Abstract
The objective of this study was to evaluate differences in clinical and radiographic outcomes between short (<3 levels) and long (≥3 levels) fusions in the setting of degenerative lumbar scoliosis. A literature search was performed from six electronic databases. The key terms of “degenerative scoliosis” OR “lumbar scoliosis” AND “fusion” were combined and used as MeSH subheadings. From relevant studies identified, demographic data, complication rates, Oswestry Disability Index (ODI), and radiographic parameters were extracted and the data was pooled and analyzed. Long fusion was associated with comparable overall complication rates to short fusion (17% vs 14%, P = 0.20). There was a significant difference in the incidence of pulmonary complications when comparing short versus long fusion (0.42% vs 2.70%; P = 0.02). No significant difference was found in terms of motor, sensory complications, infections, construct‐related or cardiac complications, pseudoarthrosis, dural tears, cerebrospinal fluid (CSF) leak, or urinary retention. A longer fusion was associated with a greater reduction in coronal Cobb angle and increases in lumbar lordosis, but both findings failed to achieve statistical significance. The ODI was comparable across both cohorts. If shorter fusion lengths are clinically indicated, they should be used instead of longer fusion lengths to reduce perioperative time, costs, and some other complications. However, there are no statistically significant differences in terms of radiographically measurable restoration associated with a short or long fusion.
Keywords: Proximal junctional kyphosis, Sacropelvic fixation, Spinal fusion, Spinal restoration
Introduction
Degenerative lumbar scoliosis (DLS) represents a spectrum of disabling curves that in the presence of sagittal imbalance is correlated with health‐related quality of outcome scores1. DLS is most common in the elderly and, thus, with the aging population, the incidence of both DLS and spine operations continue to rise1. Patients with DLS experience a spectrum of neurological symptoms, including lower back pain, leg pain, neuro‐claudication, radiculopathy, and generalized imbalance2. The symptoms themselves are secondary to degenerative manifestations to all aspects of the spinal apparatus, including facet joint arthrosis, spinal stenosis, disc degeneration, and gross vertebral disposition3, 4. In the setting of DLS, there is typically a combination of lateral displacement with some rotational dislocation of the vertebrae5.
There is a high degree of surgical complexity in the elderly patient population as they have a myriad of medical comorbidities. This caters to a high incidence of complications and, thus, the decision to operate can be difficult1. Surgical goals in DLS include decompression of the compromised neutral elements and a stable spine that is balanced in the coronal and sagittal planes6. Correction may involve a combination of decompression, fusion, and osteotomies to correct positive sagittal malalignment. At the time of decompression surgery, most surgeons also recommend fusion, which has been widely accepted to improve spinal alignment at the expense of mobility7, 8. However, there are no definitive and formalized recommendations for the number of levels fused or the best approach (anterior, posterior, lateral). There is also an overall lack of robust evidence evaluating general perioperative outcomes.
The purpose of our study is to evaluate the differences in clinical and radiographic outcomes between short and long fusions to assist in the decision‐making process for the surgical management of DLS.
Methods
Literature Search Strategy
The Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines were followed for the present systematic review. Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR) and Database of Abstracts of Review of Effectiveness (DARE) from their dates of inception to April 2015. The key terms of “degenerative scoliosis” OR “lumbar scoliosis” AND “fusion” were combined and used as MeSH subheadings where possible. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies, assessed using the inclusion and exclusion criteria defined below.
Selection Criteria
Eligible studies for the present systematic review and meta‐analysis were studies comprised of patient groups undergoing either a short and/or long segment fusion procedure for adult degenerative scoliosis. Based on previous definitions in published studies, a short fusion was defined as one with <3 segments involved or a mean number of segments fused <3, compared to a long fusion with ≥3 segments involved, or a mean number of segments ≥39, 10. Studies with fewer than 15 patients in a single cohort were excluded. If institutions published duplicate studies with accumulating numbers of patients or increased lengths of follow‐up, only the most complete reports were included for quantitative assessment. All publications were limited to those involving human subjects and in the English language. Abstracts, case reports, conference presentations, editorials, reviews, and expert opinions were excluded. No ethics approval was required for this study with all data obtained from a review of the literature.
