In McAfee classification for PO, computed tomography (CT) scans are not used, and the X‐ray based McAfee scale cannot satisfy all the conditions of PO4, 7, 17, 18, especially PO that are located beside the vertebra6. It is possible that the added details afforded by CT scans might show more subtle degrees of PO that will not recognized by a plain film, including the position information of PO4. For a more accurate study of PO, especially its occurrence rate, a more sensitive classification method based on CT scans was needed.
The purpose of this study was to introduce a novel classification system for PO based on CT scans in cervical artificial disc replacement. The true occurrence rate of PO after Bryan cervical artificial disc implantation was evaluated in a group of long‐term followed‐up patients, and, also, the clinical influence of PO for post‐CADR patients was studied. This study also investigated the predisposing factors of PO among general factors, focusing in particular on whether advanced pre‐existing PO have special influence in the long term on PO formation after CADR surgery.
Materials and Methods
Patient Population
Patient Data
Institutional board approval was obtained before the study, and informed consent was collected from all the patients who were enrolled. In this retrospective study, 110 patients were randomly selected from a large group of 292 patients who had undergone Bryan (Medtronic, Minneapolis, MN) CADR in our hospital between January 2004 and December 2009. All 292 patients had received CT and X‐rays of the cervical spine before surgery because of their symptoms and signs associated with radiculopathy and/or myelopathy from cervical disc herniation and/or cervical spondylosis19.
The surgical procedures for all the patients were performed by the same group of surgeons using the standard Bryan disc surgical technique. Patients with a history of previous cervical operation, instability of the operation segment, tumor, cervical fracture, ossification of the posterior ligament or anterior ligament, as well as abnormal calcium and phosphate metabolism and hip or knee joint replacement were excluded. From the remainder, we randomly selected 110 patients using a random number chart. Seventy‐one (65%) patients completed the follow‐up, and all the patients underwent CT and X‐ray scans again at the final follow‐up (Fig. 1).
Figure 1.
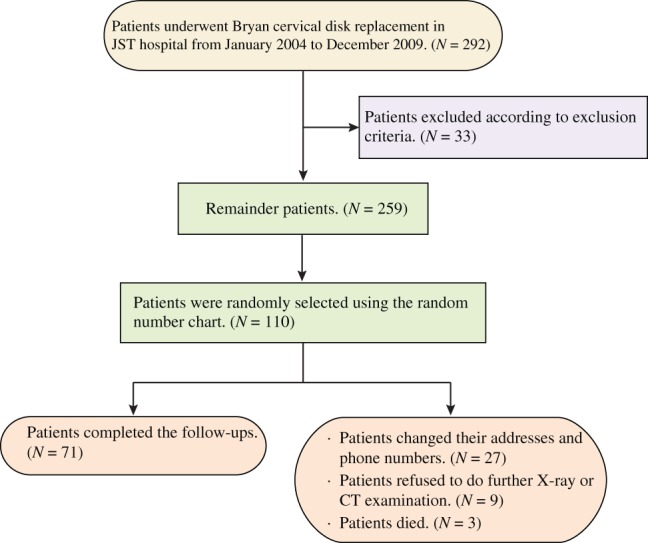
Flow diagram for the inclusion of patients. JST, Ji Shui Tan.
Computed Tomography Scan
The CT data were acquired before the operation and at the final follow‐up using an Aquilion 64‐slice scanner (Toshiba, Tokyo, Japan). The axial, sagittal, and coronal reconstructions for CT data were achieved using Mimics14.0 (Materialise, Belgium); the reconstruction slice thickness was 0.5 mm and the reconstruction field was from C2 to T2. Kouyoumdjian et al. introduced the reconstruction method previously, where the plane parallel to the posterior wall of the vertebra underlying the operated level was used as the coronal plane, the perpendicular plane to the coronal plane was used as the sagittal plane, and the axial plane was the plane parallel to the superior end plate of the vertebra underlying the operating level20.
