Abstract
Objective
To evaluate the clinical outcomes of anterior and posterior instrumentation with different debridement and graft fusion methods for multi‐level contiguous thoracic spinal tuberculosis.
Methods
We retrospectively evaluated 81 patients with multi‐level contiguous thoracic spinal tuberculosis who underwent anterior or posterior instrumentation combined with different methods of debridement, decompression, and graft fusion from January 2002 to December 2012. All patients were divided into an anterior instrumentation group and a posterior instrumentation group. In the anterior instrumentation group, there were 39 patients who underwent transthoracic debridement. In the posterior instrumentation group, there were 34 patients who underwent trans‐costotransverse decompression and strut grafting with posterior instrumentation, and another 8 patients underwent combined anterior debridement and strut grafting with posterior instrumentation in a single‐stage or two‐stage procedure. The kyphotic angles were calculated from lateral spinal X‐rays using the modified Konstam method. The symptoms and signs of tuberculosis, fusion level, fusion time of the bone graft, average kyphosis angle, average correction, average loss of correction, and clinical complications were recorded. The average follow‐up period was 37 months (range, 17–72 months).
Results
The cohort consisted of 47 males and 34 females with an average age of 38 years. The mean durations of the operations were 3.5 ± 0.4 h in the anterior group and 4.0 ± 0.3 h in the posterior group (P < 0.05). The mean blood loss volumes during surgery were 450 ± 42 and 560 ± 51 mL for the anterior group and the posterior group, respectively (P < 0.01). The kyphotic deformities were corrected from 32.1° ± 10.3° to 10.2° ± 2.1° in the anterior group and from 33.8° ± 11.7° to 12.6° ± 2.7° in the posterior group (P < 0.01). The neurologic statuses of the 23 patients with preoperative neurologic deficits improved in each group. Fusion was confirmed radiographically at 5.4 ± 1.2 months (range, 4–12 months) in the anterior group and 5.6 ± 1.4 months (range, 4–13 months) in the posterior group (P > 0.05). Postoperative relapses were noted in 1 and 3 patients in the anterior and the posterior group, respectively.
Conclusion
Posterior instrumentation was more effective than anterior instrumentation in the correction of kyphosis and the maintenance of the correction. However, postoperative sinus formation was more frequent in patients who underwent a single‐stage posterior procedure.
Keywords: Anterior, Instrumentation, Multi‐level, Posterior, Thoracic spinal tuberculosis
Introduction
The World Health Organization (WHO) has estimated that there were 9.6 million incident cases of tuberculosis and that 1.5 million people died from this disease in 20141. The most common form of extrapulmonary tuberculosis is spinal tuberculosis, which occurs in 1%–3% of all tuberculosis patients and can lead to severe complications. It is generally accepted that thoracic spinal tuberculosis is more dangerous than the lumbar type because of the ability to cause deformity and paraplegia, which makes surgical intervention for this form of tuberculosis more urgent. The aim of the surgical treatment of thoracic spinal tuberculosis is the eradication of the focus and the prevention or treatment of neurological deficits and deformities.
A proportion of cases of thoracic spinal tuberculosis have the potential to involve multi‐level contiguous vertebrae (i.e. three or more levels) due to insidious onset, delays in diagnoses, malpractice, and other factors. The lesions that result from multi‐level contiguous spinal tuberculosis are more extensive and involve more serious destruction of the vertebrae, which increases the susceptibility to instability, kyphotic deformities, and compression of the spinal cord. Therefore, it is more important to identify the best methods for the reconstruction of the stability of the spine following radical debridement and decompression of the spinal cord. The “Hong Kong operation” implements debridement and bone grafting in a single‐stage approach. However, graft failures, including slippage, absorption, and breakage, are major drawbacks of this method, particularly when more than three vertebrae are involved2, 3, 4. Due to developments in international fixation, the stability of the spine can be efficiently reconstructed following radical debridement and graft fusion.
The surgical procedures that are currently used for the treatment of thoracic spinal tuberculosis can be summarized as follows: (i) anterior radical debridement and strut grafting with instrumentation; (ii) posterolateral decompression and strut grafting with posterior instrumentation; and (iii) anterior radical debridement and strut grafting with posterior instrumentation. According to the literature, the above surgical procedures can all achieve good results in the treatment of thoracic spinal tuberculosis; however, choosing the appropriate surgical procedure for multi‐level contiguous thoracic spinal tuberculosis is often difficult and should be determined according to the position and extent of the foci, the patient's general condition, and the experience of the surgeon.