Data Extraction and Critical Appraisal
Relevant data was extracted from article texts, tables, and figures. This included demographics, complication profiles, and radiological measurements (Tables 1, 2). Two investigators (K.P. and M.M.) independently reviewed each retrieved article. Extracted study characteristics included the following: study year, period, country, number of cases, and surgical technique (short or long fusion). Complications reported included motor, sensory, infectious, construct or hardware‐related, pulmonary, cardiac, pseudoarthrosis, dural tear, and urinary retention complications. Discrepancies between the two reviewers were resolved by discussion and consensus involving the senior authors. The quality of studies was assessed using criteria recommended by the National Health Service Centre for Reviews and Dissemination case series quality assessment criteria (University of York, Heslington, UK). Risk of bias assessment questions included: (i) clear definition of study population? (ii) clear definitions of outcomes and outcome assessment? (iii) no selective loss during follow‐up? and (iv) important confounders and prognostic factors identified? The senior investigators reviewed the final results.
Table 1.
Study characteristics of included studies on short fusion or long fusion for adult degenerative scoliosis
| First author | Year | Surgical technique group | Institution | Country | Study design | n (number of patients) | Mean age (years) | Males (%) | Operation duration (min) | Hospital stay (d) | Blood loss (mL) | Follow‐up average (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aoki | 2015 | Short Fusion | Chiba University | Japan | R, OS | 52 | 67.7 | 48.1 | NR | NR | NR | 16.4 |
| Yagi | 2014 | Short fusion | Hospital for Special Surgery | USA | R, OS | 33 | 56 | 3.0 | 438 | NR | 2100 | 63.6 |
| Sun | 2014 | Short Fusion | The Third Hospital of HeBei Medical University | China | R, OS | 20 | 68.7 | 70.0 | NR | NR | NR | NR |
| Rothenfluh | 2014 | Short fusion | Oxford University Hospital | United Kingdom | R, OS | 31 | 64.9 | 41.9 | NR | NR | NR | NR |
| Castro | 2014 | Short fusion | University of California | USA | R, OS | 35 | 68 | 25.7 | 137 | 1.4 | 54 | 24 |
| Lykissas | 2013 | Short Fusion | Weill Cornell Medical College | USA | R, OS | 30 | 67 | 20.0 | NR | NR | NR | 21 |
| Daubs | 2012 | Short fusion | University of California | USA | R, OS | 39 | 66 | NR | NR | NR | NR | 55.2 |
| Burneikiene | 2012 | Short fusion | Justin Parker Neurological Institute | USA | R, OS | 29 | 65.9 | 24.1 | 528 | 8 | 1091.7 | 30 |
| Liu | 2009 | Short fusion | Chengzheng Hospital | China | R, OS | 34 | 54.7 | 138.2 | 131 | NR | 809 | 68.4 |
| Hwang | 2009 | Short Fusion | Kyung Hee University | Korea | R, OS | 47 | 65.9 | 25.5 | NR | NR | NR | 3.4 |
| Cho | 2008 | Short fusion | Inha University Hospital | Korea | R, OS | 28 | 64.4 | NR | 179 | 18.4 | 1671 | 51.6 |
| Potter | 2005 | Short fusion | Walter Reed Army Medical Centre | USA | R, OS | 100 | 38 | 69.0 | NR | NR | NR | 34 |
| Yagi | 2015 | Long fusion | Hospital for Special Surgery | USA | R, OS | 57 | 53.7 | 5.3 | 432 | NR | 2034 | 57.6 |
| Yagi | 2014 | Long fusion | Hospital for Special Surgery | USA | R, OS | 33 | 57 | 6.1 | 504 | NR | 3600 | 55.2 |
| Sun | 2014 | Long fusion | The Third Hospital of HeBei Medical University | China | R, OS | 20 | 68.7 | 35.0 | 180 | NR | NR | NR |
| Di Silvestre | 2014 | Long fusion | Instiuti Ortopedici Rizzoli | Italy | R, OS | 25 | 67.6 | 80.0 | 240 | 9.5 | 1400 | 64 |
| Caputo | 2013 | Long fusion | Duke University Medical Centre | USA | R, OS | 30 | 65.9 | 36.7 | NR | NR | NR | 14.3 |
| Hioki | 2011 | Long Fusion | Gifu University Graduate School of Medicine | Japan | R, OS | 17 | 62 | 64.7 | 209 | NR | 489.3 | 44.1 |
| Liu | 2009 | Long fusion | Chengzheng Hospital | China | R, OS | 63 | 54.7 | 74.6 | 184 | NR | 1627 | 68.4 |
| Cho | 2008 | Long fusion | Inha University Hospital | Korea | R, OS | 22 | 66.9 | NR | 242 | 23.3 | 2819 | 51.6 |
| Cho | 2007 | Long fusion | Inha University Hospital | Korea | R, OS | 47 | 66.1 | 17.0 | 197.4 | 20.7 | 2106 | 45.6 |
| Hioki | 2005 | Long fusion | Gifu University Graduate School of Medicine | Japan | R, OS | 19 | 59.5 | 42.1 | 301.8 | NR | 1277 | 43.2 |
NR, no record.
