Abstract
Objective
To compare clinical and radiographic outcomes of posterior malleolar fractures (PMF) treated with lag screws from anterior to posterior versus posterior to anterior approach.
Methods
We retrospectively analyzed 48 patients with trimalleolar fractures who underwent open reduction and internal fixation (ORIF) with either posteromedial (PM) or posterolateral (PL) approaches between January 2012 and December 2014. Fixation of the posterior malleolus was made with anteroposterior screws in 20 patients using the PM approach and posteroanterior screws in 28 patients using the PL approach. The American Orthopedic Foot and Ankle Society (AOFAS) scores and range of motion (ROM) of the ankle were used as the main outcome measurements, and results were evaluated at the 6‐month, 12‐month and final follow‐up. Postoperative radiographs and computed tomography scans were used to evaluate the residual gap/step‐off. The degree of arthritis was evaluated on final follow‐up using Bargon criteria. Other complications were also recorded to compare the clinical outcomes of the two approaches.
Result
The mean duration of follow‐up regardless of the approaches was 21.1 months (range, 15–54 months). None of the patients developed delayed union or nonunion. Functional bone healing was obtained in all patients at 10.7 weeks (range, 8–16 weeks). The mean AOFAS scores of the PM group at the postoperative 6‐mouth, 12‐month, and final follow‐up were 91.4 (range, 82–100), 92.5 (range, 84–100), and 92.9 (range, 86–100), respectively. In the PL group, the mean AOFAS scores were 89.9 (range, 72–100), 91.4 (range, 77–100), and 91.9 (range, 77–100), respectively. At the final follow‐up, the median loss of range of motion (ROM) for dorsiflexion and plantaflexion were 0°(0°, 5°) and 0°(0°, 0°), respectively, in both groups. There were no significant differences between the two approaches in AOFAS scores and ROM of the ankle in each period postoperatively (P > 0.05). Two patients in the PL group and 1 in the PM group developed Bargon grade 2 or 3 arthritis. We detected a 2‐mm and 3‐mm step‐off in 1 patient in the PM and PL groups, respectively.
Conclusion
Satisfactory results were obtained by using the two approaches for fixation of posterior malleolus, and the approaches have similar clinical and radiographic outcomes. Surgeons should choose the appropriate approach based on their experience.
Keywords: Posterior malleolar fractures, Posterolateral approach, Posteromedial approach, Trimalleolar fractures
Introduction
Ankle fractures are the fourth most common injuries treated by orthopedic surgeons, and have been reported to occur in 187 per 100,000 person‐years1, 2. The incidence rate of posterior malleolar involvement varies from 7 to 44% in all ankle fractures3, 4. Posterior malleolar fractures produced by purely rotational injuries occur as a result of undue traction exerted by the posterior–inferior tibiofibular ligament. The size of posterior malleolar fragments ranges from small extra‐articular fragments like shells to the ones involving more than 40% of the articular surface of the tibia. An anatomical reduction for an unstable ankle is necessary to achieve a successful functional outcome. Most surgeons consider that posterior malleolar fragments involving greater than 25%–30% of the distal tibial plafond surface should be fixed in order to achieve a stable ankle and a better outcome5, 6, 7, 8, 9. Recently, some studies have confirmed that posterior malleolus fractures involving over 25% of the articular surface will result in the increased incidence of post‐traumatic osteoarthritis (OA) and worse functional outcome10, 11. Biomechanical studies also suggest that fractures of 25% or smaller do not need to be fixed12. However, Langenhuijsen found that anatomic reduction of the posterior fragment with a congruent joint should be undertaken if 10% or more of the tibial articular surface is involved, if necessary with internal fixation13. The indications of the fixation of posterior malleolar fragments remain controversial.