Paravertebral Ossification Classification
The novel PO classification system was based on the rebuilt images. The axial plane of the Bryan disk level before surgery and at final follow‐up was divided into 12 equal sections, numbered from 1 to 12 clockwise to provide PO position information (Fig. 2). The severity of PO was graded into five categories based on the classification method that we mentioned in our previous study6. Grade 0 means no bone present beyond normal vertebral landmarks; Grade I means PO detectable up to the disk space, but not in the anatomic interdiscal space; Grade II means PO growing into the disk space, possibly affecting the function of the prosthesis; Grade III means the ROM of the vertebral endplates is blocked by the formation of PO on flexion‐extension or lateral bending radiographs; Grade IV means bridging trabecular bone formation causing inadvertent arthrodesis bony ankylosis and <3° of motion on flexion‐extension or lateral bending radiographs. The positional section's PO grade was assessed respectively in each positional section, and both sagittal and coronal views were considered (Figs 3, 4, 5). The highest grade of PO in all 12 sections was defined as the segment's PO grade, and the highest segment's grade was defined as the patient's PO grade in patients who had more than one cervical disc being replaced.
Figure 2.
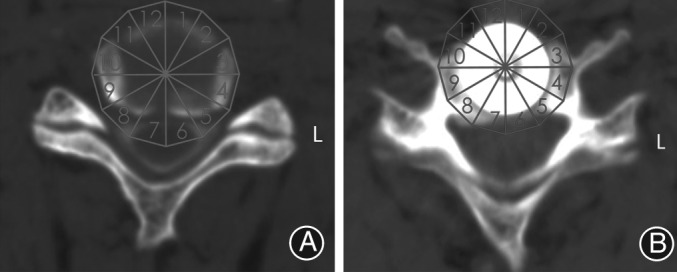
Axial plane of Bryan disc level before surgery (A) and at final follow‐up (B) was equally divided into 12 sections, numbered from 1 to 12 clockwise.
Figure 3.
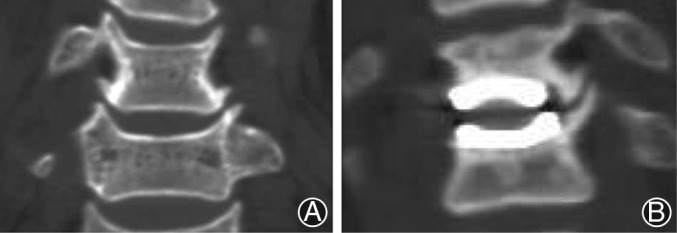
Grade I paravertebral ossification (PO). PO is detectable up to the disc space but not in the anatomic interdiscal space in both preoperation (A) and final follow‐up (B) coronal reconstruction computed tomography.
Figure 4.
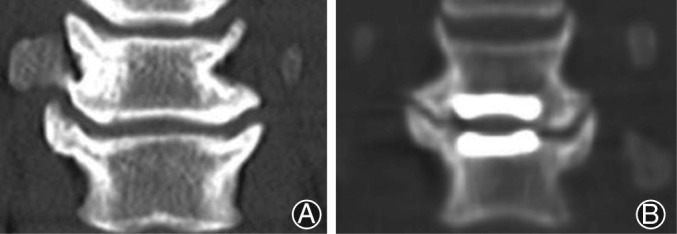
Grade II paravertebral ossification (PO). PO is growing into the disc space, possibly affecting the function of the prosthesis in both preoperation (A) and final follow‐up (B) coronal reconstruction computed tomography.
Figure 5.

Grade III and grade IV paravertebral ossification (PO). In this final follow‐up computed tomography image, PO is shown to block the upper segment's endplates, and in the lower segment, the PO caused bony ankylosis. The range of motion needs to be examined to confirm the classification.
Other Parameters
Other outcome parameters were also measured pre‐surgery and at final follow‐up using the PACS system (Rogan‐Delft, Veenendaal, Netherlands), including the ROMs on flexion, neutral and extension radiographs, respectively. The Japanese Orthopedic Association (JOA) scores and Neck Disability Index (NDI) were also recorded for evaluating the neural condition at both time points.
All the ROM measuring and PO grading results were from two independent orthopedic spine surgeons who were blinded to the purpose of this study and were not developers of this grading method. Each observer measured and graded the radiographs twice, and all the radiographs were presented in random order to reduce the possibility of recall. As for ROM, we used the mean values of the four measured data points for final analysis; however, for the PO grading, a senior orthopedic surgeon determined the final PO grade in case of disagreement caused by clinical experience.