Table 2.
Complications of short fusion and long fusion surgery for adult degenerative scoliosis
| First author | Motor deficit | Sensory deficit | Infection | Construct/hardware based | Pulmonary complication | Cardiac complication | Pseudoarthrosis | Dural tears/CSF leak | Urinary infection or retention |
|---|---|---|---|---|---|---|---|---|---|
| Aoki | 0 | 0 | 0 | 2 | 1 | 0 | 0 | 2 | 0 |
| Yagi | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 0 | 0 |
| Sun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rothenfluh | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 |
| Castro | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lykissas | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Daubs | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 0 |
| Burneikiene | 1 | 0 | 0 | 4 | 0 | 0 | 5 | 0 | 0 |
| Liu | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 6 | 0 |
| Hwang | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cho | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| Potter | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 6 | 0 |
| Yagi | 0 | 0 | 2 | 1 | 1 | 0 | 1 | 0 | 0 |
| Yagi | 0 | 1 | 2 | 1 | 1 | 0 | 1 | 0 | 0 |
| Sun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 |
| Di Silvestre | 1 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 1 |
| Caputo | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| Hioki | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Liu | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 6 | 0 |
| Cho | 0 | 0 | 1 | 3 | 3 | 0 | 1 | 0 | 0 |
| Cho | 0 | 1 | 2 | 1 | 1 | 0 | 2 | 0 | 1 |
| Hioki | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 2 | 0 |
| Total | 2 | 4 | 15 | 13 | 11 | 1 | 30 | 28 | 3 |
CSF, cerebrospinal fluid.
Statistical Analysis
Although it has limitations, a pooled analysis obviates eliminating studies not directly comparing the two approaches of interest (short fusion versus long fusion) and, thus, was used to increase the power of the comparison. Data from the individual studies were combined by cohort and compared. Statistical analyses of categorical variables were performed using χ2 and Fisher exact tests as appropriate. Meta‐regression of continuous variables based on short versus long fusion constructs were performed using t‐tests as appropriate. Because there were significant differences between cohorts, analysis of heterogeneity was not performed. P‐values ≤0.05 were considered statistically significant.
Results
Search Strategy and Study Characteristics
A total of 438 references were recovered from the primary search strategy, with 18 remaining following application of screening and eligibility criteria5, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26. This included 6 studies evaluating long fusion and 8 evaluating short fusion, with the remaining 4 studies containing dual cohorts and being comparative in nature5, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26. A total of 811 patients, subdivided into short fusion (n = 478) and long fusion (n = 333) cohorts, were analyzed from the selected studies. Table 1 summarizes the demographics of the individual cohorts including the perioperative outcomes (Fig. 1).
Figure 1.
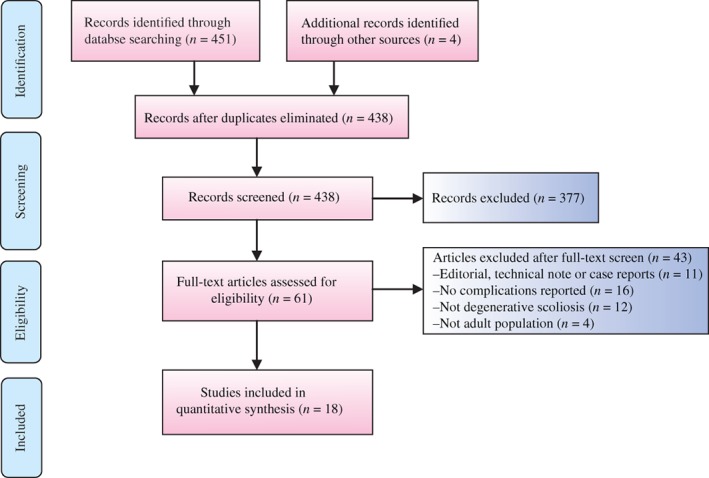
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) chart for systematic review strategy comparing short fusion versus long fusion for adult degenerative scoliosis.
Risk of Bias Assessment
Risk of bias assessment of included studies is summarized in Table 3. All studies had clear a definition of the study population, and clear definitions of outcomes and the outcome assessment. All studies except one had no selective loss during follow‐up. Seven studies reported important confounders and prognostic factors.