Simple posterior malleolar fractures can be reduced in minimally invasive ways, such as percutaneous reduction with anteroposterior screw fixation14. However, these methods have some limitations. It is technically difficult to achieve satisfactory reduction using an image intensifier. In addition, with the small fragments, it is hard to achieve solid fixation and compression. It has been shown that the most effective technique is direct reduction and fixation from the posterior approach15. Multiple approaches for the open reduction and internal fixation (ORIF) of posterior malleolus have been described. In 1983, Shelton described a long medial incision to reach the posterior fragment with dislocation of the ankle, which required extensive soft tissue stripping. In 2000, Kao et al. described a “postero–medio–anterior” approach for pilon fractures using a large J‐type incision that starts posteriorly proximally and then curves around the medial malleolus and is distally located over the dorsomedial foot16. However, which approach is better for posterior malleolus fixation is unclear. Incision of the posterior aspect of the ankle is considered the most effective operative technique. The posterolateral (PL) approach has been reported on frequently in recent studies and has been demonstrated to be a useful approach for all patterns of posterior malleolar fractures17, 18, 19, 20, 21. It is convenient to simultaneously treat fractures of the posterior rim of the tibia and the distal fibula from a single incision. However, there are some disadvantages of the posteromedial (PM) approach with anteroposterior screw fixation of the posterior malleolus. The tibialis posterior nerve or artery may be injured by overstretching the soft tissues. In addition, anteroposterior screws may not provide enough interfragmentary compression when the threads of lag screws partially cross the fracture line. In clinical studies, the PM approach has also been reported to provide a good outcome for some particular patterns of posterior malleolar fractures22. Both the PM and PL approaches have advantages and disadvantages. However, there are few comparative studies of these two different approaches for posterior malleolus fixation.
The purpose of the present study is to compare clinical and radiographic outcomes of two techniques: posteroanterior screws through the PL approach and anteroposterior screws through the PM approach. In addition, the measuring method for the size of fragments depending upon a plain lateral radiograph was not reliable when the fragments were rotationally displaced. In this study we recommend a new measuring method for evaluation of the size of posterior fragments based on CT scans.
Methods
Inclusion and Exclusion Criteria
This retrospective comparative study reviewed a case series from January 2012 to December 2014. All patients gave their informed consent, and the study was approved by the institutional review board. The inclusion criteria were: (i) adult patients with fresh trimalleolar ankle fractures; (ii) posterior malleolar fractures were fixed through either the PM or the PL approach; and (iii) patients with persistent posterior subluxation of the tibiotalar joint or the posterior instability with concomitant syndesmotic injury. The exclusion criteria were: (i) pathologic fractures; (ii) tibial pilon fractures (AO‐OTA 43 C Type); (iii) an inability to bear weight (for reasons other than post‐traumatic complications of the affected ankle); and (iv) loss to follow‐up within 12 months postoperatively.
Demographic Data of Patients
Forty‐eight patients were retrospectively divided into two groups based on surgeons' preference: 20 patients in the PM group and 28 patients in the PL group. All of the patients had unilateral fractures, with 19 fractures on the left and 29 on the right ankle. All patients were evaluated preoperatively with anteroposterior, lateral, mortise X‐rays, and 3D computed tomography (CT) scans. All fractures in this study had posterior malleolar fragments that involved partial articular injury. The size of the posterior fragments were measured by axial CT scans, and we evaluated them by percentage of the axial tibial plafond area.
Posteromedial Group
The mean age of the patients was 44.2 ± 13.4 years (range, 18–64 years). In the PM group, 10 of the patients were male and 10 were female. In this group, the causes of injury were a ground‐level fall for 15 patients, a motor vehicle accident for 3 patients, and falling from a height for 2 patients. Eight of the patients in the group had ankle fracture dislocations, which we reduced in the emergency department. There were 16 type 44‐B3, 3 type 44‐C1 and 1 type 44‐C2 fractures according to the AO/OTA classification. Based on the classification of Haraguchi et al. 11 patients had stage 1, 5 had stage 2, and 4 had stage 3 fractures24. The size of the posterior malleolar fragment in percentage of the axial tibial plafond area was 25.4% ± 12.5%.
Posterolateral Group
The mean age of the patients was 42.7 ± 12.3 years (range, 18–63 years). In the PL group, 20 of the patients were female and 8 were male. A total of 16 patients' fractures were caused by a ground‐level fall, 7 patients by a motor vehicle accident, 4 patients by falling from height and 1 patient by a crush injury. Seven of the patients had ankle fracture dislocations, which we reduced in the emergency department. A total of 19 patients had type 44‐B3, 3 had 44‐C1, and 6 had 44‐C2 fractures. Based on the classification of Haraguchi et al. 15 patients had stage 1, 8 had stage 2, and 5 had stage 3 fractures24. The size of the posterior malleolar fragment as a percentage of the axial tibial plafond area was 20.9% ± 7.9%.
