Abstract
Anterior odontoid screw fixation has been proved to be effective but technically challenging because the difficult approach is associated with high risks of screw malposition and damage to surrounding vital structures. Navigation techniques are therefore increasingly being used to improve safety and accuracy. However, no robot‐assisted odontoid screw fixation has yet been reported. We here report a 61‐year‐old woman with a type II dens fracture on whom anterior odontoid screw fixation was performed under the guidance of a newly developed robotic system (TiRobot, co‐designed by Beijing Jishuitan Hospital and TINAVI Medical Technologies). One odontoid screw was safely and accurately placed, the calculated deviation between the planned and actual positions being 0.9 mm. No intraoperative complications were identified and the patient was discharged on Day 5. Follow‐up studies after 2 weeks showed good clinical and radiological results. We believe this is the first reported case of robot‐assisted anterior odontoid screw fixation. We consider that complicated procedures can become feasible, safe and accurate using TiRobot systems.
Keywords: Bone screws, Computer‐assisted surgery, Odontoid process, Robotic surgical procedures, Spinal fractures
Introduction
Anterior odontoid screw fixation can maintain the range of motion of the atlantoaxial joint. For that reason, it is now the surgical procedure of choice for type II odontoid fractures. However, this procedure can be technically challenging because of the difficult approach and complex morphology of the upper cervical vertebrae and surrounding vital structures. Surgeons performing this procedure are exposed to high irradiation doses yet have still failed to achieve satisfactory safety and accuracy. Navigation and robot techniques to address these difficulties are thus becoming more popular for upper cervical surgeries.
We recently designed a new robot system called TiRobot that is based on intraoperative three‐dimensional (3‐D) images (Fig. 1). TiRobot has three components: the planning and navigation system, optical tracking system and robotic arm system. A set of intraoperative images is initially acquired using a 3‐D C‐arm (Siemens Medical Solutions, Erlangen, Germany). The robotic arm is identified at the same time by detecting the plate locator on it. After that, the planning and navigation system can perform an automatic registration. Surgeons then plan the entry point and trajectory of the screw on the system and send these to guide the robotic arm.
Figure 1.
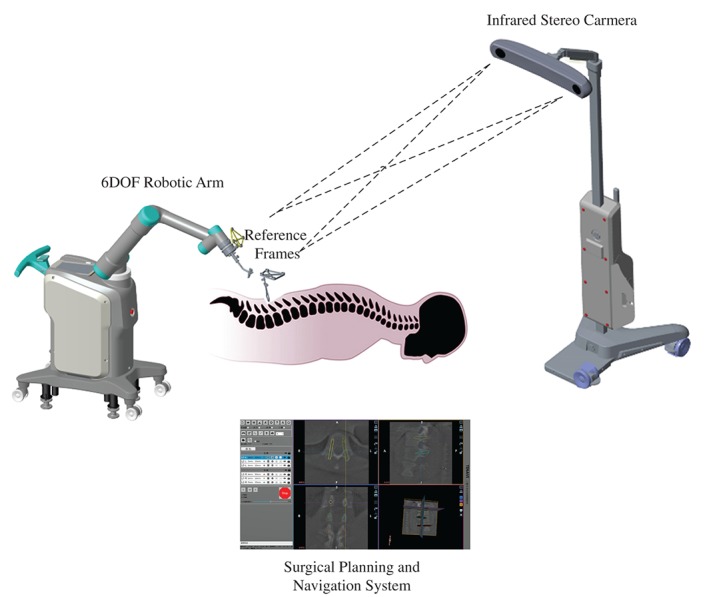
Diagram of the TiRobot system.
The optical tracking system is made up of an infrared stereo camera and two reference frames, one attached to the spinous process and the other to the robotic arm, thus enabling the optical tracking system to locate the position of the robotic arm relative to the patient and to guide the arm to the planned position. The robotic arm system is built on a mobile platform and has six degree of freedom. It has universal holders on which the reference frame, plate locator, guide holder and surgical instruments can be mounted. The robotic arm spontaneously moves accurately to the required position under the guidance of the planning and navigation and optical tracking systems.
By combining navigation and robot techniques, TiRobot can guide the screw trajectories for orthopedic surgeries. We believe this to be the first reported case of robot‐assisted anterior odontoid screw fixation.
Case Report
A 61‐year‐old woman presented to the accident and emergency department with upper neck pain after a fall at ground level. Physical examination showed tenderness in the upper cervical region and a decreased range of motion in all directions. There were no neurological deficits or relevant prior history.
Cervical CT scan demonstrated a type II fracture of the odontoid process with 2 mm anterior displacement of the upper part (Fig. 2).
Figure 2.