Table 3.
Risk of bias assessment of the studies included in the present systematic review and meta‐analysis
| First author | Year | Clear definition of study population? | Clear definition of outcomes and outcome assessment? | No selective loss during follow‐up? | Important confounders and prognostic factors identified? |
|---|---|---|---|---|---|
| Aoki | 2015 | Yes | Yes | Yes | Unclear |
| Yagi | 2014 | Yes | Yes | Yes | Yes |
| Sun | 2014 | Yes | Yes | Yes | No |
| Rothenfluh | 2014 | Yes | Yes | Yes | Yes |
| Castro | 2014 | Yes | Yes | Unclear | Yes |
| Lykissas | 2013 | Yes | Yes | Yes | Yes |
| Daubs | 2012 | Yes | Yes | Yes | No |
| Burneikiene | 2012 | Yes | Yes | Yes | No |
| Liu | 2009 | Yes | Yes | Yes | Unclear |
| Hwang | 2009 | Yes | Yes | Yes | No |
| Cho | 2008 | Yes | Yes | Yes | Yes |
| Potter | 2005 | Yes | Yes | Yes | No |
| Yagi | 2015 | Yes | Yes | Yes | Yes |
| Di Silvestre | 2014 | Yes | Yes | Yes | Unclear |
| Caputo | 2013 | Yes | Yes | Yes | No |
| Hioki | 2011 | Yes | Yes | Yes | No |
| Cho | 2007 | Yes | Yes | Yes | Yes |
| Hioki | 2005 | Yes | Yes | Yes | No |
Outcomes and Complications
Long fusion was associated with comparable overall complication rates to short fusion (17% vs 14%; P = 0.20). There was a statistically significant difference in the incidence of pulmonary complications when comparing short versus long fusion (0.42% vs 2.70%; P = 0.02). No significant difference was found in terms of motor, sensory complications, infections, construct‐related or cardiac complications, pseudoarthrosis, dural tears or CSF leak, or urinary retention. Nevertheless, the short fusion group demonstrated a trend towards lower incidence rate across all measured events except construct failure (5.00% vs 2.10%, P = 0.10; Fig. 2, Table 4).
Figure 2.
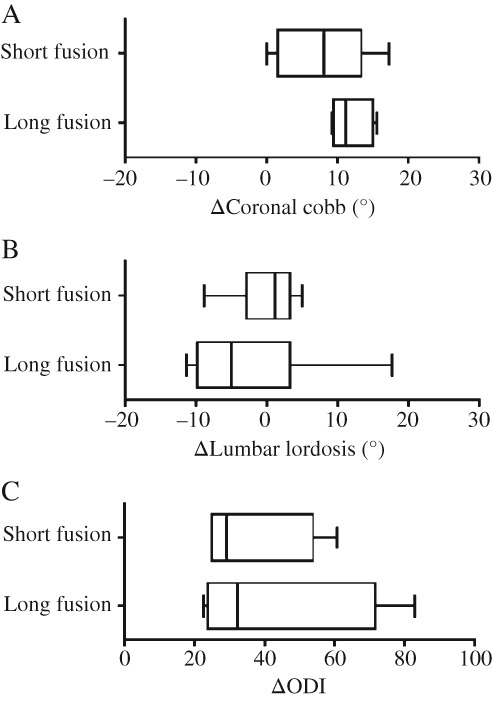
Summary whisker plot of changes in coronal Cobb (A), lumbar lordosis (B), and Oswestry Disability Index scores (C) following short versus long fusion for adult degenerative scoliosis. No significant differences were noted between short fusion and long fusion subgroups for these outcomes.
Table 4.
Summary of differences in complication rates between short fusion versus long fusion subgroups for adult degenerative scoliosis
| Complication | Short fusion | Long fusion | P‐value for difference | ||
|---|---|---|---|---|---|
| n/N | % | n/N | % | ||
| Motor | 1/478 | 0.21 | 1/333 | 0.30 | 0.97 |
| Sensory | 0/478 | 0.00 | 4/333 | 1.20 | 0.06 |
| Infectious | 7/478 | 1.46 | 8/333 | 2.40 | 0.62 |
| Construct | 24/478 | 5.02 | 7/333 | 2.10 | 0.10 |
| Pulmonary | 2/478 | 0.42 | 9/333 | 2.70 | 0.02 |
| Cardiac | 0/478 | 0.00 | 1/333 | 0.30 | 0.49 |
| Pseudoarthrosis | 16/478 | 3.35 | 14/333 | 4.20 | 0.57 |
| Dural tears or CSF leak | 16/478 | 3.35 | 12/333 | 3.60 | 0.84 |
| Urinary retention | 1/478 | 0.21 | 2/333 | 0.60 | 0.57 |
| Total complications | 67/478 | 14.02 | 58/333 | 17.42 | 0.20 |
CSF, cerebrospinal fluid.