Thus far, there is no research related to internal fixation that has compared the outcomes of each instrumentation modality in terms of the correction of the kyphotic deformities, correction losses, fusion times, relapse rates, and internal fixation‐related complications. Therefore, we have reported on a cohort of 81 cases with multi‐level contiguous thoracic spinal tuberculosis in the exudative stage that were treated with different surgical procedures. The purpose of this study was to compare the outcomes of treatments utilizing anterior and posterior instrumentations with different debridement and bone grafting procedures.
Materials and Methods
Inclusion and Exclusion Criteria
The eligibility criteria were: (i) more than three continuous thoracic vertebrae involved; and (ii) a minimum follow‐up period of 18 months. The exclusion criteria were: (i) non‐compliance with anti‐tuberculosis chemotherapy; and (ii) being lost to follow‐up or death.
Patient Population and General Characteristics
A total of 97 consecutive adult patients who were treated in our hospital from January 2002 to December 2012 for multi‐level contiguous thoracic spinal tuberculosis were reviewed. Overall, complete follow‐up data were available for 81 (83.5%) patients whose average age was 38 years (range, 17–68 years), including 47 males and 34 females. The Cobb angles were less than 30° in 42 patients with kyphotic deformities and greater than 30° in 39 patients. Neurologic examinations were conducted according to the American Spinal Injury Association (ASIA) classification, which revealed Grade A lesions in 2, B lesions in 5, C lesions in 7, and D lesions in 9 patients5. The radiologic manifestation included paraspinal abscess in 78 patients and sequestrum in 69 patients. The diagnoses were made based on the histories, clinical examinations, laboratory results, and radiologic imaging. Definitive diagnoses were made based on histological examinations of the tissues removed during the surgeries. According to the instrumentation modality, the patients were divided into an anterior instrumentation group (anterior group) and a posterior instrumentation group (posterior group).
Preoperative Procedure
The patients were administered anti‐tuberculosis drugs, including isoniazid (5 mg/kg), rifampicin (10 mg/kg), ethambutol (15 mg/kg), and pyrazinamide (25 mg/kg), for 2–5 weeks prior to the operations. Severe co‐morbidities, such as tuberculous pleuritis and tuberculous meningitis, were first controlled even in patients with paresis or paraplegia. When the erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) level exhibited significant downward trends and any hypoproteinemia and anemia had been cured, the operations were performed. The average values of ESR were 41.4 ± 6.2 mm/1 h in the anterior group and 42.5 ± 7.3 mm/1 h in the posterior group, and the average values of CRP were 7.5 ± 4.4 mg/L in the anterior group and 8.2 ± 5.4 mg/L in posterior group.
Operative Procedures
Anterior group
A total of 29 patients underwent transthoracic debridement with anterior instrumentation. These patients underwent anterior debridement, spinal‐cord decompression, and distraction to correct the kyphosis and the implantation of a titanium cage filled with morselized rib bone and/or allograft bone or a large piece of auto‐iliac bone with one‐stage anterior plate or screw‐rod instrumentation (Fig. 1). If the remaining portion of the vertebra was less than 50% of the original, internal fixation screws were placed in an adjacent normal vertebral body6.
Figure 1.
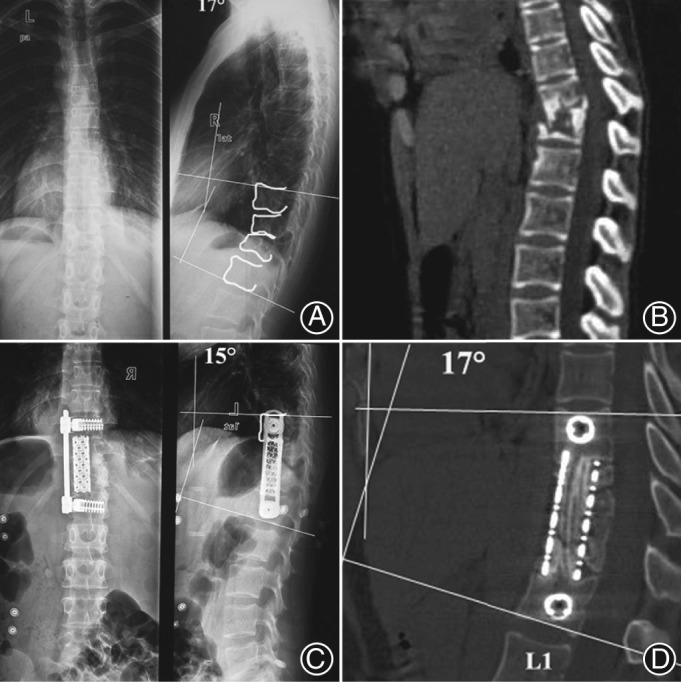
A 42‐year‐old woman who sustained a T 11–12 lesion with bone destruction and kyphotic deformity was treated by anterior debridement, spinal cord decompression, distraction to correct kyphosis, and titanium cage filled with morselized rib bone and allograft bone grafting in T 11–L 1. (A, B) Preoperative radiological images are shown. (C) Postoperative roentgenographs show that the kyphosis angle was corrected by 2°. (D) Graft fusion and a 2° loss of correction in local kyphosis angle were seen 2 years postoperatively.