Statistical Methods
All statistical analyses were performed using SPSS version 20.0 for Windows (Chicago, IL). Differences were considered statistically significant for P < 0.05. All continuous variable data were assessed for normality using Shapiro–Wilk test statistics and P‐values for independent t‐tests, and parametric t‐tests were used if the normality test was passed. For categorical variable data, the χ2‐test and Fisher exact test were used. However, we used the Mann–Whitney U‐test and Wilcoxon signed‐rank test to deal with grading variables and continuous variable data that failed the Shapiro–Wilk test. Binary logistic regression and χ2‐tests were used to estimate the odds ratio of risk factors in developing high‐grade PO after surgery.
The interobserver and intraobserver reliability for two independent raters was also assessed using the reliability statistics by intraclass correlation coefficient (ICC) for the grading system. The ICC values were graded using the following criteria: excellent for values in the 0.9–1.0 range, good for 0.7–0.89, fair/moderate for 0.50–0.69, low for 0.25–0.49, and poor for 0.0–0.24.
Results
General Results
Seventy‐one patients (49 men and 22 women) with 82 replaced segments completed the follow‐up, 61 patients with one‐level cervical disc replacement, 9 patients with two‐level cervical disc replacement and 1 patient with a three‐level cervical disc replacement. The mean age of all patients was 44.9 years (ranging from 25 to 70 years), and the mean follow‐up time was 79.2 months (ranging from 57 to 108 months). We also assessed the level of implanted device: 4 artificial discs in C3–4; 16 in C4–5; 48 in C5–6; and 14 in C6–7.
Paravertebral Ossification's Grade and Distribution
Regardless of whether it is detected preoperation or at final follow‐up, PO was common in all patients, and the distribution mode of PO was similar at these two time points, although the common grade was different (P < 0.001). PO under grade III (84.1%) was commonly present preoperation, and PO above grade II (67.1%) was common at final follow‐up; however, at both time points, nearly all high‐grade PO (grade III and grade IV) was concentrated at sections 3–5 and 8–10, where the uncovertebral joint is located. The exact distribution of PO in each section is shown in Table 1.
Table 1.
PO distribution preoperation and at final follow‐up according to CT
| Section's PO grade | Sections | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| Preoperation | ||||||||||||
| 0 | 71 | 50 | 7 | 5 | 3 | 42 | 54 | 4 | 2 | 8 | 40 | 75 |
| I | 10 | 30 | 59 | 42 | 35 | 31 | 26 | 44 | 47 | 61 | 36 | 6 |
| II | 1 | 2 | 15 | 33 | 37 | 9 | 2 | 31 | 29 | 13 | 6 | 1 |
| III and IV | 0 | 0 | 1 | 2 | 7 | 0 | 0 | 3 | 4 | 0 | 0 | 0 |
| Final follow‐up | ||||||||||||
| 0 | 77 | 25 | 2 | 1 | 2 | 46 | 54 | 2 | 0 | 0 | 17 | 79 |
| I | 5 | 32 | 17 | 12 | 16 | 9 | 15 | 26 | 12 | 15 | 35 | 3 |
| II | 0 | 14 | 41 | 35 | 37 | 22 | 8 | 36 | 43 | 51 | 26 | 0 |
| III and IV | 0 | 11 | 22 | 34 | 27 | 5 | 5 | 18 | 27 | 16 | 4 | 0 |
CT, computed tomography; PO, paravertebral ossification.
Clinical Results
The physiological motion range of related segments was preserved well in patients who have low‐grade PO (grade I and grade II) at final follow‐up; however, the extension ROM (P = 0.002), flexion ROM (P = 0.001), and total ROM (P < 0.001) of the related segments was not maintained well in high‐grade PO patients when compared with ROMs preoperation (Table 2). The independent t‐test also demonstrated that high‐grade PO at final follow‐up has lower extension ROM (P = 0.003), flexion ROM (P = 0.014), and total ROM (P = 0.001).
Table 2.