Radiological Outcomes
A longer fusion was associated with a greater reduction in coronal Cobb angle and increases in lumbar lordosis, but both findings failed to achieve statistical significance. The ODI was comparable across both cohorts. The coronal Cobb and lumbar lordosis angles are summarized in Table 5.
Table 5.
Summary of coronal Cobb angle and lumbar lordosis angles preoperatively, postoperatively and change
| First author | Preop CC | Postop CC | Change CC | Preop LL | Postop LL | Change LL |
|---|---|---|---|---|---|---|
| Aoki | NR | NR | NR | 43.1 | 44 | −0.9 |
| Yagi | NR | NR | NR | 45 | 43 | 2 |
| Sun | NR | NR | NR | NR | NR | NR |
| Rothenfluh | NR | NR | NR | NR | NR | NR |
| Castro | 21.3 | 11.5 | 9.8 | 32.6 | 41.46 | −8.86 |
| Lykissas | 27 | 15 | 12 | −45 | −50 | 5 |
| Daubs | 22 | 22 | 0 | NR | NR | NR |
| Burneikiene | 32.3 | 15 | 17.3 | 37.6 | 40.5 | −2.9 |
| Liu | 17.6 | 15.5 | 2.1 | 30.6 | 27.3 | 3.3 |
| Hwang | NR | NR | NR | NR | NR | NR |
| Cho | 16.3 | 10.1 | 6.2 | 32.7 | 31.6 | 1.1 |
| Potter | NR | NR | NR | NR | NR | NR |
| Yagi | NR | NR | NR | −43.7 | −38.3 | −5.4 |
| Yagi | NR | NR | NR | 40 | 51 | −11 |
| Sun | NR | NR | NR | NR | NR | NR |
| Di Silvestre | 19.2 | 8.1 | 11.1 | −28.8 | −46.5 | 17.7 |
| Caputo | 20.2 | 5.8 | 14.4 | NR | NR | NR |
| Hioki | NR | NR | NR | 23.4 | 28.1 | −4.7 |
| Liu | 24.3 | 14.6 | 9.7 | 21.7 | 28.2 | −6.5 |
| Cho | 21.7 | 6.1 | 15.6 | 25.7 | 22.1 | 3.6 |
| Cho | 18.6 | 9.42 | 9.18 | 30.7 | 28.4 | 2.3 |
| Hioki | NR | NR | NR | 25.2 | 36.6 | −11.4 |
CC, coronal Cobb angle; LL, lumbar lordosis angle; NR, No record.
Discussion
With the aging population, the prevalence of both DLS and spine surgery continues to increase1. Although there is a clear role for conservative therapy as a means of minimizing morbidity, surgical intervention is sometimes necessary for the treatment of DLS5. While decompression alone is a surgical procedure that can reduce symptoms of claudication, it is not ideal when performed in isolation as it can lead to further spine instability and collapse at the degenerative curve8, 27. Thus, most surgeons recommend that decompression be performed in conjunction with fusion and instrumentation7, 8. Generally, decompression and short fusion is performed when there is minimal laterolisthesis or the Cobb angle is small28. In contrast, longer fusions are recommended in patients with a greater Cobb angle and larger sagittal and coronal imbalance5.
The results of our study indicate that both short and long fusion can successfully contribute to restoration of sagittal imbalances as observed through reductions in coronal Cobb angle and restoration of lumbar lordosis. We did not find a statistically significant difference between the two groups in terms of magnitude of correction. This is not surprising as this is in part a reflection that most surgeons aim to restore appropriate balance, and would not undertake the procedure unless it allowed this to be achieved or approximated. Furthermore, the current literature does not allow for the evaluation of other balance parameters such as the sagittal vertical axis as well as pelvic parameters. Follow‐up data from multiple studies supports that the level of radiologically measurable restoration is maintained29. As such, while we are able to conclude that surgical fusion is an effective intervention in the setting of DLS, we are unable to make further recommendations on the number of levels fused on the basis of objective radiographic changes alone. However, fusion in combination with decompression has been demonstrated to provide greater alleviation of DLS symptoms in comparison to decompression alone. As noted by Castro et al. and Oliveira et al. decompression alone may not be sufficient in alleviating symptoms in patients with significant facet joint arthrosis due to a lack of direct impact on the neuroforamen itself14, 30. There is also evidence that posterior fusion may be ineffective in restoring sagittal balance and, thus, supplementary osteotomy or some type of lumbar interbody fusion should be considered for patients where sagittal balance is a concern15.