Posterior group
Thirty‐four patients underwent trans‐costotransverse decompression and strut grafting with posterior instrumentation. Pedicle screws were placed at least two levels superior and inferior to the level of decompression (Figs 2, 3). Unilateral or bilateral costotransversectomies were performed to expose the foci. Appropriately sized titanium cages filled with morselized rib bone and/or allograft bone or a large piece of auto‐iliac bone or rib bone were imbedded in the interbody following radical debridement. Moreover, 8 patients underwent combined anterior debridement and strut grafting with posterior instrumentation in a single‐stage or two‐stage procedure (Fig. 4).
Figure 2.
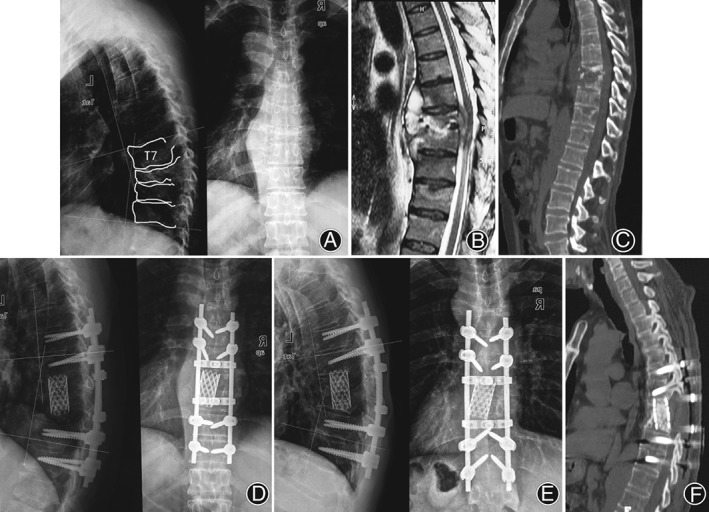
A 49‐year‐old male sustained a T 7–10 lesion with bone destruction and formation of epidural cold abscess and kyphotic deformity was treated by posterolateral decompression and strut grafting with posterior instrumentation. Preoperative ASIA Grade was A grade, and was D grade at the final follow‐up. (A–C) Preoperative radiography, computed tomography (CT) scan, and magnetic resonance images are shown. (D) Postoperative radiography imaging showed that kyphosis angle was corrected by 6°. (E, F) Graft fusion and a 5° loss of correction in local kyphosis angle were seen 1 year postoperatively.
Figure 3.
A 56‐year‐old female who sustained T 3–5 vertebral tuberculosis with neurological deficit was treated by posterolateral decompression and strut grafting with posterior instrumentation in a single‐stage procedure. (A–D) Preoperative radiography, computed tomography scan, and magnetic resonance images are shown. (E, F) Radiography and magnetic resonance images at the final follow‐up show that the thoracic spinal cord had sufficient decompression. Preoperative ASIA Grade was C grade, and was E grade at the final follow‐up.
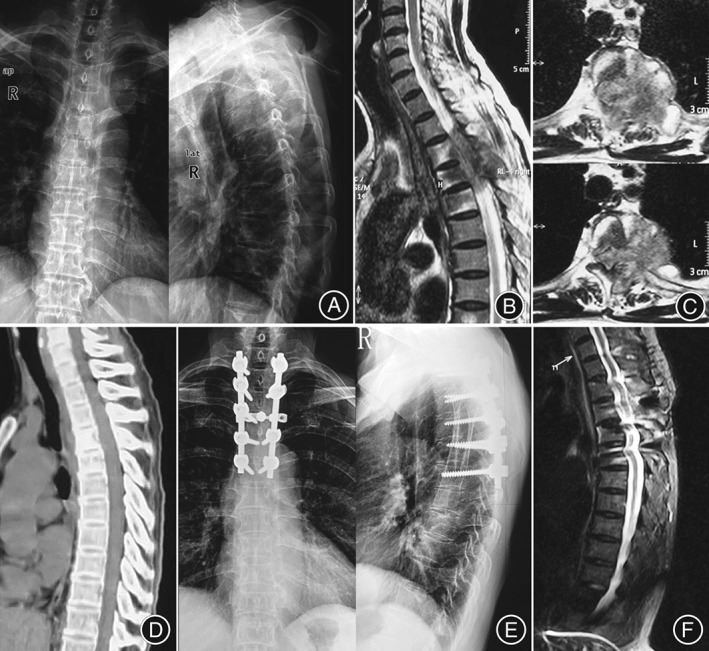
Figure 4.