Comparison of range of motion pre‐surgery and at final follow‐up (mean ± SD, °)
| Movement | Low‐grade PO segments (27 levels) | High‐grade PO segments (55 levels) | All segments (82 levels) |
|---|---|---|---|
| Extension | |||
| Pre‐surgery | 2.96 ± 2.36 | 3.50 ± 2.79 | 3.32 ± 2.65 |
| Final follow‐up | 3.59 ± 2.79 | 1.82 ± 2.27 | 2.40 ± 2.58 |
| P‐value | 0.275 | 0.002 | 0.027 |
| Flexion | |||
| Pre‐surgery | 6.85 ± 3.42 | 6.34 ± 3.41 | 6.51 ± 3.40 |
| Final follow‐up | 6.23 ± 2.61 | 4.44 ± 3.21 | 5.03 ± 3.13 |
| P‐value | 0.375 | 0.001 | 0.001 |
| Total | |||
| Pre‐surgery | 9.80 ± 3.65 | 9.73 ± 4.03 | 9.75 ± 3.89 |
| Final follow‐up | 10.03 ± 3.73 | 6.63 ± 4.21 | 7.75 ± 4.34 |
| P‐value | 0.801 | <0.001 | <0.001 |
High‐grade PO, grade III and grade IV PO; Low‐grade PO, grade I and grade II PO; PO, paravertebral ossification; ROM, range of motion.
As for neurological symptoms, all patients showed significant improvement in JOA and NDI scores, including the patients who had high‐grade PO at final follow‐up. In addition, the independent t‐test also showed that there was no significance difference in JOA and NDI scores between high‐grade and low‐grade PO at final follow‐up.
Male gender, old age, long follow‐up time, poor pre‐surgery neurological condition, low pre‐surgery ROM, high level operation, and multilevel arthroplasty do not appear to be risk factors for high‐grade PO formation post‐surgery. The only predisposing factor for high‐grade PO after operation was pre‐existing PO preoperation (OR = 4, P = 0.012, Table 3).
Table 3.
Relationship between pre‐exist PO and postoperation PO (χ2‐test, LSD)
| PO grade preoperation | PO grade at final follow‐up (segments) | Comparison pairs | OR | P * | CI | |
|---|---|---|---|---|---|---|
| Low‐grade | High‐grade | |||||
| I | 12 | 7 | III and IV vs II | 1.371 | 0.027 | 1.154–1.629 |
| II | 15 | 35 | II and I | 4 | 0.012 | 1.317–12.152 |
| III and IV | 0 | 13 | III and IV vs I | 2.857 | <0.001 | 1.572–5.192 |
P values were corrected with the Bonferroni test. CI, confidential interval; High‐grade, grade III and grade IV PO; Low‐grade, grade I and grade II PO; LSD, least significant difference; PO, paravertebral ossification; OR, odds ratio.
Using ICC reliability statistics, the intraobserver reliability between two different spine surgeons and the interobserver reliability were both higher than 0.891.
Discussion
Cervical artificial disc replacement remains a relatively new technique in cervical surgery; it is a recent innovation in the management of degenerative cervical spine disease that is resistant to conservative treatment. Intuitively, the CADR maintaining the physiological motion in the cervical spine, if possible, makes perfect sense16. However, recent reports have shown a relatively high incidence of PO after CADR. Although PO does not affect clinical outcomes, it does decrease the mobility of affected segments in the long run, and may even lead to complete ankylosis, which is responsible for adjacent segment degeneration and disease, and this is in conflict with CADR1, 7, 8, 9, 10, 11. This means that we have to evaluate PO after CADR carefully because of its tremendous effect, especially in long‐term follow‐ups. However, long‐term follow‐ups for PO after CADR are rare; furthermore, CT scans are also not commonly used in recent studies when evaluating PO after CADR. It is obvious that CT will add more details that might not show in X‐ray images. Studies need CT scans to verify and supply more information for the McAfee classification when assessing the occurrence of PO after CADR14, 17, 18, although the most widely‐used McAfee classification is based on X‐rays12.
The PO located beside the bilateral uncovertebral joints is not easy to see using X‐rays, and will result in false negative judgments (Fig. 6). If we simply use the X‐ray to evaluate PO incidence preoperation and at final follow‐up, the grade III PO percentage preoperation and at final follow‐up is 0% and 4.9% respectively, and the grade IV PO percentage is 0% and 8.5%, respectively. The omission diagnostic rate for grade IV PO at final follow‐up is as high as 66.7%, which dramatically affects the complete assessment of PO in CADR and can result in misunderstandings about this novel technique.
Figure 6.