Surgical Techniques
Posteromedial Approach
In the PM group, under combined lumbar plexus–sciatic nerve block anesthesia, patients were positioned supine on a radiolucent table. Their affected lower limbs were then prepped and draped in the usual sterile fashion. The incision was made along the tibialis posterior tendon, and the proximal limit of the incision was dependent on the metaphyseal extension of the fracture (Figs 1, 2). Entry was through the interval between the subcutaneous tissue and flexor retinaculum to the tibialis posterior tendon sheath. Dissection was continued in posterolateral and medial directions to expose the posterior and medial malleolar fragments. The articular surface could be visualized through the unreduced medial malleolar fracture. Gentle dorsiflexion of the foot aids in reduction of the posterior fragments. A large pointed reduction forcep was used to clamp the posterior malleolus, and one or two 3.0 or 3.5 mm lag screws were placed from anterior to posterior into the posterior malleolus. An additional screw was used in large posterior malleolar fragments. The aponeurotic fascia was closed with interrupted 2‐0 Vicryl suture and skin was then closed with interrupted 2‐0 Mersilk.
Figure 1.

Posteromedial approach: the incision is made along the tibialis posterior tendon and the proximal limit of the incision is dependent on the metaphyseal extension of the fracture.
Figure 2.
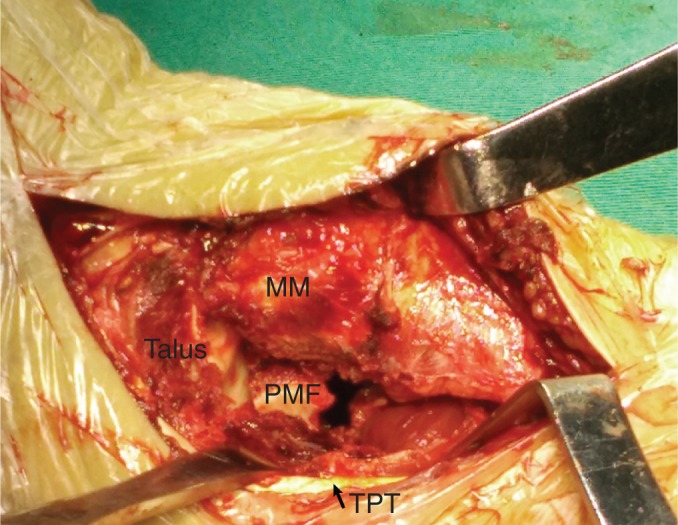
A retractor is used to pull the tibialis posterior tendon and flexor digitorum longus posteriorly. The posterior malleolar fragment and the distal tibial articular surface are clearly visualized. MM, medial malleolus; PMF, posterior malleolar fragment; TPT, tibialis posterior tendon.
Posterolateral Approach
In the PL group, under combined lumbar plexus–sciatic nerve block anesthesia, the patients were positioned lateral on a radiolucent table. Their affected lower limbs were then prepped and draped in the usual sterile fashion. The fibula and posterior malleolus were reduced and fixed first, then the patients were placed supine in order to fix the medial malleolar fractures. The skin incision was made between the posterior border of the lateral malleolus and the border of the Achilles tendon (Figs 3, 4). Entry was through the interval between the peroneal and the flexor hallucis longus muscles. The peroneal tendons were retracted medially to fix the fibula first. The flexor hallucis muscle was elevated. The extra‐articular fracture lines could guide reduction of the posterior malleolar fragments, although subtle edge comminution made it necessary to directly visualize the joint line. Multiple posterior to anterior lag screws was placed close to the joint line to maximize bone purchase. The aponeurotic fascia was closed with interrupted 2‐0 Vicryl suture and skin was then closed with interrupted 2‐0 Mersilk.
Figure 3.

Posterolateral approach: the incision is made between the posterior border of the lateral malleolus and the border of the Achilles tendon.