A 52‐year‐old female with T 5–8 vertebrae involvement and paraplegia, who underwent a single‐stage posterior instrumentation combined with anterior debridement and rib bone grafting. (A–C) Preoperative radiography, computed tomography (CT) scan, and magnetic resonance images are shown. (D) Radiography demonstrated that satisfactory graft union was achieved 3 years postoperatively. ASIA Grade was B preoperatively and was E at the final follow‐up.
Postoperative Management and Evaluations
The standard chemotherapy consisting of isoniazid (5 mg/kg), rifampicin (10 mg/kg), ethambutol (15 mg/kg), and pyrazinamide (25 mg/kg) was administered for 3 months after the operations. Subsequently, a regimen of rifampicin, isoniazid, and ethambutol was continued for at least 9 months. Thoracolumbosacral orthosis support was maintained for at least 3 months postoperatively. All patients were X‐rayed, and the erythrocyte sedimentation rate (ESR), C‐reactive protein (CRP) levels, hepatic functions, and other parameters were examined at 1‐month intervals for the first 3 months, 3‐month intervals for the next 9 months, 6‐month intervals for the second year and once per year thereafter. The patients were then followed up for 17–72 months (average, 37 months). The kyphotic angles were calculated from lateral spinal X‐rays with the modified Konstam method7. The symptoms and signs of tuberculosis, fusion level, fusion time of the bone graft, average kyphosis angle, average correction, average loss of correction, and clinical complications were recorded.
Statistical Analysis
Student's t‐test was used to analyze the statistical significance of the differences between groups. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 16.0 software (SPSS, Chicago, IL, USA).
Results
General Results
Three‐level thoracic spinal tuberculosis was the most common thoracic spinal tuberculosis. The distribution of numbers of pathologic vertebrae is presented in Table 1. The histopathologic examination results were suggestive of tuberculosis in all cases, but the organisms were isolated for Mycobacterium tuberculosis culture in 35 of the 81 cases. The organisms were sensitive to first‐line antitubercular drugs in all 35 cases. The mean durations of the operations were 3.5 ± 0.4 hours in the anterior group and 4.0 ± 0.3 hours in the posterior group (P < 0.05). The mean blood loss volumes during surgery were 450 ± 42 mL and 560 ± 51 mL for the anterior group and the posterior group, respectively (P < 0.01; Table 2). The local symptoms of all of the patients were significantly relieved 1–3 weeks postoperatively. The average preoperative and postoperative pain visual analog score (VAS) scores, and ESR and CRP values for all the patients are given in Table 2.
Table 1.
Distribution of the number of pathologic vertebrae
| Groups | 7 | 6 | 5 | 4 | 3 | Total |
|---|---|---|---|---|---|---|
| Anterior group | 0 | 0 | 2 | 7 | 28 | 37 |
| Posterior group | 2 | 4 | 7 | 8 | 23 | 44 |
Table 2.
Clinical outcomes of thoracic spinal tuberculosis treated by anterior and posterior instrumentation (mean ± SD)
| Index | Anterior group | Posterior group | t‐value | P value |
|---|---|---|---|---|
| Number of patients | 39 | 42 | — | — |
| Average operation time (h) | 3.5 ± 0.4 | 4.0 ± 0.3 | −2.015 | 0.047 |
| Average blood loss (mL) | 450 ± 42 | 560 ± 51 | −2.034 | 0.045 |
| ESR | ||||
| Preoperation (mm/1 h) | 41.4 ± 6.2 | 42.5 ± 7.3 | −1.482 | 0.164 |
| Postoperationoperation (mm/1 h) | 81.6 ± 7.7 | 82.3 ± 6.9 | −1.782 | 0.135 |
| 12 weeks postoperation (mm/1 h) | Normal | Normal | — | — |
| CRP | ||||
| Pre‐op | 7.5 ± 4.4 | 8.2 ± 5.4 | −1.531 | 0.092 |
| Post‐op | 16.9 ± 7.3 | 17.1 ± 8.5 | −1.468 | 0.157 |
| 12 weeks postoperation | Normal | Normal | — | — |
| VAS | ||||
| Preoperation | 8.5 ± 1.4 | 8.6 ± 1.7 | −0.721 | 0.213 |
| Postoperation | 2.6 ± 1.3 | 3.8 ± 1.5 | −2.021 | 0.027 |
| Final follow‐up | 1.8 ± 1.1 | 1.9 ± 1.3 | −2.021 | 0.118 |
| Fusion level | 2.3 ± 0. 5 | 3.2 ± 0.9 | −1.021 | 0.014 |
| Fusion time of bone graft (months) | 5.4 ± 1.2 | 5.6 ± 1.4 | −1.721 | 0.344 |
| Preoperative average kyphosis angle (°) | 32.1 ± 10.3 | 33.8 ± 11.7 | −2.021 | 0.091 |
| Average angle of correction (°) | 10.2 ± 2.1 | 12.6 ± 2.7 | −1.521 | 0.046 |
| Average angle loss of correction at final follow‐up (°) | 6.9 ± 1.9 | 5.6 ± 1.4 | −1.488 | 0.037 |
| Treatment failure | 3 | 4 | — | — |
| Instrumentation failure | 2 | 1 | — | — |
| Sinus formation | 1 | 3 | — | — |
CRP, C‐reaction protein; ESR, indicates erythrocyte sedimentation rate; VAS, Visual Analogue Scale; —, none.