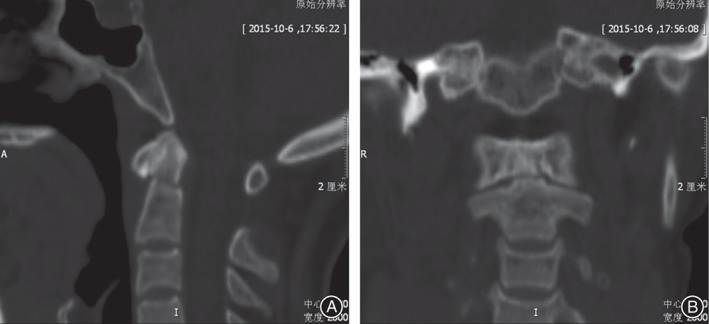
(A) Sagittal and (B) coronal CT images showing a type II odontoid fracture.
After receiving approval by the ethics committee of our institution and informed consent from the patient, surgical odontoid fracture reduction and robot‐assisted anterior screw fixation was planned.
The patient was placed in supine position after induction of general anesthesia. Mayfield tongs were placed to manipulate to achieve reduction while keeping the head in traction and slight extension. The patient tracker was then settled on the Mayfield tongs and 3‐D C‐arm scanning and robotic planning carried out using the TiRobot system. Virtual drill trajectories were planned on 3‐D software (Fig. 3).
Figure 3.
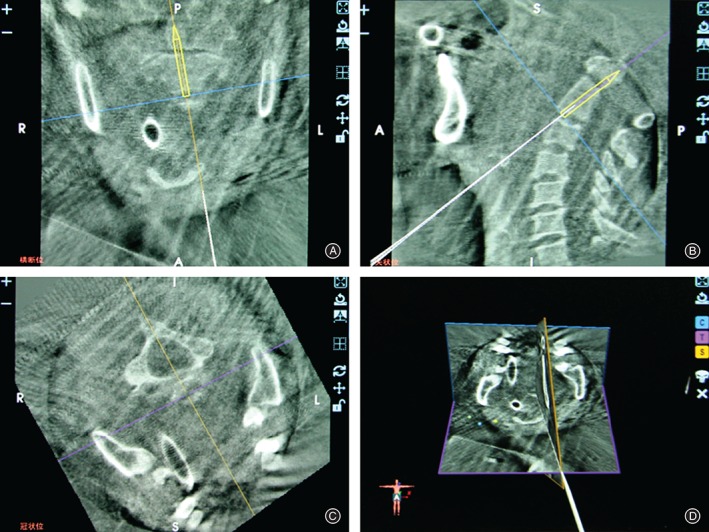
Graphical user interface of surgical planning in the TiRobot system. The surgeon can use intraoperative 3‐D images to determine the best screw trajectory.
The arm of the TiRobot then moved spontaneously to guide the planned trajectory. A left‐sided 2 cm skin incision was made under robotic guidance and exposure to the anterior inferior border of the axis achieved. A cannula was inserted through the sleeve of the robotic arm, after which a Kirschner wire was drilled into the odontoid process (Fig. 4). A 36 mm long, 4 mm diameter cannulated screw was then inserted under K‐wire guidance and the placement of the screw found to be satisfactory according to an intraoperative 3‐D C‐arm fluoroscopy scan. The calculated deviation between the planned and actual position was 0.9 mm and it took 50 min to insert the screw.
Figure 4.

A cannula is inserted through the robotic sleeve to reach the bone cortex, after which a K‐wire is placed through the cannula.
There were no intraoperative complications and the patient was discharged on Day 5 with full strength and sensation in her extremities. Postoperative CT images (Day 0, Fig. 5) showed no perforation or loosening of the screw. At her first clinical and radiological follow‐up 2 weeks after surgery the patient was pain‐free and examination showed she had good wound healing and full strength in her extremities. X‐ray films showed satisfactory reduction and position of the screw (Fig. 6). The cervical range of motion could not be ascertained because of the brace.
Figure 5.
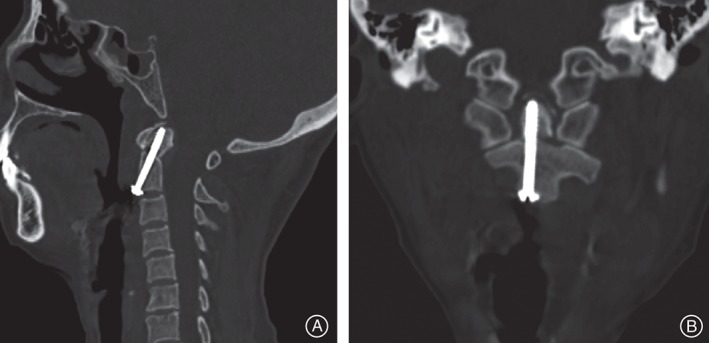
(A) Sagittal and (B) coronal postoperative CT images showing accurate placement of the screw.
Figure 6.