Figure 4.
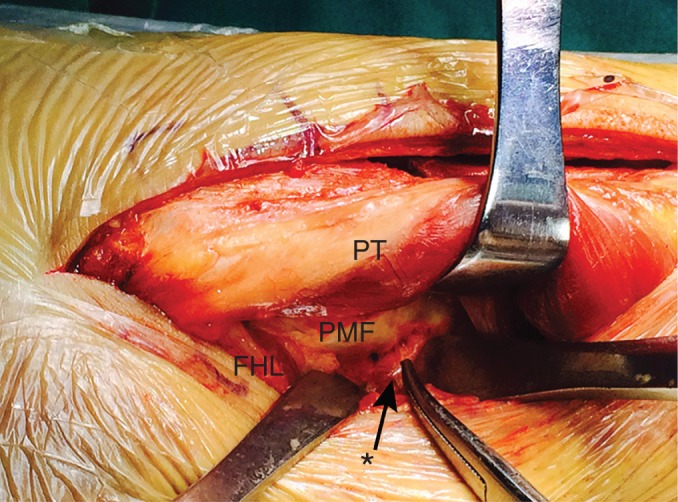
A retractor is used to pull the peroneal tendons over the fibula to expose the posterior malleolar fracture site. FHL, flexor hallucis longus; PMF, posterior malleolar fragment; PT, peroneal tendon; *, a branch of peroneal artery.
Postoperative Protocol
Postoperatively, a short leg cast in neutral position was applied for 3 weeks. All patients were kept non‐weight‐bearing for 6 weeks and started ROM exercises after we removed casts. Patients were instructed to begin 50% partial weight bearing at 6 weeks, with full weight bearing by 12 weeks. We evaluated the functions of all patients using American Orthopedic Foot and Ankle Society (AOFAS) scores and the range of motion (ROM) at the 6‐month, 12‐month and final follow‐up. We compared the ROM of the treated ankle with the contralateral ankle. Postoperative X‐rays and CT scans were performed to determine the occurrence of residual step‐off or gap in the articular reduction. The degree of arthritis was evaluated by final follow‐up X‐rays according to Bargon criteria. For analysis, Bargon grades 0 and 1 were combined representing no or mild arthritis, and grades 2 and 3 were combined representing more significant arthritis.
Statistical Analysis
The Statistical Package for Social Sciences, version 17.0 for Windows (SPSS, Chicago, IL, USA) was used for statistical analysis. The mean AOFAS scores and standard deviations of each group were calculated and compared with each other using the independent‐samples t‐test. The median loss of ROM was calculated and compared using the Mann–Whitney U‐test. The χ2 test was used to calculate differences in postoperative complications. A power analysis using (G*Power freeware) version 3.1.9.2 was performed and the statistical power was calculated to verify whether the non‐significant results were due to the lack of a relationship between the groups or the lack of statistical power.
Results
General Outcomes
All posterior malleolus were fixed by one or two screws, with the fixation of lateral malleolus using a plate, and medial malleolus using two screws. Forty‐eight patients were followed up for more than 12 mouths. The mean follow‐up was 21.3 months (range, 15–54 months) in the PM group and 21.0 months (range, 15–36 months) in the PL group. None of the patients developed delayed union or nonunion, and functional bone healing was obtained in all patients by 10.7 weeks (range, 8–16 weeks). The articular reduction was assessed intraoperatively and all patients had reduction of the joint surface within 1 mm.
American Orthopedic Foot and Ankle Society Scores
The mean AOFAS scores of the PM group at the postoperative 6‐month, 12‐month, and final follow‐up were 91.4 (range, 82–100), 92.5 (range, 84–100), and 92.9 (range, 86–100), respectively. In the PL group, the mean AOFAS scores were 89.9 (range, 72–100), 91.4 (range, 77–100), and 91.9 (range, 77–100) at the 6‐mouth, 12‐month, and final follow‐up, respectively. No significant differences were observed between the two groups at each follow‐up period (P > 0.05). Both groups had obtained similar ankle function at each follow‐up period (Table 1).
Table 1.