Bone Graft Fusion
The fusion levels were 2.3 ± 0.5 in the anterior group and 3.2 ± 0.9 in the posterior group (P < 0.01). Fusion was confirmed radiographically at 5.4 ± 1.2 months (range, 4–12 months) in the anterior group and 5.6 ± 1.4 months (range, 4–13 months) in the posterior group (P > 0.05). Graft fusion was achieved in all patients at 4–13 months postoperatively.
Neurologic Improvement
Details of the preoperative and postoperative neurologic statuses are given in Table 3. All cases with neurological deficits achieved significant improvement postoperatively. In the anterior group, 10 of 11 patients recovered normal neurologic function and the 1 other case with ASIA Grade A recovered to D level. In the posterior group, 10 of 12 patients recovered to normal neurologic function and the other 2 cases recovered to ASIA Grade D level.
Table 3.
ASIA classification of the patients with neurological deficits preoperatively and at the final follow‐up (anterior group, posterior group)
| Preoperative grade | Total | Grade at the final follow‐up | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| A | 1, 1 | 1, 0 | 0, 1 | |||
| B | 2, 3 | 0, 1 | 2, 2 | |||
| C | 2, 5 | 0, 1 | 2, 4 | |||
| D | 6, 3 | 6, 3 | ||||
ASIA, American Spinal Injury Association.
Correction of Deformity
The kyphotic deformities were significantly improved with average correction angles of 10.2° in the anterior group and 12.6° in the posterior group (P < 0.01). At the final follow‐up, mean correction losses were 6.9° in the anterior group and 5.6° in the posterior group (P < 0.01). The average correction angle and mean correction loss between the preoperative and postoperative values and between the preoperative and final follow‐up values were found to be significant for both groups (P < 0.001). The differences between the postoperative and final follow‐up values were also found to be significant (P < 0.01; Table 2). The results revealed that posterior instrumentation was superior to anterior instrumentation in terms of correcting deformities and maintaining those corrections.
Complications
Three patients had operation‐related complications. In the anterior group, 1 patient suffered vertebral screw pullout 8 months after the operation, which was resolved after revision surgery by posterior instrumentation and anterior graft fusion. Another patient in the anterior group underwent a revision surgery because of pseudoarthrosis and subsidence of titanium mesh 12 months after the first procedure, and was finally cured. In the posterior group, 1 patient underwent a revision surgery because of pseudoarthrosis and pedicle screw broken 16 months after the first procedure, and achieved satisfactory bone union 4 months after the reoperation. Regarding postoperative local recurrence, 1 patient in the anterior group and three patients in the posterior group suffered sinus formation at the incision after the surgery and were successfully treated by excision of the sinus.
Discussion
Thoracic spinal tuberculosis accounts for approximately 50% of spinal tuberculosis cases and typically involves 1–2 vertebrae. However, in developing countries, such as China, the focus often extends across more than two vertebrae due to delays in diagnosis, malpractice, tuberculosis drug resistance, and other factors. Although the thoracic region has the support of the bony thorax, which makes it more stable than the lumbar region, multi‐level contiguous spinal tuberculosis increases patients’ susceptibilities to instability, kyphotic deformities, and paraplegia due to severe damage to the stability of the spine. Therefore, it is important to perform decompression of the spinal cord and reconstruct the stability of the spine based on chemotherapy. Our study revealed that unlike spinal cord injuries caused by thoracic spinal fractures, the spinal cord function of patients with multiple‐level contiguous thoracic spinal tuberculosis could be substantially recovered following decompression surgery.