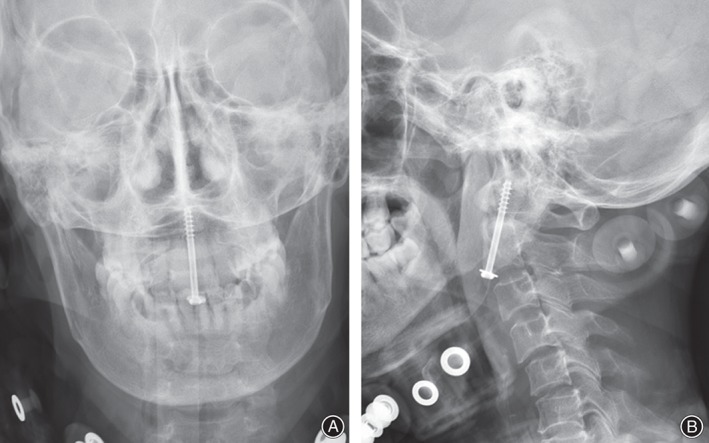
(A) Anteroposterior and (B) lateral X‐ray films 2 weeks after surgery showing good position of the screw.
Discussion
Odontoid fracture accounts for approximately 20% of all cervical spine injuries. According to the Anderson and D'Alonso classification, type II odontoid fracture, the commonest type, is unstable and vulnerable to nonunion1. Many treatment options including hard collars, halo‐vests and several surgical procedures, have been tried. Recent systemic reviews have found that operative treatment has better results2, 3. Anterior odontoid screw fixation, first described by Bohler in 1982, is considered the surgical procedure of choice because it can minimizes loss of cervical movement after fusion, especially rotational function. However, many major or minor complications have been reported, these being attributable to the limited visibility and complicated anatomy of upper cervical surgery, which can lead to high risks of screw malposition and damage to vital structures. For this reason, researchers have increasingly focused on devising a feasible, safe and minimally invasive approach.
Computer‐assisted navigation techniques have been widely used in recent years, including having been tried for anterior odontoid screw insertion4, 5; this has partially resolved the limitations on visualization of the surgical field. However, the limitation of difficulty in manipulation by the surgeon, which can also result in severe complications during upper cervical procedures, has promoted the development of robotic techniques. In 1985, Kwoh et al. designed the first neurosurgery robot arm based on PUMA200 (Westinghouse Automation, Pittsburgh, PA, USA)6. In 2003, Mazor (SpineAssist; Mazor Surgical Technologies, Caesarea, Israel) designed the first spine robot7.
Recently, our department designed the new surgical robot, called TiRobot, described herein (co‐designed by Beijing Jishuitan Hospital and TINAVI Medical Technologies [Beijing, China]). It was created for orthopedic surgery based on intraoperative C‐arm 3‐D images and combines navigation and robot techniques to enable accurate positioning, adequate steadiness and repeatability. Surgeons can use the system for intraoperative planning, after which the serial structured mechanical arm moves to guide the surgeon finding a proper entry point and trajectory as planned. The drilling and screw insertion are still performed manually by the surgeon.
This case report has some limitations. First, we have performed anterior odontoid screw fixation on only one patient. Clearly, more experience is required before drawing conclusions about the reliability of this new robot. Second, because the surgery was performed recently, further follow‐up is needed to assess union.
Disclosure: No conflict of interests relevant to this manuscript.
References
- 1. Heggeness MH, Doherty BJ. The trabecular anatomy of the axis. Spine (Phila Pa 1976), 1993, 18: 1945–1949. [DOI] [PubMed] [Google Scholar]
- 2. Schroeder GD, Kepler CK, Kurd MF, et al. A systematic review of the treatment of geriatric type II odontoid fractures. Neurosurgery, 2015, 77 (Suppl. 4): S6–S14. [DOI] [PubMed] [Google Scholar]
- 3. Robinson Y, Robinson AL, Olerud C. Systematic review on surgical and nonsurgical treatment of type II odontoid fractures in the elderly. Biomed Res Int, 2014, 2014: 231948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Battaglia TC, Tannoury T, Crowl AC, Chan DP, Anderson DG. A cadaveric study comparing standard fluoroscopy with fluoroscopy‐based computer navigation for screw fixation of the odontoid. J Surg Orthop Adv, 2005, 14: 175–180. [PubMed] [Google Scholar]
- 5. Chibbaro S, Benvenuti L, Carnesecchi S, Marsella M, Serino D, Gagliardi R. The use of virtual fluoroscopy in managing acute type II odontoid fracture with anterior single‐screw fixation. A safe, effective, elegant and fast form of treatment. Acta Neurochir, 2005, 147: 735–739, discussion 739. [DOI] [PubMed] [Google Scholar]
- 6. Kwoh YS, Hou J, Jonckheere EA, Hayati S. A robot with improved absolute positioning accuracy for CT guided stereotactic brain surgery. IEEE Trans Biomed Eng, 1988, 35: 153–160. [DOI] [PubMed] [Google Scholar]
- 7. Lieberman IH, Togawa D, Kayanja MM, et al. Bone‐mounted miniature robotic guidance for pedicle screw and translaminar facet screw placement: part I–technical development and a test case result. Neurosurgery, 2006, 59: 641–650, discussion 641–650. [DOI] [PubMed] [Google Scholar]