AOFAS scores and ROM results
| Variable | AOFAS (mean ± SD) | Loss of ROM (°) | |||
|---|---|---|---|---|---|
| 6 month | 12 month | Final follow‐up | LDF (P25, P75) | LPF (P25, P75) | |
| PM | 91.35 ± 5.69 | 92.45 ± 4.43 | 92.85 ± 4.42 | 0 (0, 5) | 0 (0, 0) |
| PL | 89.86 ± 6.40 | 91.36 ± 5.88 | 91.93 ± 5.87 | 0 (0, 5) | 0 (0, 0) |
| t | 0.83 | 0.70 | 0.59 | — | — |
| U | — | — | — | 255.00 | 279.50 |
| P | 0.409 | 0.487 | 0.557 | 0.527 | 0.986 |
AOFAS, American Orthopedic Foot and Ankle Society Scale; LDF, loss of dorsiflexion; LPF, loss of plantaflexion; PL, posterolateral; PM, posteromedial; ROM, range of motion.
Loss of Range of Motion
In the PM group, the median loss of ROM for dorsiflexion and plantaflexion were 0° (0°, 5°) and 0° (0°, 0°) at the final follow‐up, respectively. In the PL group, the median loss of ROM for dorsiflexion and plantaflexion were 0° (0°, 5°) and 0° (0°, 0°) at the final follow‐up, respectively. No significant differences were observed between the two groups at each follow‐up period (P > 0.05). Most patients in both groups did not have limitation of ankle activity (Table 1).
Postoperative Complications
Postoperative radiographs showed that 2 patients in the PM group and 2 in the PL group had a residual step‐off of 2 and 3 mm at the final follow‐up visit, respectively (P = 0.665). In the PM group, 1 patient experienced superficial infection on the 7th day postoperatively, which required no surgical intervention. Another patient experienced postoperative wound dehiscence on the 10th day postoperatively and underwent operative closure with no subsequent complications. Superficial infection also occurred in 1 patient in the PL group on the 5th day postoperatively, which completely healed in the 3rd week postoperatively without surgical intervention. None of the patients experienced peroneal nerve sensory deficit or tibialis posterior nerve‐associated complications. Two patients in the PL group and 1 in the PM group developed postoperative arthritis (Bargon grade 2 or 3) (P = 0.627). There was no significant difference between the two groups. Figures 5 and 6 show clinical examples of patients from both groups.
Figure 5.

The figure showed the right ankle of a 48‐year‐old female caused by a ground‐level fall, AO type 44B3. Preoperative mortise (A), lateral (B) radiographs and axial (C), sagittal (D) computed tomography (CT) scans of the trimalleolar fracture in the posteromedial group. Postoperative mortise (E) and lateral (F) radiographs and axial (G), sagittal (H) CT scans of the patient showed anatomic reduction with anteroposterior screws fixation.
Figure 6.

The figure shows the right ankle of a 58‐year‐old female caused by a ground‐level fall, AO type 44B3. Preoperative mortise (A), lateral (B) radiographs and axial (C), sagittal (D) computed tomography (CT) scans of the trimalleolar fracture in posterolateral group. Postoperative mortise (E) and lateral (F) radiographs and axial (G), sagittal (H) CT scans of the patient showed anatomic reduction with posteroanterior screws fixation.
We put forward a null hypothesis that the population means of the groups were equal with the probability (power) 0.813 at the 5% level of significance for our subjects. The power analysis demonstrated that we could reject the null hypothesis.
Discussion
Few published studies have compared the different approaches for the fixation of posterior malleolar fractures. Bois and Dust report the results of 12 patients with large posterior fragments or posteromedial malleolar fractures who underwent ORIF with a PM approach22. Good results were obtained, with 3 patients developing grade III arthritis. Ruokun et al. discuss 30 of 32 patients obtaining good or excellent AOFAS scores, with only 1 patient developing arthritis using a PM approach20. In our study, the mean AOFAS score regardless of groups was 92.3 at the final follow‐up, with 2 patients experiencing loss of reduction and 3 patients developing arthritis. In the present study, we obtained similar results to previous studies. We found that ankle function, including AOFAS scores and ROM, was not significantly different. There were also no statistical differences between the two groups in the percentage of patients who developed postoperative arthritis.