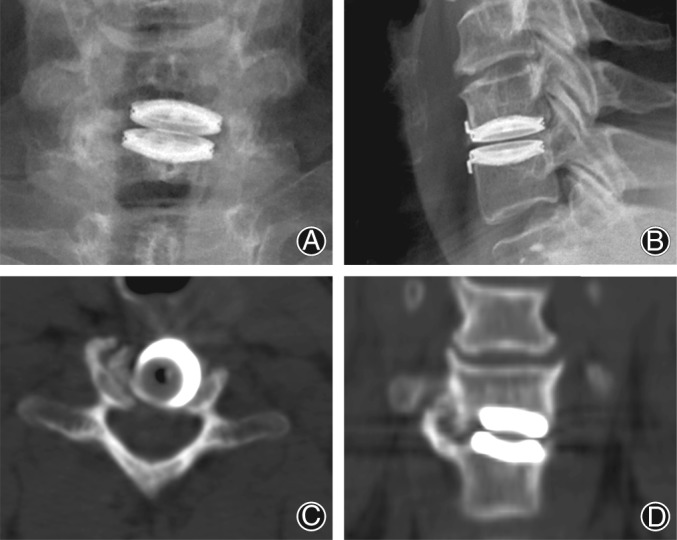
The paravertebral ossification (PO) located beside the uncovertebral joints is not easy to see through X‐ray photographs (A and B); however, it can be easily seen through computed tomography (C, D).
Cervical artificial disc replacement is designed to maintain cervical motion, and can preserve mobility for a relative long time. In our study, CADR preserved a certain degree of ROM at final follow‐up compared with preoperation; however, PO affected this kind of protection, especially high‐grade PO, which decreased the ROM more significant than low‐grade PO. Although high‐grade PO affected mobility in related segments and might induce segmental fusion in some cases, the artificial discs still delayed the adjacent level degeneration and protect patients from adjacent level disease. CADR is also supposed to achieve neural decompression; however, whether motion preservation is correlated with improved clinical outcomes is still unclear5. Theoretically, the PO presented at final follow‐up will cause neurological symptoms if it grows out into the spinal canal. However, in our study, the neurological recovery was not affected by PO in the long run, and there was no significance difference between the low‐grade PO group and the high‐grade PO group in JOA and NDI scores at final follow‐up, which is consistent with previous research21. These long‐term data and device‐specific follow‐ups will provide essential evidence for the use of Bryan disc implantation.
Paravertebral ossification has been reported in many parts of the body, including the hip, shoulder, and elbow, and is always associated with musculoskeletal trauma or nervous system injury22. There might be common etiology and pathology in PO in the hip and knee joint and PO in CADR; however, the etiology and pathology remain unclear so far. The potential risk factors for PO after CADR include old age, male sex, surgical indications, techniques, inflammation, and multilevel arthroplasty8, 11, 14, 17, 23. However, according to our research, male gender, old age, long follow‐up time, poor pre‐surgery neurological condition, low pre‐surgery ROM, high level operation, and multilevel arthroplasty do not appear to be risk factors for high‐grade PO formation post‐surgery. The only predisposing factor for high‐grade PO after operation is pre‐existing PO preoperation. This may because we do not intensively remove PO during the standard procedure process of Bryan disc replacement, and the low‐grade PO hidden at the bilateral uncovertebral joint finally becomes high‐grade PO at final follow‐up. Another possible reason is that the CADR changes the biomechanical environment in the related segment and accelerates the degeneration.
Furthermore, no matter whether detected preoperation or at final follow‐up, high‐grade PO was all concentrated at the bilateral uncovertebral joint. The occurrence rate for high‐grade PO in bilateral uncovertebral joint was 60.2% at final follow‐up. Even if the PO is excised during the cervical artificial disc planting process, it still can be newly generated at the bilateral uncovertebral joint locations in the long term24. Pre‐existing PO preoperation is a risk factor for high‐grade PO after operation, and PO will affect cervical motion in the long run, so whether we should perform resection of the whole uncovertebral joint to gain long‐term preserved mobility is a question still under discussion.