The anterior approach has been increasingly applied since Oga reported on the security of titanium alloy implants for lesions due to spinal tuberculosis8. The advantages of anterior debridement and instrumentation are that the focus can be removed more thoroughly, strut grafting is easier and more precise, and the instrumentation can be applied through the same incision to reconstruct the stability of the spine. For some patients with multi‐level contiguous thoracic spinal tuberculosis, the instrumentation has to be fixed to adjacent vertebrae because the residual portion of the destroyed vertebra is too small for fixation. To date, the pullout strengths of the vertebral screws have not been evaluated in clinical and biomechanical research in situations in which the MRI signals of the vertebrae neighboring the focus are infiltrated by changes related to abscesses. The advantages of the single‐stage combined anterior–posterior approach are that the focus can be thoroughly removed, and the stability can be substantially reconstructed; however, the surgical trauma can be considerable9, 10, 11, 12, 13. Many researchers have highlighted the safety and efficacy of the use of the posterolateral, (trans‐costotransverse) approach alone2. Through this approach, the focus debridement, spinal cord decompression, bone graft fusion, instrumentation application, and kyphosis correction can be performed simultaneously. However, occasionally, one or two intercostal nerves have to be cut to perform the strut grafting via this approach. In addition, sinus formation is a risk of this approach because the lesion may connect with the posterior incision.
Zhang et al. indicate that the anterior, posterior, and combined anterior–posterior approaches can all result in ideal therapeutic effects in the treatment of thoracic spinal tuberculosis and suggest that the appropriate surgical procedure should be determined according to the position and extent of the lesion, the patient's general condition, and the types of complications14, 15. The anterior approach is indicated for mild kyphosis of less than 30° and for recurrent thoracic spinal tuberculosis following posterolateral decompression and strut grafting with posterior instrumentation16, 17. For patients with upper thoracic spinal tuberculosis, the scapula limits the degree of lateral exposure, and, thus, the transsternal approach has to be used. In our research, we found that the posterolateral approach has many advantages and is very practical. First, through the posterolateral approach, posterior instrumentation application, focal debridement, and fusion can all be performed through a single incision. Thus, this approach is more applicable for thoracic spinal tuberculosis with adjacent segment lesions, particularly for patients with poor pulmonary function or extensive pleural adhesions18. Second, through unilateral or bilateral facet joint resection and the excision of the adjacent costotransverse joint with a small fragment of the ribs, the focus can be exposed at a 270° angle under direct visualization of the outside of the dura mater without injuring the spinal cord3. Third, kyphotic deformities can easily be corrected as in vertebral column resection (VCR) osteotomy procedures following radical debridement and interbody fusion with a titanium mesh or autogenous bone grafting19. Fourth, the trauma and risk associated with this approach are minimal because opening of the chest is not required, and the surgical field is far from the mediastinum and pleural cavity. However, the posterolateral approach should not be applied for patients with paravertebral abscess that are too broad clear up posteriorly20. Anterior radical debridement and strut grafting with posterior instrumentation in a single‐stage or two‐stage procedure is a better indication for patients with multiple‐level tuberculosis lesions (i.e. more than three vertebrae) that preclude the possibility of anterior instrumentation, patients with initial anterior instrumentation failure, and those with kyphosis exceeding 30°21, 22, 23, 24. The combined procedure is a well‐documented technique that has been proven to provide good reconstruction stability with the support of the complete posterior column, although this procedure is associated with prolonged operating times, greater blood loss, more operation related complications, and longer hospital stays22, 23, 24, 25.
No reports have compared the use of anterior and posterior instrumentation in the treatment of multi‐level contiguous thoracic spinal tuberculosis in terms of the differences in surgical trauma, fusion level, fusion time for the bone graft, kyphosis correction, recurrence, and internal fixation‐related complications (e.g. correction loss, instrumentation failure, and sinus formation)26. The fusion level in the posterior instrumentation group was greater than that in the anterior instrumentation group due to the biomechanical characteristics of the two instrumentation modalities. The results of our study revealed that the symptoms of tuberculosis in the patients disappeared within 1–3 weeks postoperatively regardless of the use of anterior or posterior instrumentation, and the mean ESR and CRP values returned to normal within 8–12 weeks postoperatively in both groups. There were no significant differences in the fusion times of the bone grafts, neurological improvements, or recurrence. The neurologic statuses of the 23 patients with preoperative neurologic deficits improved in both groups (Table 2).