The extent of spinal fusion is a very important factor that must be determined prior to surgery. Simmons and Simmons suggest that the spinal fusion should incorporate the level of rotatory subluxation so that it is not aggravated following surgery31. It is recommended that the most horizontal vertebra is chosen for the upper instrumented vertebrae as this can assist with the balance of the spine31. Along with that, fusion should not end on a vertebral level with kyphosis or spondylolisthesis31. The fusion levels and length must also be carefully chosen so that it is not confined to the region of deformed spine as this can result in disease between the adjacent vertebrae5. In particular, the decision to extend a fusion to the sacrum/pelvis is a subject of controversy as shorter fusions up to L5 can lead to adjacent segment disease at L5–S1 due to a larger lever arm from the higher instrumented levels as well as loss of distal fixation5, 32. However, sacropelvic fixation affords more rigid fixation at the bottom of a long construct5, 32. In addition, patients with significant coronal or sagittal plane deformities where ending the distal construct at L5 would result in residual coronal tilt or sagittal kyphosis may warrant extension of fusion to the sacrum and pelvis16. Extension of fusion past L5 may be warranted in the setting of certain pedicle subtraction osteotomy procedures to further stabilize the spine5, 32. Therefore, the decision to perform short or long fusion remains individualized to each patient, and depends on a multitude of factors as discussed. The current study results suggest that either approach can achieve sufficient correction if performed appropriately. Thus, the surgeon must balance the advantages and disadvantages of each fusion procedure when deciding which surgical procedure is most suitable for a patient.
Although long fusion did have higher complication rates in all domains except for construct and instrumentation‐related complications, which made up almost one‐third of adverse events in the short fusion group, these differences did not reach statistical significance. These construct and instrumentation‐related complications may be related to proximal junctional kyphosis (PJK)33, 34. There is evidence that shorter fusion lengths that stop proximally at T8 or lower can increase the risk of PJK35. However, the association between PJK and fusion length has not been fully elucidated as longer fusion lengths that include the sacrum have been shown to also greatly increase the risk of PJK33. We speculate the magnitude of the secondary immobility associated with a longer fusion apparatus to be facilitative in reducing construct failure. Long segment fusion is also associated with lengthier operation times and blood loss, which may increase the incidence of morbidity and complications36. The incidence of reoperation and adjacent segment disease were omitted in our study due to a lack of reporting standardization and may have resulted in an underestimation of the true complication rates. There also remains controversy surrounding the upper instrumented vertebra stopping points in the context of long fusions, which varies from study to study and could not be accounted for in the present analysis. Although short fusion was found to be associated with a lower incidence of pulmonary complications compared to long fusion (0.42% vs 2.70%; P = 0.02), in this study, whether there is a unique predisposition for this in long fusions is uncertain but may be related to longer intubation and delayed mobilization after surgery. More specific diagnoses in the reporting of pulmonary complications in future studies may shed more light on this finding. The greater age of the DLS population is naturally associated with a high prevalence of medical comorbidities, which confer increased surgical complication rates1, 5. In these clinical scenarios, a surgeon would be predisposed to choose less invasive procedures if feasible, and we were unable to control for this confounding factor given the existing literature included in this study.
There are some limitations to the present findings. First, the approach in both groups (anterior, posterior, lateral) was not isolated in order to maintain a meaningful cohort volume for analysis. Approach‐specific complications should also be assessed in future studies37, 38. With greater patient numbers, future studies would ideally subgroup patients based on surgical approach as it has been shown to have a significant impact on cage positioning within the intervertebral space, which will affect alignment and alterations of lordosis7. Combined anterior/posterior approaches have also been shown to have a higher risk of PJK and, thus, may affect the complication rates in the current study. In addition, we were unable to stratify our study cohorts into minimally‐invasive and non‐minimally invasive procedures given the lack of specification from the selected studies. It is known that these two techniques have differing complication profiles and, as such, future studies should clearly define this in the procedure conducted. Other contributors to the large heterogeneity across the selected studies include the fusion length being independently dictated by different surgeons and varying degrees of DLS severity in the patients, which, in turn, may be affected by differing practices, surgeon expertise, and training. In addition, meaningful comments on the parameters of operative time, blood loss, and post‐operative hospital stay cannot be made with confidence given the differences in definitions and recording across the studies. Finally, there is a distinct lack in the quality of evidence with studies limited to retrospective and observational methods in design39. Despite this, our study provides rigid definitions of the various outcomes, which has led to the inclusion of fewer studies at a higher level of methodology quality.