The uncovertebral joint is a unique structure at the cervical spine25. The term “processus uncinatus” first appeared in 1893, when introduced by Trolard26. The bilateral uncovertebral joints served as two guide rails to control the movement of the cervical spine, as they control the anterior and posterior translation that occurs during flexion and extension movements in the sagittal plane. During the flexion and extension movements, the posterolateral aspects of the uncovertebral joints limit the coronal plane motion as the vertebra above translates to the vertebra below27. It contributes in excess of 60% of the stability of the spinal motion segment in extension and flexion28. After the appearance of high‐grade PO after CADR, the uncovertebral joint is limited more in sagittal and coronal motion. According to Wolff's law, it is easy to grow PO at the uncovertebral joint location because of the force generated during cervical movement. With CADR, which changes the biomechanical environment to preserve more cervical motion, the degeneration of the related segment's articulations may accelerate, which makes it easier for PO to grow. Complete resection of the bilateral uncovertebral joints may decrease the risk of progressive PO growth and allow for larger footprint disc prosthesis insertion, which also decreases the risk of implant subsidence and migration24, 29. However, complete resection will also increase the risk of vertebral artery injury during surgery and may cause hypermobility exceeding physiological levels of motion24. Therefore, whether the uncovertebral joints should be resected during the Bryan disc CADR procedure cannot be decided by our current study, and we have to make the choice between motion stability and motion range.
Conclusions
This study is a device‐specific follow‐up with long‐term data, that uses a novel CT classification system to evaluate PO after Bryan disc CADR. The novel CT image‐based PO classification system has good intraobserver and interobserver reliability, and it helped us to learn more about PO. The incidence of PO after Bryan cervical disc replacement is relatively high. High‐grade PO will affect the ROM after surgery, although it does not affect neurological symptoms. High‐grade PO is mainly distributed at the uncovertebral joint, and the only risk factor for high‐grade PO postoperation is pre‐existing PO before the operation; however, it is still unclear whether the uncovertebral joints should be resected in the current study. We have to make the choice between motion stability and motion range in the implanted segment.
Disclosure: The authors have no conflict of interest to declare.
References
- 1. Heidecke V, Burkert W, Brucke M, Rainov NG. Intervertebral disc replacement for cervical degenerative disease‐‐clinical results and functional outcome at two years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochir, 2008, 150: 453–459, discussion 459. [DOI] [PubMed] [Google Scholar]
- 2. Zhang X, Zhang X, Chen C, et al. Randomized, controlled, multicenter, clinical trial comparing BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion in China. Spine (Phila Pa 1976), 2012, 37: 433–438. [DOI] [PubMed] [Google Scholar]
- 3. Cheng L, Nie L, Zhang L, Hou Y. Fusion versus Bryan cervical disc in two‐level cervical disc disease: a prospective, randomised study. Int Orthop, 2009, 33: 1347–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rhee JM. Cervical arthroplasty: a success, failure, or both? Spine J, 2010, 10: 731–732. [DOI] [PubMed] [Google Scholar]
- 5. Demetriades AK, Ringel F, Meyer B. Cervical disc arthroplasty: a critical review and appraisal of the latest available evidence. Adv Tech Stand Neurosurg, 2014, 41: 107–129. [DOI] [PubMed] [Google Scholar]
- 6. Tian W, Han X, Liu B, He D, Lv Y, Yue J. Generation and development of paravertebral ossification in cervical artificial disc replacement: a detailed analytic report using coronal reconstruction CT. Clin Spine Surg, 2016, doi: 10.1097/BSD.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 7. Yi S, Kim KN, Yang MS, et al. Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976), 2010, 35: 1556–1561. [DOI] [PubMed] [Google Scholar]
- 8. Suchomel P, Jurak L, Benes V 3rd, Brabec R, Bradac O, Elgawhary S. Clinical results and development of heterotopic ossification in total cervical disc replacement during a 4‐year follow‐up. Eur Spine J, 2010, 19: 307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lee JH, Jung TG, Kim HS, Jang JS, Lee SH. Analysis of the incidence and clinical effect of the heterotopic ossification in a single‐level cervical artificial disc replacement. Spine J, 2010, 10: 676–682. [DOI] [PubMed] [Google Scholar]