However, our study confirms that posterior instrumentation is superior to anterior instrumentation in the correction and maintenance of the correction in the treatment of thoracic spinal tuberculosis (Table 2). The probable reason for these findings is that with the posterior instrumentation, the pedicle screws cross the pedicle of the vertebral arch, which is the strongest part of the vertebral body, and, thus, provide 3‐D correction and strengthening of spinal three‐column stability to a much greater extent than the anterior instrumentation. Moreover, the anterior instrumentation consists of four screws that are fixed in the vertebral body and used only in residual cephalic and caudal vertebrae, which might also exhibit osteoporosis caused by spinal tuberculosis and, thus, cannot provide the same strength as pedicle screws. Zhang et al. report on a series of 23 cases with thoracic spinal tuberculosis in which anterior decompression, strut autografting, posterior instrumentation, and fusion were used, and observed a kyphosis correction of 24° and a 4° correction loss15. Conversely, Li et al. reported on a series of 42 cases in which anterior instrumentation was used and observed a mean kyphosis correction of 16.1° and a 0.9° correction loss5. The difference between our study and those of Zhang et al. and Li et al. may be that the conditions of our patients was more serious than theirs; the small numbers of patients employed in their studies might be an additional relevant difference.
In contrast, our study also revealed shortcomings of the use of posterior instrumentation. First, postoperative sinus formation is more likely to occur in patients who have undergone posterior debridement, bone grafting, and instrumentation because the lesion can connect with the posterior incision with this approach. Second, the average operation time, blood loss, and postoperative VAS scores were significantly higher in the posterior instrumentation group (Table 2). Furthermore, we found that the combined anterior–posterior approach induced greater surgical trauma than the posterolateral approach in the posterior instrumentation group.
In conclusion, our study suggests that both anterior and posterior instrumentation can achieve good results provided that the operative indications are accurately identified. Patients with paresis or paraplegia often exhibit satisfactory recovery after only 1 or 2 months of preoperative treatment for concurrent diseases, such as tuberculous pleuritis and tuberculous meningitis. However, the use of posterior instrumentation is superior to the use of anterior instrumentation in terms of correcting deformities and maintaining those corrections.
Acknowledgment
Appreciation is extended to Dr Chao‐xi Zhou and Dr Su‐xi Gu for collection of data.
Disclosure: This study was supported by Capital Characteristic Clinic Project Z141107002514055.
References
- 1. World Health Organization . Global tuberculosis report 2015. Geneva: WHO, 2015; 2–8. [Google Scholar]
- 2. Lee SH, Sung JK, Park YM. Single‐stage transpedicular decompression and posterior instrumentation in treatment treatment of thoracic and thoracolumbar spinal tuberculosis a retrospective case series. J Spinal Disord Tech, 2006, 19: 595–602. [DOI] [PubMed] [Google Scholar]
- 3. Zhang H, Huang S, Guo H, et al. A clinical study of internal fixation, debridement and interbody thoracic fusion to treat thoracic tuberculosis via posterior approach only. Int Orthop, 2012, 36: 293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Li L, Xu J, Ma Y, et al. Surgical strategy and management outcomes for adjacent multisegmental spinal tuberculosis. Spine (Phila Pa 1976), 2014, 39: E40–E48. [DOI] [PubMed] [Google Scholar]
- 5. Li M, Du J, Meng H, Wang Z, Luo Z. One‐stage surgical management for thoracic tuberculosis by anterior debridement, decompression and autogenous rib grafts, and instrumentation. Spine J, 2011, 11: 726–733. [DOI] [PubMed] [Google Scholar]
- 6. Wang Z, Ge Z, Jin W, et al. Treatment of spinal tuberculosis with ultrashort‐course chemotherapy in conjunction with partial excision of pathologic vertebrae. Spine J, 2007, 7: 671–681. [DOI] [PubMed] [Google Scholar]
- 7. Rajasekaran S, Shanmugasundaram TK. Prediction of the angle of gibbus deformity in tuberculosis of the spine. J Bone Joint Surg Am, 1987, 69: 503–509. [PubMed] [Google Scholar]
- 8. Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in the spinal tuberculosis: clinical and biologic study. Spine (Phila Pa 1976), 1993, 18: 1890–1894. [DOI] [PubMed] [Google Scholar]