Conclusion
Spine surgery involving decompression and fusion is safe and recommended in the setting of DLS treatment. Operations on spine deformity are complex and require a lot of thought when determining fusion levels. This study found no statistically significant differences in terms of coronal Cobb angle and lumbar lordosis correction associated with a short or long fusion. This study indicates that if shorter fusion lengths are clinically indicated, they should be used instead of longer fusion lengths to reduce perioperative time and costs along with some complications. Nevertheless, prospective randomized trials with substantial patient numbers and a wider range of standardized preoperative parameters and outcome measures must be conducted to further the suggested findings of this study.
Disclosure: There were no conflicts of interest related to this manuscript, and no funding was received for this work.
References
- 1. Pritchett JW, Bortel DT. Degenerative symptomatic lumbar scoliosis. Spine (Phila Pa 1976), 1993, 18: 700–703. [DOI] [PubMed] [Google Scholar]
- 2. Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine (Phila Pa 1976), 1994, 19: 1619–1627. [DOI] [PubMed] [Google Scholar]
- 3. Marchesi DG, Aebi M. Pedicle fixation devices in the treatment of adult lumbar scoliosis. Spine (Phila Pa 1976), 1992, 17: S304–S309. [DOI] [PubMed] [Google Scholar]
- 4. Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976), 2002, 27: 387–392. [DOI] [PubMed] [Google Scholar]
- 5. Cho KJ, Suk SI, Park SR, et al Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J, 2008, 17: 650–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen PG, Daubs MD, Berven S, et al Surgery for degenerative lumbar scoliosis: the development of appropriateness criteria. Spine (Phila Pa 1976), 2016, 41: 910–918. [DOI] [PubMed] [Google Scholar]
- 7. Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop (Belle Mead NJ), 2003, 32: 77–82. [PubMed] [Google Scholar]
- 8. Vaccaro AR, Ball ST. Indications for instrumentation in degenerative lumbar spinal disorders. Orthopedics, 2000, 23: 260–271. [DOI] [PubMed] [Google Scholar]
- 9. Wang G, Hu J, Liu X, Cao Y. Surgical treatments for degenerative lumbar scoliosis: a meta analysis. Eur Spine J, 2015, 24: 1792–1799. [DOI] [PubMed] [Google Scholar]
- 10. Liu W, Chen XS, Jia LS, Song DW. The clinical features and surgical treatment of degenerative lumbar scoliosis: a review of 112 patients. Orthop Surg, 2009, 1: 176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Aoki Y, Nakajima A, Takahashi H, et al Influence of pelvic incidence‐lumbar lordosis mismatch on surgical outcomes of short‐segment transforaminal lumbar interbody fusion. BMC Musculoskelet Disord, 2015, 16: 213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burneikiene S, Nelson EL, Mason A, Rajpal S, Serxner B, Villavicencio AT. Complications in patients undergoing combined transforaminal lumbar interbody fusion and posterior instrumentation with deformity correction for degenerative scoliosis and spinal stenosis. Surg Neurol Int, 2012, 3: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Caputo AM, Michael KW, Chapman TM, et al Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. J Clin Neurosci, 2013, 20: 1558–1563. [DOI] [PubMed] [Google Scholar]
- 14. Castro C, Oliveira L, Amaral R, Marchi L, Pimenta L. Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis?. Clin Orthop Relat Res, 2014, 472: 1776–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cho KJ, Suk SI, Park SR, et al Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976), 2007, 32: 2232–2237. [DOI] [PubMed] [Google Scholar]
- 16. Daubs MD, Lenke LG, Bridwell KH, Cheh G, Kim YJ, Stobbs G. Decompression alone versus decompression with limited fusion for treatment of degenerative lumbar scoliosis in the elderly patient. Evid Based Spine Care J, 2012, 3: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Di Silvestre M, Lolli F, Bakaloudis G. Degenerative lumbar scoliosis in elderly patients: dynamic stabilization without fusion versus posterior instrumented fusion. Spine J, 2014, 14: 1–10. [DOI] [PubMed] [Google Scholar]