Most surgeons prefer to use the PL approach for the fixation of a single posterior malleolar fragment19. If the fragment is located posterolaterally, using the PL approach it is easy to access the fracture site with direct visualization of the posterior fragment. The PL approach also has other advantages. The distal fibular fractures are conveniently fixed by the PL antiglide plate, which had demonstrated improved biomechanical stability compared with the lateral locking plate in osteoporotic bone23. The PL antiglide plate also offers a reduced risk of intra‐articular screw penetration, wound healing problems, and prominent metalwork6. Traditionally, the PL approach was not the approach of choice if the fibula and medial malleolus had to be fixed at the same time25. It is awkward for the surgeon to fix the medial malleolus fracture with the patient in the prone position. Moreover, this can potentially lead to malreduction of the medial malleolus. We prefer to place the patient in the floating position if there is a combined medial malleolar fracture, and reduce the fibula first in the lateral position. When the posterior malleolar fragments are split into two main pieces, the reduction of the medial edge of posteromedial fragment is difficult using a single PL approach26. For this situation, a combined posteromedial and posterolateral approach in the prone position could help decrease those limitations as opposed to sequential posterolateral and medial approaches through lateral and then supine positions. However, the distal tibial articular surface cannot be visualized using this approach, and the reduction of posterior malleolar fragments has to be guided by the extra‐articular fracture lines. Furthermore, we should pay attention to the sural nerve which usually lies in relatively close proximity to the incision or crosses the incision27, 28. The peroneal artery and its branches can be identified during operative fixation (Fig. 4)29.
For the PM approach, the main advantage is that the distal tibial articular surface can be visualized through the unreduced medial malleolar fracture, which provides direct reduction of the posterior malleolar fragments. Gentle dorsiflexion of the foot make the tibiotalar joint subluxation, which can easily be reduced without widely stripping the soft tissue attached to a large posterior fragment. There are also some limitations for the PM approach. The neurovascular bundle is close to the dissection but not usually visualized. Overstretching the soft tissues has the potential to result in tibialis posterior nerve or artery injury. The fixation type in the PM group may also be associated with soft tissue complications. Patel et al. describe a case of tibial nerve impingement by an anteroposterior screw inserted for stabilization of a posterior malleolar fracture30. We measured lengths of the screws to avoid tibialis posterior tendon and tibial nerve irritation caused by the protrusion of screws. None of our patients in the PM group experienced a tibial nerve or tibialis posterior tendon irritation. Anteroposterior screws could not provide enough interfragmentary compression while the threads of lag screws partially crossed the fracture line31. In our study, the screws partially threaded in 10 patients and a step‐off of 2 mm occurred in only 1 patient. Although the two techniques have own their advantages and disadvantages, we found that there was no statistical difference between them in regards to postoperative complications.
The size of the fragments were usually measured by using simple radiographs, Ferries et al. determined that it was inaccurate to assess the size of the posterior fragments using simple radiographs32. Haraguchi et al. argued for the use of CT to obtain the most reliable estimate of fragment size24. We evaluated the size of the posterior malleolar fragments as a percentage of the axial tibial plafond area, which was measured on the axial CT scans, instead of the sagittal tibial plafond diameter. The indications for ORIF of posterior malleolus include the size of the posterior fragments measured on the plain radiographs. Our measurement approach meant that the sizes of the posterior fragments were determined more accurately, which also affected the indications for ORIF of posterior malleolus.
There are limitations to this study. First, our study is a retrospective analysis of available information, and there may be selective bias. Second, simple radiographs were sometimes not standardized and the posterior fracture could be hidden by the lateral plate. Third, PM and PL groups did not randomize, so the type of medial and lateral malleolus fractures may affect the results. We did not obtain CT scans for every patient at final follow‐up. Furthermore, the duration of follow‐up was short and long‐term follow‐up is necessary.
Conclusion
There were no statistical differences between PM and PL approaches for posterior malleolar fractures in AOFAS scores, ROM, and postoperative complications. Hence, we conclude that the approaches have similar clinical and radiographic outcomes. Surgeons should choose the appropriate approach based on their experience. More importantly, anatomical reduction and stable fixation of the intra‐articular fractures may be critical regardless of the fixation technique. More prospective studies and randomized controlled trials are necessary to support this conclusion.