- 10. Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976), 2006, 31: 2802–2806. [DOI] [PubMed] [Google Scholar]
- 11. Leung C, Casey AT, Goffin J, et al. Clinical significance of heterotopic ossification in cervical disc replacement: a prospective multicenter clinical trial. Neurosurgery, 2005, 57: 759–763. [DOI] [PubMed] [Google Scholar]
- 12. McAfee PC, Cunningham BW, Devine J, Williams E, Yu‐Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech, 2003, 16: 384–389. [DOI] [PubMed] [Google Scholar]
- 13. Park JH, Rhim SC, Roh SW. Mid‐term follow‐up of clinical and radiologic outcomes in cervical total disk replacement (Mobi‐C): incidence of heterotopic ossification and risk factors. J Spinal Disord Tech, 2013, 26: 141–145. [DOI] [PubMed] [Google Scholar]
- 14. Yi S, Shin DA, Kim KN, et al. The predisposing factors for the heterotopic ossification after cervical artificial disc replacement. Spine J, 2013, 13: 1048–1054. [DOI] [PubMed] [Google Scholar]
- 15. Sasso RC, Best NM, Metcalf NH, Anderson PA. Motion analysis of Bryan cervical disc arthroplasty versus anterior discectomy and fusion: results from a prospective, randomized, multicenter, clinical trial. J Spinal Disord Tech, 2008, 21: 393–399. [DOI] [PubMed] [Google Scholar]
- 16. Alvin MD, Abbott EE, Lubelski D, et al. Cervical arthroplasty: a critical review of the literature. Spine J, 2014, 14: 2231–2245. [DOI] [PubMed] [Google Scholar]
- 17. Wu JC, Huang WC, Tu TH, et al. Differences between soft‐disc herniation and spondylosis in cervical arthroplasty: CT‐documented heterotopic ossification with minimum 2 years of follow‐up. J Neurosurg Spine, 2012, 16: 163–171. [DOI] [PubMed] [Google Scholar]
- 18. Wu JC, Huang WC, Tsai TY, et al. Multilevel arthroplasty for cervical spondylosis: more heterotopic ossification at 3 years of follow‐up. Spine (Phila Pa 1976), 2012, 37: E1251–E1259. [DOI] [PubMed] [Google Scholar]
- 19. Tian W, Han X, Liu B, et al. Clinical and radiographic results of cervical artificial disc arthroplasty: over three years follow‐up cohort study. Chin Med J (Engl), 2010, 123: 2969–2973. [PubMed] [Google Scholar]
- 20. Kouyoumdjian P, Bronsard N, Vital JM, Gille O. Centering of cervical disc replacements: usefulness of intraoperative anteroposterior fluoroscopic guidance to center cervical disc replacements: study on 20 discocerv (scient'x prosthesis). Spine (Phila Pa 1976), 2009, 34: 1572–1577. [DOI] [PubMed] [Google Scholar]
- 21. Cho YH, Kim KS, Kwon YM. Heterotopic ossification after cervical arthroplasty with ProDisc‐C: time course radiographic follow‐up over 3 years. Korean J Spine, 2013, 10: 19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol, 2005, 34: 609–619. [DOI] [PubMed] [Google Scholar]
- 23. Tu TH, Wu JC, Huang WC, et al. Heterotopic ossification after cervical total disc replacement: determination by CT and effects on clinical outcomes. J Neurosurg Spine, 2011, 14: 457–465. [DOI] [PubMed] [Google Scholar]
- 24. Snyder JT, Tzermiadianos MN, Ghanayem AJ, et al. Effect of uncovertebral joint excision on the motion response of the cervical spine after total disc replacement. Spine (Phila Pa 1976), 2007, 32: 2965–2969. [DOI] [PubMed] [Google Scholar]
- 25. Hartman J. Anatomy and clinical significance of the uncinate process and uncovertebral joint: a comprehensive review. Clin Anat, 2014, 27: 431–440. [DOI] [PubMed] [Google Scholar]
- 26. Pait TG, Killefer JA, Arnautovic KI. Surgical anatomy of the anterior cervical spine: the disc space, vertebral artery, and associated bony structures. Neurosurgery, 1996, 39: 769–776. [DOI] [PubMed] [Google Scholar]
- 27. Milne N. The role of zygapophysial joint orientation and uncinate processes in controlling motion in the cervical spine. J Anat, 1991, 178: 189–201. [PMC free article] [PubMed] [Google Scholar]
- 28. Petty P. Surgical anatomy of the anterior cervical spine: the disc space, vertebral artery, and associated bony structures. Neurosurgery, 1997, 41: 325–325. [DOI] [PubMed] [Google Scholar]
- 29. Kotani Y, McNulty PS, Abumi K, Cunningham BW, Kaneda K, McAfee PC. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine. A biomechanical study. Spine (Phila Pa 1976), 1998, 23: 1559–1565. [DOI] [PubMed] [Google Scholar]