- 18. Hioki A, Miyamoto K, Hosoe H, Sugiyama S, Suzuki N, Shimizu K. Cantilever transforaminal lumbar interbody fusion for upper lumbar degenerative diseases (minimum 2 years follow up). Yonsei Med J, 2011, 52: 314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hioki A, Miyamoto K, Kodama H, et al Two‐level posterior lumbar interbody fusion for degenerative disc disease: improved clinical outcome with restoration of lumbar lordosis. Spine J, 2005, 5: 600–607. [DOI] [PubMed] [Google Scholar]
- 20. Hwang DW, Jeon SH, Kim JW, Kim EH, Lee JH, Park KJ. Radiographic progression of degenerative lumbar scoliosis after short segment decompression and fusion. Asian Spine J, 2009, 3: 58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lykissas MG, Cho W, Aichmair A, et al Is there any relation between the amount of curve correction and postoperative neurological deficit or pain in patients undergoing stand‐alone lateral lumbar interbody fusion?. Spine (Phila Pa 1976), 2013, 38: 1656–1662. [DOI] [PubMed] [Google Scholar]
- 22. Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW Jr, Kuklo TR. Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech, 2005, 18: 337–346. [DOI] [PubMed] [Google Scholar]
- 23. Rothenfluh DA, Koenig M, Stokes OM, Behrbalk E, Boszczyk BM. Access‐related complications in anterior lumbar surgery in patients over 60 years of age. Eur Spine J, 2014, 23 (Suppl 1): S86–S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sun Y, Shen Y, Ding W, et al Comparison in clinical outcome of two surgical treatments in degenerative scoliosis. Cell Biochem Biophys, 2014, 70: 189–193. [DOI] [PubMed] [Google Scholar]
- 25. Yagi M, Patel R, Boachie‐Adjei O. Complications and unfavorable clinical outcomes in obese and overweight patients treated for adult lumbar or thoracolumbar scoliosis with combined anterior/posterior surgery. J Spinal Disord Tech, 2015, 28: E368–E376. [DOI] [PubMed] [Google Scholar]
- 26. Yagi M, Patel R, Lawhorne TW, Cunningham ME, Boachie‐Adjei O. Adult thoracolumbar and lumbar scoliosis treated with long vertebral fusion to the sacropelvis: a comparison between new hybrid selective spinal fusion versus anterior‐posterior spinal instrumentation. Spine J, 2014, 14: 637–645. [DOI] [PubMed] [Google Scholar]
- 27. Aebi M. The adult scoliosis. Eur Spine J, 2005, 14: 925–948. [DOI] [PubMed] [Google Scholar]
- 28. Tribus CB. Degenerative lumbar scoliosis: evaluation and management. J Am Acad Orthop Surg, 2003, 11: 174–183. [DOI] [PubMed] [Google Scholar]
- 29. Caputo AM, Michael KW, Chapman TM, et al Clinical outcomes of extreme lateral interbody fusion in the treatment of adult degenerative scoliosis. ScientificWorldJournal, 2012, 2012: 680643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976), 2010, 35: S331–S337. [DOI] [PubMed] [Google Scholar]
- 31. Simmons ED Jr, Simmons EH. Spinal stenosis with scoliosis. Spine (Phila Pa 1976), 1992, 17: S117–S120. [DOI] [PubMed] [Google Scholar]
- 32. Bridwell KH, Edwards CC 2nd, Lenke LG. The pros and cons to saving the L5‐S1 motion segment in a long scoliosis fusion construct. Spine (Phila Pa 1976), 2003, 28: S234–S242. [DOI] [PubMed] [Google Scholar]
- 33. Cho SK, Shin JI, Kim YJ. Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J, 2014, 23: 2726–2736. [DOI] [PubMed] [Google Scholar]
- 34. Lau D, Clark AJ, Scheer JK, et al Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976), 2014, 39: 2093–2102. [DOI] [PubMed] [Google Scholar]
- 35. Bridwell KH, Sedgewick TA, O'Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord, 1993, 6: 461–472. [DOI] [PubMed] [Google Scholar]
- 36. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am, 2003, 85: 2089–2092. [DOI] [PubMed] [Google Scholar]
- 37. Phan K, Rao PJ, Scherman DB, Dandie G, Mobbs RJ. Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci, 2015, 22: 1714–1721. [DOI] [PubMed] [Google Scholar]
- 38. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI‐TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg, 2015, 1: 2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Phan K, Mobbs RJ. Systematic reviews and meta‐analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg, 2015, 1: 19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]