Disclosure: The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of the article.
References
- 1. Daly PJ, Fitzgerald RH, Melton LJ, Llstrup DM. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand, 1987, 58: 539–544. [DOI] [PubMed] [Google Scholar]
- 2. Garrett WE, Swiontkowski MF, Weinstein JN, et al. American board of orthopaedic surgery practice of the orthopaedic surgeon: part‐II, certification examination case mix. J Bone Joint Surg Am, 2006, 88: 660–667. [DOI] [PubMed] [Google Scholar]
- 3. Court‐Brown CM, McBirnie J, Wilson G. Adult ankle fractures—an increasing problem?. Acta Orthop Scand, 1998, 69: 43–47. [DOI] [PubMed] [Google Scholar]
- 4. Jaskulka RA, Ittner G, Schedl R. Fractures of the posterior tibial margin: their role in the prognosis of malleolar fractures. J Trauma, 1989, 29: 1565–1570. [DOI] [PubMed] [Google Scholar]
- 5. David MH, Colton CL. Malleolar fractures In: Rüedi TP, Murphy WM, eds. AO Principles of Fracture Management, 1st edn. New York: Thieme, 2000; 559–582. [Google Scholar]
- 6. Marsh J, Saltzman C. Ankle fractures In: Bucholz RW, Heckman JD, Court‐Brown C, Tornetta P, Koval KJ, eds. Rockwood and Green's Fractures in Adults, 6th edn. Philadelphia: Lippincott, Williams, & Wilkins, 2005; 2147–2249. [Google Scholar]
- 7. Harper MC, Hardin G. Posterior malleolar fractures of the ankle associated with external rotation‐abduction injuries. Results with and without internal fixation. J Bone Joint Surg Am, 1988, 70: 1348–1356. [PubMed] [Google Scholar]
- 8. Mont MA, Sedlin ED, Weiner LS, Miller AR. Postoperative radiographs as predictors of clinical outcome in unstable ankle fractures. J Orthop Trauma, 1992, 6: 352–357. [DOI] [PubMed] [Google Scholar]
- 9. Forberger J, Sabandal PV, Dietrich M, Gralla J, Lattmann T, Platz A. Posterolateral approach to the displaced posterior malleolus: functional outcome and local morbidity. Foot Ankle Int, 2009, 30: 309–314. [DOI] [PubMed] [Google Scholar]
- 10. Xu H, Li X, Zhang D, et al. A retrospective study of posterior malleolus fractures. Int Orthop, 2012, 36: 1929–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Drijfhout van Hooff CC, Verhage SM, Hoogendoorn JM. Influence of fragment size and postoperative joint congruency on long‐term outcome of posterior malleolar fractures. Foot Ankle Int, 2015, 36: 673–678. [DOI] [PubMed] [Google Scholar]
- 12. Hartford JM, Gorczyca JT, McNamara JL, Mayor MB. Tibiotalar contact area. Contribution of posterior malleolus and deltoid ligament. Clin Orthop Relat Res, 1995, 320: 182–187. [PubMed] [Google Scholar]
- 13. Langenhuijsen JF, Heetveld MJ, Ultee JM, Steller EP, Butzelaar RM. Results of ankle fractures with involvement of the posterior tibial margin. J Trauma, 2002, 53: 55–60. [DOI] [PubMed] [Google Scholar]
- 14. Lee HJ, Kang KS, Kang SY, Lee JS. Percutaneous reduction technique using a Kirschner wire for displaced posterior malleolar fractures. Foot Ankle Int, 2009, 30: 157–159. [DOI] [PubMed] [Google Scholar]
- 15. Bartoníček J, Rammelt S, Tuček M, Naňka O. Posterior malleolar fractures of the ankle. Eur J Trauma Emerg Surg, 2015, 41: 587–600. [DOI] [PubMed] [Google Scholar]
- 16. Kao KF, Huang PJ, Chen YW, Cheng YM, Lin SY, Ko SH. Postero‐medio‐anterior approach of the ankle for the pilon fracture. Injury, 2000, 31: 71–74. [DOI] [PubMed] [Google Scholar]