- 9. Chen YC, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. One‐stage posterior surgery for treatment of advanced spinal tuberculosis. J Chin Med Assoc, 2003, 66: 411–417. [PubMed] [Google Scholar]
- 10. Liu P, Sun M, Li S, Wang Z, Ding G. A retrospective controlled study of three different operative approaches for the treatment of thoracic and lumbar spinal tuberculosis: three years of follow‐up. Clin Neurol Neurosurg, 2005, 128: 25–34. [DOI] [PubMed] [Google Scholar]
- 11. Zhang HQ, Hu X, Yin X, Chen Y. One‐stage combined anterior–posterior approach treatment of multiple cervicothoracic spinal tuberculosis with kyphosis. Int Orthop, 2015, 39: 1605–1610. [DOI] [PubMed] [Google Scholar]
- 12. Zeng H, Shen X, Luo C, et al. Comparison of three surgical approaches for cervicothoracic spinal tuberculosis: a retrospective case–control study. J Orthop Surg Res, 2015, 10: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shen X, Huang X, Xiao S, et al. Surgical treatment of selected patients with multilevel contiguous thoracolumbar spinal tuberculosis by only posterior instrumentation without any bone fusion. Int J Clin Exp Med, 2015, 8: 18611–18619. [PMC free article] [PubMed] [Google Scholar]
- 14. Yin XH, Liu SH, Li JS, et al. The role of costotransverse radical debridement, fusion and postural drainage in the surgical treatment of multisegmental thoracic spinal tuberculosis: a minimum 5‐year follow‐up. Eur Spine J, 2016, 25: 1047–1055. [DOI] [PubMed] [Google Scholar]
- 15. Zhang HQ, Guo CF, Xiao XG, Long WR, Deng ZS, Chen J. One‐stage surgical management for multilevel tuberculous spondylitis of the upper thoracic region by anterior decompression, strut autografting, posterior instrumentation, and fusion. J Spinal Disord Tech, 2007, 20: 263–267. [DOI] [PubMed] [Google Scholar]
- 16. Benli IT, Kaya A, Acaroğlu E. Anterior instrumentation in tuberculous spondylitis: Is it effective and safe. Clin Orthop Relat Res, 2007, 460: 108–116. [DOI] [PubMed] [Google Scholar]
- 17. Cavuşoğlu H, Kaya RA, Türkmenoğlu ON, Tuncer C, Colak I, Aydin Y. A long‐term follow‐up study of anterior tibial allografting and instrumentation in the management of thoracolumbar tuberculous spondylitis. J Neurosurg Spine, 2008, 8: 30–38. [DOI] [PubMed] [Google Scholar]
- 18. Wu P, Luo C, Pang X, Xu Z, Zeng H, Wang X. Surgical treatment of thoracic spinal tuberculosis with adjacent segments lesion via one‐stage transpedicular debridement, posterior instrumentation and combined interbody and posterior fusion, a clinical study. Arch Orthop Trauma Surg, 2013, 133: 1341–1350. [DOI] [PubMed] [Google Scholar]
- 19. Ozturk C, Alanay A, Ganiyusufoglu K, Karadereler S, Ulusoy L, Hamzaoglu A. Short‐term X‐ray results of posterior vertebral column resection in severe congenital kyphosis, scoliosis, and kyphoscoliosis. Spine (Phila Pa 1976), 2012, 37: 1054–1057. [DOI] [PubMed] [Google Scholar]
- 20. Zhang H, Sheng B, Tang M, et al. One‐stage surgical treatment for upper thoracic spinal tuberculosis by internal fixation, debridement, and combined interbody and posterior fusion via posterior‐only approach. Eur Spine J, 2013, 22: 616–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wang XB, Li J, Lü GH, Wang B, Lu C, Kang YJ. Single‐stage posterior instrumentation and anterior debridement for active tuberculosis of the thoracic and lumbar spine with kyphotic deformity. Int Orthop, 2012, 36: 373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Klockner CK, Valencia R. Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976), 2003, 28: 1036–1042. [DOI] [PubMed] [Google Scholar]
- 23. Liu Z, Wang X, Xu Z, et al. Two approaches for treating upper thoracic spinal tuberculosis with neurological deficits in the elderly: a retrospective case–control study. Clin Neurol Neurosurg, 2016, 141: 111–116. [DOI] [PubMed] [Google Scholar]
- 24. Liu J, Wan L, Long X, Huang S, Dai M, Liu Z. Efficacy and safety of posterior versus combined posterior and anterior approach for the treatment of spinal tuberculosis: a meta‐analysis. World Neurosurg, 2015, 83: 1157–1165. [DOI] [PubMed] [Google Scholar]
- 25. Shi JD, Wang Q, Wang ZL. Primary issues in the selection of surgical procedures for thoracic and lumbar spinal tuberculosis. Orthop Surg, 2014, 6: 259–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang X, Pang X, Wu P, Luo C, Shen X. One‐stage anterior debridement, bone grafting and posterior instrumentation vs. single posterior debridement, bone grafting, and instrumentation for the treatment of thoracic and lumbar spinal tuberculosis. Eur Spine J, 2014, 23: 830–837. [DOI] [PMC free article] [PubMed] [Google Scholar]