- 17. Amorosa LF, Brown GD, Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma, 2010, 24: 188–193. [DOI] [PubMed] [Google Scholar]
- 18. O'Connor TJ, Mueller B, Ly TV, Jacobson AR, Nelson ER, Cole PA. “A to P” screw versus posterolateral plate for posterior malleolus fixation in trimalleolar ankle fractures. J Orthop Trauma, 2015, 29: 151–156. [DOI] [PubMed] [Google Scholar]
- 19. Abdelgawad AA, Kadous A, Kanlic E. Posterolateral approach for treatment of posterior malleolus fracture of the ankle. J Foot Ankle Surg, 2011, 50: 607–611. [DOI] [PubMed] [Google Scholar]
- 20. Ruokun H, Ming X, Zhihong X, et al. Postoperative radiographic and clinical assessment of the treatment of posterior tibial plafond fractures using a posterior lateral incisional approach. J Foot Ankle Surg, 2014, 53: 678–682. [DOI] [PubMed] [Google Scholar]
- 21. Erdem MN, Erken HY, Burc H, Saka G, Korkmaz MF, Aydogan M. Comparison of lag screw versus buttress plate fixation of posterior malleolar fractures. Foot Ankle Int, 2014, 35: 1022–1030. [DOI] [PubMed] [Google Scholar]
- 22. Bois AJ, Dust W. Posterior fracture dislocation of the ankle: technique and clinical experience using a posteromedial surgical approach. J Orthop Trauma, 2008, 22: 629–636. [DOI] [PubMed] [Google Scholar]
- 23. Minihane KP, Lee C, Ahn C, Zhang LQ, Merk BR. Comparison of lateral locking plate and antiglide plate for fixation of distal fibular fractures in osteoporotic bone: a biomechanical study. J Orthop Trauma, 2006, 20: 562–566. [DOI] [PubMed] [Google Scholar]
- 24. Haraguchi N, Haruyama H, Toga H, Kato F. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am, 2006, 88: 1085–1092. [DOI] [PubMed] [Google Scholar]
- 25. Hoppenfeld S, DeBoer P, Buckley R. Surgical Exposures in Orthopadics. The Anatomic Approach, 4th edn. Philadelphia: Lippincott Williams & Wilkins, 2009; 644–653. [Google Scholar]
- 26. Weber M. Trimalleolar fractures with impaction of the posteromedial tibial plafond: implications for talar stability. Foot Ankle Int, 2004, 25: 716–727. [DOI] [PubMed] [Google Scholar]
- 27. Jowett AJL, Sheikh FT, Carare RO, Goodwin MI. Location of the sural nerve during posterolateral approach to the ankle. Foot Ankle Int, 2010, 31: 880–883. [DOI] [PubMed] [Google Scholar]
- 28. Webb J, Moorjani N, Radford M. Anatomy of the sural nerve and its relation to the Achilles tendon. Foot Ankle Int, 2000, 21: 475–477. [DOI] [PubMed] [Google Scholar]
- 29. Lidder S, Masterson S, Dreu M, Clement H, Grechenig S. The risk of injury to the peroneal artery in the posterolateral approach to the distal tibia: a cadaver study. J Orthop Trauma, 2014, 28: 534–537. [DOI] [PubMed] [Google Scholar]
- 30. Patel A, Charles L, Ritchie J. A complication of posterior malleolar fracture fixation. J Foot Ankle Surg, 2016, 55: 383–386. [DOI] [PubMed] [Google Scholar]
- 31. Stephan MP, Robert F, Markus H, Slobodan T. Lag screws In: Rüedi TP, Murphy WM, eds. AO Principles of Fracture Management, 1st edn. New York: Thieme, 2000; 157–168. [Google Scholar]
- 32. Ferries JS, DeCoster TA, Firoozbakhsh KK, Garcia JF, Miller RA. Plain radiographic interpretation in trimalleolar ankle fractures poorly assesses posterior fragment size. J Orthop Trauma, 1994, 8: 328–331. [DOI] [PubMed] [Google Scholar]


